Running Head: Abstracts: COPD9-2014
Citation: Abstracts: COPD9-Birmingham, UK-June 2014. Chronic Obstr Pulm Dis. 2015; 2(2): 152-176. doi: http://doi.org/10.15326/jcopdf.2.2.2014.0158
Introduction
The 9th international, multidisciplinary meeting dedicated to COPD was held in Birmingham, United Kingdom in June 2014. The biennial meeting attracted a record number of delegates with 675 attending from 30 different countries, spanning a wide range of disciplines. Interestingly, there was an increase in the number of European delegates compared to previous events.
We are pleased that the conference series continues to attract attendance from key opinion leaders whilst also introducing emerging leaders from research, clinical practice and allied health care disciplines. Feedback received from individuals working in both commercial and health care settings supports the fact that it provides an ideal opportunity to meet and discuss ongoing work and exchange ideas.
All 5 of the Plenary Sessions of the conference included a period of discussion and debate facilitated by science writer and broadcaster Vivienne Parry. Themes included Future Challenges, Early COPD, COPD phenotypes, and Comorbidities – Common Pathophysiology and Management Challenges in COPD. There were 12 simultaneous sessions running over the established tracks of clinical science, basic science and care delivery. Speakers presented recent advances and current thinking regarding exacerbations, biomarkers, self-management and pathophysiology and there was an update session on alpha-1 antitrypsin deficiency which was last featured at COPD6 in 2008.
For the first time in the conference series, delegates experienced a presentation via Skype. Professor Alvar Agusti, MD, PhD, was unable to travel to the United Kingdom from Spain due to last minute air travel disruption, but he was determined to give his presentation on Biomarkers and Disease Activity, Severity and Impact and the session was a great success.
Insights from the Experts sessions were held each morning and were well attended and often oversubscribed. There were also dedicated sessions for allied health care professionals to network and discuss topics from the previous day.
The third Tim Griffiths Memorial Lecture was delivered by Dr Martijn Spruit, PhD, from The Netherlands on ‘Rehabilitation year in review’, a topic that Dr. Griffiths championed.
The conference saw 3 very deserving individuals inducted into the COPD Hall of Fame, namely Dr Suzanne Hurd, PhD, and Bartolome Celli, M.D, from the United States and Peter Barnes, DM, DSc, FRCP, from the United Kingdom. They have all made an outstanding contribution to the field of COPD and their work is summarized below.

Dr. Suzanne Hurd
Dr. Hurd was recognized for her organizational skills and exceptional contribution to the impact and work of the Global initiative for chronic Obstructive Lung Disese (GOLD) and Global Initiative for Asthma (GINA) strategies. She is the single most important person in the success of these internationally recognized documents.

Professor Bartolome Celli
Dr. Celli was recognized for his long and innovative contribution and leadership to the assessment, management and clinical impact of COPD. He is an inspirational speaker who challenges the status quo.

Professor Peter Barnes
Professor Barnes was recognized for his outstanding contribution to COPD research over decades. He remains the most published author in the field and has initiated many new ways of thinking about the disease. His enthusiasm for innovative thought and inspiring new thought in others remains unabated.
There was also an increase in the number of abstracts submitted for consideration at COPD9 and of these a total of 55 were presented in poster format. The accompanying 36 abstracts are those selected by the COPD9 Organizing Committee for publication.
The next meeting in the United States series will be COPD9usa in Chicago on June 5-6, 2015 and we are already making plans for COPD10, to be held in Birmingham from June 29 to July 1, 2016 where we hope to deliver the next update on progress and challenges of COPD.
From a personal point of view, and that of my co-organizer Sue Hill, we would like to thank our sponsors who provided non-commercial input to the educational program, our organizers Jackie Hutchinson and Executive Business Support and our conference manager Anita Pye.
Note: The following abstracts have not been edited but are presented here in their original format, as presented at COPD9.
The 24-Hour Lung Function Profile of Once-Daily Tiotropium (T) and Olodaterol (O) Fixed-Dose Combination (Fdc) Compared with Placebo and Monotherapies in Chronic Obstructive Pulmonary Disease
E. Derom,1 J. Westerman,2 L. Groenke,3 A. Hamilton,4 C. Li,5 K-M. Beeh,6
1Ghent University Hospital, Ghent, Belgium; 2Pulmonary and Sleep Associates of Jasper, Jasper, Alabama, USA; 3Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim, Germany; 4Boehringer Ingelheim, Burlington, Ontario, Canada; 5Boehringer Ingelheim Pharmaceuticals Inc., Ridgefield, Connecticut, USA; 6Insaf GmbH Institut für Atemwegsforschung, Wiesbaden, Germany
Rationale : This study investigated the 24-hour bronchodilator profile of once-daily FDCs of T and O, delivered via Respimat® Soft Mist™ inhaler in patients with moderate to very severe chronic obstructive pulmonary disease.
Methods : In a double-blind, Phase III, placebo-controlled incomplete crossover study, 219 patients were randomised to receive four treatments for 6 weeks: placebo, O 5 μg, T 2.5 μg, T 5 μg, T+O FDC 2.5/5 μg, T+O FDC 5/5 μg. Primary end point was forced expiratory volume in 1 second (FEV1) area under the curve from 0–24 hours (AUC0–24) after 6 weeks’ treatment.
Results: The 24-hour time profiles for both FDCs showed clear increases in FEV1 compared to placebo and monotherapies. For FEV1 AUC0–24, both FDCs were significantly superior to placebo (T+O FDC 5/5 μg: 0.280 L, p<0.0001; T+O 2.5/5 μg: 0.277 L, p<0.0001) and monotherapies (T+O 5/5 μg: 0.110–0.127 L, p<0.0001; T+O 2.5/5 μg: 0.107–0.124 L, p<0.0001).
Adverse-event incidence was similar between treatment arms.
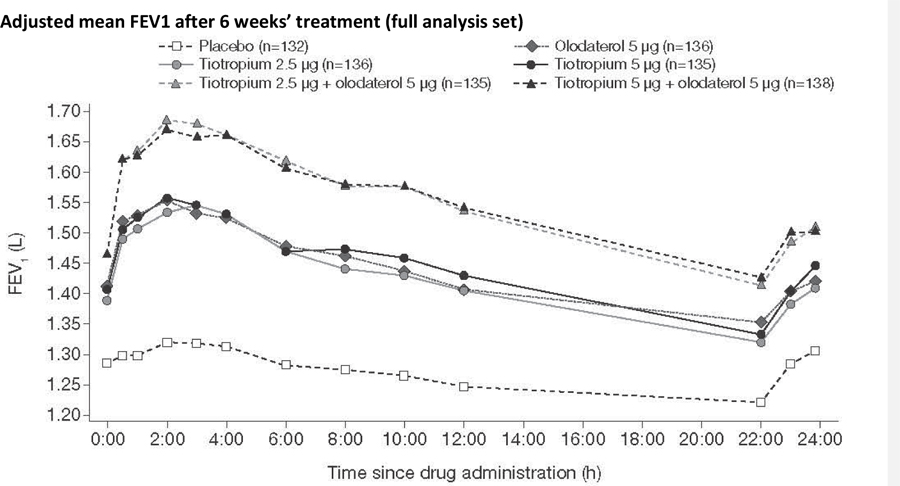
Conclusions: Both FDCs showed consistent increases in FEV1 AUC0–24 compared to placebo and monotherapies, with a similar tolerability profile to the well-established therapy T.
Funding : Boehringer Ingelheim.
48-week Administration of Olodaterol QD via Respimat® vs Placebo and Formoterol BID in patients with COPD: Pooled Safety Analysis
L. McGarvey,1 A. Koch,2 P. Sachs,3 A. Hamilton,4 K. Tetzlaff,5 L. Korducki,6 G.T. Ferguson,7
1Centre for Infection and Immunity, School of Medicine, Dentistry and Biomedical Sciences, The Queen’s University of Belfast, Belfast, UK;2 Medizinische Klinik III for Pneumology, Allergology and Sleep-Medicine, University Hospital Bochum- Bergmannsheil, Bochum, Germany;3 Pulmonary Associates of Stamford, Stamford, Connecticut, USA;4 Boehringer Ingelheim, Burlington, Ontario, Canada; 5 Boehringer Ingelheim Pharma GmbH & Co. KG, Biberach, Germany;6 Boehringer Ingelheim Pharmaceuticals Inc., Ridgefield, Connecticut, USA;7 Pulmonary Research Institute of Southeast Michigan, Livonia, Michigan, USA
Background: The novel LABA olodaterol (O) has an acceptable safety profile in clinical studies of ≤4 weeks.
Objective: To evaluate the long-term safety of olodaterol QD in patients with GOLD 2-4 COPD.
Methods: 4 randomised, double-blind, placebo-controlled, parallel-group studies (1: NCT00782210; 2: NCT00782509; A: NCT00793624; B: NCT00796653) investigated olodaterol (5 or 10 μg) QD via Respimat®, formoterol (F; 12 μg) BID via Aerolizer® (A and B) or placebo (P) for 48 weeks. Patients continued to receive usual care COPD maintenance therapy including SAMA, LAMA, ICS and xanthines. An independent Mortality Adjudication Committee (MAC) evaluated fatalities before trial unblinding. Safety data from the pooled dataset are presented.
Results: 3104 patients were included.
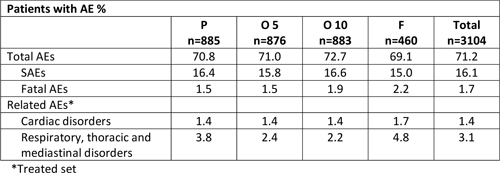
No significant safety signals were identified. AEs, SAEs and deaths were balanced across groups, including treatment-related respiratory and cardiac disorders (particularly relevant to β-agonists). Based on MedDRA classification, there was 83% concordance between MAC and site investigator (SI) at System Organ Class (SOC) level although concordance was lower (70%) at Preferred Term level. There was a shift to ‘cardiac’ SOC in 8 cases (15%) based on the SI determination.
