Running Head: Barriers to Influenza Vaccination in COPD
Funding Support: This study was supported in part by a grant from the Center for Health Care Delivery Science, Beth Israel Deaconess Medical Center (DJH) and P30ES000002 (CMN)
Date of Acceptance: February 4, 2016
Abbreviations: chronic obstructive pulmonary disease, COPD; Behavioral Risk Factor Surveillance System, BRFSS; Centers for Disease Control and Prevention, CDC; confidence interval, CI; odds ratio, OR
Citation: Hsu DJ, North CM, Brode SK, Celli BR. Identification of barriers to influenza vaccination in patients with chronic obstructive pulmonary disease: analysis of the 2012 Behavioral Risk Factors Surveillance System. Chronic Obstr Pulm Dis. 2016; 3(3): 620-627. doi: http://doi.org/10.15326/jcopdf.3.3.2015.0156
Introduction
Chronic obstructive pulmonary disease (COPD) is the third leading cause of morbidity and mortality in both the United States and globally.1,2 Acute exacerbations of COPD are one of the most important causes of COPD-related morbidity and mortality, with infectious triggers such as influenza playing a major role.3 Influenza affects 5%-15% of the population annually, with just under 30,000 related deaths per year, predominantly in older patients and those with chronic respiratory diseases.4 In patients with chronic respiratory diseases such as COPD who are at risk for severe complications from influenza infection, vaccination has been shown to decrease influenza incidence, severity, hospitalizations, and mortality by up to 50%.5 Data from 2010 – 2011 indicate that 40.5% of all adults ≥ 18 years of age received influenza vaccinations and only 46.7% of adults with at least 1 high-risk medical diagnosis were vaccinated, rates that are well below the Healthy People 2020 goal of 70% vaccination for all adults.6
Identification of barriers to influenza vaccination among patients with COPD may provide insight into focusing efforts to increase vaccination rates in this particularly vulnerable population. The objective of this study was to determine the rate of influenza vaccination among patients with COPD and to identify independent factors associated with receipt of influenza vaccination.
Methods
Design
This analysis was performed using cross-sectional data from the 2012 Behavioral Risk Factor Surveillance System (BRFSS), a publicly available telephone survey of self-reported personal health behaviors, chronic health conditions and utilization of preventative services of non-institutionalized adults ≥ 18 years old residing in households.7 Conducted annually by the Centers for Disease Control and Prevention (CDC), the BRFSS uses a stratified sampling approach to obtain responses representative of state populations of adults aged 18 or older. Participants were identified through random digit dialing in all 50 states, the District of Colombia, Puerto Rico, Guam and the U.S. Virgin Islands, and the de-identified data is publicly available. The 2012 response rate was 49.1% for landline participants and 35.3% for cell phone participants, and the median weighted state-based response rate was 45.2%. To more accurately reflect the demographics of the American population and to deemphasize the effect of non-responder bias, the CDC uses iterative proportional fitting (ranking) to appropriately weight the respondent data.8 The Beth Israel Deaconess Medical Center Institutional Review Board has previously determined that the use of this database meets criteria for exempt status.
Study Sample
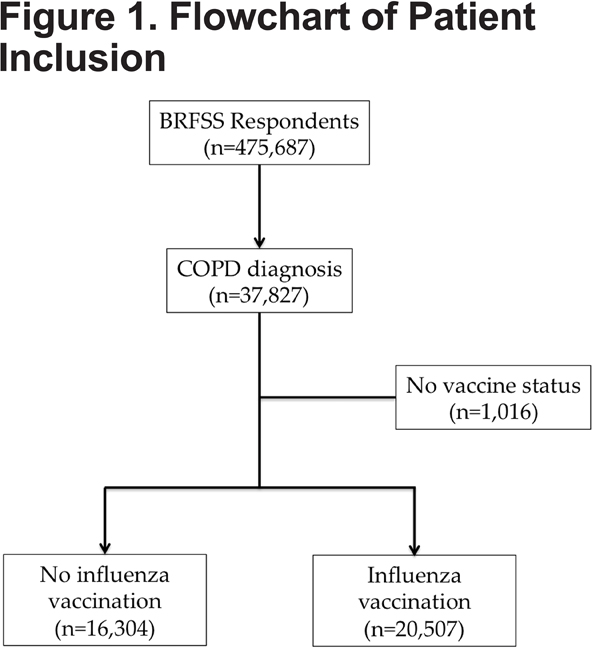
The primary outcome for this study was receipt of an influenza vaccination, either inactive or live attenuated, within the past 12 months as defined by an affirmative response by the respondent when directly queried regarding vaccination status. Likewise, respondents were determined to have COPD if they answered in the affirmative to having been given a prior diagnosis of COPD by a health care professional. The 2012 BRFSS survey included 475,687 respondents, of which 7.95% (n=37,827) reported a prior diagnosis of COPD. Of the respondents with COPD, 97.3% responded to the question assessing whether they had received an influenza vaccination in the past 12 months. The final study sample included 36,811 respondents with COPD who reported an influenza vaccination status, which represents 6.1% of the United States population (Figure 1).
