Running Head: Ventilatory Mechanics Before and After LVRS
Funding Support: This publication was supported, in part, by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1 TR000040.
Date of Acceptance:October 17, 2014
Abbreviations: lung volume reduction surgery, LVRS; optoelectronic plethysmography, OEP; maximum voluntary ventilation, MVV; beats per minute, BPM; forced expiratory volume in 1 second, FEV1; inspiratory duty cycle, TI/TTOT%; total lung capacity, TLC; residual lung volume, RV; dynamic lung hyperinflation, DH; National Emphysema Treatment Trial, NETT; San Diego Shortness of Breath Questionnaire, SOBQ; fraction of inspired oxygen, FiO2; heart rate, HR; peak volume of oxygen consumption,VO2; blood oxygen level, SpO2; percentage of predicted heart rate reserve, %HRR; pulmonary ribcage compartment, RCp; abdominal ribcage compartment, RCa; abdominal compartment, Ab; percent contribution of the pulmonary ribcage compartment to total tidal volume, %RCp; percent contribution of the abdominal ribcage compartment to total tidal volume, % RCa; percent contribution of the abdominal compartment to total tidal volume, %Ab; body mass index, BMI; tidal volume,VT; tidal volume of the pulmonary ribcage compartment, VT RCp; tidal volume of the abdominal ribcage compartment, VT RCa; tidal volume of the abdominal compartment, VT Ab; residual lung volume to total lung capacity, RV/TLC; pulmonary ribcage end expiratory volume, RCpEEV; abdominal ribcage end expiratory volume, RCaEEV; forced vital capacity, FVC; change in spirometry measure after bronchodilator, Chg w/BD; diffusing capacity of the lung for carbon monoxide, DLCO; minute ventilation, VE; 6-minute walking distance, 6MWD; ventilatory equivalent per liter of carbon dioxide expelled, VE/VCO2; ventilatory equivalent per liter of oxygen expelled, VE/VO2 end-expiratory volume of the entire chest wall, CWEEV; end-expiratory volume of the pulmonary ribcage compartment, RCpEEV; end-expiratory volume of the abdominal ribcage compartment, RCaEEV; end-expiratory volume of the abdominal compartment, AbEEV
Citation: Layton AM, Armstrong HF, Moran SL, et al. Quantification of improvements in static and dynamic ventilatory measures following lung volume reduction surgery for severe COPD.
Chronic Obstr Pulm Dis. 2015; 2(1): 61-69. doi:
http://doi.org/10.15326/jcopdf.2.1.2014.0145
Introduction
Lung volume reduction surgery (LVRS) has been found to improve exercise capacity, lung function, quality of life scores, and dyspnea scores in patients with predominately upper lobe emphysema.1-3 Decreased thoracic distension with associated improved respiratory mechanics have been proposed as mechanisms for these benefits.2 Therefore, the prime candidates for LVRS are those with significant lung hyperinflation.4 Such lung hyperinflation, quantified at rest by abnormally high static total lung capacity (TLC) and residual lung volume (RV), has been linked to increased dyspnea and mortality, and decreased exercise capacity.5 Dynamic lung hyperinflation (DH) more difficult to measure, has been hypothesized to alter ventilatory mechanics and is one of many postulated mechanisms for increased exertional dyspnea and exercise intolerance in patients with COPD.5 Patients with severe COPD and lung hyperinflation also exhibit inspiratory muscle weakness and, potentially, dysfunction that may contribute to impaired ventilatory mechanics.6,7 LVRS, by decreasing lung hyperinflation, may thereby improve static and dynamic ventilatory mechanics.
The traditional approach to measuring DH has been to have patients perform serial inspiratory capacity maneuvers throughout exercise. A decrease in the inspiratory capacity relative to rest indicates the presence of DH. Although this technique has been found to be reliable in patients with COPD,5 it provides only a single volume at a given point in exercise and provides no information about the various contributions of each of the components of the respiratory system to gas trapping and hyperinflation. Optoelectronic plethysmography (OEP), a novel, non-invasive motion analysis technology, provides an alternative means for measuring DH which assesses the various compartmental volume changes in patients with severe COPD. OEP divides the chest wall into 3 mechanical compartments, thus allowing for quantification of compartmental chest wall movement and tidal volume changes 8 and potential insight into how such changes in stationary ventilatory mechanics impact spirometric lung function and clinical parameters including dyspnea and exercise capacity.
