Running Head: Perceived Stress and Outcomes in COPD
Funding support: The Comparing Urban and Rural Effects of Poverty on COPD (CURE COPD) study was developed under Assistance Agreement No. 83615001 awarded by the U.S. Environmental Protection Agency (EPA). It has not been formally reviewed by the EPA. The views expressed in this document are solely those of the authors and do not necessarily reflect those of the Agency. The EPA does not endorse any products or commercial services mentioned in this publication. CURE COPD was supported by the National Institute for Minority Health and Health Disparities P50MD010431. OO is supported by the National Heart, Lung, and Blood Institute (NHLBI) T32HL007534. AF was supported by the National Institute of Environmental Health Sciences F32ES028576 and NHLBI K23HL151758.
Date of Acceptance: January 29, 2025 │ Publication Online Date: February 11, 2025
Abbreviations: 8-OHdG=8-hydroxydeoxyguanosine; 11dTxB2=11-dehydro-thromboxane B2; CAT=COPD Assessment Test; CCQ=Clinical COPD Questionnaire; CI=confidence interval; COPD=chronic obstructive pulmonary disease; CURE COPD=Comparing Urban and Rural Effects of Poverty on COPD; ECSC=Ease of Cough and Sputum Clearance Questionnaire; ELISA=enzyme-linked immunosorbent assays; FEV1=forced expiratory volume in 1 second; FEV1%pred=forced expiratory volume in 1 second percentage predicted; GOLD=Global initiative for chronic Obstructive Lung Disease; IFN=interferon; IL=interleukin; MCID=minimum clinically important difference; HADS=Hospital Anxiety and Depression Scale; mMRC=modified Medical Research Council; PSS=Perceived Stress Scale; SD=standard deviation; SGRQ=St George’s Respiratory Questionnaire; TBARS=thiobarbituric acid reactive substances; TNF=tumor necrosis factor
Citation: Offor O, Eakin MN, Woo H, et al. Perceived stress is associated with health outcomes, platelet activation, and oxidative stress in COPD. Chronic Obstr Pulm Dis. 2025; 12(2): 98-108. doi: http://doi.org/10.15326/jcopdf.2024.0561
Online Supplemental Material: Read Online Supplemental Material (263KB)
Introduction
Psychosocial factors such as loneliness, social isolation, emotional support, and perceived stress disproportionately affect individuals suffering from chronic diseases and significantly impact health outcomes.1 Perceived stress is an individual’s appraisal of how unpredictable, uncontrollable, and overloaded their life is.2 In cardiovascular disease, high perceived stress, along with other psychosocial factors, are associated with worse outcomes,3-6 and biopsychosocial pathways have been identified as predictors of disease outcomes.7 Whether high levels of perceived stress among individuals with chronic obstructive pulmonary disease (COPD) impact respiratory outcomes is unknown, and the mechanisms by which psychosocial factors play a role in COPD is understudied.
In COPD, increasing exertional dyspnea, lack of energy, and limitations in daily activities result in deteriorating quality of life and impact mental health symptoms.8 Several studies have shown a higher prevalence of symptoms of anxiety and depression among individuals with COPD, which are associated with adverse clinical outcomes.9,10 There is limited literature on the biological mechanisms and pathways by which psychosocial factors, such as perceived stress, may impact COPD outcomes and potentially be therapeutically targeted.
Several studies have identified heightened platelet activation, oxidative stress, and systemic inflammation as extrapulmonary manifestations of COPD that impact COPD morbidity.11-14 Additionally, prior studies have shown an association between acute and chronic psychological stress with increased and sustained proinflammatory platelet activation.15,16 This study aims to evaluate the association of perceived stress with respiratory outcomes in COPD and explore the association of perceived stress with platelet activation, oxidative stress, and systemic inflammation in a prospective cohort study of former smokers enriched with individuals from a low-income urban setting disproportionately impacted by psychosocial factors. Elevated levels of the systemic platelet activation marker 11-dehydro-thromboxane-B2 (11dTxB2), a stable metabolite of thromboxane A2, have been associated with worse respiratory symptoms and quality of life in this cohort.17,18 Oxidative stress, the imbalance between toxic oxidants and protective antioxidants, has been identified as pertinent to the pathobiology of COPD.19 Finally, chronic systemic inflammation involving dysregulation of pro- and anti-inflammatory cytokines is an established hallmark of COPD.20 We hypothesize that, in this cohort with a higher burden of psychosocial factors such as perceived stress, elevated perceived stress will be associated with worse respiratory outcomes including symptoms, quality of life, and exacerbations as well as elevated platelet activation, oxidative stress, and systemic inflammation.
