Running Head: Primary Care Beliefs, Attitudes, and Barriers for COPD Management
Funding Support: None
Date of Acceptance: February 4, 2016
Abbreviations: chronic obstructive pulmonary disease, COPD; Global initiative for chronic Obstructive Lung Disease, GOLD; continuing medical education, CME; nurse practitioners, NPs; physician assistants, PAs; medical doctor, MD; doctor of osteopathic medicine, DO; American Thoracic Society, ATS; European Respiratory Society, ERS
Citation: Yawn B, Wollan PC, Textor KB, Yawn RA.Primary care physicians’, nurse practitioners’ and physician assistants’ knowledge, attitudes and beliefs regarding COPD: 2007 to 2014. Chronic Obstr Pulm Dis. 2016; 3(3): 628-635. doi: http://doi.org/10.15326/jcopdf.3.3.2015.0168
Introduction
Chronic obstructive pulmonary disease (COPD) is common and people with COPD receive much of their care from primary care physicians1 and, more recently, nurse practitioners (NPs) and physician assistants (PAs). Yet that care is reported to result in significant rates of un-recognized and under-treated disease. Reported reasons for the gaps in care include limited awareness of COPD guidelines, time constraints, and lack of easy access and ability to interpret results of spirometry testing.1,2-13
Previously we reported an additional barrier, therapeutic nihilism,14 which is often discussed but seldom reported in studies of COPD management barriers.15 Yet beliefs that no useful therapies exist may affect primary care physicians’ and other clinicians’ prioritization to learn about diagnosing and managing COPD in their patient populations.
Since our previous report, COPD education has increased through the efforts of the Global initiative for chronic Obstructive Lung Disease (GOLD) dissemination committee,16 the National Heart Lung and Blood Institute’s Learn More, Breathe Better® campaign17 and continuing medical education (CME) programs from many sources. To assess the impact of these and other educational efforts on COPD-related knowledge, attitudes and beliefs of primary care health professionals, specifically physicians, NPs and PAs working in primary care, we again surveyed members of these groups attending large regional CME programs that included at least one session addressing COPD. By using the same survey that we used in 2007, we are able to assess current responses and compare them to those reported in 2007.14 The results should help determine the direction and potential value of future efforts to enhance COPD care among primary care clinicians.
Methods
This is a survey study of clinician attendees at 3 large regional continuing medical education (CME) programs designed to provide didactic presentations on a broad range of primary care topics including a 60 to 90 minute presentation on COPD. In addition to physicians, we included responses from nurse practitioners who have 2 years of training beyond their RN degree and in most areas of the United States practice in collaboration with a physician as well as physician’s assistants who have 3 to 4 years of training beyond their bachelor’s degree and are licensed to practice collaboratively with physicians.
Two of the CME programs were held in Florida (Continuing Education Company, Inc. in November 2013 and March 2014) and 1 in Chicago (Pri-Med Midwest, June 2014). The study was approved by the Olmsted Medical Center Institutional Review Board and the executive and scientific staff of Pri-Med Midwest and of the Continuing Education Company, Inc. Palm Coast, Florida.
For the 2013/2014 study, we used the same survey questions and the same methods of giving the survey to all attendees of selected CME programs as done in 2007 and reported in 2008.14 At each of the 3 CME events during 2013/2014, copies of the questionnaires were placed at each available seat in the educational venue or handed to each attendee as they entered the auditorium. The purpose of the survey, each individual’s right to choose to complete or ignore that survey and the name of the lead investigator were provided at the beginning of the day’s educational program and again 15-20 minutes prior to the COPD educational session provided by one of the authors (BPY). Attendees were requested to complete the survey prior to the COPD CME talk. The Florida sites provided time and encouragement for the attendees to complete the survey before the start of the day’s conference while the attendees at the Chicago conference had limited time for survey completion immediately prior to the COPD-related CME presentation. Surveys were collected either immediately prior to the beginning of the COPD talk or within the first 10 minutes of the talk to minimize the impact of information provided during the lecture on survey responses.