Factors of interest were identified as candidate predictors prior to data analysis based on plausible association with influenza vaccination within the framework of the Andersen Behavioral Model and access to health care construct.10 The original Andersen Behavioral Model was developed as a framework to understand an individual’s utilization of health care services. This model organizes explanatory factors into 3 groups: pre-disposing, enabling, and need, with updated versions also incorporating behavioral and outcomes factors to account for the relationships between health outcomes, health care utilization, and explanatory factors. This model has been widely used as both a conceptual framework for understanding why specific populations utilize health care services, as well as an organizational framework for examining specific determinants of utilization.11-15 Predisposing factors used in this study included demographic covariates (age, race/ethnicity, sex, location, and family structure), enabling factors included household income, health insurance, ability to afford medical care, availability of medical resources, and employment. Need factors included perceived health status and chronic medical conditions.
Statistical Analyses
Descriptive statistics were used to compare vaccinated and unvaccinated respondents with COPD. Data were assessed to ensure completeness of response, and as missing data were minimal for most variables (defined as less than 3%), respondents with missing outcome variables or covariates of interest were excluded from the final study sample. Pre-specified candidate covariates were then included in a logistic regression model of influenza vaccination. A parsimonious model was created by using a backwards stepwise approach to remove variables from the main effects model with p values > 0.05. For all variables independently associated with influenza vaccination, odds ratios (ORs) and 95% confidence intervals (CIs) are reported. As the race/ethnicity, income, and rural/urban data elements had greater than 3% missing data, a sensitivity analysis was performed where these covariates were excluded during the model building process to assess the stability of the final model covariates. Data were analyzed with SAS 9.4 (SAS Institute, Inc., Cary, North Carolina) and SUDAAN (RTI International, Research Triangle Park, North Carolina) to account for the complex sampling design. All data were weighted to reflect national estimates; unweighted sample sizes and weighted percentages are reported.