Methods
Study Population and Study Design
Comparing Urban and Rural Effects of Poverty on COPD (CURE COPD) was a longitudinal observational study of former smokers with COPD from low-income urban areas examining the impact of obesity, adverse dietary patterns, and indoor air pollution on adverse respiratory outcomes. Eligible participants were aged 40 years and older with moderate-to-severe COPD (forced expiratory volume in 1 second [FEV1] <80% predicted, FEV1/forced vital capacity <0.7), former smokers with a smoking history of ≥10 years, and residence in low-income neighborhoods (defined as census tract poverty rate >10%) or having public insurance or high school education or less. Participants were evaluated at baseline, 3-month, and 6-month visits with questionnaires to assess perceived stress, and biospecimens were collected at each visit. The study protocol was approved by the Johns Hopkins School of Medicine Institutional Review Board and written consent was obtained from all participants prior to data collection.
Psychological Stress Assessment
The Perceived Stress Scale (PSS) was administered by trained research staff at each study visit to assess perceived stress over the past month. PSS is a validated 10-item self-reported instrument, with each item assessed on a 5-point Likert scale (maximum 40 points). Although not psychometrically validated, recent studies by Medvedev et al and Townsend et al describe evaluations of the robustness of the PSS as a categorical scale, including ordinal and linear transformations of PSS scores.21,22 PSS score categories have been described, and tertiles of the continuous scale with cut-offs for low (0–13), moderate (14–26), and high (24–40) stress used in population health studies.22-24 The PSS score category for each participant was determined at each study visit.
Respiratory Outcomes
Validated questionnaires were used at each study visit to assess respiratory-related quality of life (St George's Respiratory Questionnaire [SGRQ]), respiratory health status (COPD Assessment Test [CAT] and Clinical COPD Questionnaire [CCQ]), and respiratory symptoms (modified Medical Research Council [mMRC] scale and Ease of Cough and Sputum Clearance [ECSC] questionnaire). The minimum clinically important difference (MCID) was defined as a difference in score of 4 for SGRQ,25 a difference of 2 for CAT,26 and 0.4 for CCQ,27 but has not been defined for mMRC or ECSC. Incidence of exacerbations was assessed at each study visit and with monthly telephone interviews. At baseline, participants were asked “In the past 12 months, have you been to the emergency room or hospitalized for any lung problems?” For longitudinal exacerbations, the initial question was either “Have you had a flare-up of your chest trouble in the past month or since your last study contact?” when elicited during phone calls or “Have you had a flare-up of your chest trouble in the last 3 months?” when assessed at study visits. A moderate exacerbation was defined as treatment with antibiotics or corticosteroids, a visit to an urgent care facility, or an unscheduled visit to a doctor’s office due to COPD-related illness. A severe exacerbation was defined as a COPD-related emergency department visit or hospitalization. Spirometry was performed at each study visit using the American Thoracic Society protocol.28 A race-neutral percentage predicted FEV1 was recalculated at the time of analysis using the Global Lung Function Initiative equation29 which led to some participants categorized as having moderate COPD at enrollment to be recategorized as having mild COPD.
Biomarker Assessment
Markers of platelet activation (urine 11dTxB2), oxidative stress (urine thiobarbituric acid reactive substances [TBARS], 8-hydroxydeoxyguanosine [8-OHdG], and 8-isoprostane), and inflammation (serum tumor necrosis factor-α, interleukin [IL]-6, IL-8, interferon-γ) were measured at each study visit. Serum and urine specimens were collected, aliquoted, and stored at -80⁰C. Serum biomarkers were analyzed at the conclusion of the study whereas urine biomarkers (except 11dTxB2) were analyzed in batches. Serum biomarkers were measured using a custom multiplex assay at the University of Maryland Cytokine Core Laboratory (Luminex MAGPIX platform; Austin, Texas). Enzyme-linked immunosorbent assays (ELISA) were used to analyze urine samples at the Johns Hopkins Institute for Clinical and Translational Research Core Laboratory, including 11dTxB2 (Enzo Life Sciences; Lyon, France), TBARS (BioAssay Systems; Hayward, California), 8-OHdG (Antibody online GMBH), and 8-isoprostane (8-iso-PGF2α; Cayman Chemical). All urine assays were adjusted for urine creatinine also measured using ELISA (Quidel Corporation; San Diego, California) by dividing the measured value by the urine creatinine level. Samples with undetectable levels of a biomarker were assigned a value that is half of the value of the lower limit of detection. Samples that exceeded the upper limit of detection were diluted to obtain a numeric value.