The purpose of this study was to investigate changes in chest wall mechanics and volumes during tidal breathing and during maximal voluntary breathing in patients with severe COPD before and after LVRS, and to determine if such changes correspond with improvements in spirometric measurements, exercise capacity, and dyspnea.
Materials and Methods
Participants
Consecutive patients who were eligible for LVRS by the National Emphysema Treatment Trial (NETT) criteria9 were recruited for the study. All patients were receiving treatment for their emphysema, and were referred for LVRS by their treating pulmonologist or thoracic surgeon to the Center for Chest Disease at Columbia University Medical Center. Informed written consent, as approved by Columbia University’s Institutional Review Board, was obtained consecutively in 22 patients with Global initiative for chronic Obstructive Lung Disease stage III or IV COPD.
Study Design
This was a non-randomized, observational study. Individuals were first evaluated within 1-2 months preceding LVRS, after having completed a pulmonary rehabilitation program, and re-evaluated within 12 months post-LVRS (mean follow up = 7 months ± 2 months). Demographic and anthropometric measures were obtained day of testing.Patients were instructed to take all normally prescribed medications prior to testing. Evaluations consisted of spirometry, OEP measurements at rest and during a maximal voluntary ventilation (MVV) maneuver prior to exercise, and cardiopulmonary exercise testing measures via a metabolic cart with stationary ergometer.
Measurements and Equipment
All spirometry and exercise testing were performed by NETT protocol.9,10 The University of California, San Diego Shortness of Breath Questionnaire (SOBQ)10 was used to acquire self-administered ratings of dyspnea associated with activities of daily living. This is a 6-point scale (0= “not at all” to 5 = “maximum or unable to do because of breathlessness”). Total SOBQ scores range from 0-120.3
Pulmonary Function: Spirometry followed NETT protocol, including post bronchodilator changes.10 Spirometry and body plethysmography were performed using Vmax Autobox v62J and Sensormedics Vmax software version e29-1 (Yorba Linda, CA).
Cardiopulmonary Exercise Testing:Symptom limitedincremental exercise testing was performed using a Carefusion Vmax Encore 29 series metabolic cart and Viasprint 2900 cycle ergometer (Carefusion, Palm Springs, California) with the participant breathing supplemental inspired oxygen throughout exercise (fraction of inspired oxygen [FiO2] 29.99 ± 0.25%), per NETT protocol, via a closed system. Tests consisted of a 5-minute baseline measurement phase, a 3-minute warm-up consisting of pedaling against 5 watts of resistance, and a ramping exercise phase at a ramp of 5 watts per minute if the MVV was < 40 L/min or a ramp of 10 watts per minute if the MVV was > 40 L/min. Blood pressure was obtained with a stethoscope and blood pressure cuff (Welch Allyn adult arm blood pressure cuff, Welch Allyn, Skaneateles Falls, New York ) and assessed and recorded at 1-2 minute intervals throughout the test. Electrical activity of the heart was monitored continuously using a 12-lead electrocardiogram (Cardio V4 MDL37 ECG, Cardiosoft, Houston, Texas). Arterial oxygen saturation was monitored from the index finger continuously with pulse oximetry (Nellcor N-600x Pulse Oximeter with Oximax, Covidien-Nellcor, Boulder, Colorado). The following variables were collected and included in the analysis: resting and peak heart rate (HR), peak volume of oxygen consumption (VO2 , mL/kg/min and L/min), peak power (Watts), expiratory flow (L/sec), breathing reserve (L/min), duty cycle (Ti/Ttot,),blood oxygen level (SpO2), and end-tidal CO2 (PetCO2, mmHg). Age predicted peak HR was calculated as = 208-0.7 x age.11 The percentage of predicted heart rate reserve (%HRR) was calculated as = (HRmax– HRrest) / ([age predicted HR]– HRrest) x 100.12
Six Minute Walk Tests: A 6-minute walk test was performed with the patient breathing ambient air or supplemental oxygen as determined by NETT protocol. The corridor utilized for testing was >100 feet long, with 2 turning points (1 at each end of the 100 feet). Heart rate, rating of perceived dyspnea, rating of perceived exertion (using the modified Borg scale) and SpO2, were monitored before the test, at minute 6, and at recovery minutes 1 and 2.
