Running Head: COPD Foundation Guide
Funding Support: Not applicable
Date of Acceptance: March 7, 2014
Abbreviations: mobile device application, app; American Thoracic Society, ATS; European Respiratory Society, ERS; National Clinical Guideline Centre, NICE; Global Initiative for chronic Obstructive Lung Disease, GOLD; American College of Physicians, ACP; American College of Chest Physicians, ACCP; forced volume capacity, FVC; forced expiratory volume in 1 second, FEV1; spirometry grade, SG; computed tomography, CT
Citation: Thomashow B, Crapo J, Yawn B, McIvor A, Cerreta S, Walsh J, Mannino D, Rennard S. The COPD Foundation Pocket Consultant Guide. Chronic Obstr Pulm Dis. 2014; 1(1): 83-87. doi: http://doi.org/10.15326/jcopdf.1.1.2014.0124
Introduction
Guidelines have evolved into large, evidence-based, textbook-like documents and are hence becoming less practical for the pragmatic physician. Little effort during guideline development is spent considering dissemination or implementation.
The COPD Foundation Guide to COPD Diagnosis and Treatment (the Guide) is designed to provide best practice advice for the clinician. Originally developed in partnership with the NewYork- Presbyterian Healthcare System and launched in 2006 as the Pocket Consultant Card, the Guide has been updated frequently as new treatments have been introduced and as the information base regarding COPD has increased.1
The Guide is meant to be practical, easy-to-use and designed to address the key questions faced by a clinician. It is not a formal guideline. The Guide recommendations differ in several respects from other documents such as the American Thoracic Society/European Respiratory Society (ATS/ERS) COPD statement, the National Clinical Guideline Centre (NICE) recommendations and the Global Initiative for chronic Obstructive Lung Disease (GOLD) strategy document, which are excellent, but lengthy and often not very specific.2-6
Spirometry Recommendations
The Guide makes specific recommendations on who should have spirometry.1 All agree that spirometry is warranted in individuals with symptoms of dyspnea on exertion, cough, sputum, decreased physical activity levels and fatigue. However, in contrast to the consensus statement from ATS/ERS/American College of Physicians (ACP)/American College of Chest Physicians (ACCP) in 2011 that recommended against performing spirometry in individuals at risk for COPD but without symptoms, the Guide recommends spirometry for individuals at-risk who have comorbidities associated with COPD.1,7
This is recommended because many patients under-appreciate symptoms or ascribe limitations based on their age, weight, deconditioning or allergies. Patients often do not report symptoms due to short health care provider visits. Comorbidities are extremely common in COPD and COPD appears to be an independent risk factor for a number of conditions including cardiovascular disease.8-9 Misdiagnosis is a problem of potential major importance for individual patients. The Guide suggests that spirometry be considered in individuals at-risk who have one or more significant comorbid diseases.1 The Guide recommends testing all COPD patients for alpha-1antitrypsin deficiency.10
The Guide’s staging of spirometry was designed to be comprehensive. Five spirometry grades are described to ensure that all individuals fit into a group. The fact that many individuals are unclassified by other systems, but may have problems, has been an impediment for many clinicians 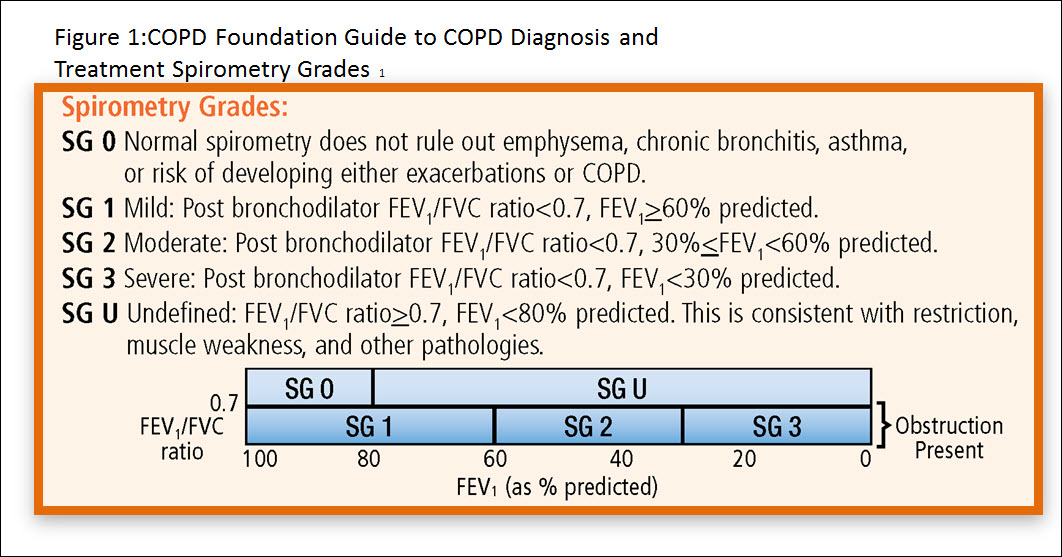 .