Statistical Analysis
Baseline participant characteristics were summarized using means with standard deviations (SD) for continuous variables and frequency (n, %) for categorical variables PSS was assessed30,31 continuously with results scaled to a 4-point increase to reflect the PSS MCID of 4. Additional analyses also explored PSS categorically as tertiles of the continuous scale, using intervals of low (0–13), moderate (14–26), and high (24–40) stress. In all analyses, biomarkers were log-transformed because of skewed distributions, and comparisons are reported as percentage differences. The association between concurrently collected PSS and respiratory outcome questionnaires or biomarkers measured repeatedly across all visits was evaluated using generalized linear mixed models. The association between PSS and incidence of at least one exacerbation (yes/no) was assessed using generalized logistic mixed models that included PSS data from all visits. All models accounted for repeated measures and were adjusted for baseline age, gender, race, educational attainment (high school degree or above versus less than high school degree), annual household income level (above or below $30,000), pack years smoked, baseline body mass index, FEV1 percentage predicted, and history of cardiovascular disease or diabetes. History of cardiovascular disease was defined as a baseline history of congestive heart failure, stroke, heart attack, or percutaneous coronary angiography. Models assessing urinary biomarkers (except 11dTxB2) were additionally adjusted for batch number and urine 11dTxB2 models were also adjusted for aspirin use. Effect modification by COPD severity was tested for each outcome by adding to the model a multiplicative interaction between continuous PSS and COPD severity classified as mild-moderate (Global initiative for chronic Obstructive Lung Diseases [GOLD]32 category ≤2; FEV1>50% predicted) or severe (GOLD≥3; FEV1<50% predicted) with a significance threshold of p=0.1, and results for all outcomes are presented stratified by COPD severity. To explore whether associations with perceived stress were independent of symptoms of depression and anxiety, food insecurity, or neighborhood socioeconomic factors, sensitivity analyses were conducted further adjusting for: (1) Hospital Anxiety and Depression Scale (HADS) score, dichotomized as having any anxiety (HADS-Anixety≥8) or depressive symptoms (HADS-Depression≥8) at each study visit; (2) Household Food Insecurity Access Scale score, dichotomized as having food insecurity during any study visits; and (3) national ranking percentile of Area Deprivation Index at baseline.33-35 To explore whether associations of perceived stress with respiratory outcomes and biomarkers were differently impacted by the outbreak of COVID-19, we repeated our analyses excluding all data obtained after March 15, 2020, during the height of the pandemic. All analyses were performed using STATA version 15.1 (StataCorp; College Station, Texas).
