Running Head: Serum Proteins with Emphysema in Alpha-1
Funding Support: The QUANTUM-1 Study was supported by the National Heart Lung and Blood Institute, the Office of Rare Diseases through the Rare Lung Disease Clinical Research Network (1 U54 RR019498-01, Trapnell PI), and the Alpha-1 Foundation. The protein analysis was performed by a grant from the Chest Foundation (Beiko, PI).
Date of Acceptance: April 5, 2017
Abbreviations: alpha-1 antitrypsin deficiency, AATD; chronic obstructive pulmonary disease, COPD; protease inhibitor ZZ, PiZZ; protease inhibitor SZ, PiSZ; forced expiratory volume in 1 second, FEV1; computed tomography, CT; -post-bronchodilator, post-BD; National Health and Nutrition Examination Survey III, NHANES III; QUANTitative lung CT UnMasking emphysema progression in AATD, QUANTUM-1; diffusing capacity of the lung for carbon monoxide, DLCO; total lung capacity, TLC; percentile density at 15%, PD15; false discovery rate, FDR; body mass index, BMI; forced vital capacity, FVC; Hounsfield units, HU;C-reactive protein, CRP;adipocyte fatty acid-binding protein, AFBP; tissue plasminogen activator, tPA; wingless-related integration, WNT; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints, ECLIPSE
Citation: Beiko T, Janech MG, Alekseyenko AV, et al; for QUANTUM-1 Investigators. Serum proteins associated with emphysema progression in severe alpha-1 antitrypsin deficiency. Chronic Obstr Pulm Dis. 2017; 4(3): 204-216. doi: http://doi.org/10.15326/jcopdf.4.3.2016.0180
Introduction
Alpha-1 antitrypsin deficiency (AATD) predisposes individuals to early chronic obstructive pulmonary disease (COPD). COPD is one of the leading causes of medical hospitalizations and the third leading cause of death worldwide.1 AATD individuals experience even more hospital visits and cost more to the health care system compared to the older and more comorbid cohort of patients with usual COPD.2 The search for biomarkers that inform future clinical events is important. Unfortunately, only a few existing therapies (e.g., smoking cessation and oxygen therapy for hypoxemic individuals) reduce mortality or modify the natural history of disease. In addition, few novel drugs with systemic action are currently in clinical trials. Among the many problems with COPD drug development is the slow progression of disease in the majority of affected individuals. In addition, the many clinical phenotypes of disease complicate a comprehensive disease understanding.
AATD is the most common known genetic cause of COPD3 that affects at least 100,000 Americans and over 3 million individuals worldwide. The blood level of alpha-1 antitrypsin is determined by each of the inherited alleles on SERPINA1, the gene that codes for alpha-1 antitrypsin. Various genotypes exist with the largest burden of disease ascribed to protease inhibitor ZZ (PiZZ) and protease inhibitor SZ (PiSZ).
Individuals with AATD present at an earlier age and have more rapid disease progression than individuals with usual COPD.4 AATD individuals are at increased risk for developing COPD compared to the general population, especially when tobacco or environmental exposures exist, causing disease at younger age. Additionally, individuals with AATD have an emphysema-predominant phenotype that is more homogeneous than usual COPD. Intravenous alpha-1 antitrypsin, known as augmentation therapy, is currently approved by regulatory authorities for AATD individuals with forced expiratory volume in 1 second (FEV1) in the range of 30%-65% predicted.5 Observational studies have noted excess mortality in AATD and have shown a survival benefit in selected subgroups of individuals receiving augmentation therapy.6,7 We hypothesized that biomarkers may characterize AATD individuals with rapid progression of emphysema, thereby creating the possibility of new, targeted therapy.
Most traditional biomarkers of COPD severity and progression have been related to lung function decline, measured as FEV1.8,9 Chest radiography is not sensitive enough to detect early emphysema. Computed tomography (CT) of the chest can reveal early emphysematous changes that are sometimes present in individuals with normal lung function who are minimally symptomatic. Emphysema is usually detected earlier in life and in a higher proportion of AATD affected individuals compared to individuals with usual COPD.