.
Spirometry grade 0 (SG-0) includes normal individuals as well as individuals who may have disease but whose measured values remain within the normal population boundary. SG-0 does not exclude the presence of emphysema, chronic bronchitis or the risk of developing exacerbations. Further, individuals within SG-0 may have symptoms requiring treatment.
Spirometry grade U (SG-U) includes those with a normal forced expiratory volume in 1 second to forced volume capacity (FEV1 /FVC) ratio but reduced FVC and FEV1. This group has classically been described as having restrictive lung disease. Recent evidence shows that many of these individuals have emphysema and/or airway inflammation on computed tomography (CT) scanning.11
The Guide describes three obstructive grades all with an FEV1/FVC ratio <0.7 and follows the recommendations of the ATS/ERS/ACP/ACCP Consensus Statement7:
Spirometry grade-1 (SG-1), mild, with FEV1≥60% predicted
Spirometry grade-2 (SG-2), moderate, with FEV1<60% predicted and≥30% predicted
Spirometry grade-3 (SG-3), severe, with FEV1<30%predicted
The previously mentioned consensus statement stressed the importance of an FEV1 of 60% in determining those who might benefit from regular maintenance therapy. 7 The Guide has adjusted the spirometry grades to reflect this cut-off for those with significant COPD where management should be based on patient performance as well as symptoms.1 Spirometric severity <30% is a reasonable guide to initiate management plans for those with severe disease, although spirometry is but one measure of COPD severity.
COPD Severity Domains
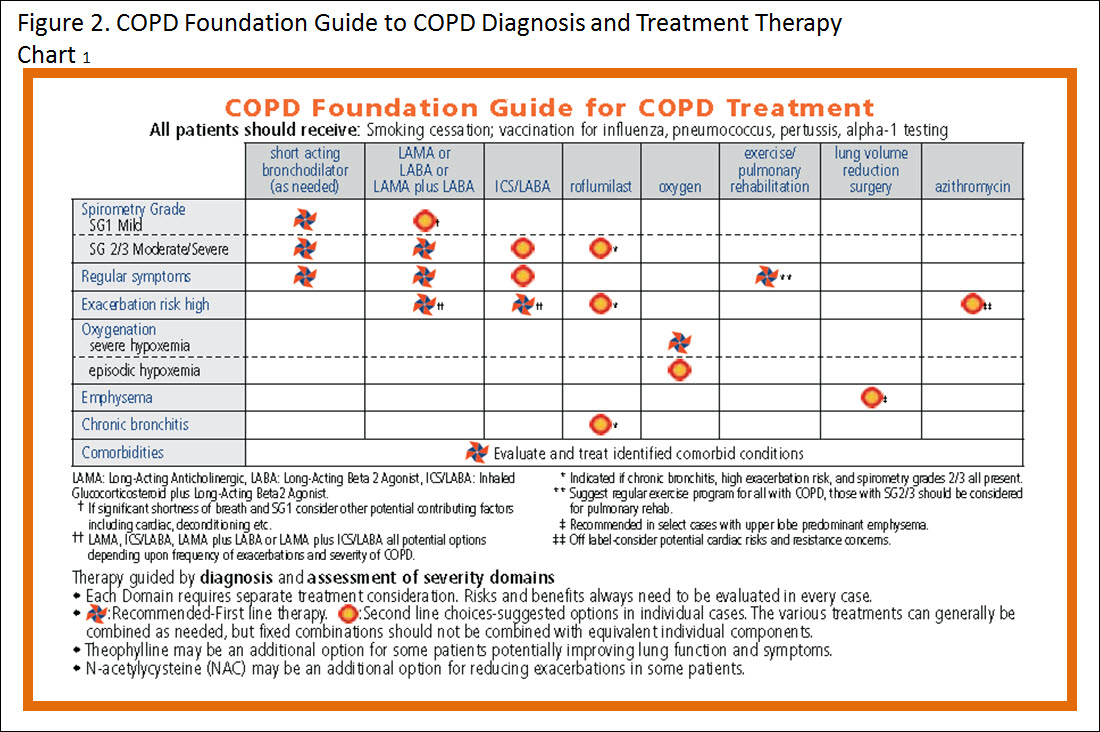 To address the heterogeneous clinical problems that beset COPD patients, the 2013 revision of the Guide suggested an approach based upon 7 severity domains: spirometry, symptoms, exacerbations, oxygenation, the presence of emphysema, the presence of chronic bronchitis, and comorbidities.1 A Therapy Chart listing the 7 severity domains in rows and recommended therapy options in columns is a new feature. This approach can guide clinicians to make decisions appropriate for the heterogeneous problems faced by COPD patients in a systematic and easily implemented fashion.