Results
Study Population Characteristics
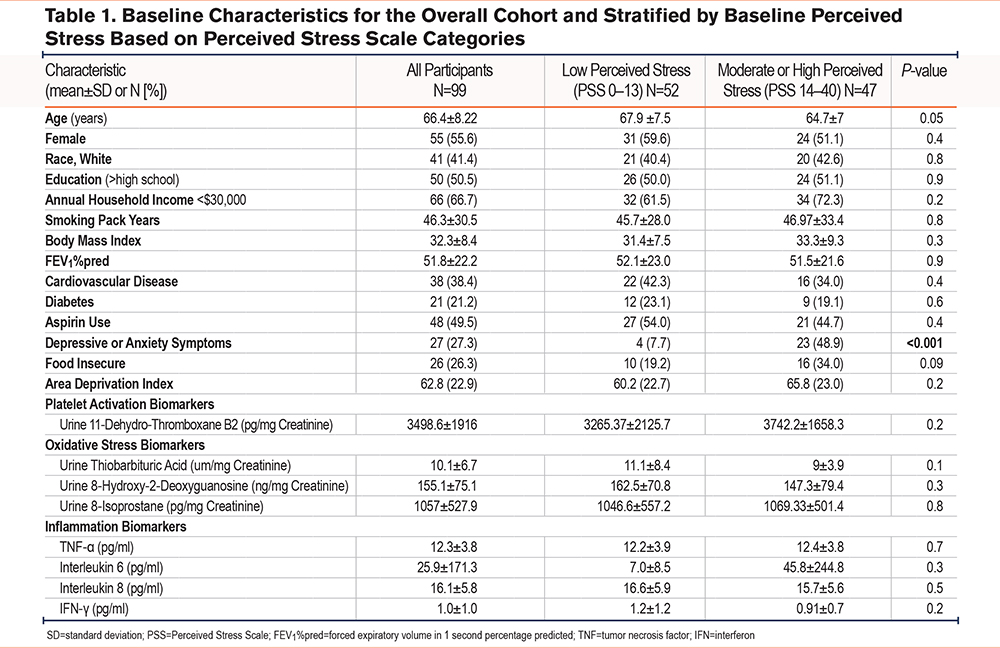
Of the 116 individuals recruited into the study, 17 (14.7%) withdrew before all baseline data was collected resulting in 99 participants completing a baseline visit between 2016 and 2021. The mean age of the study population was 66.4 years, 56% female, 57% Black, and the participants on average had moderate COPD (Table 1). At baseline, the mean±SD PSS score was 12.9±6.4, with 52 (52.5%) participants in the lowest tertile (0–13), 45 (45.5%) in the middle tertile, and 2 (2.0%) in the highest tertile of PSS scores. The mean PSS was similar at each follow-up visit (14.1±8.6 at 3 months and 12.8±8.1 at 6 months). Although most participants reported PSS scores within the same category throughout the study period, 38.4% moved between categories at least once (Supplemental Figure 1 in the online supplement). Average baseline biomarker levels are presented in Table 1.
Associations Between Perceived Stress and COPD Morbidity
Among all participants, a 4-point increase in PSS score was associated with a higher CAT score (mean difference [β] 0.91; 95% confidence interval [CI]: 0.40, 1.43), SGRQ (β 2.17; 95%CI: 1.21, 3.13), CCQ (β 0.11; 95%CI: 0.05, 0.17), and ECSC (β 0.36; 95%CI: 0.11, 0.61) but not mMRC (β 0.03; 95%CI: -0.05, 0.10) or odds of at least one exacerbation during the 12-month study period (Supplemental Table 1 in the online supplement). Compared with low PSS, moderate PSS and high PSS were associated with progressively worse respiratory symptoms, with the association between high versus low PSS and CAT, SGRQ, and CCQ all surpassing the MCID (Table 2). In addition, compared with low stress, high stress was associated with a 4.15 higher odds of at least one moderate/severe COPD exacerbation (95%CI 1.28, 13.47) over the 12 months. Moderate stress was not associated with odds of experiencing an exacerbation (Table 2).
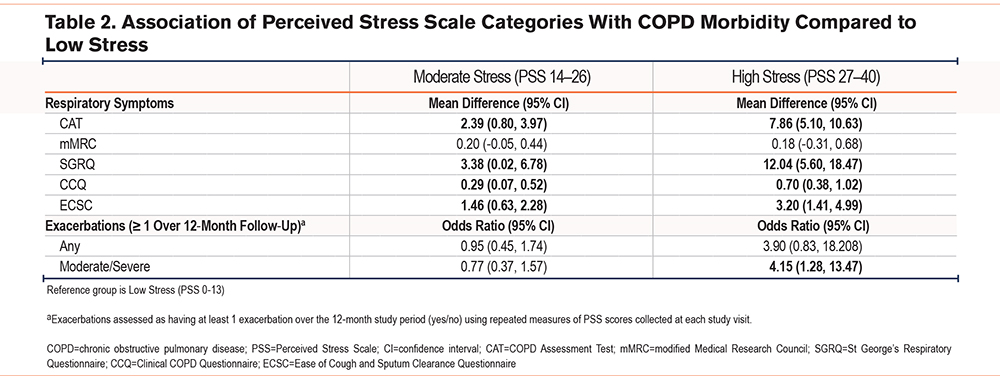
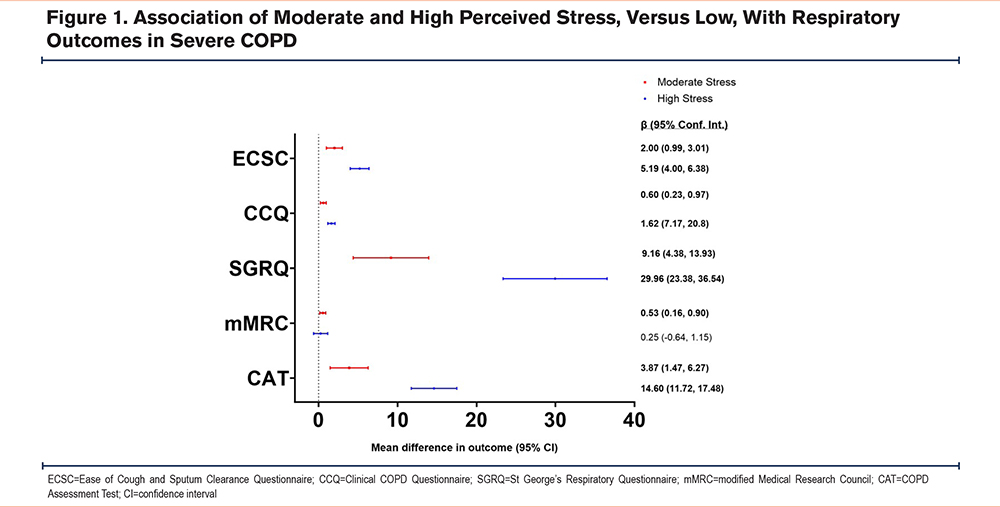
