Running Head: Defining Airflow Obstruction
Funding Support: n/a
Date of Acceptance: November 20, 2015
Abbreviations: forced expiratory volume in 1 second, FEV1; forced vital capacity, FVC; lower limits of normal, LLN; chronic obstructive pulmonary disease, COPD
Citation: Eschenbacher WL. Defining airflow obstruction. Chronic Obstr Pulm Dis. 2016; 3(2): 515-518. doi: http://doi.org/10.15326/jcopdf.3.2.2015.0166
Introduction
Pulmonary function testing including spirometry testing is performed in a clinical setting to evaluate patients who present with respiratory symptoms. The interpretation of spirometric test results can identify an abnormal pattern which may be associated with the presence of disease. One of the abnormal patterns of spirometric test results is airflow obstruction. Airflow obstruction refers primarily to a finding, by spirometry, of a reduced expiratory airflow compared to the total amount of air exhaled. This has been defined as a reduction in the ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC). This is the physiologic definition of airflow obstruction. As such, the finding of airflow obstruction has been considered to be a critical element of certain diseases such as chronic obstructive pulmonary disease (COPD). In fact, for many, the identification of the presence of COPD has required that physiologic airflow obstruction be present.
The problem has been that we have defined airflow obstruction either as the ratio of FEV1/FVC being below a fixed value (70%)1 or below the lower limits of normal (LLN) (less than the 5th percentile) of a normally distributed set of values of FEV1/FVC for a population of non-smoking, normal individuals.2,3
With other diagnostic test results, a positive or abnormal test result is found in patients with the disease or condition. By the same logic, it might be more appropriate to define airflow obstruction not by a normal population but as found in patients with an airways disease or condition such as COPD. Unfortunately, we do not know the distribution of FEV1/FVC values for a patient population with COPD because we do not have a gold standard for the definition of the presence of the disease or syndrome of COPD.
Said differently, the distribution of values of FEV1/FVC for a normal population is not the same as the distribution of values of FEV1/FVC for a population of patients with a disease such as COPD.
Thus, a concern has been using a definition of airflow obstruction based on comparison of actual spirometric results to values of FEV1/FVC (LLN) from a set of values from normal populations or a fixed cutoff to identify the possible presence of a disease such as COPD where the values of FEV1/FVC are different from the normal populations.
Presence Versus Absence of Airflow Obstruction
The next issue is that we have defined airflow obstruction as either being present or absent based on spirometric test results: FEV1/FVC below 70% or the LLN from reference equations or above those values. Instead, we should use a different approach to define airflow obstruction based on the probability or likelihood that the airflow obstruction is present which in turn would give us the probability or likelihood of a disease state such as COPD.
In addition to using cutoffs for FEV1/FVC for defining airflow obstruction, some authors have recommended using Z-scores for determining the severity of airflow obstruction based on FEV1 values from the spirometric test results.4
Instead, if we used Z-scores for the difference between predicted values of FEV1/FVC and the test result of FEV1/FVC to estimate the likelihood of the presence or probability of the presence of airflow obstruction, we are still basing these comparisons with those values from normal populations. Ideally, if the Z-score is of a certain value, we could estimate the probability that the presence of airflow obstruction that exists could be associated with a clinical condition such as COPD. The higher the magnitude of the negative Z-score, the more likely that airflow obstruction as found in COPD is present. For example:
Likelihood of Airflow Obstruction
> 0 zero likelihood (none)
0 to -1 10% likelihood (minimal chance)
>10% to < 20% likelihood (intermediate chance)
>20% to < 75% likelihood (high chance)
> 75% likelihood (very high chance)
This may be a more useful way of interpreting spirometry test results for airflow obstruction. As an example, there may be a patient who could have COPD with known smoking history and respiratory symptoms and even radiographic findings who has a value of FEV1/FVC that is above the LLN but below the predicted value (Z score between -1.64 and 0). For this patient, there might be some likelihood that he or she has some degree of airflow limitation rather than interpreting the spirometry as no airflow obstruction.
One problem becomes in assigning the values for the probability or likelihood of airflow obstruction for a given Z-score (10% versus 10%-20% versus 20%-75% in the table above). Since the definition of airflow obstruction in the past has been arbitrarily based on a cutoff of the FEV1/FVC (either LLN or 70%), it would be uncertain how the values for probabilities or likelihoods in the table above would be determined.
More importantly, even if we say that there is greater likelihood of airflow obstruction by Z-score, it is unclear that there would be a direct correlation with finding a higher likelihood of a disease such as COPD. Thus, as discussed above, does the finding of airflow obstruction by spirometry using comparisons to test results from normal populations equate to the identification of a disease such as COPD?