Conclusions: The safety profile for olodaterol 5 and 10 μg QD was satisfactory and comparable to formoterol BID and placebo.
Glycopyrronium is Safe and Well Tolerated in Patients with Moderate-to-Severe COPD Compared to Placebo and Tiotropium.
E.M. Kerwin,1 A. D'Urzo,2 T. Overend,3 P. Goyal,4 M. Gavornikova,4 H. Chen,5 D. Banerji,5
1 Clinical Research Institute of Southern Oregon, PC, Medford, OR, USA; 2 Department of Family and Community Medicine, University of Toronto, ON, Canada; 3 Novartis Horsham Research Centre, Horsham, UK;4 Novartis Pharma AG, Basel, Switzerland;5 Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA
Introduction: Glycopyrronium is a once-daily inhaled LAMA for maintenance treatment of COPD. We present the safety profile of glycopyrronium in phase II and III clinical studies.
Methods: Glycopyrronium safety database comprised of pooled safety populations (2436 patients) from phase II (A2205, A2207 and A2208) and III (GLOW 1 to 3) studies including glycopyrronium 50µg via the Breezhaler,® device, placebo, and open- label tiotropium 18µg via the HandiHaler,® device over 26 to 52 weeks.
Results: Overall incidence of adverse events (AEs) with glycopyrronium (58.2%) and placebo (54.4%) was lower than tiotropium (74.2%). Discontinuations due to AEs were lower with glycopyrronium (5.9%) versus placebo (7.1%) and tiotropium (7.5%). Dry mouth occurred in <2% of all patients; urinary tract infections occurred in <2% of patients on glycopyrronium versus 6.0% on tiotropium. Frequency of SAEs was similar with glycopyrronium (8.2%) and placebo (8.6%) versus higher with tiotropium (15.0%). Major adverse cardiovascular events was similar with glycopyrronium (0.4%) and placebo (0.3%), and higher (1.1%) with tiotropium. 14 deaths (mostly respiratory/cardiovascular) were reported (glycopyrronium-7; placebo-5 and tiotropium-2), none were considered to be related to study medication by investigator.
Conclusion: In patients with moderate-to-severe COPD, glycopyrronium is well tolerated with a safety profile similar to placebo and tiotropium.
Efficacy and Safety of Once-Daily Glycopyrronium in Predominantly Chinese Patients with Moderate-To-Severe Chronic Obstructive Pulmonary Disease: The Glow7 Study
C. Wang,1 T. Sun,1 Y. Huang,2 M. Humphries,3 L. Bai,3 L. Li,3 Q. Wang,3 P. Kho,4 R. Firth,4 M. Gavornrikova,5 P. D’Andrea,6
1 Beijing Hospital, Dongcheng District, Beijing, China; 2 Hainan Provincial People's Hospital, Xiuying District, Haikou, China; 3 Beijing Novartis Pharma Co. Ltd., Boyun Road, Zhangjiang Hi-Tech Park, Shanghai, China;4 Novartis Horsham Research Centre, Horsham, West Sussex, UK;5 Novartis Pharma AG, Basel, Switzerland;6 Novartis Pharmaceuticals Corporation, East Hanover, New Jersey, USA
Introduction: The GLOW7 study evaluated the efficacy and safety of once-daily glycopyrronium 50µg versus placebo in predominantly Chinese patients with moderate-to-severe COPD.
Methods: In this 26-week, multicentre, double-blind, placebo-controlled study, patients ≥40 years with moderate-to-severe COPD were randomised to glycopyrronium or placebo (2:1). Primary endpoint was trough FEV1 at Week12. Secondary endpoints included peak FEV1, FEV1AUC5min-4h, TDI, SGRQ, and COPD exacerbations at Week26. Safety and tolerability were also evaluated.
Results: Of 460 patients randomised, 92.4% completed the study. At Week12, glycopyrronium significantly improved trough FEV1 compared with placebo (least square mean treatment difference [LSMTD]: 141mL (95% CI: 0.111, 0.171;p<0.001). At Week26, glycopyrronium significantly (p<0.001) improved peak FEV1 (LSMTD: 196mL), FEV1AUC5min-4h (LSMTD: 197mL), TDI (LSMTD: 1.0) and SGRQ (LSMTD: –4.92) compared with placebo. Glycopyrronium reduced the risk of exacerbations in terms of time to first (28%;p=0.153) and rate (29%;p=0.119) of moderate or severe COPD exacerbation versus placebo. Incidence of death was 1.3% (4 patients) with glycopyrronium and 0% in placebo. Overall incidence of adverse events (glycopyrronium 43.6%; placebo 47.4%) and serious adverse events (glycopyrronium 5.6%; placebo 9.1%) were similar.
Conclusion: In predominantly Chinese patients, once-daily glycopyrronium significantly improved lung function, dyspnoea and health status versus placebo with a comparable safety profile.
QVA149 Improves Dyspnoea, Health Status, and Lung Function Vs. Tiotropium and Salmeterol/Fluticasone Combination in Patients with COPD and Moderate-To-Severe Baseline Dyspnoea: The Ignite Trials
A. D'Urzo,1 D.A. Mahler,2 D. Keininger,3 K. Mezzi,3 R. Fogel,4 D. Banerji,3
1 Department of Family and Community Medicine, Faculty of Medicine, University of Toronto, Toronto, ON, Canada;2 Geisel School of Medicine at Dartmouth, Hanover, NH, USA;3 Novartis Pharma AG, Basel, Switzerland;4 Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA
Introduction: QVA149 is an approved once-daily dual bronchodilator fixed-dose combination of indacaterol and glycopyrronium, for maintenance treatment of patients with symptomatic COPD. We assessed efficacy of QVA149 in improving dyspnoea, lung function and health status in a subgroup of patients with moderate-severe baseline dyspnoea from the SHINE and ILLUMINATE studies.
Methods: This subgroup population included patients with a baseline dyspnoea index (BDI) ≤7 (moderate-to-severe dyspnoea, GOLD Groups B/D) from SHINE [(N=2144); placebo, open-label (OL) tiotropium or QVA149]; and ILLUMINATE [(N=523); salmeterol/fluticasone combination (SFC) or QVA149]. TDI, SGRQ, FEV1 were assessed at 26 weeks.
Results: The mean BDI was similar in SHINE [tiotropium (n=313): 5.57, QVA149 (n=305): 5.44, placebo (n=131): 5.47] and ILLUMINATE (QVA149 [(n=166): 5.78, SFC (n=179): 5.85]. QVA149 provided improvements in all endpoints compared to placebo, OL- tiotropium and SFC (Table).

Conclusion: In patients with moderate-to-severe baseline dyspnoea (comparable to patients in GOLD Groups B & D), QVA149 was more effective in improving dyspnoea, health status, and lung function vs. OL-tiotropium and SFC.
Once-Daily QVA149 Demonstrates Superior Improvement in Dyspnoea and Lung Function Compared with Tiotropium in Symptomatic Patients Using LABA/ICS Prior to Study Enrollment: The Blaze Study
A. D’Urzo,1 D.A. Mahler,2 K. Mezzi,3 H. Chen,4 R. Fogel,4 D. Banerji,4
1 Department of Family and Community Medicine, Faculty of Medicine, University of Toronto, Toronto, ON, Canada;2 Section of Pulmonary & Critical Care Medicine; Geisel School of Medicine at Dartmouth; Hanover, NH, USA;3 Novartis Pharma AG, Basel, Switzerland;4 Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA
Introduction: In the BLAZE study, QVA149 significantly improved dyspnoea (assessed by self-administered computerised [SAC]-TDI) and lung function versus placebo and tiotropium.,1 This post-hoc analysis evaluates these outcomes from the subgroup population who were on prior LABA/ICS therapy at study entry.
Method: This 6-week blinded, crossover study randomised moderate-to-severe COPD patients (mMRC≥2) to once-daily QVA149 110/50μg, placebo or tiotropium 18μg.,1
Results: Of the 247 patients randomised, 82 were on prior LABA/ICS therapy. At Week 6, QVA149 improved the SAC-TDI score (≥1unit) in a higher proportion of patients (39.5%) than placebo (19.0%; odds ratio [OR] 3.16) and tiotropium (20.0%; OR 3.31; both p<0.01). QVA149 significantly improved mean FEV1 at all the timepoints versus placebo and tiotropium (p<0.05). Similarly, significant improvement (p<0.001) was seen with QVA149 in FEV1AUC0-4h versus placebo (least squares mean treatment difference [LSMTD] 293mL) and tiotropium (LSMTD 102mL) respectively. QVA149 reduced mean rescue medication use by 1.53 puffs/day (p<0.001) versus placebo and 0.44 puffs/day (p=0.128) versus tiotropium.
Conclusion: Significant improvements in dyspnoea and lung function were seen with QVA149 versus tiotropium and placebo in the subgroup population using LABA/ICS preceding study enrolment.
Reference: Mahler DA. et al. Eur Respir J 2013.
Once-Daily QVA149 Improves Dyspnoea, Lung Function and Reduces Rescue Medication Use in Symptomatic Patients with COPD Using LAMA as Prior Medication: The Blaze Study
A. D’Urzo,1 D.A. Mahler,2 K. Mezzi,3 H. Chen,4 R. Fogel,4 D. Banerji,4
1 Department of Family and Community Medicine, Faculty of Medicine, University of Toronto, Toronto, ON, Canada;2 Section of Pulmonary & Critical Care Medicine; Geisel School of Medicine at Dartmouth; Hanover, NH, USA;3 Novartis Pharma AG, Basel, Switzerland;4 Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA
Introduction: QVA149, an approved dual-bronchodilator, has been shown to improve self-administered computerised (SAC)-TDI total score and lung function versus placebo and tiotropium in moderate-to-severe COPD patients in the BLAZE study,1. This post-hoc analysis explores the effect of QVA149 on dyspnoea, lung function, and rescue medication use in the subgroup of patients on prior LAMA therapy.
