Running Head: Bullous Emphysema with Mycetoma
Abbreviations: Global initiative for chronic Obstructive Lung Disease, GOLD, chronic obstructive pulmonary disease, COPD; computed tomography, CT
Citation: Mutasa S. Images in COPD: Bullous emphysema with mycetoma. Chronic Obstr Pulm Dis. 2017; 4(2): 168-171. doi: http://doi.org/10.15326/jcopdf.4.2.2017.0144
Case Study: Severe Pulmonary Emphysema with Mycetoma Formation
A 65 year-old male presented for a double lung transplantation evaluation in August of 2013. There was a history of Global initiative for chronic Obstructive Lung Disease (GOLD)1 stage IV chronic obstructive pulmonary disease (COPD) with severe emphysematous changes on a regimen that included 0-2 liters of oxygen via nasal cannula initially. Further history included moderate pulmonary hypertension, New York Heart Association Class III2 congestive heart failure and an episode of mycobacterium avium complex that was successfully treated 3 years prior to the initial visit with us. The patient underwent a pre-transplant workup and returned for follow up in December 2013 with new complaints of worsening dyspnea on exertion and an occasional cough with productive sputum. His oxygen requirements increased to 2 liters by nasal cannula. At that time a decision was reached not to list the patient for transplant and a 6-month follow up with further imaging was scheduled.
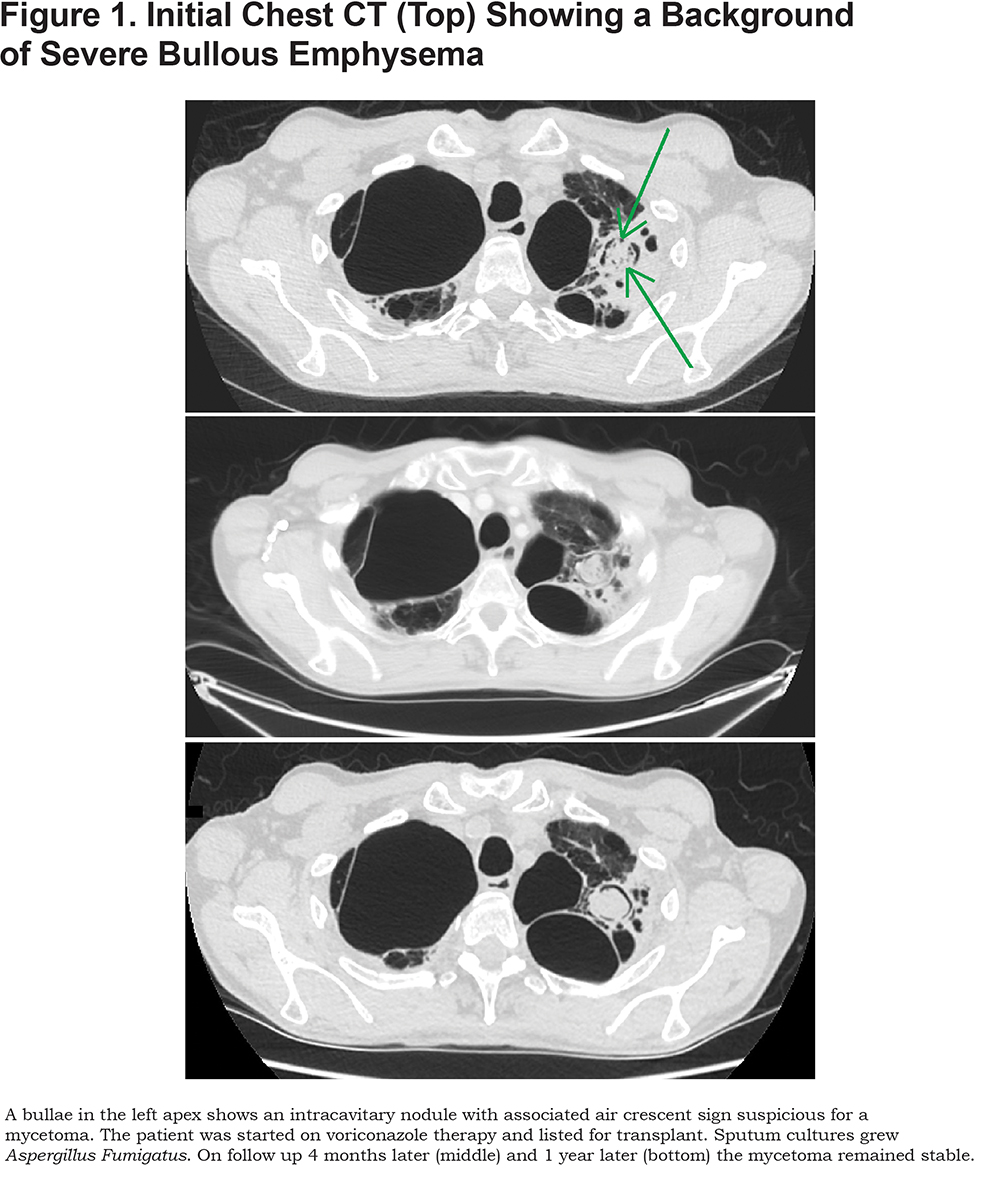
The patient returned in June 2014 with worsening shortness of breath. He remained on 2 liters of oxygen via nasal cannula. Lab results revealed a decline in pulmonary function testing and increased dyspnea after a 6- minute walk test. Chest computed tomography (CT) revealed a left apical bullae with a new spherical lesion, consistent with a mycetoma (Figure 1). The patient was listed for lung transplant and was started on a course of Voriconazole to be completed 14 days after transplant. Sputum cultures later returned positive for Aspergillus Fumigatus.