Results
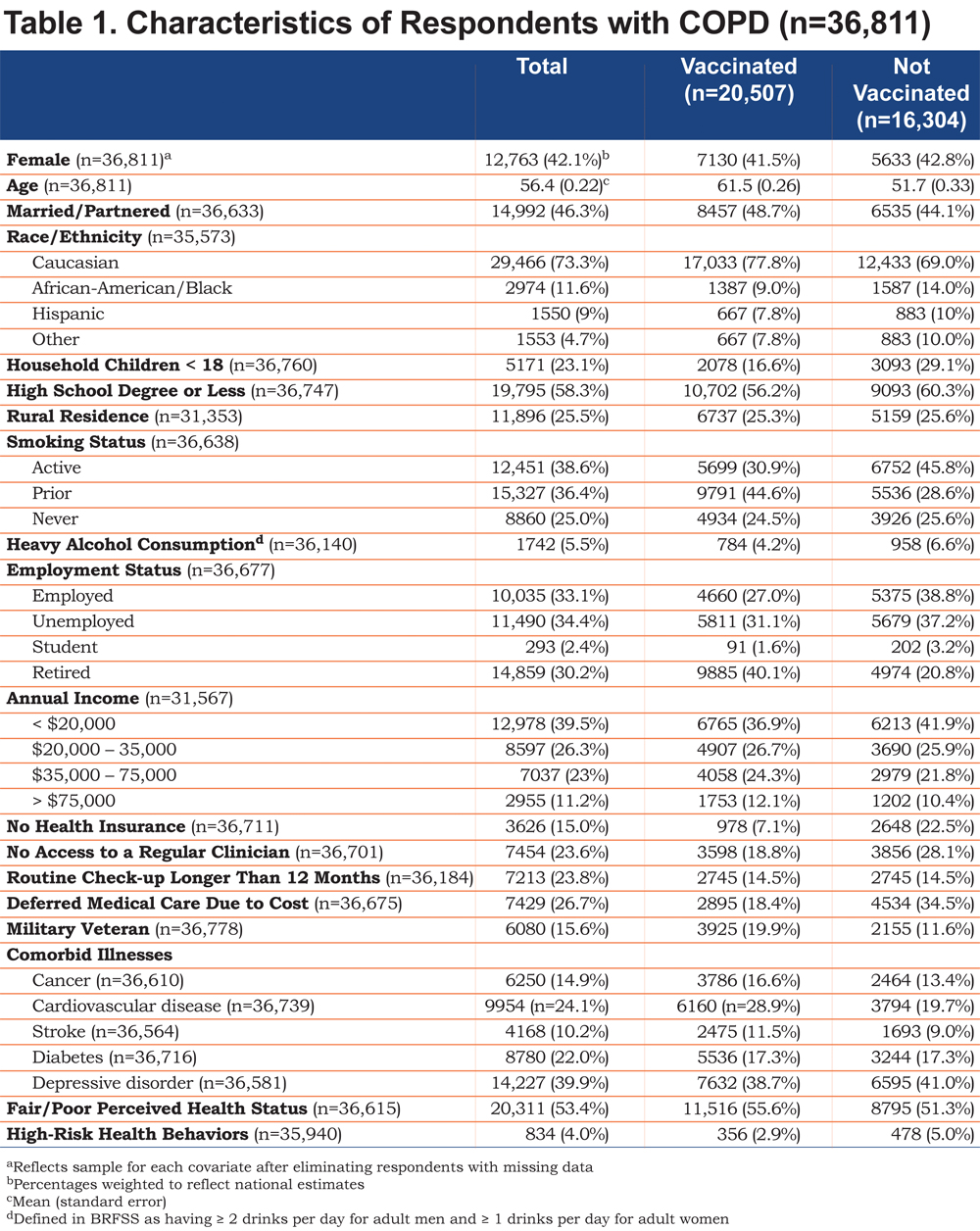
Overall, 48.5% (n=20,507) of COPD patients reported having been vaccinated, while 51.5% (n=16,304) were not vaccinated (Figure 1). The mean age of the study sample was 56.4 years, 42.1% were women, and 73.3% were white. We found that 23.1% of the sample with COPD reported having household children, and 46.3% reported being married or having a live-in partner. With regards to highest level of education and current income, 58% had a high school degree or less, and 39.5% had an income of less than $20,000. In terms of factors reflecting access to health care services, 15% of the COPD population did not have health insurance, 23.6% did not have access to a regular outpatient physician, 26.7% deferred care due to cost, and 23.8% had not had a routine check-up in the past year. National estimates of demographic and candidate variables of interest are presented in Table 1.
Predictors of Influenza Vaccination
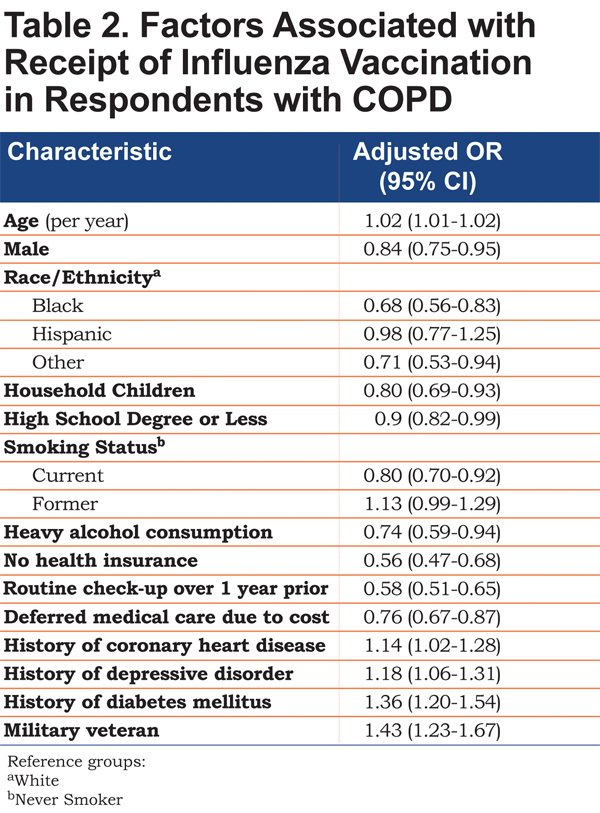
The results of the multivariate logistic regression analysis are presented in Table 2. We identified 15 factors independently associated with influenza vaccination in COPD patients. Predisposing factors associated with a lower likelihood of receiving an influenza vaccination included younger age, male sex, black or non-white/non-Hispanic/non-black race/ethnicity, a maximum educational level attained of a high-school degree or less, the presence of household children, current smoking, and heavy alcohol consumption. Enabling factors associated with lower likelihood of influenza vaccination include a lack of health insurance, deferring medical care due to cost, and not having had a routine check-up within the past 12 months. Need factors associated with higher likelihood of influenza vaccination include chronic comorbidities including coronary heart disease, depression, and diabetes. Additionally, veterans had a higher likelihood of influenza vaccination than non-veterans. After excluding rural location, income, and race/ethnicity from the model building process, there was no change in the independent predictors identified.