Methods: The BLAZE study (blinded, double-dummy, crossover) treated patients (mMRC≥2) with QVA149 110/50µg, placebo and tiotropium 18µg in random order.
Results: Of the 247 patients randomised, 115 were on prior LAMA therapy. QVA149 improved SAC-TDI total score (≥1unit) in a higher proportion of patients (36.5%) versus placebo (16.4%; odds ratio [OR] 3.71; p<0.001) and tiotropium (20.2%; OR 2.51; p=0.007). QVA149 significantly improved (p<0.001) mean FEV1 at all time-points, and FEV1AUC0–4h with a least squares mean treatment difference of 205 and 305mL versus placebo; 63 and 111mL versus tiotropium, at Day1 and Week6, respectively. QVA149 significantly reduced (p<0.01) mean rescue medication use by 1.55puffs/day versus placebo and 0.68puffs/day versus tiotropium.
Conclusion: In the subgroup of patients on prior LAMA therapy, QVA149 statistically significantly improved dyspnoea and lung function while reducing rescue medication usage versus placebo and tiotropium.
Reference: Mahler DA. et al. Eur.Respir.J 2013.
A Significant Proportion of Patients with COPD Show Marked Improvements in Lung Function with QVA149 (High Responders): A Post-Hoc Analysis of the Shine Study
K.R. Chapman,1 E.D. Bateman,2 P. Olsson,3 H. Chen,4 D. Banerji,4 R. Fogel,4
1 Asthma & Airway Centre, University Health Network, Toronto Western Hospital, Toronto, Canada;2 University of Cape Town, Cape Town, South Africa;3 Novartis Pharma AG, Basel, Switzerland;4 Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA
Rationale: QVA149 is an approved once-daily dual bronchodilator combination of the LABA indacaterol and LAMA glycopyrronium recommended for the maintenance treatment of COPD (GOLD 2014 patients group B-D). This post-hoc analysis from the SHINE study reports results from the subgroup of patients who had major improvement in lung function (high-responders) on different treatment regimes.
Methods: This 26-week, double-blind, placebo- and active-controlled study randomised (2:2:2:2:1) patients ≥40 years with moderate-to-severe COPD and smoking history ≥10 pack-years to QVA149-110/50μg, indacaterol-150μg, glycopyrronium-50μg, open-label tiotropium-18μg or placebo. The proportion of patients with superior bronchodilation (trough FEV1 [tFEV1] >200, 300 and 400mL) was evaluated.
Results: Of the 2,144 patients randomised, 89.1% completed the study. A percentage of patients in each treatment group showed an increase from baseline in tFEV1 of >200, 300 and 400mL at week 26 (table).
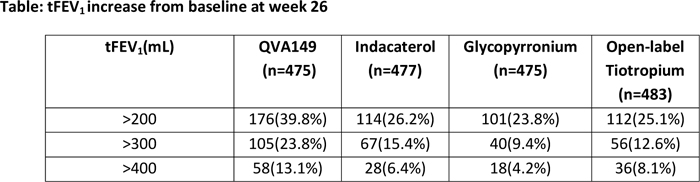
Conclusion: In this analysis, a significantly higher proportion of patients in QVA149 showed very large changes from baseline in trough FEV1 (high-responders) compared with its monocomponents and open-label tiotropium at week 26.
Cardio- and Cerebrovascular (CCV) Safety of QVA149 in Patients with Moderate-To-Severe COPD: A Pooled Analysis
R.Dahl,1 R. Buhl,2 P. Olsson,3 A. Schubert-Tennigkeit,3 H. Chen,4 D. Banerji,4 R. Fogel,4
1 Department of Dermatology, Allergy Centre, Odense University Hospital, Odense, Denmark;2 Pulmonary Department, Mainz University Hospital, Mainz, Germany;3 Novartis Pharma AG, Basel, Switzerland;4 Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA.
Introduction: QVA149 is an approved once-daily dual bronchodilator combining indacaterol and glycopyrronium for the maintenance treatment of patients with COPD. Since COPD patients commonly suffer cardio- and cerebrovascular co-morbidities, we evaluated the cardiac safety of QVA149 versus indacaterol, glycopyrronium, tiotropium, salmeterol/fluticasone (SFC) and placebo based on the IGNITE pivotal registration program.
Methods: Safety data was pooled from five clinical studies (ARISE, SHINE, SPARK, ENLIGHTEN and ILLUMINATE) with a duration of ≥6 months. All CCV adverse events (AEs) and serious AEs (SAEs: major adverse cardiac events [MACE] and Non-MACE) were analysed.
Results: Frequencies of CCV events in patients with COPD who received QVA149 (n=1805; CCV-AEs, 3.9%; CCV-SAEs, 1.8%) was similar compared with placebo (n=345; CCV-AEs, 2.6%; CCV-SAEs, 0.3%), indacaterol (n=476; CCV-AEs, 2.5%; CCV-SAEs, 0.8%), glycopyrronium (n=1213; CCV-AEs, 5.3%; CCV-SAEs, 2.5%), open-label tiotropium (n=1256; CCV-AEs, 4.7%; CCV-SAEs, 2.2%) and SFC (n=264; CCV-AEs, 2.3%; CCV-SAEs, 1.1%). QVA149 also showed consistently lower or similar frequencies of respiratory infections and other respiratory AEs compared to placebo and active comparators.
Conclusion: Overall the CCV safety profile of QVA149 is similar to its mono-components, other standard COPD treatments and placebo, providing reassurance for safe use as a regular long-term treatment in patients with moderate-to-very severe COPD.
Once-Daily QVA149 Showed Significant Improvements in Lung Function and Health Status and Was Well Tolerated Versus Glycopyrronium and Open-Label Tiotropium in a Subgroup of Patients with Severe COPD: The Spark Study
J.A. Wedzicha,1, A. D’Urzo,2 K. Mezzi,3 H. Chen,4 D. Banerji,4 R. Fogel,4,
1 Airway Disease Section, National Heart and Lung Institute, Imperial College London, London, UK;2 Department of Family and Community Medicine, Faculty of Medicine, University of Toronto, Toronto, ON, Canada;3 Novartis Pharma AG, Basel, Switzerland ; 4 Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA
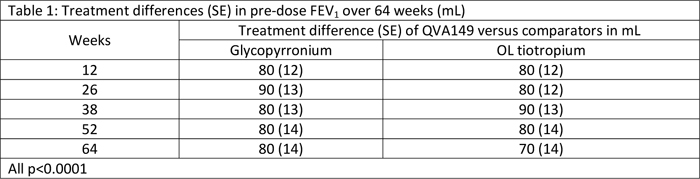
Introduction: QVA149 is an approved once-daily dual bronchodilator combining indacaterol and glycopyrronium for the maintenance treatment of patients with symptomatic COPD. This subgroup analysis evaluated the efficacy and safety of QVA149 versus glycopyrronium and tiotropium in patients with severe COPD from the SPARK study.
Methods: SPARK (64-week, multicentre, double-blind, parallel-group, active-controlled) randomised (1:1:1) severe to very-severe patients with COPD to once-daily QVA149 110/50µg, glycopyrronium 50µg, or open-label (OL) tiotropium 18µg. Efficacy parameters included pre-dose FEV1 and health status (SGRQ). Safety data was also recorded.
Results: Of the 2224 randomised patients, 1742 (78.3%) had severe COPD (GOLD 2008) [QVA149=578; glycopyrronium=583; OL tiotropium=581]. Pre-dose FEV1 was significantly higher with QVA149 at all time-points compared with glycopyrronium and tiotropium in patients with severe COPD (p<0.0001 for both, Table 1). At Week 64, SGRQ total score was significantly lower in the QVA149 group than glycopyrronium (treatment difference [TD]: -2.56; p=0.002) or tiotropium (TD: -3.38; p<0.001) groups. The incidence of adverse events were similar across all groups (QVA149=92.9%; glycopyrronium=93.0%; tiotropium=94.1%).
Conclusion: In patients with severe COPD, QVA149 resulted in significant improvements in lung function and health status compared with glycopyrronium and tiotropium with a safety profile similar to that of both glycopyrronium and tiotropium.
Once-Daily QVA149 Reduces Moderate-To-Severe Exacerbations Compared with Open-Label Tiotropium in Patients with Severe COPD: Results from the Spark Study
J.A. Wedzicha,1 M. Decramer,2 P. Olsson,3 H. Chen,4 R. Fogel,4 D. Banerji,4
1 Airway Disease Section, National Heart and Lung Institute, Imperial College London, London, UK;2 Respiratory Division, University of Leuven, Leuven, Belgium;3 Novartis Pharma AG, Basel, Switzerland;4 Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA.
Introduction: QVA149 is an approved once-daily (OD) dual bronchodilator combination of the LABA, indacaterol, and the LAMA, glycopyrronium, for the maintenance treatment of patients with symptomatic COPD. This post-hoc analysis reports the rate ratio (RR) of exacerbations in patients with severe COPD from the SPARK study.,1
Methods: SPARK was a 64-week, multicentre, double-blind, parallel-group, active-controlled (open-label [OL] tiotropium and glycopyrronium) study that randomised patients with severe-to-very severe COPD (post-bronchodilator FEV1/FVC<0.7 and FEV1 <50% predicted) and history of ≥1 exacerbation in previous year to receive OD QVA149 110/50μg, glycopyrronium 50μg or OL-tiotropium 18μg.
Results: Of the 2224 patients randomised, 1744 had severe COPD (QVA149=579; glycopyrronium =584; tiotropium=581). QVA149 reduced the risk of moderate-to-severe exacerbations versus glycopyrronium by 11% (RR 0.89; 95% CI 0.77, 1.04) and tiotropium by 15% (RR 0.85; 95% CI 0.73, 0.98). In a majority of subgroups, QVA149 compared with tiotropium, reduced the risk of moderate-to-severe exacerbations QVA149 showed similar reduction in risk of moderate-to-severe exacerbations compared with glycopyrronium in most of the subgroups.