Attendees were asked to provide demographic information on age, sex, years in practice as medical doctor (MD), NP, or PA, size of practice, location of practice (city size), practice size, and specialty mix of practice. COPD-related questions included awareness and use of COPD guidelines, barriers to diagnosing COPD, factors used to make a COPD diagnosis, diagnostic tests for COPD, and questions about the perceived therapeutic benefit of available COPD therapies. A final series of questions queried attendees about overall COPD treatment effectiveness, specifically about the value of pulmonary rehabilitation and impact of pharmacotherapy on COPD symptoms, exacerbations, and patient longevity. The full survey is available in the Online Supplement Table 1.
Data Analysis
Simple descriptive statistics were used to present demographic characteristics of the responders as well as frequencies of response to knowledge and attitude questions. Knowledge and attitude responses were compared by clinician credentials and training and by region of the country (Florida versus Chicago) using chi-squared statistics. Finally, the 2013/2014 data were compared to responses from the 2007 survey using chi-squared statistics for responses to individual questions.
Results
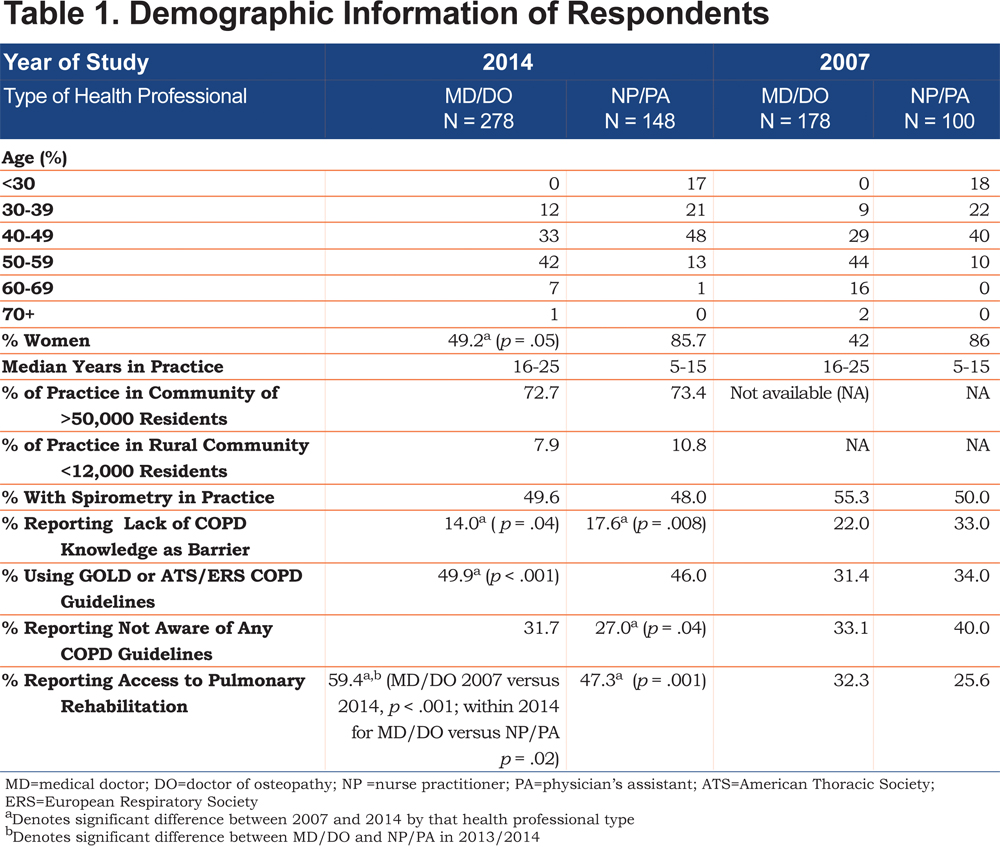
Overall 436 surveys (278 MD/doctor of osteopathic medicine [DO] and 148 NP/PA) were returned with all or most (>95%) questions answered. The response rate varied by site from 75% and 81% for the 2 Florida events to 44% from the Chicago event for an overall response rate of 61%. Information is not available on response rate by level of training. Physician respondents were older, less likely to be women and have more years in practice