To address the heterogeneous clinical problems that beset COPD patients, the 2013 revision of the Guide suggested an approach based upon 7 severity domains: spirometry, symptoms, exacerbations, oxygenation, the presence of emphysema, the presence of chronic bronchitis, and comorbidities.1 A Therapy Chart listing the 7 severity domains in rows and recommended therapy options in columns is a new feature. This approach can guide clinicians to make decisions appropriate for the heterogeneous problems faced by COPD patients in a systematic and easily implemented fashion.
Accessibility of the Guide
The COPD Foundation is committed to making the Guide freely available in multiple formats. Pocket cards and mobile device applications (apps) are inexpensive tools to aid in practice change. The advantage of the online, eHealth format is the possibility it offers to easily alter, update or evolve and improve the information in a dynamic fashion.12
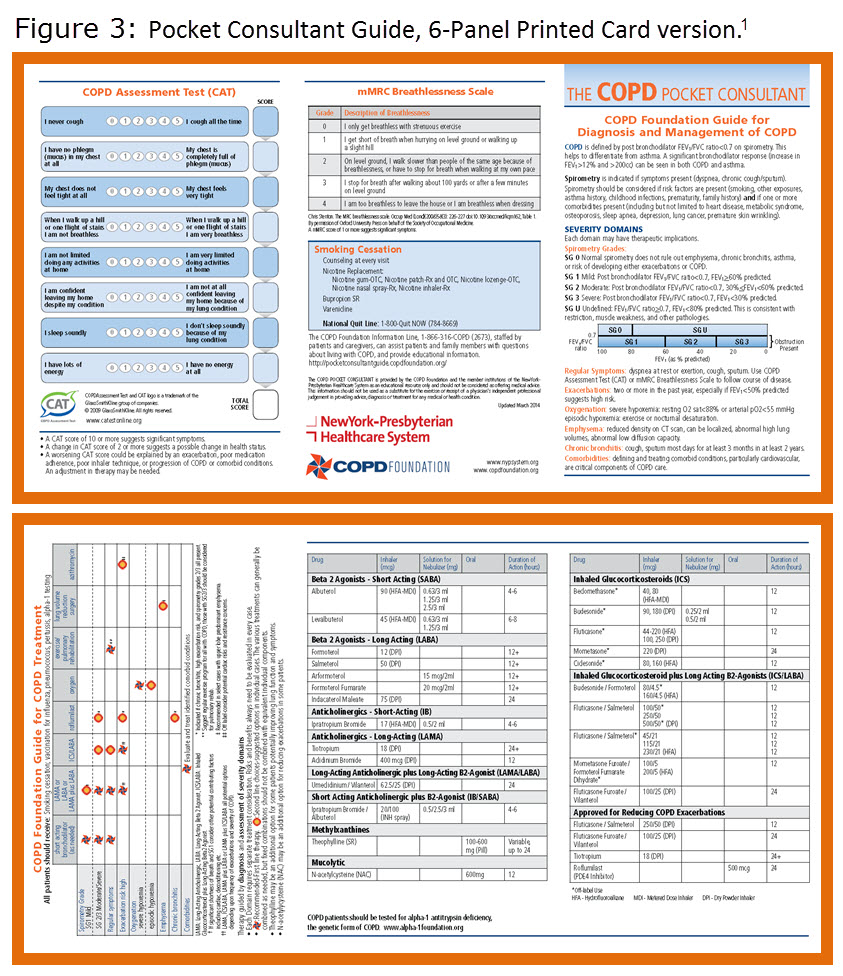 The Pocket Consultant Guide card is available in a 2-panel version that provides basic information on diagnosis and therapy and two 6-panel versions that include information on diagnostic tools and commonly used medications--one with generic names and one with brand names. The Pocket Consultant Guide card is available to health care providers at no cost. Printed cards can be ordered from the COPD Foundation’s online catalogue (http://copd.oiondemand.com).13 Electronic downloads can be obtained from the Pocket Consultant Guide Online Community site (http://pocketconsultantguide.copdfoundation.org ).14
The Pocket Consultant Guide card is available in a 2-panel version that provides basic information on diagnosis and therapy and two 6-panel versions that include information on diagnostic tools and commonly used medications--one with generic names and one with brand names. The Pocket Consultant Guide card is available to health care providers at no cost. Printed cards can be ordered from the COPD Foundation’s online catalogue (http://copd.oiondemand.com).13 Electronic downloads can be obtained from the Pocket Consultant Guide Online Community site (http://pocketconsultantguide.copdfoundation.org ).14