Conclusions: Risk of moderate-to-severe exacerbation was reduced in patients with severe COPD who were treated with QVA149 compared with glycopyrronium and tiotropium.
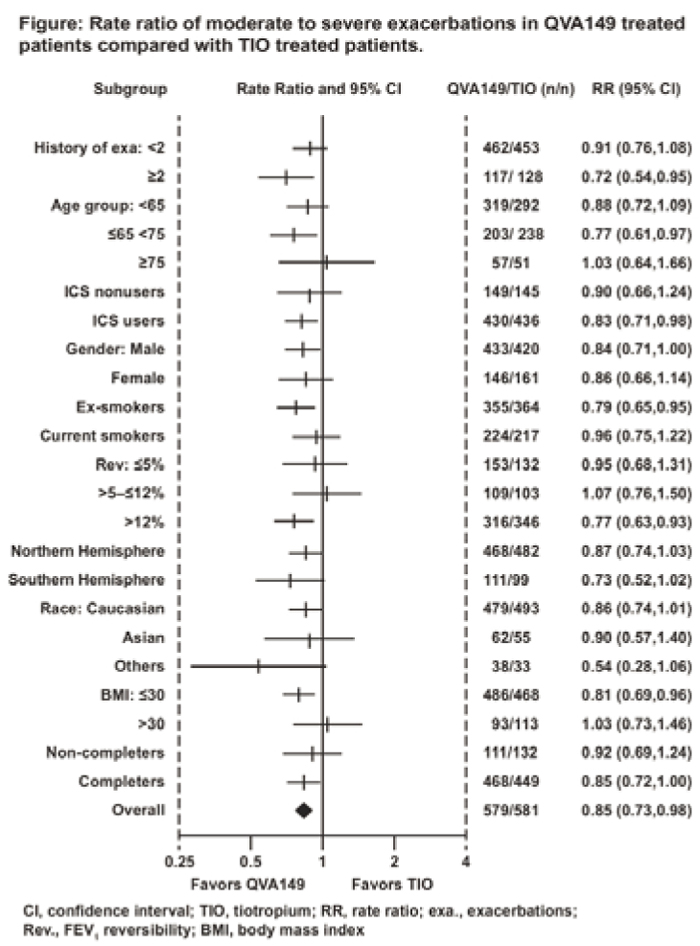
Reference: Wedzicha J A.et al. Lancet Respir Med 2013;1: 199–209.
Once-Daily Glycopyrronium Improves Lung Function and Health Status, and Reduces Exacerbations In Patients With Severe-To-Very Severe COPD: Analysis from the Spark Study
J.A. Wedzicha, 1 M. Decramer, 2 J.H. Ficker, 3 A. Fowler Taylor, 4 P. D'Andrea, 4 C. Arrasate,4 H. Chen, 4 D. Banerji, 4
1 Airway Disease Section, National Heart and Lung Institute, Imperial College London, London, UK;2 Respiratory Division, University Hospitals, Leuven, Belgium;3 Department of Respiratory Medicine, Allergology, and Sleep Medicine, Klinikum Nuernberg, Nuernberg, Germany;4 Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA
Introduction: Glycopyrronium and tiotropium are once-daily inhaled LAMAs for the treatment of COPD. Here we present the efficacy results of glycopyrronium versus tiotropium in patients with severe-to-very severe COPD from the SPARK study.
Methods: This 64-week, multicentre, double-blind, parallel-group, active-controlled study randomised patients ≥40 years with severe-to-very severe COPD and a history of exacerbations to receive QVA149-110/50μg, glycopyrronium-50μg or open-label tiotropium- 18μg. COPD exacerbations, lung function (pre-dose FEV1), health status (SGRQ) and rescue medication use were analysed.
Results: Of the 1483 patients randomised, 99.5% were analysed (glycopyrronium=739, tiotropium=737). At Week 64, the reduction in the rate of COPD exacerbations with glycopyrronium was comparable to tiotropium (Rate ratio: 1.01, 95% confidence interval [CI]: 0.913, 1.107; p=0.919). Glycopyrronium showed similar improvement in pre-dose FEV1 (LSM treatment difference [Td] of –0.02L; CI: –0.04, 0.01L; p=0.179) and SGRQ scores (Td = –0.62; CI: –2.12, 0.89L; p=0.421) as compared to tiotropium at Week 64. The reduction in daily rescue medication usage was similar for glycopyrronium (Td = 0.05 puffs/day; CI: –0.20, 0.31; p=0.676) as compared to tiotropium.
Conclusion: Once-daily glycopyrronium showed similar efficacy in improving lung function and health status, and reducing exacerbations and rescue medication use as tiotropium in patients with severe-to-very severe COPD.
Glycopyrronium is Safe and Well Tolerated in Patients with Severe-To-Very Severe COPD: Analysis from the Spark Study
M. Decramer,1 J.A. Wedzicha,2 J.H. Ficker,3 A. Fowler Taylor,4 P. D'Andrea, 4 C. Arrasate,4 H. Chen,4 D. Banerji,4
1 Respiratory Division, University Hospitals, Leuven, Belgium;2 Airway Disease Section, National Heart and Lung Institute, Imperial College London, London, UK;3 Department of Respiratory Medicine, Allergology, and Sleep Medicine, Klinikum Nuernberg, Nuernberg, Germany;4 Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA.
Introduction: Glycopyrronium is a once-daily inhaled LAMA approved in the EU for treatment of patients with COPD. It exhibits rapid onset of action along with sustained bronchodilation. Here, we compare the safety profile of glycopyrronium with tiotropium in patients with severe-to-very severe COPD from the SPARK study.
Methods: This study randomised patients ≥40 years with severe-to-very severe COPD and a history of exacerbations to receive double-blind QVA149 110/50μg, glycopyrronium 50μg or open-label (OL) tiotropium 18μg. Safety was assessed by recording adverse events (AEs) and serious AEs (SAEs).
Results: The overall safety profile was similar for glycopyrronium and OL-tiotropium.
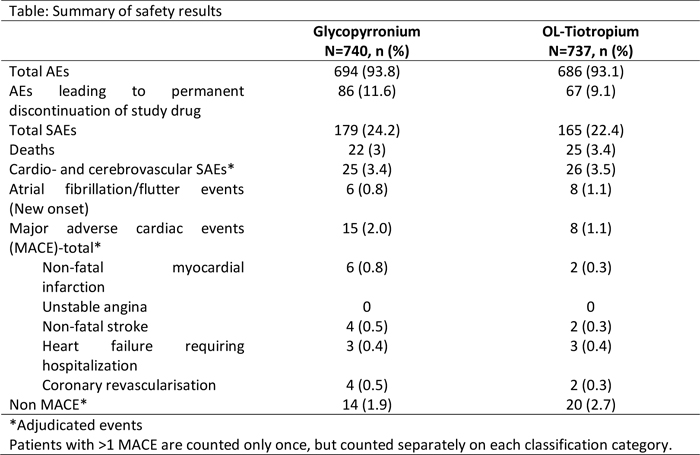
Conclusion: In this analysis from the SPARK study, glycopyrronium showed an overall good safety profile in patients with severe-to-very severe COPD that was similar to tiotropium.
The Effect of CXCR1 and CXCR2 Inhibition on Neutrophilic Migration in COPD
J.A. Stockley,1 R.A.Stockley,1 and E. Sapey,2.
1 Lung Function & Sleep Department, Queen Elizabeth Hospital Birmingham, UK,2 School of Clinical and Experimental Medicine, University of Birmingham, UK.
Rationale: We have previously shown that neutrophils from COPD patients migrate with increased speed (chemokinesis) but reduced accuracy (chemotaxis) compared to those from healthy donors (Sapey et al. AJRCCM 2011; 183:1176-86). Evidence suggests that CXCR2 blockade is associated with a reduction in neutrophil airway recruitment (Leaker et al. Respir Res 2013; 14:137), which may be of therapeutic benefit. However, the precise effects on neutrophilic migratory dynamics of CXCR1 or CXCR2 inhibition are currently unclear.
Methods: Neutrophilic migration was assessed using a modified Insall chamber in RPMI (control medium) and gradients of IL-8, GROα and sputum sol phase (Sol) with a CXCR1 inhibitor, CXCR2 inhibitor, a dual inhibitor (SCH527123) or vehicle controls. SCH527123 was used at two concentrations; 42nM (more specific to CXCR1) and 3nM (more specific to CXCR2).
Results: CXCR1 inhibition caused a reduction in chemokinesis to IL-8 (p<0.0001), GROα (p=0.029) and Sol (p<0.001) but did not influence chemotaxis. CXCR2 inhibition also significantly attenuated chemokinesis to IL-8 and GROα (p<0.0001) but the effect was less pronounced in Sol (p=0.052). CXCR2 inhibition also resulted in significantly reduced chemotaxis in all chemotactic gradients (p<0.01). SCH527123 significantly reduced chemokinesis to IL-8 and GROα (p<0.0001) but only at 3nM to Sol (p<0.01). The only effect of SCH527123 on chemotaxis was a significant reduction at 3nM to GROα (p<0.01).
Conclusions: The dominant effect of CXCR1 and CXCR2 blockade on neutrophilic migration in COPD appears to be a reduction in the general speed of migration. However, as chemotaxis was not improved, it is unclear if CXCR1/2 inhibition would be beneficial or detrimental to COPD, as slower transmigration could potentially increase tissue exposure to and hence damage by proteolytic enzymes.
Does Serum Ccl-18 Level Discriminate the Frequent Exacerbator Type of COPD ?
A. Görek Dilektaşlı,1 E. Demirdogen Cetinoglu,1 E. Uzaslan,1 F. Budak,2 F. Coşkun,1 A. Ursavaş,1 E. Ege,1
1 Uludag University Faculty of Medicine, Department of Pulmonary Disesaes, Bursa, Turkey,2 Uludag University Faculty of Medicine, Department of Immunology, Bursa, Turkey
Introduction: Pulmonary and activation-regulated chemokine/CC-chemokine ligand-18(CCL-18) is mainly expressed in lungs. We aimed to study if serum CCL-18 level differentiates the frequent exacerbator COPD phenotype from the infrequent exacerbators.