than NPs/PAs (Table 1). Overall, more than 70% of the respondents practiced in communities > 50,000 residents with about 8.0% of physicians and 10.8% of NPs/PAs practicing in rural communities. Half of the physicians practiced in single specialty primary care groups and 66.2% in groups of 5 or fewer physicians. Of the NPs, 15 of 56 (26.8%) worked in NP only offices. NPs and PAs reported that 57% had 5 physicians or fewer in their offices. NPs and PAs were slightly but not significantly less likely to work in single specialty practices compared to physicians. The only significant difference between Florida and Chicago respondents was that the Chicago clinicians were on average older than those from Florida. About half of the respondents reported awareness and use of COPD guidelines (49.9% of physicians versus 46.0% NPs/PAs) with 31.7% versus 27.0% respectively, reporting lack of awareness or use of any COPD guideline. The rest reported awareness that COPD guidelines were available but did not use them in daily practice. Only about one quarter of respondents thought that COPD patients’ symptoms were usually delayed until after 60 years of age and less than 10% considered COPD primarily a disease of men.
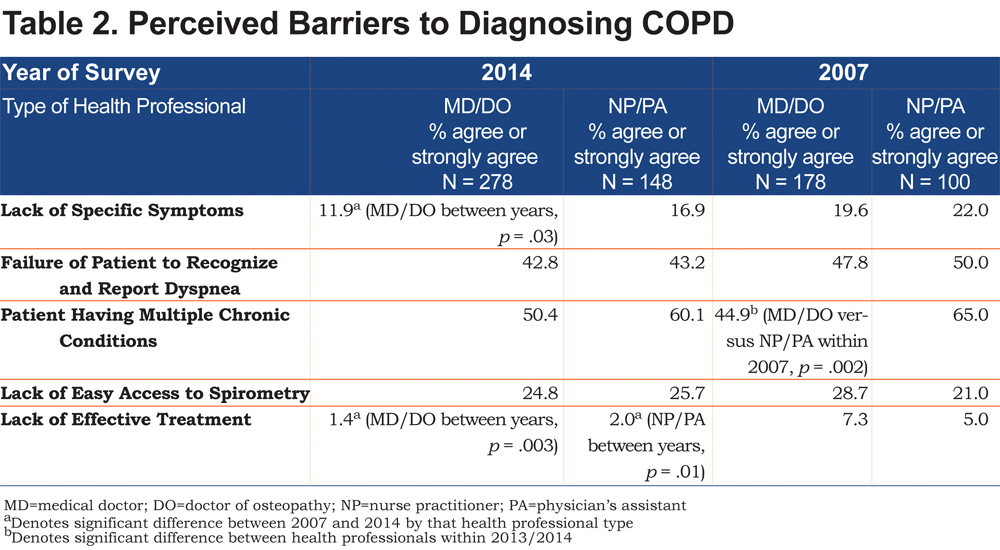
Barriers to making a COPD diagnosis varied little between MDs/DOs and NPs/PAs (Table 2). The most common barriers noted were patients having multiple chronic conditions and failure of the patients to recognize and report dyspnea. Lack of easy access to spirometry was reported by only one quarter of the respondents overall. Two percent or fewer thought that lack of effective COPD therapies was a barrier. None of the between group differences were statistically significant.