On continuing follow up over the next 2 years, while awaiting transplant, the patient remained on Voriconazole. He continued to have gradually worsening dyspnea on exertion with increasing oxygen requirements up to 4 liters per day. He underwent hospitalization for a COPD exacerbation requiring steroids and antibiotics in July 2015, after which he required 6 liters of oxygen per day.
The patient underwent double lung transplantation in January 2017. His post-transplant course was complicated by hypercapnic respiratory failure, renal failure and bilateral diaphragmatic paralysis.
Discussion3-8
Infection by Aspergillus fungus can be classified into several clinically distinct syndromes. One type of chronic infection leads to the formation of an aspergilloma. An aspergilloma is a fungus ball composed of the Aspergillus hyphae, mucus, cellular debris and fibrin. They tend to arise in patients with pre-existing pulmonary cavities that have become colonized with Aspergillus, such as those from tuberculosis, sarcoidosis or bullous emphysema. Almost all cases of chronic pulmonary aspergillosis are caused by Aspergillus Fumigatus.
A single, cavitary aspergilloma is usually stable over the course of months and years. Patients will usually have very minor symptoms, such as a mild cough, and little evidence of systemic inflammation. When symptoms progress, patients may present with weight loss, productive cough, fatigue and shortness of breath. Fever and night sweats may occur occasionally.
Radiographs in patients with an aspergilloma will typically reveal one or more cavities, particularly within the upper lobes which may contain one or more fungus balls. The radiographic appearance remains stable over months and such nodules have been noted to be moderately to strongly positive on positron emission tomography. Acute or subacute invasive pulmonary aspergillosis may form cavitary lesions, however they tend to enlarge over the course of several months. Serial imaging is useful for following the progression of disease and evaluating the response to therapy.
Treatment for aspergillomas is individualized based on patient symptomatology, progression of disease and the existence of comorbidities. Surgical resection is usually recommended for symptomatic patients including those with hemoptysis. Symptomatic patients who are unable to undergo surgery are treated with voriconazole or itraconazole for a minimum of 6 months.
Our case highlights a case of chronic aspergilloma infection in a patient with bullous emphysema and management leading up to transplant.
To submit manuscripts for consideration for publication as an “Images in COPD” article, contact: Robert M. Steiner, MD at rs3674@cumc.columbia.edu
1. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of COPD. GOLD website. http://www.goldcopd.org. Published 2016. Accessed January 2017.
2. New York Heart Association (NYHA). Classes of heart failure-NYHA Functional Classification. NYHA website. http://www.heart.org/HEARTORG/Conditions/HeartFailure/AboutHeartFailure/Classes-of-Heart-Failure_UCM_306328_Article.jsp#.WN8RO_nys2w Published 2015. Accessed February 2017.
3. Judson MA, Stevens DA. The treatment of pulmonary aspergilloma. Curr Opin Investig Drugs. 2001; 2(10):1375-1377.
4. Denning DW, Riniotis K, Dobrashian R, Sambatakou H. Chronic cavitary and fibrosing pulmonary and pleural aspergillosis: case series, proposed nomenclature change, and review. Clin Infect Dis. 2003; 37(Suppl 3): S265-S280. doi: https://doi.org/10.1086/376526
5. Baxter CG, Bishop P, Low SE, Baiden-Amissah K, Deming DW. Pulmonary aspergillosis: an alternative diagnosis to lung cancer after positive [18F] FDG positron emission tomography. Thorax. 2011; 66 (7): 638-640. doi: https://doi.org/10.1136/thx.2010.155515
6. Denning DW, Cadranel J, Beigelman-Aubry C, et al. Chronic pulmonary aspergillosis: rationale and clinical guidelines for diagnosis and management. Eur Respir J. 2015; 47(1):45-68.
7. Roberts C M, Citron KM, Strickland B. Intrathoracic aspergilloma: Role of CT in diagnosis and treatment. Radiology. 1987;165(1): 123-128. doi: https://doi.org/10.1148/radiology.165.1.3628758
8. Desai SR, Hdeayati V, Patel K, Hansell DM.Chronic aspergillosis of the lungs: Unravelling the terminology and radiology. Eur Radiology. 2015; 25(10): 3100-3107. doi: https://doi.org/10.1007/s00330-015-3690-7