Optoelectronic plethysmography (OEP): Chest wall volumes were assessed by OEP, an optical tracking system (BTS SpA 20024 Garbagnate Milanese, MI, Italy) that analyzed the motion of 89 retro-reflective markers adhered to the individual’s chest, abdomen and back, as described by us and others.13,14 Briefly, the optical tracking system consisted of 8 video cameras, 3 in front of the patient and 3 behind, connected to an automatic motion analyzer (OEP, BTS bioengineering, Milano, Italy). Each set of cameras was aligned at approximately head height in a semicircle around the patient. The cameras recorded the motion of the markers so that their 3-dimensional displacements were reconstructed using stereo-photogrammetric methods. OEP was analyzed for both absolute and percentage contributions from 3 chest wall component changes. Total chest wall volume was calculated and divided into 3 thoraco-abdominal compartments, expressed in absolute volume contribution to tidal volume: the pulmonary ribcage compartment (RCp) from clavicle to xiphoid process, the abdominal ribcage compartment (RCa) from xiphoid process to lower costal margin) and the abdomen compartment (Ab) from lower costal margin to the anterior superior iliac spines. The percentage contribution from each of these compartments to total tidal volume was quantified respectively as %RCp, %RCa, and %Ab. Tidal volumes collected by OEP have been previously validated against tidal volumes collected by mass flow meter.14 To determine variations from normal compartmental utilization, resting and MVV OEP data were collected from 13 healthy age and body mass index (BMI) matched controls. Changes in end expiratory chest wall and compartmental volumes were measured during tidal breathing and throughout a 12- second MVV maneuver in all participants. A video of the OEP assessed reconstructed chest wall of a representative participant pre-LVRS performing MVV maneuver is attached.
Data Analysis