Discussion
In this analysis, we have identified important factors independently associated with receipt of influenza vaccination in persons with COPD. Barriers associated with lower likelihood of influenza vaccination included demographics, factors associated with access to health care, and unhealthy habits, while factors associated with increased likelihood of vaccination included chronic health conditions.
The results of this study extend prior literature on influenza vaccination by examining predictors of influenza vaccination in a previously unexamined at-risk group in the United States. Prior reports have identified similar deficiencies in influenza vaccination in smokers, older veterans, minorities, and individuals living in rural areas.16-19 We found some independent risk factors for not receiving influenza vaccination were similar to those previously reported. These included: younger age, black or non-white/non-black/non-Hispanic race/ethnicity, a lower educational level, access to health care (including lack of health insurance, not having had a routine check-up in the past 12 months, and an inability to afford routine care), active smoking, heavy alcohol consumption, and chronic comorbidities. In contrast, we did not find that rural residence, employment status, having a regular clinician or self-perceived overall health status were predictors of affirmative vaccination status.
The implications of our findings can be viewed in the context of the Anderson behavioral model and access to health care.10 Predictors of not receiving an influenza vaccination include predisposing factors (black or non-white/non-black/non-Hispanic race/ethnicity, younger age, male gender, household children, active smoking, heavy alcohol consumption, and a maximum education level of a high school degree or less) and enabling resources (lack of health insurance, not having a routine check-up in the past 12 months, and having deferred medical care due to cost), whereas need factors (chronic diseases including diabetes, depression, coronary heart disease) were associated with increased likelihood of influenza vaccination.
Within this framework, predisposing factors including age, race/ethnicity, family size, sex, active smoking, and heavy alcohol consumption can be used to target educational programs at specific at-risk sub-groups of COPD patients, which have proven effective in increasing vaccination uptake in older adults and minorities.20-22 Likewise, these results can aid in the design of provider-specific educational interventions by focusing efforts towards at-risk COPD groups, as prior studies have reported increased immunization rates with provider education programs.23 Additionally, enabling factors including a lack of health insurance, deferring health care due to cost, and not having had a check-up in the past 12 months reflect health care access, which can be viewed in the context of broader health policies on a state and national level. Interestingly, our findings suggest that, within the COPD population, only some enabling factors that reflect availability and access to health care (health insurance and ability to afford medical care) were associated with influenza vaccination, whereas provider availability (defined as having access to a regular clinician) was not.
The main strength of this analysis is the use of a large, nationally representative data set, as our results are generalizable to the COPD population in the United States. The present study also has several limitations. The BRFSS data relies on participant self-reporting, and is therefore subject to misclassification. That said, vaccination self-reporting in the BRFSS has been shown to be a reliable metric for vaccination status.9 Additionally, national prevalence estimates of COPD in the 2012 BRFSS survey (6.3%) is very similar to other accepted COPD prevalence estimates.24 Therefore, we feel confident that self-reporting of COPD and influenza in the BRFSS are representative metrics for this analysis. Any misclassification of other variables will be non-informative and thus bias towards the null.
Americans without landlines or cell phones are not eligible for study inclusion, which has the potential to introduce selection bias. The survey is conducted only in English or Spanish, further limiting eligible respondents. The use of weighted variables, however, incorporates factors for non-response, thus accounting for these factors. There was a negligible amount of missing data for a minority of pre-selected variables. Thus, these respondents were excluded from analysis, which is unlikely to affect the results. With rigorous statistical methods incorporating weighting and other advanced techniques, the BRFSS survey is a representative sample of the American adult population, allowing the results of this analysis to be generalizable to all adults living with COPD.
In summary, this is the first population-based study identifying predictors of influenza vaccination in COPD patients in the United States. This study identifies at risk-groups on whom vaccination programs can be focused in order to improve influenza vaccination rates in patients with COPD.
Acknowledgements
The authors acknowledge the methodological support and guidance of Ellen McCarthy, PhD.
Declaration of Interest
BRC has received research grants to his academic division from AstraZeneca, advisory board or consultancy payments from GlaxoSmithKline, Boehringer Ingelheim, Almirall, AstraZeneca, Takeda, and Novartis. Neither he nor any family members have shares or commercial interests in any company. DJH, CMN, and SKB report that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.