There was significant effect modification by COPD severity for CAT (pinteraction=0.04), SGRQ (pinteraction<0.01), CCQ (pinteraction<0.01), and ECSC (pinteraction=0.04). In stratified analyses, the PSS was only associated with respiratory outcomes among those with severe COPD (GOLD≥3) wherein a 4-point increase in PSS was associated with a higher CAT (β 1.50; 95%CI: 0.74, 2.25), mMRC (β 0.11; 95%CI: 0.01, 0.22), SGRQ (β 3.95; 95%CI: 2.39, 5.52), CCQ (β 0.22; 95%CI: 0.13, 0.32), and ECSC (β 0.64; 95%CI: 0.38, 0.90), but not with mild-moderate COPD (GOLD≤2) (Supplemental Table 1 in the online supplement). Similarly, when considering PSS categories, associations were strongest and most consistent among individuals with severe COPD. Among individuals with severe COPD, compared to low stress, both moderate and high stress were associated with an elevated CAT, SGRQ, CCQ, and ECSC at levels above the MCID (Figure 1). Among individuals with mild-moderate COPD, compared to individuals with low stress, high stress was associated with an elevated CAT (β 5.84; 95%CI: 2.94, 8.74), SGRQ (β 8.06; 95%CI: 01.58, 14.54), and CCQ (β 0.45; 95%CI: 0.15, 0.76) scores above the MCID but moderate stress was not associated with any clinical outcomes (Supplemental Table 2 in the online supplement). Results were similar in sensitivity analysis models additionally adjusting for symptoms of anxiety or depression, food insecurity, and area deprivation index with only small attenuation of effects in respiratory outcomes (Supplemental Table 3 in the online supplement).
Associations Between Perceived Stress and Biomarkers
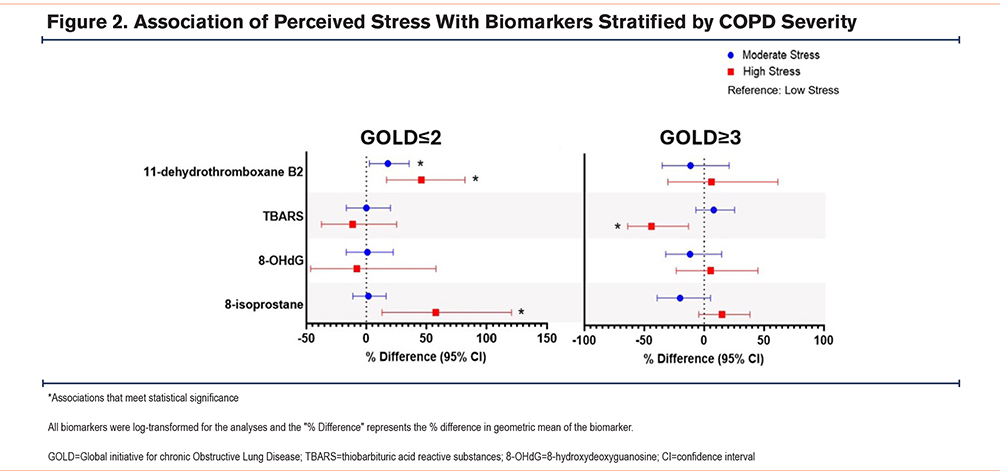
Among all participants, there were no associations between a 4-point increase in PSS with markers of inflammation or oxidative stress (Supplemental Table 4 in the online supplement) though there was a trend toward higher urine 11dTxB2 (β 2.8%; 95%CI: -0.5%, 6.3%) with higher PSS. There was significant effect modification between PSS and COPD disease severity for TBARS (pinteraction=0.07) and 8-isoprostane (pinteraction=0.06).