Material-Methods: Clinically stable COPD patients and healthy controls (HC) were enrolled. Severity of dyspnea and symptoms were assessed by the modified Medical Research Council (mMRC) Dyspnea Scale, and COPD Assessment Test (CAT).Spirometry and six-minute walking test (6MWT) were performed. Serum CCL-18 levels were measured with a commercial ELISA Kit.
Results: Sixty COPD patients and 29 HCs were recruited. COPD patients were grouped as frequent exacerbators(FE-COPD,n=33) and infrequent exacerbators(IE-COPD,n=27) based on exacerbation frequency (≥2/year vs.<2/year).CCL18 levels were elevated in COPD patients when compared with the HCs (p=0.0001).CCL18 values did not differ significantly among IE-COPD and FE-COPD groups, though there was an increasing trend between these groups (p=0.09).The number of COPD exacerbations were associated with the serum CCL-18 levels. Elevated serum CCL-18 level correlated with mMRC and CAT scores. Decreased exercise capacity as measured by 6MWD was inversely related with serum CCL-18 levels.
Conclusion: CCL-18 could be a useful biomarker in COPD, since it is associated with frequency of exacerbations in addition to functional parameters and symptom scores.Further studies are needed to explore these results.
Is High C-Reactive Protein a Risk Factor for High In-Hospital Mortality in Chronic Obstructive Pulmonary Disease Patients wıth Exacerbatıon ?
A. Görek Dilektaşlı, E. Uzaslan, E. Demirdöğen Çetinoğlu, D. Ediger, E. Ege
Uludag University School of Medicine, Department of Pulmonary Diseases, Bursa, Turkey
Background: C-reactive protein (CRP) was shown to be related with important clinical outcomes, including exercise tolerance, health status and the exacerbations in chronic obstructive pulmonary disease (COPD) patients. We aimed to evaluate if the serum CRP level on admission is associated with in-hospital mortality outcome in acute exacerbation of COPD (AECOPD) patients requiring hospitalization. We also sought to determine the affecting factors on in-hospital mortality in these patients.
Methods: We included COPD patients retrospectively whom admitted to a tertiary reference center and hospitalized with acute exacerbation in the last three years.
Results: We identified a total of 393 patients hospitalized for AECOPD.Of these 84.2% were males. The mean age of the group was 66.7±10.9 years old. 51 patients lost follow-up and 11.1% (n=38) of the patients died. The median length of stay for hospitalization was longer in the lost patients (p<0.05). C-reactive protein levels on admission were significantly higher in patients who died than the alive ones (p<0.05). The sensitivity, specificity of a CRP level > 3.14 mg/dL was calculated as 70% (95% CI: 50.5-85.2) and 61.6 % (95% CI: 55.5-67.4) using receiver-operating characteristic analysis.
Conclusion: Mortality of AECOPD is high. High CRP levels during AECOPD episode might correlate with short-term prognosis.
Serum Polyclonal Free Light Chains: A Potential Biomarker for Immune Activation in Alpha-1 Antitrypsin Deficiency (A1ATD) Related and Usual COPD
J. Brebner,1,2 A. Turner,1,2 R. Stockley,1,2
1 School of Clinical and Experimental Medicine, University of Birmingham, Birmingham, UK,2 ADAPT project, University Hospital Birmingham, Birmingham, UK
Background: Immunoglobulin free light chains (FLCs) are produced as a by-product of antibody synthesis and have recently been implicated in the pathogenesis of COPD.
Aims: To investigate the utility of serum FLCs as a marker of adaptive immune system activation, phenotypic variation and disease severity in patients with COPD.
Method: We measured FLC levels in 547 patients with severe A1ATD and 82 patients with usual COPD using the Freelite® serum FLC assay. We compared combined (κ & λ) FLC levels (cFLC) in different subgroups and performed a cross sectional analysis to look for correlations with lung function parameters.
Results: In both groups, patients with chronic bronchitis had significantly higher cFLC levels compared to those without. A1ATD patients who had subsequently died also had higher cFLC levels (Table 1). In the A1ATD group, there were no correlations between cFLC and lung function parameters. However in the usual COPD cohort there was a significant negative correlation between cFLC level and gas transfer (rs= -0.38 p = 0.004).
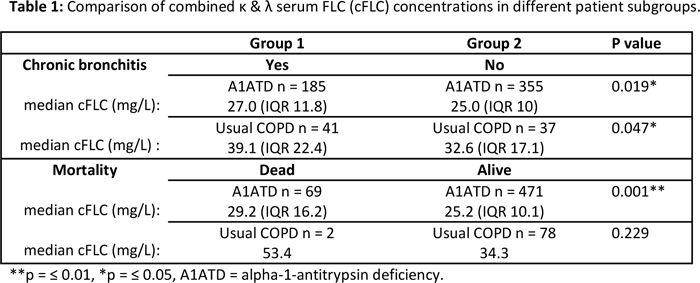
Conclusions: COPD patients with chronic bronchitis may have a greater adaptive immune response compared to those without. Further evaluation is needed to establish if FLCs could serve as a useful clinical biomarker for phenotyping or risk-stratification in COPD.
Rate of Decline in Lung Density May Predict Long-Term Outcome in Patients with Alpha 1 Antitrypsin Deficiency (AATD)
C.E. Green,1 D. Parr,2 A.S. Zbrozek,3 R.A. Stockley,1 A.M. Turner,1
1 Centre for Translational Inflammation Research, University of Birmingham, Birmingham, B152WB, UK,2 University Hospital Coventry and Warwickshire, Clifford Bridge Road, Coventry, West Midlands CV2 2DX,3 CSL Behring, 1020 1st Ave, King of Prussia, PA 19406, United States
Lung function and CT densitometry predict mortality in augmentation naïve AATD patients.(1) We hypothesised decline in CT densitometry would relate to survival/transplantation in these patients.
Methods: UK AATD registry augmentation naïve patients with 2 quantitative CT scans (PD15) were selected. Subsequent death or lung transplant was noted. Patients were divided into 3 categories: no decline (no change in density), slow decline (0-2g/L/year) and rapid (>2).
Multivariate analysis was undertaken to ascertain predictors of survival or transplantation for 3 groups. 1: FEV1 < 30% predicted (n=35). 2: 30-50% (n=31). 3: >50% (n=44).
Results: 110 patients were identified. 43 died and 6 were transplanted.
In group 1 decline in density showed a slight trend to death/ transplantation (rapid decline: p = 0.137).
In group 2 (figure) slow decline in density showed a trend to death/transplantation (p=0.083), but rapid decline was significantly associated with death/transplantation (p=0.014).
There was no relationship between decline in densitometry and survival/transplantation in group 3.
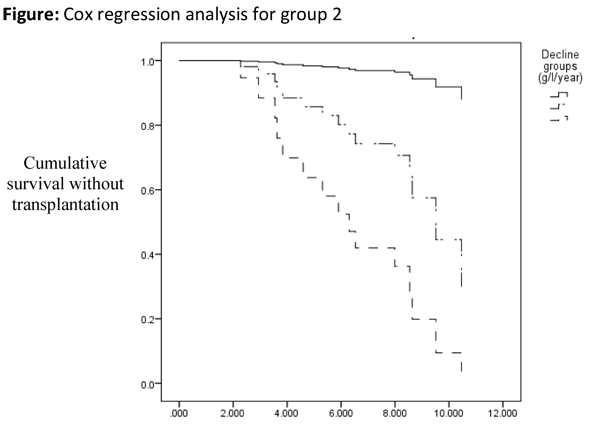
Conclusions: Decline in lung density may be a suitable surrogate outcome measure for likely survival/transplantation in AATD, and could identify a group more likely to benefit from augmentation in the shorter term.
Reference: Dawkins P, et al. Thorax. 2003;58: 1020-6
The Effect of Posture on Ventilation Using Structured Light Plethysmography (SLP) in Alpha-1 Anti-trypsin Deficiency (A1ATD)
L.C. O’Reilly, E. Sapey, S.D. Desando, J.A. Stockley, R.A Stockley, B.G. Cooper
Lung Function & Sleep, Queen Elizabeth Hospital Birmingham, B15 2WB, UK.
Introduction: Structured Light Plethysmography (SLP) determines changes in ventilatory patterns by utilising relative thorax contribution (RTC), inspiration to expiration ratio (IE50), inspiration time (Ti), inspiration and exhalation flux (Ti/Ttot) & breathing asynchrony by phase angle (PA).
Aims: To measure the change in breathing patterns by SLP between sitting and supine in patients with A1ATD with varying levels of respiratory disease.
Methods: We measured respiratory signals using Thor3Di (PneumaCare, Cambridge, UK) in 27 A1ATD patients [16M:11F, mean age 56.0 years (SD +/-10.4); FEV1L: 2.10 (1.12); FVCL: 4.22 (1.30)] both sitting and supine for 1-2 minutes and analysed them using Mann-Whitney tests.
Results: There were differences in both IE50 & Ti/Ttot between A1ATD patients and healthy controls when supine (See Table1 ).
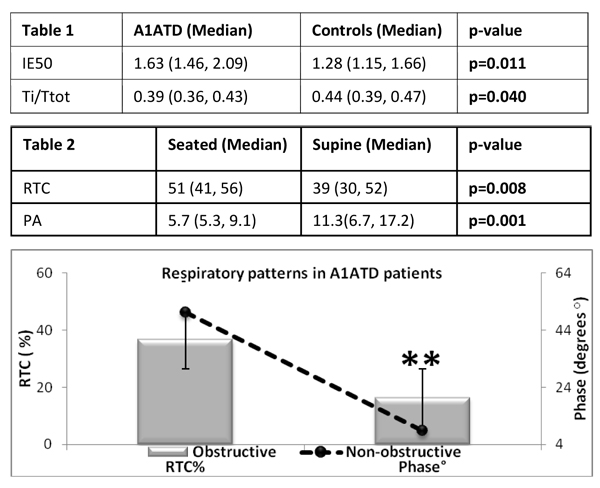
When supine data from A1ATD patients were separated into those with or without reduced FEV1/FVC ratio (<-1.64SR), the reduction in RTC & increase in PA was greater in the patients with airflow obstruction (Figure 1.)