Post hoc power analysis was performed to determine effect size within our population on %RCp, %RCa, %Ab and tidal volume of the pulmonary ribcage compartment (VT RCp), tidal volume of the abdominal ribcage compartment (VT RCa), and tidal volume of the abdominal compartment (VT Ab) using a SPSS v21 statistical software program (IBM Corp, Armonk, New York).
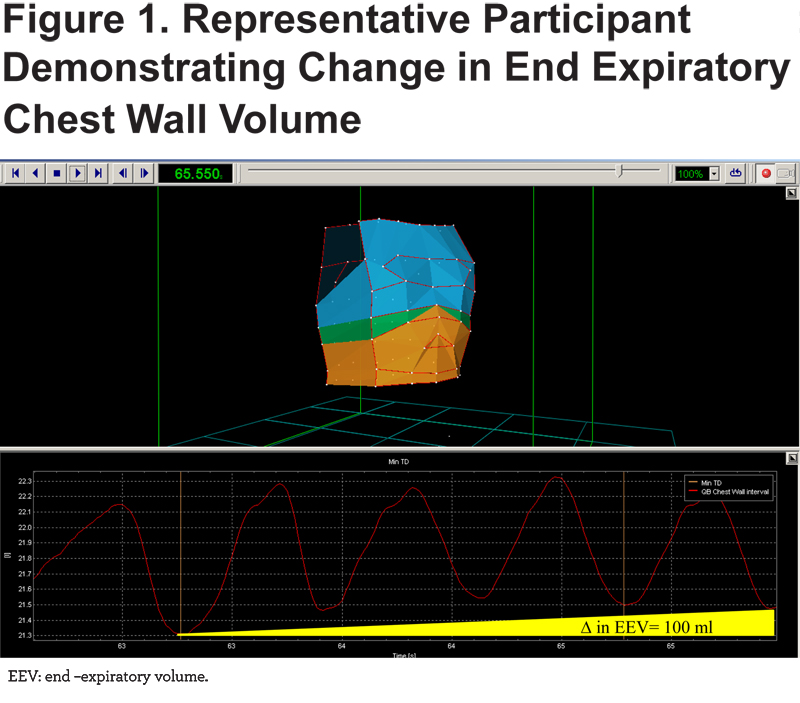
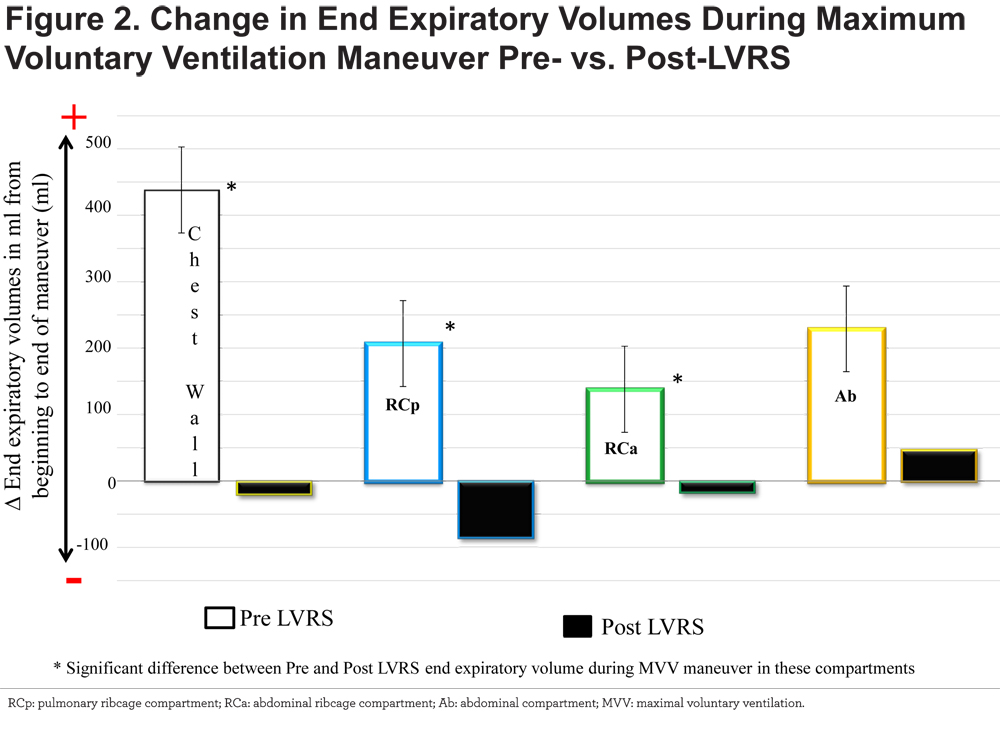
The following analyses were completed using SAS V. 9.4 (SAS Institute, Cary, North Carolina). Differences in spirometric, exercise and OEP outcome measures before and after LVRS were analyzed. Change in end expiratory volume with MVV was calculated as the end-expiratory volume at the end of the maneuver minus the end expiratory volume at the beginning of the maneuver. A positive value was considered an increase in end expiratory volume and thus hyperinflation; a negative value was considered a decrease in end expiratory volume and a normal response to increased tidal volumes over time (Figure 1).
All variables are presented as mean ± standard deviation, with the exception of gender, which is presented as frequency (percentage). Between group comparisons (before and after LVRS) were performed using a paired samples t-test (Tables 1-4). Correlations were determined with Pearson’s Correlation Coefficients. The relationships between parameters were determined with a generalized linear model. All tests were 2-tailed and statistical significance was set a priori at an a=0.05.
Results
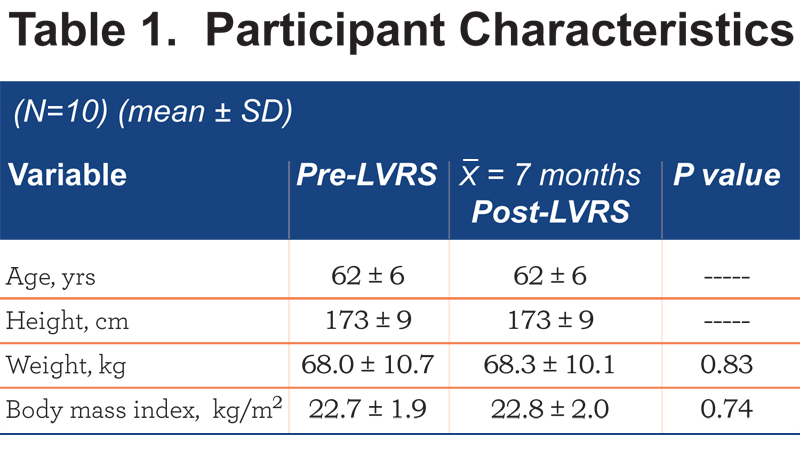
Eleven patients met NETT criteria for surgical eligibility after recruitment and were approved by the LVRS team as appropriate surgical candidates (6 females, 5 males). One female patient withdrew from the research study post surgical intervention; thus the final analysis included 5 females and 5 males. Table 1 summarizes patients’ anthropometric measurements before and after LVRS. There were no significant differences in the patients’ anthropometric measurements after surgery.