 In addition, the Foundation has launched a free i-Phone app that allows the Guide to be used in a more interactive format. The first edition of the app lists available generic medications. Subsequent editions will allow the user to toggle between brand name and generic name drugs. An edition featuring European medications is also being developed. The app can be found in the Apple App Store by searching COPD Foundation. An Android app is under development as well and will be released in Summer 2014.
In addition, the Foundation has launched a free i-Phone app that allows the Guide to be used in a more interactive format. The first edition of the app lists available generic medications. Subsequent editions will allow the user to toggle between brand name and generic name drugs. An edition featuring European medications is also being developed. The app can be found in the Apple App Store by searching COPD Foundation. An Android app is under development as well and will be released in Summer 2014.
To facilitate implementation of the Guide, the COPD Foundation has prepared an Institutional Pack. These can be ordered from the online catalogue13 and includes a variety of cards, posters and other materials. A Grand Rounds PowerPoint slide deck with Notes for the presenter is also available for free download from the Pocket Consultant Guide Online Community website. 14
The Guide is designed to be a practical and useful clinical tool. Future revisions that reflect changes in clinical knowledge and practice will take place at least once per calendar year. The most current revision was released March 2014. To facilitate the broadest possible base for improving the Guide going forward, the COPD Foundation has launched a social collaboration website, the Pocket Consultant Guide Online Community at pocketconsultantguide.copdfoundation.org.14 In addition to a download library and information about how to use the Guide, there is a community forum for health care professionals to discuss the Guide. Subsequent revisions to the Guide will be based on these conversations.