Conclusion: These data shows that breathing becomes more abdominally dominant and more asynchronous in the supine position and is increased in the presence of airflow obstruction. SLP measures this remotely.
AE COPD 3Rs: Introduction and Efficacy of a Novel Mnemonic to Improve Compliance with Guidelines for the Management of Acute Exacerbations of COPD
S. Lugg,1 C.M. Jones,1,2 & S. Gompertz,1
1 Queen Elizabeth Hospital Birmingham, University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK,2 College of Medical & Dental Sciences, University of Birmingham, UK
There is a paucity of literature concerning compliance with guidelines for the early management of acute exacerbations of COPD (AE-COPD), predominantly performed by junior doctors. We introduced a novel mnemonic to aid recall of national guidelines,‘AE-COPD-3Rs’: antibiotics, enoxaparin, corticosteroids, oxygen, nicotine patches, dilator (bronchodilator) nebulisers, consideration of respiratory failure, respiratory support team (RST, a specialist respiratory multidisciplinary team) referral and triage to a respiratory ward.
The initial management of 44 prospectively identified patients presenting with an AE-COPD during February 2013 was retrospectively audited, after which the mnemonic was introduced and disseminated to junior doctors. Management was reassessed in 45 patients prospectively identified during February 2014 to avoid confounders. Paper and computerised medical and prescribing records were reviewed using a set pro-forma.
A greater proportion of patients were correctly prescribed enoxaparin (80vs39%), corticosteroids (93vs84%), nebulised salbutamol (91vs82%) and ipratropium bromide (87vs73%) following the introduction of the mnemonic. There were additional increases in referrals to our RST (44vs20%) and admissions under the care of a respiratory consultant (71vs57%). Minimal difference was seen in oxygen prescription rates (47vs43%).
Compliance with guidelines for AE-COPD management has improved, potentially benefiting patient outcome, which in part is secondary to the introduction of our AE-COPD-3Rs mnemonic.
A Comparison of Current and New Predicted Normal Ranges for Identifying the Presence and Severity of Lung Disease
P.H. Khaing,1 J.A. Stockley,2 and B.G. Cooper,2
1 School of Medical and Dental Sciences, University of Birmingham,2 Lung Function & Sleep Department, Queen Elizabeth Hospital Birmingham
Rationale: Accurate interpretation of spirometry results requires comparison to predicted normal ranges derived from reference equations. The European Community for Coal and Steel (ECCS) equations (Quanjer et al. 1983; Bull Eur Physiopathol Respir 1983; 19:66-92) are currently used but the Global Lung Initiative (GLI) have recently developed equations based on a much larger and diverse global cohort (Quanjer et al. Eur Respir J 2012; 40:1324-43). We sought to compare these reference equations for both Forced Vital Capacity (FVC) and Forced Expired Volume in 1 Second (FEV1).
Methods: Spirometry data from 433 patients (243 males, 190 females, mean age 58 (SEM=0.69)) with varying respiratory conditions were retrospectively analysed. Percentage predicted (% Pred) and standard residuals (SR) for ECCS and GLI were compared for all data. In 186 patients with Chronic Obstructive Pulmonary Disease (COPD), we also compared the classification of disease severity (based on FEV1 % Pred).
Results: There were significant, strong correlations in % Pred and SR between ECCS and GLI values for both FEV1 and FVC (r,2>0.95, p<0.0001 for all correlations). However, the GLI equations produced significantly lower % Pred and SRs for FEV1 and FVC (p<0.05). There was a small percentage of patients who were classified as normal by ECCS but abnormal (below -1.645 SR) by GLI for FEV1 (9.9%) and FVC (8.5%). These patients were predominantly female (p<0.04 for FEV1 and FVC), older (p<0.0001 for FEV1 only), and shorter (p<0.001 for FEV1 and FVC). For COPD, 15% of patients were reclassified into more severe stages by the GLI equations.
Conclusion: The GLI equations generally resulted in lower % Pred and SR values for FEV1 and FVC. This may impact on the clinical management of respiratory diseases such as COPD and could also affect inclusion/exclusion of patients into clinical trials.
The Impact of Exacerbations and Hospitalisations on the Economic Burden of COPD in Turkey: A Payer’s Perspective
M. Polatli,1 S. Malhan,2 C. Öztürk,3 on behalf of European COPD Audit Turkey Study Group
1 Adnan Menderes University, School of Medicine, Aydin, Turkey,2 Başkent University, The Faculty of Medical Sciences, Ankara, Turkey,3 Gazi University, School of Medicine, Ankara, Turkey
Background: Acute exacerbations of chronic obstructive pulmonary disease (COPD) are a leading cause of hospitalisations and the major cost driver in COPD healthcare. Patients with a history of exacerbation or hospitalisation account for much of the COPD-related mortality and incur excessive financial burden and medical care utilization. This study has estimated the total direct costs for the management of COPD patients with a history of exacerbation or hospitalisation. We also aimed to find the key cost drivers within this perspective.
Methods: The methodology was based on the results the first European COPD Audit report published by ERS and The Burden of Obstructive Lung Disease Initiative (BOLD). The economic costs was extrapolated according to the records of 22 hospitals (mostly tertiary care hospitals) entered to the European COPD Audit study. One-year costs were identified by applying cost data to medical information obtained by medical records. The cost analysis was based on cost of illness methodology. Costs included those for medications, laboratory and diagnostic tests, and hospitalizations.
Results: Data available on admission from 612 patients were included in the analyses. According to GOLD spirometric classification, the patients are categorized as: 14.28 % GOLD I, 15.28 % GOLD II, 38.21 % GOLD III, and 32.23 % GOLD IV. The mean total direct cost was €3764.10 per patient per year. The total annual cost was correlated with the disease severity, and hospitalization contributed to the major portion of the cost. The average hospitalization cost including intervention was €1412,.59, laboratory and diagnostic tests cost were €82.91, comorbidity and complication cost were €1366.50, medication cost with side effects were €560.33.
Discussion: There is a significant correlation between the cost of COPD and disease severity with hospitalization leading to disease exacerbation being a major contributor to cost. The highest cost components were hospitalization cost, comorbidity and complication cost, respectively. Our results suggest that reducing the frequency of exacerbations and controlling disease progression might be the major factors to alleviate the economic burden of COPD.
Benchmarking the Assessment for Hospitalisation in Chronic Obstructive Pulmonary Disease Exacerbation: Special Reference to a Multicentre Study
K. Motegi,1 T. Horie,2 H. Katsura,3 K. Dobashi,4 K. Kida,1
1 Respiratory Care Clinic, Nippon Medical School, Tokyo,2 Yachiyo Medical Center, Tokyo Women Medical University,3 Respiratory Unit, Maebashi Red Cross Hospital,4 Faculty of Medicine School of Health Sciences, Gunma University, Japan
Purpose: To improve the treatment quality of patients with COPD, the Japanese Respiratory Society implemented a guideline based on the GOLD criteria. We assessed the actual treatment of COPD exacerbation in Japanese hospitals.
Methods: The current benchmarking report submitted by 8 centres contains the centres’ reference results over one year. The figures included in the report reflect the guideline-compliant treatment administered during hospitalisation. Treatment patterns were as follows: Group A: only medication, Group B: medication with oxygen therapy, and Group C: medication with invasive or non-invasive ventilation.
Results: We assessed a total of 142 patients (mean age 76) who were discharged from the centres. These included 4 public, 3 private, and 1 university hospital. The median length of hospital stay (LOS) was 13 days (inter quartile range, 11-21 days). The prevalence rates of Groups A, B, and C were 8.4%, 72.7%, and 18.9%, respectively. LOS was significantly prolonged in Group C (Group A vs. B vs. C: LOS, 14.8 days vs. 18.6 vs. 24, p < 0.05) LOS and duration of antibiotic administration showed a positive correlation (r = 0.54, p < 0.001). Similarly LOS and duration of administration of steroids showed a positive correlation (r = 0.3, p = 0.0007). Early start of pulmonary rehabilitation was associated with a shorter LOS (r = 0.43, p < 0.01). The duration of steroid administered for <7days, 7–14 days, and >14 days, and no steroid use was 34.8%, 27.7%, and 13.5% of all cases, respectively; 24% of all cases received no steroids. No significant difference was observed in the LOS between groups administered steroids for <7 days and those administered the same for 7– 14 days. However, LOS was significantly prolonged in the >14 days group. In univariate linear regression analysis, Stage 4 in GOLD 2010, long-term oxygen user prior to the hospitalisations, duration of administration of steroid/ antibiotics/oxygen/NPPV, and early start of rehabilitation were significantly correlated with LOS. In multiple regression analysis, the duration of use of oxygen during hospitalisation and until the start of rehabilitation were correlated with long LOS.
Conclusions: We have shown that an extended LOS was associated with oxygen use and systemic steroid therapy. Early pulmonary rehabilitation was closely associated with a shorter LOS.
Subjects with COPD Score Lower than Norm Compared to International Patients
B.M. Deering,1 R.W. Costello ,1,2
1 Department of Respiratory Medicine, and,2 Royal College of Surgeons in Ireland, Beaumont Hospital, Dublin 9, Ireland.
“The Montreal Neurocognitive Assessment (MoCA) is a simple stand-alone cognitive screening tool with superior sensitivity”. The normal range is 26-30 which is also the range for normal elderly individuals; patients with mild cognitive impairment (MCI) score <26 (range 19.0 -25.2). The purpose of this study was to compare the MoCA score with age matched norms as reported by Nasrredine et al, 2005.