Predominately upper lobe disease was present in all patients with the average right side perfusion being: upper = 7.0 ± 3.6%, middle =25.4 ± 4.8%, lower =19.9 ± 5.0% and the average left side perfusion being: upper = 8.1 ± 4.1%, middle = 23.0 ± 5.7%, lower =15.7 ± 7.4%.
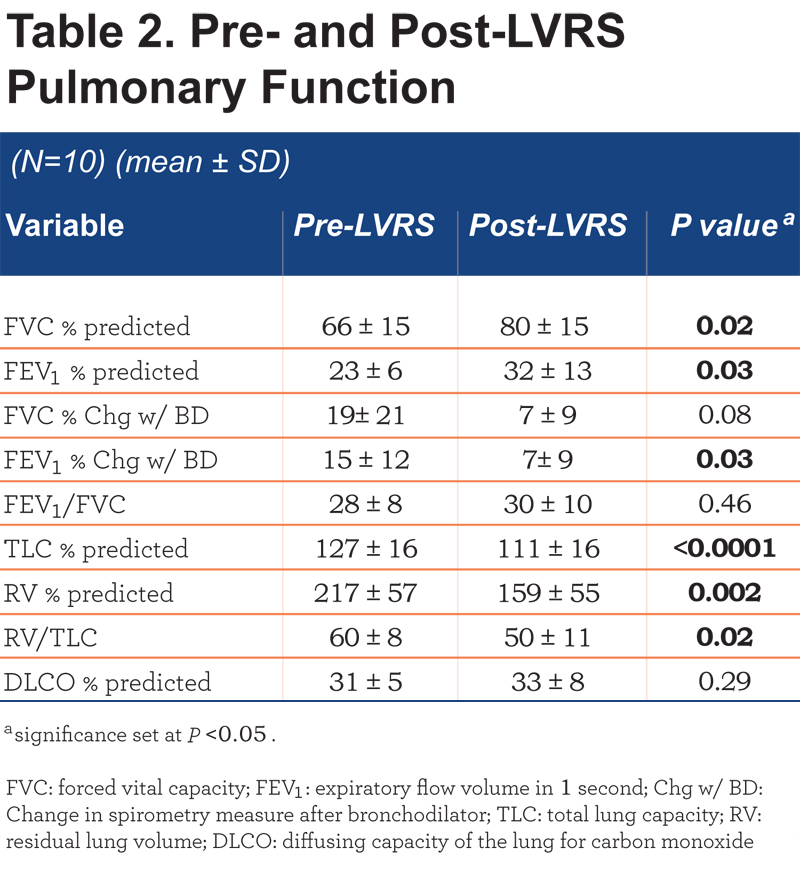
Patients demonstrated significant improvements post-LVRS: the forced vital capacity (FVC) percentage reference normal, the forced expiratory volume in 1 second (FEV1) percentage reference normal, and the total lung capacity (TLC) percentage reference normal all increased, while, residual lung volume (RV) percentage reference normal, and the ratio of residual lung volume to total lung capacity (RV/TLC) decreased. Response to a bronchodilator significantly decreased after LVRS. Single breath diffusion capacity for CO was unchanged.
Dyspnea
Patients demonstrated a significant improvement in their self report dyspnea survey scores by the SOBQ with LVRS (pre 2.50 ± 0.97 versus post 1.20 ± 0.92, p=0.01). During exercise, the dyspnea score by modified Borg scale was also significantly improved at an iso-workload post-LVRS (P=0.042) (Table 3).