Severity of Airflow Obstruction
In the past, many have followed the lead of the American Thoracic Society and the European Respiratory Society2 and defined the severity of the abnormality as identified by lung function testing as the % of predicted for the value of the measured FEV1:
Mild defecta: FEV1 % of predicted ≥ 70%
Moderate defecta: FEV1 % of predicted ≤ 69% and ≥ 60%
Moderately Severe defecta: FEV1 % of predicted ≤ 59% and ≥ 50%
Severe defecta: FEV1 % of predicted ≤ 49% and ≥ 35%
Very Severe defecta: FEV1% of predicted < 34%
adefect refers to the presence of an abnormal parameter such as airflow obstruction, restrictive lung defect, or mixed impairment
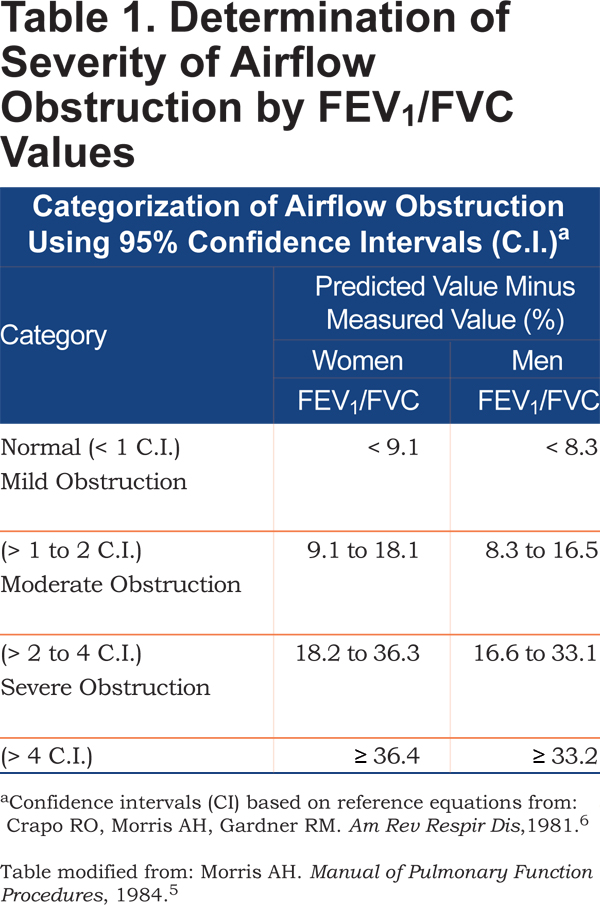
Instead, we could use the value of the FEV1/FVC ratio as the measure of not just the presence of airflow obstruction but also the degree of severity as shown in Table 1 which has been modified from the Intermountain Thoracic Society’s Manual of Pulmonary Function Procedures.5 The values for the confidence intervals for this table come from an earlier report on spirometric reference values.6
However, again we are comparing test results to those results from normal populations to define the presence and severity of airflow obstruction when our ultimate goal is the identification of the presence of an abnormal pattern of spirometry that is found in a disease such as COPD.
Summary
Our current definition of airflow obstruction based on spirometric values of FEV1/FVC compared to a fixed cutoff (70%) or LLN, may not be the most appropriate approach to identifying patients who may have an airways disease such as COPD. Since abnormal airflow mechanics exist in conditions such as COPD and asthma, it would be more appropriate to define airflow obstruction knowing the distributions of airflow limitation in patients with these airways diseases. In addition, it would also be more appropriate to determine the likelihood or probability of the presence of airflow obstruction (not just the absence or presence) that could better help evaluate the presence of the airways disease itself.
The goal of interpreting lung function testing is to provide an expert opinion regarding the results of the test and how the test results are useful based on the clinical context to help in the evaluation of the patient. Knowing that our current approach to interpreting airflow obstruction is based on values of FEV1/FVC from normal populations is less than ideal for the identification of the presence of airway diseases in the patient.
I would recommend that at this time, without knowledge of the distribution of FEV1/FVC values for a diseased population, that spirometric test results should be interpreted with a cautionary note that the interpretation of airflow obstruction by comparing test results to those from a population of normal individuals may not identify the presence of an airway disease. Also, I suggest that we should interpret the probability or likelihood of the presence of airflow obstruction and not that it is either present or absent, especially in the clinical context of the identification of an airways disease. Thus, the finding of a reduced FEV1/FVC by itself does not equate to disease just as a normal value for FEV1/FVC does not exclude the presence of a disease like COPD.