Results: Patients reviewed n=66, patients included n=55 (23M, 32F). Eleven patients were excluded due to either a history of depression (n=7), legally blind (n=1) or refused (n=3)[. The average age was 72 (±8), COPD GOLD stage I n=3 stage, II n=12, stage III n=25, stage IV n=11. The average self reported exacerbation rate was 3 (±2) with a range of 0-8 and an average smoke pack years of 53 (±40). Twelve patients reported difficulties with cognitive function but none had reported this to their GP. The average MoCA score was 21 (±4.3), ]plus 1 for <12 years education = 21.6 (±4.1)[ with an average Z-score for age matched controls of -0.191 (±0.9) . Of the 55 patients 87% scored below 26 and 8 scored lower than 16.
Irish COPD patients score lower than age matched norms which could impact overall health status and morbidity.
Adherence to Inhalers After Discharge from Hospital Following an Exacerbation of COPD
B.M. Deering,1 N.M. McCormack,1 K. Hennigan,2 S. D’Arcy,3 M. Holmes,3 R.B. Reilly,3 R.W. Costello ,1,2.
1 Beaumont Hospital, Dublin, Ireland,2 RCSI, Dublin Ireland,3 Trinity College, Dublin Ireland.
Introduction: Non-adherence to inhaler medication is a major problem in managing COPD. We used a novel audio recording device (INCA) attached to an inhaler, to assess both temporal and technique adherence.
Method: A cohort of 24 patients with COPD were recruited on discharge from Hospital to take part in this study. Each patient was given an INCA enabled inhaler to use over the course of a month, at the end of which the recordings of inhaler use were downloaded from the devices and analysed.
Results: A total of 912 inhaler events were recorded from the INCA devices. Overall, 40% had less than 50% adherence. The results indicated three types of patterns of inhaler use; adequate adherence was seen in 9. Six of 20 had >50% errors in inhaler technique, and 5 omitted >40% of doses. The overall rate of adherence was 0.41±12. The use of an inhaler requires several steps to be performed in a co-ordinated manner; this relies on functional frontal-striatal regions of the brain, termed executive function. In this study, the median Montreal Cognition (MOCA) score for this cohort was 24 (9-30), with a strong inverse relationship of MOCA and adherence.
Conclusion: In this pilot study on adherence in COPD patients there were low levels of adherence.
Appropriateness of COPD Inhaler Prescribing in an Integrated Community-Based COPD Clinic
A. Hardy, S. Cowdell, P. Griffiths
Calderdale and Huddersfield NHS Foundation Trust, Calderdale Royal Hospital, Halifax, HX3 0SG
Background: A community based integrated COPD service commenced in 2011 and includes a weekly respiratory consultant led clinic.
Method: A retrospective review of prescribing in the first 12 months of the consultant led clinic.
Results: 108 patients were diagnosed with COPD on their initial visit. Mean predicted FEV1 44%, mean COPD assessment test score 23, and mean number of self-reported exacerbations in the preceding 12 months 2.9. GOLD staging was complete for 106 patients. 2 were GOLD group A, 19 GOLD B, 1 GOLD C and 83 GOLD D.
43% had medications changed at their first visit. Following this 8% were on a LAMA, 90% were on a LABA and 84% were on a combination device. 13% were on correct 1,st line therapy, 71% on correct 2,nd line therapy and 15% on therapy not recommended by GOLD (16 patients). The large majority of these were patients in GOLD B prescribed an ICS (13 patients).
Conclusions: Stratification of COPD using the GOLD criteria is feasible in a community based integrated COPD clinic. 15% of patients were on incorrect inhaled medications. ICS are over-prescribed in GOLD group B. Stopping ICS in these patients would save money and reduced unwarranted side effects.
Development of a 30-Day Hospital Readmission Predictive Model for Chronic Obstructive Pulmonary Disease
H.L. Kirchner, J.B. Leader, J.A. Stamm
Geisinger Medical Center, Danville, USA
Background: Hospital readmissions are a central focus of quality improvement and reimbursement methods. Historically, all-cause 30-day readmission for chronic obstructive pulmonary disease(COPD) is 22.6% among the United States Medicare population.
Methods: A retrospective cohort was assembled consisting of adult primary care patients with COPD (2004-2012) who were discharged alive from Geisinger Health System. Data was extracted from the electronic health record (EHR) which included demographic, co-morbidities, lab results and utilization history. A predictive model, using machine learning techniques, was developed to identify patients at increased risk of readmission within 30 days. Internal validation was performed using 10-fold Cross-Validation (CV).
Results: A total of 1908 patients met study criteria (age 68.5 y, 52% male). 18% had a readmission within 30 days after discharge. A predictive model incorporating variables across domains of recent inpatient and outpatient utilization, laboratory tests, and admission characteristics yielded a CV area under the curve (AUC) of 0.70. The most influential variables were recent hospitalizations and discharge disposition. Analysis was repeated for readmission within 120 days; similar results were obtained.
Conclusions: A robust EHR can facilitate the identification of COPD patients at risk for readmission after hospitalization and allow for targeted interventions designed to reduce readmissions.
The Relationship Between GOLD Grouping and Nutritional Status of Patients with Chronic Obstructive Pulmonary Disease: A Pilot Study
Y-Y. Chen, H-Y. Chan, Y-T.Dai
Department of Nursing, College of Medicine, National Taiwan University.
Background and aims: The GOLD ABCD grouping for chronic obstructive pulmonary disease (COPD) patients was established in 2011, and it made the treatment for COPD patients more efficient. However, nutrition was neglected in the managements of patients with COPD. The study was to examine the relationship between the GOLD grouping.
Methods: A total of subjects were recruited. In the COPD assessment, we selected the COPD assessment test (CAT) scale for assessing symptom, and used lung function and the history of exacerbation for assessing risk of exacerbation. The nutritional status was evaluated using their body mass index (BMI).
Results: Thesubjects were mostly men (88.9%) and a mean age of 72.14 (SD=10.46) years. Underweight (BMI<20) occurred in 24.4% of the patients. The average BMI of GOLD group A, B, C, and D were 24.62 (n=9), 23.58 (n=18), 18.79 (n=3), and 22.58 (n=15), respectively. There was no significant difference between BMI and GOLD ABCD grouping (P=0.109).
Conclusions: We found that malnutrition existed in patients with COPD. However, patients had no difference in BMI by GOLD ABCD grouping. In additional to BMI, we suggested that the indicators of nutritional status: mini nutritional assessment (MNA) and fat-free mass (FFM) could be measured and compared using GOLD ABCD grouping in future study.
Randomized Controlled Trial of a Respiratory Retraining Program for Hospitalized COPD Patients
H-Y.Chan, Y-T.Dai
Department of Nursing, College of Medicine, National Taiwan University
Aims: To evaluate a respiratory retraining program for COPD inpatients in a medical center.
Methods: From May 2013 to Feb 2014, participants were randomly assigned to experimental group (n=24) or control group (n=21). The same training protocol was conducted by a research nurse in both groups, additional tablet-computer for assisting participants to practice respiratory. The self-efficacy, quality of life, accuracy in breathing skill, frequency of practice and the feedback on tablet-computer teaching were evaluated with double-blind assessments at baseline, immediate, 1-month and 3-month follow-up after training completion.
Results: The participants were mostly male (88.89%) and age 72.14 (SD=10.46) years old in averaged. Findingshowed the average total means of target indicators were improved but no statistic difference between experimental group and control group. Nevertheless, experimental participants expressed they have more satisfaction during learning. In addition, we found Gold group C and D had higher frequency of practice than group A and B (Wald χ,2=11.500, p=0.000) according the combined COPD assessment released in GOLD 2011.
Conclusions: Using tablets-computer for health training might be an alternative to motivate and enhance elders’ learning. Nurses may need to find strategy or material to motivate the COPD patients with lower risk (group A & B) to practice more and benefit from the respiratory retraining.
The Distribution of COPD Patients by GOLD 2011 Classification In UK Primary Care
N.Rajakumaraswamy,1 H.Mullerova,2 P.Engel,3 J.Chapaneri,1 J.James,3
1 GSK UK LOC, Medical Affairs,2 GSK R&D, Respiratory Epidemiology,3 Quintiles, Real-World & Late Phase Research
Background: The GOLD Strategy 2011 introduced a combined assessment of symptoms, airflow limitation and exacerbations in order to comprehensively assess the disease impact on COPD patients. Using the Patient Outcomes and Information Service (POINTS), an analysis and audit service in UK general practice, we explored characteristics of COPD patients and categorised them based on the GOLD 2011 groups.
Methods: POINTS allowed the extraction of entire anonymised disease cohort for each participating general practice. Patients who had the first COPD-related review on or after 1,st Jan 2010 were included in the analysis. mMRC was used to define symptom severity.
Results: Since 2010, a total of 252,340 COPD patients visited one of the 2,469 participating general practices. Among them, 107,629 (42.7%) had all data allowing ascertainment of the 2011 GOLD Grade with proportional representation of Group A in 33%, B in 24.8%, C in 17.1% and D in 25.1% patients, respectively.
Conclusion: In this large cohort, there was representation from all the GOLD grades. Despite different risk level and symptom severity, these groups were comparable across demographic characteristics.
The Patient Outcomes and Information Service (POINTS) is sponsored by GlaxoSmithKline.