In stratified analyses, among participants with mild-moderate COPD, a 4-point increase in PSS was associated with a 6.0% higher level of urine 11dTxB2 (95%CI: 1.6, 10.6) and 8-isoprostane (β 4.9%; 95%CI: 0.7%, 9.3%) but there were no associations with inflammatory markers or other oxidative stress markers (Supplemental Table 4 in the online supplement). In categorical analyses, compared to low stress, moderate stress (β=20.1%, 95%CI: 3.1, 40.0%) and high stress (β=52.9%, 95%CI:22.1, 91.6%) were associated with progressively higher urine thromboxane and high stress was also associated with higher 8-isoprostane (β=59.4%; 95%CI: 20.6, 110.8%) but not with any other biomarkers (Figure 2, Supplemental Table 5 in the online supplement). Among individuals with severe COPD, a 4-point increase in PSS was associated with a 6.5% lower level of urine TBARS (95%CI: -11.6, -1.0) and compared to low stress, high stress was associated with 53.9% lower levels of urine TBARS (95%CI: -64.8, -39.7). There were no associations between PSS and any other biomarkers among individuals with severe COPD (Supplemental Table 5 in the online supplement).
Results were similar in analyses excluding all data obtained after March 15, 2020, during the height of the COVID-19 pandemic.
Discussion
In an urban cohort of low-income former smokers with COPD, perceived stress was associated with worse respiratory morbidity, particularly among those with severe COPD. Additionally, higher levels of perceived stress were associated with elevated systemic platelet activation and oxidative stress markers among individuals with mild-moderate COPD but not with inflammation. These findings add to the growing evidence that psychosocial factors contribute to COPD outcomes, though impacts on underlying biological mechanisms may differ by disease severity.
COPD presents significant challenges to the physical and psychological well-being of individuals, and in turn, psychosocial factors impact respiratory health.36 There are many potential drivers of psychosocial stress in COPD including financial stress from the cost of health care, and adverse social circumstances such as neighborhood violence, community deprivation, and emotional and physical neglect.36-38 Previous studies have demonstrated that food insecurity and social isolation contribute to high stress and adverse outcomes in COPD.39,40 In this study we found that associations between perceived stress and respiratory symptoms were independent of food insecurity, area deprivation index, and anxiety and depression symptoms, suggesting that perceived stress is an important measure that represents psychosocial factors beyond symptoms of depression or anxiety, food insecurity, and area deprivation. Additionally, the burden of respiratory symptoms and physical debility may lead to a bidirectional association wherein respiratory disease morbidity is the primary driver of perceived stress, particularly in more severe disease. As was the case in this study, others have demonstrated that associations of perceived stress and depression with COPD morbidity are strongest among individuals with more severe disease.41 Importantly, our analysis demonstrated that the association of perceived stress with COPD outcomes is independent of depression and anxiety symptoms.