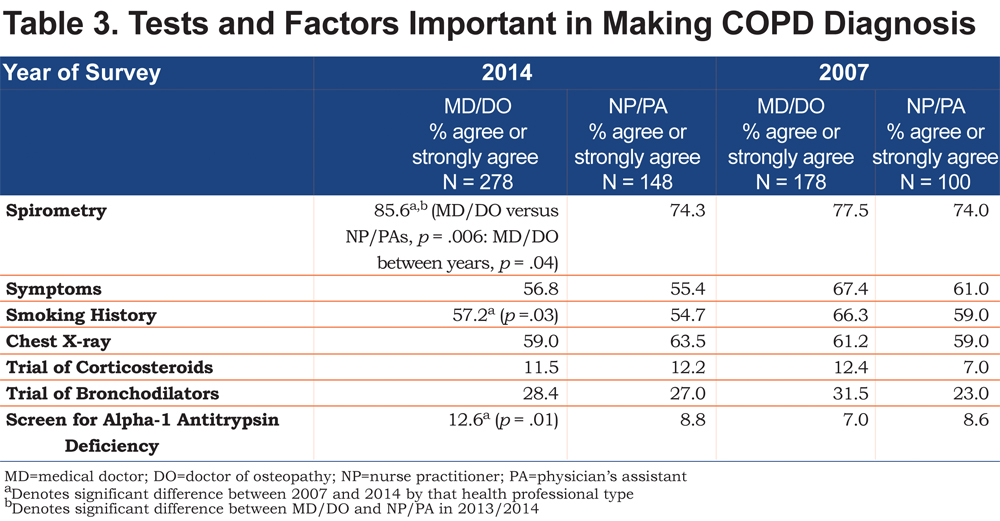
Spirometry was the tool most commonly reported to be used for diagnosis of COPD followed by chest x-rays, and a trial of bronchodilators (Table 3). Agreement that spirometry was important for COPD diagnosis was more common among physicians compared to NPs/PAs (85.6% versus 74.3% respectively, p = .006) despite reporting similar levels of easy access to spirometry. More than one quarter of physicians and NPs/PAs continue to use therapeutic trials of bronchodilators to diagnose COPD and over 10% reported use of a trial of corticosteroids to diagnose COPD. Screening for alpha-1 antitrypsin deficiency was limited but was reported to be close to 10% in both groups (12.6% of physicians and 8.8% of NPs/PAs).
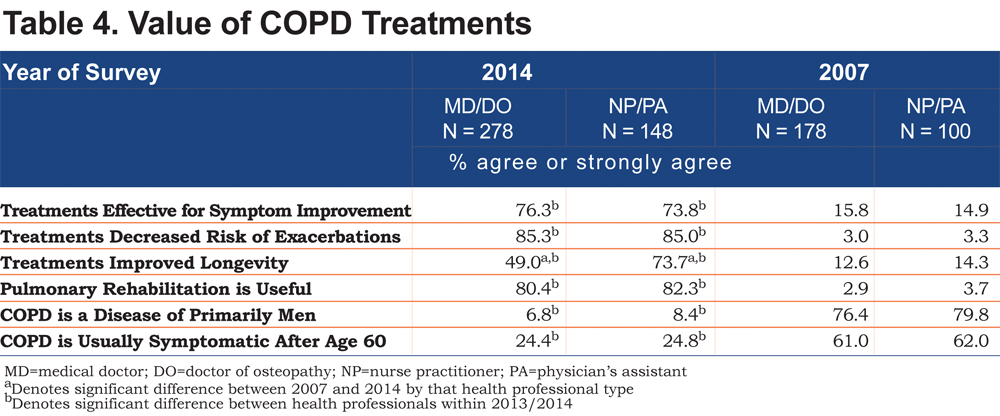
Three quarters or more of the 2013/2014 survey respondents thought that effective COPD treatment was available for several aspects of COPD including relieving COPD symptoms, and reducing exacerbations (Table 4). Only 7.9% of physicians and 13.6% of NPs and PAs disagreed or strongly disagreed that current COPD treatment improved symptoms. However, physicians were less likely than NP/PAs to report they thought current treatments were effective in increasing longevity in COPD patients (49.0% versus 73.7%, p <.001). Over 80% of respondents reported that pulmonary rehabilitation was useful in COPD and over 50% reported it was available to their COPD patients.