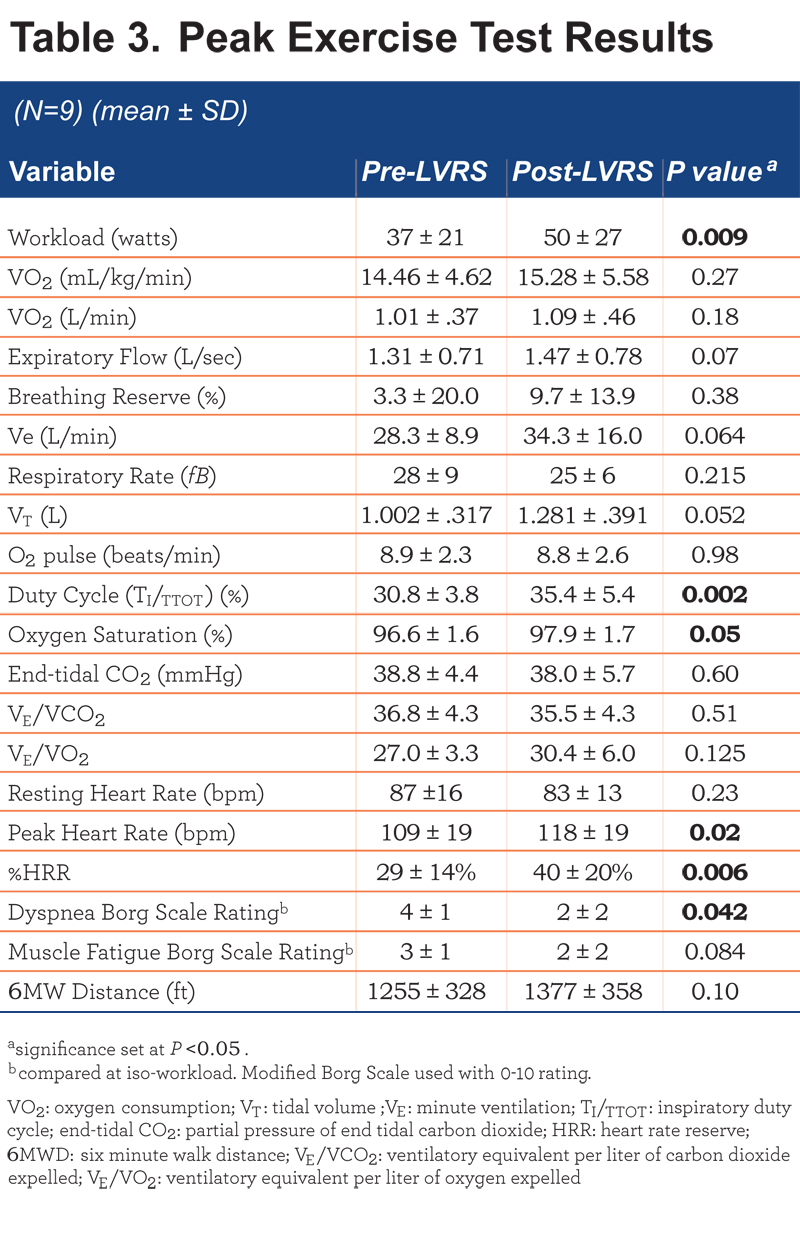
Exercise Test Results (Table 3)
COPD patients demonstrated significant improvements post- LVRS in: TI/TTOT, peak oxygen saturation, peak HR and %HRR (as a measure of chronotropic competence). Peak workload increase approached statistical significance (P=0.07). One patient decreased peak workload after LVRS. This patient was recovering from a pneumococcal pneumonia and still on high doses of prednisone during her follow up visit (discharged from a 5-day hospital stay, 3 weeks prior to the exercise testing). When this patient was removed from the analysis, the difference in post-LVRS increase in peak workload became significant for the group (P=0.009). There were no other changes in the significance of any other parameter with the removal of this outlier.