The relationship between psychosocial factors and underlying pathobiological mechanisms has been poorly studied in COPD. This study focused on 3 mechanisms of interest in COPD that have been associated with adverse clinical outcomes: systemic inflammation, platelet activation, and oxidative stress. Although there were no associations between systemic inflammatory markers and perceived stress in this study, platelet activation and oxidative stress were associated with perceived stress in subgroup analyses that stratified participants based on COPD severity. Among individuals with mild-moderate COPD, high perceived stress was associated with higher levels of urine 11dTxB2 and 8-isoprostane whereas, among those with severe COPD, high perceived stress was associated with lower TBARS. Urine 11dTxB2, a stable metabolite of the platelet activation product thromboxane A2(TxA2)42 has previously been associated with worse respiratory symptoms in COPD.17,18 Platelet activation in response to acute and chronic stress has been associated with the release of serotonin and chemokines from platelet-dense granules, and increased surface expression of markers of platelet activation.15 These changes have also been demonstrated in psychological disorders such as anxiety and depression which have been associated with serotonin and cytokine dysregulation.15,43 Recent studies have identified platelets as a possible link between cardiovascular disease and chronic stress, and these results suggest that similar pathophysiological changes may occur in chronic respiratory diseases such as COPD.4,15 Likewise, several studies have implicated endogenous oxidative stress as a driver of COPD pathogenesis due to the persistence of elevated markers of oxidative stress in the absence of continued exposure to traditional sources that generate reactive oxygen species and are implicated in COPD pathogenesis such as cigarette smoke and pollution.44,45 Acute and chronic psychosocial stress have been associated with oxidative stress and lower antioxidant activity in both animal and human studies.46,47 Of the oxidative stress markers investigated in this study, both 8-isoprostane and TBARS reflect lipid peroxidation while 8OHDG reflects oxidative DNA damage.
Notably we identified discrepant findings between perceived stress and respiratory symptoms or biomarkers based on COPD severity. This may reflect a decoupling of the relationship between perceived stress and underlying biological mechanisms wherein psychosocial stressors such as perceived stress dominate in mild-moderate disease. However, respiratory symptoms are a primary driver of systemic manifestations such as oxidative stress and platelet activation in severe COPD. Alternatively, our models may better account for confounding factors of the relationship between biological mechanisms and perceived stress in milder COPD, whereas, residual confounding may mask associations with more severe COPD. Unmeasured confounders such as genetics, social support, and personality traits of optimism or pessimism may also account for discrepant results between individuals with mild-moderate and severe COPD.48 The inverse association between TBARS and perceived stress among individuals with severe COPD may reflect the dynamic nature of the imbalance between prooxidant and antioxidant processes which changes with disease progression.49 Airway oxidative stress is complex and has been associated with adaptive responses to disease progression that may play a role in mitigating ongoing inflammation.49,50 Genetic and psychosocial factors may also play a role in this adaptive response by increasing antioxidant defenses resulting in varying levels of oxidative stress markers as disease progresses.50,51 Statistical limitations of generalized estimating equations with smaller sample sizes and in handling complex time-varying covariates may also explain discrepant findings with severe COPD and urine TBARS.52
This study is limited by a relatively small sample size drawn from a single center and enriched with socioeconomically disadvantaged individuals living in an urban environment, potentially limiting generalizability. Although this was a highly selected population that would be expected to have higher prevalence of perceived stress and other adverse social determinants of health, few reported high perceived stress throughout the study period which limited the power to detect differences. Biomarkers of platelet activation and oxidative stress were measured in urine, reflecting these biological mechanisms systemically without corresponding samples to characterize these biological processes in the lung compartment. Finally, we had inadequate power to investigate whether specific biological mechanisms mediated associations between perceived stress and respiratory outcomes which should be investigated in larger studies.
In conclusion, perceived stress was associated with worse respiratory morbidity, particularly among individuals with severe COPD, and with higher levels of systemic platelet activation and lipid peroxidation among individuals with mild-moderate COPD. This study suggests that individuals with milder COPD may exhibit a relationship between psychosocial stress and adverse biological mechanisms that are potential therapeutic targets.
Acknowledgments
Author contributions: OO, NH, NP, and AF provided study conceptualization, HW provided data analysis, and ME, MW, and MC provided resources. OO, NP, and AF were responsible for methodology, and NH was responsible for funding acquisition, with NP and AF providing supervision. OO wrote the manuscript’s original draft and ME, HW, DB, MW, SR, MM, NH, NP, and AF contributed to the manuscript’s writing, review and editing. All authors approved the manuscript for publication.
Declaration of Interests
NP reports reimbursement for participation in advisory boards for Verona and AstraZeneca, both unrelated to the work published. NP reports funding from the National Institutes of Health (NIH)/ National Institute of Environmental Health, and the NIH/National Institute of Allergy and Infectious Diseases, both also unrelated to the work. All other authors have no financial relationships or conflicts of interest related to the submitted work.