Changes from 2007 Study
The personal demographics of the survey respondents between 2007 and 2013/2014 changed only in the increase percent of the respondents who were women, primarily due to more women physicians responding. No significant changes in practice demographics were noted between 2007 and 2013/2014, including no increase in access to office-based spirometry. Both physicians and NPs/PAs reported that lack of COPD-related knowledge was less of a barrier to COPD care and use of COPD management guidelines, and access to pulmonary rehabilitation increased over the period (Table 1). Between 2007 and 2013/2014 physicians, but not NPs/PAs, reported an increase in the importance of spirometry in diagnosing COPD and were more likely to screen for alpha-1-antitrypsin deficiency. (Table 3) Among potential barriers to COPD diagnoses, reports of lack of COPD-specific symptoms and reliance on smoking history declined significantly among physicians.
By 2013/2014, fewer family physicians were referring patients to specialists for a COPD diagnosis, dropping from 20% in 2007 to 11.9% in 2014 while rates remained about 20% for NPs and PAs. The use of alpha-1 antitrypsin deficiency screening rose from 7.0% in 2007 to 12.6% in 2014 among physicians but remained basically unchanged among NPs/PAs.
The largest changes between 2007 and 2013/2014 responses were in all health professionals’ perceptions of the value of both pharmacological and pulmonary rehabilitation treatments for improving the lives of people with COPD. All groups reported very large increases in the perceived value of treatments in reducing symptoms, decreasing exacerbations, and improving longevity. The groups were less likely to report that COPD is a disease primarily of men and that COPD was usually not symptomatic until after age 60.
Discussion
Between 2007 and 2013/2014, there was a large and significant increase in the number of primary care physicians and NPs/PAs who reported believing that COPD treatments are beneficial. Confidence that COPD treatments could improve symptoms and decrease exacerbations increased by 4.8 and 28.4 fold respectively to 75.8% believing treatment improves symptoms and 85.2% believing treatment reduces exacerbations. The 2013/2014 groups also reported a few other significant changes in their knowledge, attitudes and beliefs compared to the 2007 group with greater reported awareness and use of COPD care guidelines and awareness that COPD is prevalent in both sexes and symptomatic prior to age 60. Only MDs/DOs were more likely to say they thought spirometry was a necessary test for COPD diagnosis in 2013/2014 compared to 2007. However, reported access to spirometry changed little over time as did other reported practice barriers to addressing COPD. The fact that physicians reported a decreased reliance on smoking history in making a COPD diagnosis, is interesting. Perhaps they have become aware of the reports that up to 20% of those with COPD have limited or no smoking history. 15,18
These results are encouraging and highlight an area often overlooked in studies of primary care management of COPD, namely primary care clinicians’ confidence in the benefit of COPD treatment or its inverse: therapeutic nihilism. Belief that no effective therapies exist can be a major barrier to any health care professional’s choice to attempt to identify, confirm or manage a chronic disease.15 The 2007 responses by physicians and NPs/PAs demonstrated limited confidence in existing COPD therapies that may have slowed any and all attempts to increase recognition of individuals at risk of COPD or to obtain and learn how to use and interpret results of diagnostic techniques such as spirometry. By 2013/2014, the primary care health professionals appeared to have hope that they could provide some relief for those diagnosed with COPD. This should provide an improved foundation for future work to include primary care physicians and other clinicians in improved COPD case finding, use of confirmatory testing and implementation of evidence-based guideline care. It may also explain why earlier attempts to promote more wide spread identification of a condition felt to be poorly treatable were less effective than planned.19-21
Comparison of our results with other surveys is limited due to the differing focus of various surveys. However, an international study that included 200 U.S. physicians2 also reported high confidence in current COPD therapies with 68% of responding physicians agreeing that “better treatments are leading to improved COPD outcomes” and 10% reporting that pulmonary rehabilitation was useful. This is comparable to the 85.6% of physicians answering our survey who reported believing medication could reduce exacerbations and the 78.7% who reported that COPD treatments were effective in relieving symptoms. The reported rates of use of spirometry, for those diagnosed with COPD, was 86% and reported to be similar across most countries including the United States. This is very comparable to the 85.6% of our physician respondents who reported they believed spirometry was important for a COPD diagnosis. Support for the value of pulmonary rehabilitation was higher among our physicians surveyed with 81.6% reporting that pulmonary rehabilitation was useful for COPD treatment versus only 10% in the Menezes U.S. respondents.2 Other recent studies include samples of international physicians, most with no representation of U.S. physicians, making comparisons with our results difficult.6,11,12,13