Optoelectronic Plethysmography (Table 4)
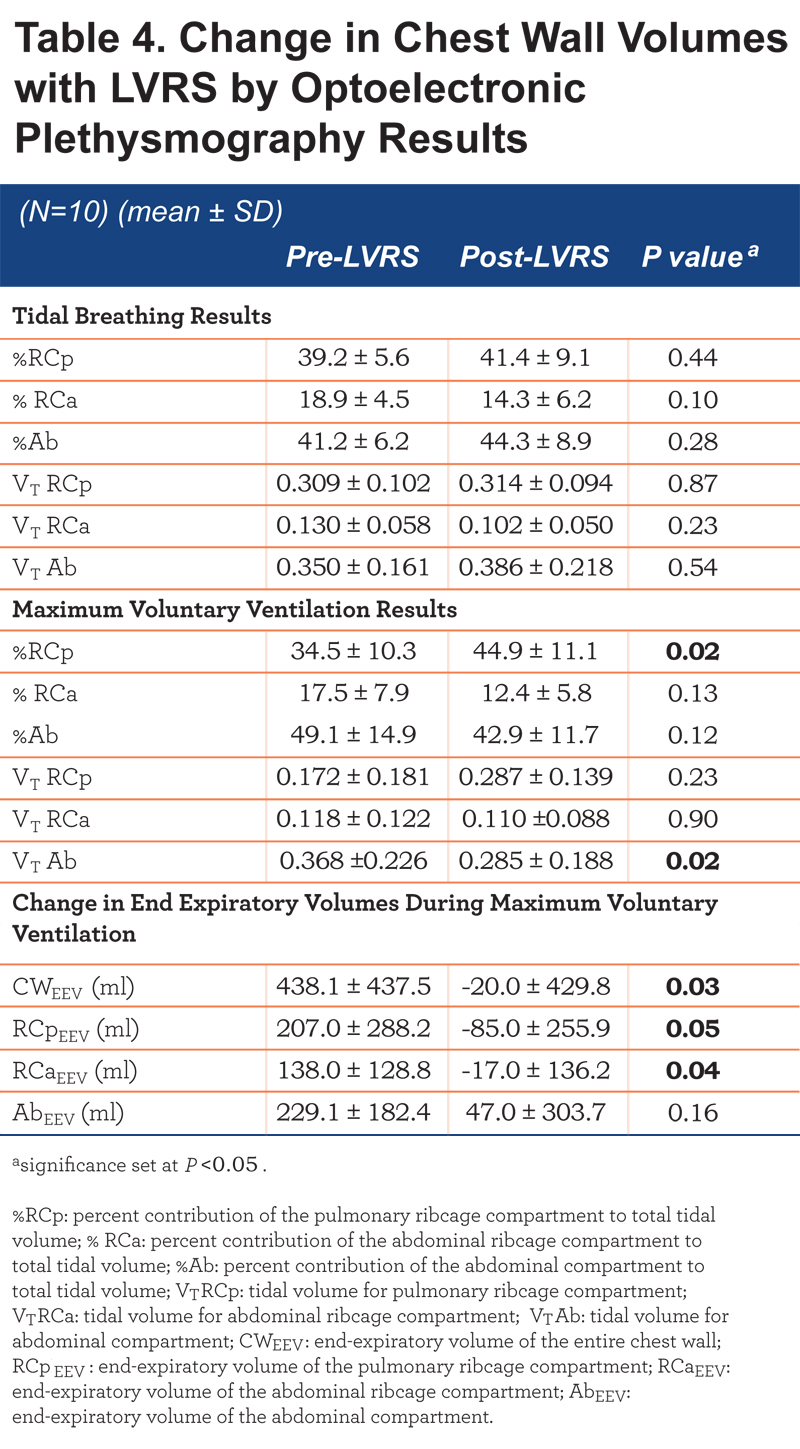
At rest, there were no significant changes in ventilatory mechanics after LVRS; however during the MVV there was a significant increase in the utilization of the RCp compartment and decrease in the tidal volume from the Ab compartment (Table 4). There was also a significant attenuation in dynamic hyperinflation with LVRS. Prior to LVRS, our patient population increased their chest wall and compartmental end expiratory volumes during the MVV maneuver. In contrast, post-LVRS, patients decreased end expiratory chest wall volume (CWEEV), RCp end expiratory volume (RCpEEV), and RCa end expiratory volume (RCaEEV) with the MVV maneuver. The change in end expiratory volume was significantly different between pre- and post-LVRS (Figure 2).
Post hoc analysis was performed to determine if any OEP parameters pre- LVRS were associated with improvements in clinically relevant outcome measures after LVRS. The only such statistically significant finding was a significant relationship between exercise-related O2 pulse (an estimate of stroke volume at peak exercise) and MVV RCpEEV such that increases in peak exercise O2 pulse post- LVRS correlated with a greater change in RCpEEV during the MVV (R2=0.41, Estimate =0.87, P-value 0.05). Additionally, pre to post-LVRS increases in FEV1 were significantly correlated with a pre to post-LVRS decrease in SGRQ dyspnea scores (R2=0.729, P=0.002).