Real World Utilization of Methylprednisolone, Prednisolone or Hydrocortisone Among Hospitalized COPD Patients in the United States (US)
C.M. Graham,1 H. Tucker,2 J. Gayle,1 J. Orazem,2 L.Z. Liu,2,3
1 Premier Inc., Charlotte, NC,2 Pfizer Inc, New York, NY,3 Weill Medical College of Cornell University, New York, NY
COPD patients are often hospitalized for emergency treatment. This retrospective database study was conducted to assess the real world treatment pattern of hospitalized COPD patients in the US. This study, using the Premier research hospital database, focused on COPD patients discharged between 2007 and 2012 and treated with methylprednisolone, prednisolone, or hydrocortisone in the US. A total of 140,378 patients were included in the analysis. The average age for the three groups was 69, 54 and 70, respectively. A vast majority of the patients were treated with methylprednisolone (138,248; 98%), followed by hydrocortisone (1,928) and prednisolone (210). The patients on methylprednisolone were predominantly treated with IV formulation (99%), while most prednisolone patients were given oral (99%). The study population was predominately white (66-76%), first seen in the emergency department (72-79%) and discharged to their homes (64-83%). In-hospital death rate varied from 1-11% among the three groups. The mean hospital length of stay varied from 4.6-8.8 days for the three groups. All-cause 30-day readmission rates for the three groups were 13.9-19.1%. There were substantial differences in demographics and other factors among COPD patients treated with the three medications. COPD patients were predominantly treated with methylprednisolone in the US hospitals.
Vitamin D and Diagnosis of COPD in a Working Population
K. Nishimura,1 S. Mitsuma,2 K. Nakayasu,3
1 Department of Pulmonary Medicine, National Center for Geriatrics and Gerontology, Obu, Japan,2 Niigata Association of Occupational Health Incorporated, Niigata, Japan,3 Data Research Section, Kondo P.P. Inc., Osaka, Japan
The purpose of the present study was to investigate whether serum concentrations of 25-hydroxy vitamin D could play a role in or could be related to the diagnosis of COPD. Serum 25-hydroxy vitamin D (25(OH)D) levels were measured in 299 industrial workers. To determine the relationship between vitamin D and airflow limitation, all the participants underwent spirometry. The prevalence of COPD defined by the fixed ratio was 14.1%. Mean 25(OH)D levels didn’t differ significantly between patients with COPD and healthy smokers (24.6±6.7 ng/mL in patients with COPD vs. 24.6±6.7 ng/mL in healthy smokers; not significantly different). Statistically significant correlations were not found between any measurements done by spirometry, including FEV1 as well as FEV1/FVC, and 25(OH)D levels. The mean±SD values of the FEV1 were 3.26 L ± 0.47 L in the lowest 25(OH)D quartile (<19.0 ng/mL), and 3.08 L ± 0.63 L in the highest quartile (≧29.1 ng/mL) (not significantly different). Although it has been reported that vitamin D insufficiency and deficiency are common in smokers with COPD, the association between 25(OH)D levels and COPD did not meet the level of statistical significance in the present study conducted in a working population.
A Systematic Review of Laboratory- and Field-Based Exercise Capacity Tests in Patients with COPD: Correlations with Forced Expiratory Volume in 1 Second and the St George Respiratory Questionnaire
M. Bell,1 I. Fotheringham,1 Y. Punekar,2 J.H. Riley,2 S. Cockle,2 S. Singh,3
,1Value Demonstration Practice, Oxford PharmaGenesis™ Ltd, Oxford, UK, ,2GlaxoSmithKline, Uxbridge, UK, ,3Department of Respiratory Medicine, University Hospitals of Leicester NHS Trust, Leicester, UK
Objectives: Laboratory- and field-based exercise tests are used to assess exercise capacity in patients with COPD. However, it is unclear how these tests relate to forced expiratory volume in 1 second (FEV1) or to the St George Respiratory Questionnaire (SGRQ). We systematically reviewed correlations between SGRQtotal, FEV1 and measures of exercise capacity.
Methods: A search of Embase, MEDLINE,® and The Cochrane Library identified primary publications in English that reported Pearson’s or Spearman’s rank correlations between FEV1, SGRQtotal and the following exercise tests: 6- and 12-minute walk tests (6MWTs and 12MWTs), incremental and endurance shuttle walk tests (ISWTs and ESWTs), treadmill test (TT) and incremental and endurance cycle ergometer tests (ICETs and ECETs).
Results: Correlations between exercise tests and FEV1 and SGRQ were reported in 39 (N=3,544) and 13 (N=3,296) studies, respectively (Table).
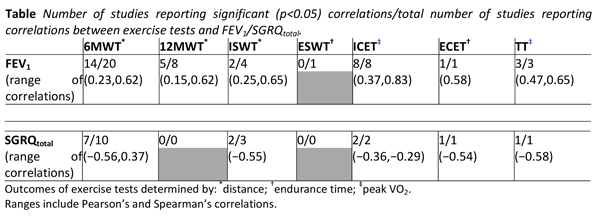
Conclusions: This systematic review suggests that most exercise tests correlate to some extent with FEV1 in patients with COPD; however, the evidence is too inconsistent to make meaningful assessment of the relationship between exercise tests and SGRQtotal. The lack of evidence to support strong correlations between exercise tests and FEV1 or SGRQtotal suggests further evaluations are needed to interpret the results of these tests in patients with COPD.
The Association of Anxiety or Depression on Early Hospital Readmission in COPD: Prospective Observational Study
L. Crawfurd, V. Padmanaban, C. Bloom, S.L. Elkin.
Imperial College Healthcare NHS Trust, St Mary’s Hospital, Praed Street, London- W2 1NY
Introduction: Chronic Obstructive Pulmonary Disease (COPD) results in substantive burden on healthcare utilisation (Simon-Tuval et al, Respiratory Research 2011; 12 (1): 7). Understanding factors that influence this are important. We wanted to assess if depression or anxiety were associated with early readmission at 30 days.
Methods: We conducted a prospective observational study on 58 patients admitted with COPD exacerbation between October 2013 and February 2014. Patient’ Hospital Anxiety and Depression Scores were completed on admission and data on hospital readmission, A&E attendances or community contact (COPD team) were collated.
Results: Twelve patients made unscheduled hospital attendances (readmission or A&E), 7 only contacted the community team and 39 made no known contact. Anxiety was found to be significantly associated with patients who only made contact with the community team compared to those who either attended hospital or made no contact (p=0.05, Pearson’s chi-squared). Depression was not found to be significantly different across the three groups (fig. 1).
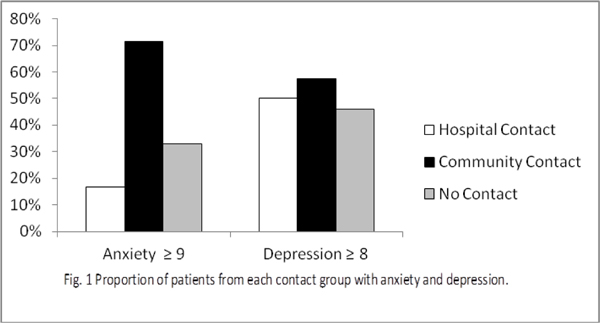
Discussion: In our post admission COPD cohort we found an association between early contact with community teams and anxiety. Whilst there was no association with 30 day hospital attendance we hypothesise that if there were no community services these patients may have attended A&E.
Role of Recurrent Admission Patient Alert System (RAPA) in Chronic Obstructive Pulmonary Diseases
V. Padmanaban, S.L. Elkin.
Imperial College Healthcare NHS Trust, St Mary’s Hospital, Praed Street, London- W2 1NY
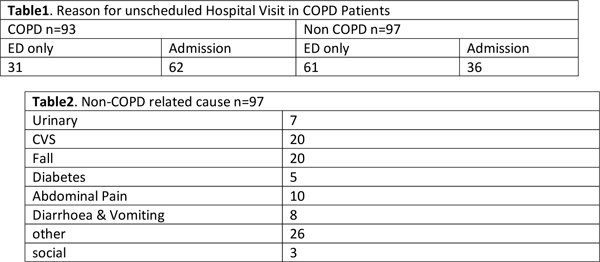
Introduction: The increasing prevalence of chronic obstructive pulmonary diseases (COPD) requires innovative approaches to improve care. RAPA is automated alert system, which notifies Clinicians that a patient has made unscheduled hospital visit, including Emergency department (ED). It is already used in cancer care. We developed this technology to receive alerts for COPD patients already known to integrated care teams and piloted it in our hospital.
Methods: We observed the alerts for a period of six months. During this period both hospital and community COPD teams received alerts to their mobile device via email. There was simple modus operandi in place to support staff when the alerts received.
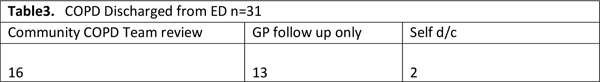
Findings: Between September 2013 to March 2014, we received a total of 190 alerts. Of this only 49% were due to COPD and rest were due to other reason (Table2). Thirty one patients with COPD related visit were discharged from ED without admission, 50% of these patients received community COPD team support based on the alerts.
Conclusion: We found RAPA useful in promptly alerting clinician and help plot admission trends in COPD patients at risk for readmission. Further work is needed in establishing alert pathway and defining role of Clinicians receiving alerts.
Can an Inhaler Technique Programme Show Sustained Improvements Among Health Care Professionals?
K. Fern, P. Marks, D. Dev, S. Gaduzo
Stockport NHS Foundation Trust, Floor 2 Kingsgate, Wellington Road North, Stockport, SK4 1LW
Introduction: Despite developments in inhaled treatments and devices, good inhaler technique remains a challenge for patients AND health care professionals (HCP). An inhaler technique improvement project was devised to standardise training for HCP across Primary and Secondary care.
Project overview: We produced educational podcasts showing correct techniques for each device. Key instructions were; inhale “gently and deeply” for MDI devices and “forcefully and deeply” for dry powder devices (DPI’s). Launch events were held and resources provided to wards, practices and pharmacies.The podcasts are also available for patients. A training session at the hospital was repeated 8 times over 2 days, and included an expert speaker.
Here we report outcomes of the training session.
Outcomes: 156 HCP attended training from a range of disciplines. Their inhaler technique was assessed using the InCheck Dial. Results in the desired range were 92% for the DPI and 5% for the MDI. 44/156 were reassessed after 3 months with improvements evident (correct DPI 97.7%, MDI 50%). 70% had advised patients about inhalers, but only 16% had checked technique on >10 patients in 3 months.
Conclusions: Results suggest sustained improvements 3 months after training. More work is needed locally to promote routine inhaler technique checks.
]