A 2008 study of 309 U.S. family physicians and 191 general internists was designed primarily to assess barriers to COPD guideline implementation with an emphasis on the use of spirometry.4 Self-reported use or importance of spirometry in making a COPD diagnosis was similar but lower than the rate reported by our physician respondents (69.1% versus 85.5%, respectively). Lack of familiarity with COPD guidelines was also similar across the 2 studies (24.0% in the Salinas et al sample versus 31.1% in our sample).4 A 2010 New York City based study of 154 general internists and internal medicine residents from 2 practices in Harlem1 reported that awareness of guidelines was similar to that reported by our physician respondents (about 47% in Harlem versus 49% among our respondents). In general, the New York general internists were younger and more recently in training than the family physicians we surveyed but the younger group reported no greater awareness of guidelines or use of spirometry evaluations than their older and less recently trained colleagues.1 Older data confirm the limited awareness of COPD management guidelines, therapeutic nihilism and under appreciation of the value of pulmonary rehabilitation reported by the respondents in our 2007 study.5,9
We found no other study that reported data on NP or PA knowledge, attitudes, beliefs or care activities related to COPD management. Some United Kingdom studies reported on the knowledge and attitude of practice nurses who always work collaboratively with a physician using collaboratively developed written care algorithms.8 In the United States, such guidelines may not be widely used and an increasing number of states allow independent practice of NPs. Therefore, it is important to better understand the NP training opportunities, knowledge base, and approach to the recognition, diagnosis, and management of individuals with COPD.
Our study has limitations due to its use of a convenience sample of physicians and NPs/PAs attending CME programs. The CME programs provided educational sessions on a wide variety of primary care topics making it unlikely that these clinicians chose to attend the programs due to either special interest or concern about lack of knowledge specific to COPD. Therefore, the respondents should represent a broad spectrum of primary care physicians and NPs/PAs working in primary care. While our data were self reported, we did not ask about what the clinicians did within their practices but rather about their knowledge, attitudes and beliefs,2,3,12,13 which may be less subject to reporting bias than actual practice activities.11 The attendees were from 2 large CME program sites and may not represent clinicians from other regions of the United States and therefore, the results may not be generalizable to all U.S. family physicians and NPs/PAs working in primary care. Very few general internists were included among the respondents. Information shared during the COPD CME lectures may have influenced the answers. Although surveys were collected either before or within the first 15 minutes of the COPD talks, slides from the talk were available within the coursework materials prior to the lecture.
Physicians and NPs/PAs demonstrated some marked changes in attitudes between 2007 and 2014 especially toward the therapeutic benefits of medications and pulmonary rehabilitation for individuals with COPD. There was also a marked decrease in the belief that COPD is a disease of men and only symptomatic after age 60. Overall, the results are encouraging, suggesting an increase in the confidence of being able to provide individuals with COPD benefit with treatment of symptoms and prevention of exacerbations, e.g., a decline in therapeutic nihilism. However, future studies need to assess whether these changes in self-reported awareness actually translate into enhanced guideline adherence and clinician COPD care and ultimately in patient diagnosis and outcomes.
Acknowledgements
The authors appreciate the cooperation of the staff of Continuing Medical Education Company, Inc. Palm Coast, Florida, director Walter Enjes, MD, and the staff of PrimeMed Midwest in collecting data from the CME conference participants to obtain the survey data and the assistance of Jennifer Johnson, MBA, in preparation of this manuscript.
Declaration of Interest:
None of the authors have any real or apparent conflicts of interest including no financial or consulting relationships to disclose.