Pre-LVRS, COPD patients demonstrated greater %Ab during MVV than controls (49.1 ± 14.9 versus 35.7 ± 10.8, P=0.031). Post-LVRS, COPD patients no longer demonstrated significant differences from controls in the utilization of the Ab compartment (42.9 ±11.7 versus 35.7 ± 10.8, P=0.204).
Discussion
Similar to previous work, following LVRS our patients demonstrated improvements in peak work load, FEV1, exercise airflow obstruction, peak exercise heart rate and heart rate reserve, and dyspnea. 1,15,16 However, to our knowledge, this is the first study to directly quantify changes in absolute and relative chest wall volumes both during tidal breathing and maximal voluntary ventilation pre- and post-LVRS, correlating these with improvements in static and dynamic ventilatory and exercise parameters as well as dyspnea scores. These novel data also confirm the inferences Tschernko et al15 made, via changes in inspiratory thoracic pressures, regarding a significant decrease in dynamic hyperinflation at rest following LVRS in patients with severe COPD.
Post-LVRS, patients demonstrate slower and deeper breathing patterns during exercise, leading to both improved alveolar ventilation and reduced work of breathing.15 Our data suggest that this improvement in ventilatory efficiency is mediated by increased contribution of the abdominal compartment during tidal breathing, and increased contribution of the pulmonary rib cage compartment (%RCp during MVV). It remains to be established whether such data apply to ventilatory mechanics and efficiency during exercise
Although no significant relationship between changes in OEP parameters and dyspnea were observed, there was a significant relationship between increased FEV1 post-LVRS and reduced dyspnea score. This relationship supports the physiological mechanism between airflow obstruction and dyspnea and perhaps why dyspnea is improved with LVRS.
The current results also demonstrate a potential relationship between decreased dynamic hyperinflation during MVV and increased O2 pulse (i.e, estimated peak exercise stroke volume). The relationship between decreased RCpEEV and O2 pulse supports the findings of Lammi et al 17 who demonstrated a relationship between reduced dynamic hyperinflation and improved O2 pulse. Work by Criner et al 18 similarly favored a potential relationship between hyperinflation and cardiac outcome measures by demonstrating evidence that reduced intrathoracic pressures with LVRS lead to reduced intracardiac pressure by echocardiogram. Both the current work and the work of Lammi and colleagues noted above 17 utilized supplemental oxygen during testing per NETT protocol. To our knowledge, estimating O2 pulse in the setting of high inspiratory oxygen has not yet been validated; therefore we cannot definitively determine if O2 pulse findings post-LVRS in the setting of supplemental oxygen use pertain to patients breathing room air.
A potential limitation of this study may be the power limitation of a small sample size. Although the study was adequately powered to determine changes in our main outcome measures; small data sets such as this one, can always be greatly influenced by the addition of a single individual. The sample size of this study represents the approximate number of LVRS cases performed at the center in a year; therefore, future work may want to consider a multicenter study design to investigate larger sample sizes of LVRS patients.
Conclusion
These data demonstrate the ventilatory mechanics effects of LVRS in patients with severe COPD: there was, most notably, an increased utilization of the RCp compartment and decreased dynamic hyperinflation during the MVV, which corresponded to the pattern of utilization of this compartment seen in non-COPD age and sex-matched controls. Based on the current findings, larger scale studies assessing the relationships among directly assessed ventilatory mechanics and functional capacity and dyspnea during tidal breathing and during environments of increased ventilatory demand pre-and post-LVRS appear imperative in the vulnerable, large population of patients living with severe COPD.
Acknowledgements
This research was supported in part by the VIDDA foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. This publication was in part supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1 TR000040. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Author Contributions: All authors have contributed to and approved the final draft of the manuscript; conception and design: AML, BMT , RCB, and MNB; experiment and data acquisition: AML, SLM and PAJ; data analysis and interpretation: AML, SLM, RCB, and HFA; drafting of manuscript, data analysis, and critical revision: AML, JG, AWS and RCB.
Declaration of Interest No author has any conflict of interest to report.