CT lung density has been utilized as a promising biomarker in AATD.10 In a mixed cohort of both usual COPD and AATD-associated COPD, assessment of emphysema progression was more sensitive by lung densitometry than FEV1 and measurements of gas transfer.11 For this reason, CT density has been allowed as a primary endpoint in trials of augmentation therapy efficacy by U.S. and European regulatory authorities.5 Desmosine is the most promising biomarker in AATD-related COPD,12 although several others have been evaluated, including fibrinogen,13 matrix-metalloprotease-9,14,15 and angiopoietin-like protein 4.16
In 2008, the National Institutes of Health Office of Rare Diseases and the National Heart, Lung, and Blood Institute funded the Rare Lung Disease Consortium to study radiographic emphysema decline in a cohort of PiZZ AATD individuals with normal lung function as defined by post-bronchodilator (post-BD) FEV1% predicted ≥ 80% per the National Health and Nutrition Examination Survey III (NHANES III).17 The primary hypothesis of the study, called QUANTitative lung CT UnMasking emphysema progression in AATD (QUANTUM-1), was to determine whether baseline CT density predicted a more rapid decline in FEV1. Because the large biorepository of this carefully phenotyped cohort is available for additional projects, we analyzed this cohort to identify serum proteins that correlate with CT density decline in individuals with early stage AATD-associated COPD.
Methods
Study Design and Population
The 49 participants in QUANTUM-1 were enrolled between September 9, 2007 and December 11, 2008 following informed consent at 1 of 7 participating U.S. study centers and followed for 3 years. All participants had normal lung function at baseline as defined by post-bronchodilator FEV1% predicted ≥ 80% per the NHANES III.17 Baseline demographics are included in Table 1. No participant smoked during the time of biospecimen collection. At each visit, absence of significant smoke exposure was confirmed in all individuals by urinary cotinine. Participants had bimonthly telephone calls to assess exacerbations and serial site visits (at baseline, 6, 12, 18, 24, and 36 months) with chest CT, pulmonary function tests (spirometry, lung volumes, and diffusing capacity of the lung for carbon monoxide (DLCO) tests, and serum collection to explore the natural history of disease progression over the course of 3 years. Although the protocol specified 50 individuals, funding ended once 49 participants were enrolled.
The annual changes in FEV1 were calculated utilizing baseline, 6, 12, 18, 24, and 36-month visits. The PD15/TLC slope was calculated by endpoint analysis (36 months-baseline) based on acceptability of the CT scans for analysis. The exacerbation frequency for the year preceding the study was assessed at the baseline site visit using the AlphaNet exacerbation questionnaire.18 This AATD-specific questionnaire was developed to address exacerbation type and frequency by a variety of exacerbation definitions and has been used in large cohorts of AATD individuals who receive augmentation therapy through AlphaNet.
Contiguous non-overlapping 0.6-1.0mm slice thickness multi-detector row CT scans were acquired at 80 mAs, 120 kVp. Images were reconstructed using a medium spatial frequency reconstruction algorithm (GE: Standard, Philips: B, Siemens: B30f, Toshiba: FC86). A Gammex phantom was used to assure the accuracy of each CT scanner in the study at 6-month intervals.
We included all participants with acceptable baseline and 36-month CT scans that could be analyzed using Apollo image analysis software (VIDA Diagnostics, Inc.). Briefly, the lungs were segmented in 3-dimensions from the chest wall and mediastinal components using Apollo. The CT-derived total lung capacity (TLC), mean lung density and the lowest percentile density at 15% (PD15) corrected for lung volume was derived from all air density voxels. Of the original cohort of 49 participants, 7 had missing data, and 11 had CT scans that did not follow the specific acquisition protocol. Thirty-one individuals remained eligible for analyses.
Blood Samples
A total of 50 ml of blood was drawn at the initial study visit for serum and plasma analysis. Serum samples were allowed to clot for 15 minutes per protocol, spun at 3500 rpm, and placed into a -80° C freezer until transported on dry ice to the central repository. Serum samples were stored at the University of Florida Alpha-1 Genetics Laboratory or at the Medical University of South Carolina Alpha-1 Registry at -80° C until analyzed.
Primary Outcome Measures
We measured 317 proteins from serum obtained at the baseline visit using a multiplexed immunoassay (Myriad Discovery MAP® panel) in the 31 study individuals with a complete dataset. Values were expressed as mean ± standard deviation. We analyzed the associations between baseline PD15/TLC, PD15/TLC annual decline, and baseline protein levels using Pearson’s product moment correlation. A p-value < 0.05 was considered statistically significant. Correlations were determined to be weak, moderate, or high when the r coefficient was in the range 0.2-0.39, 0.4-0.59, or 0.6-0.79, respectively. The two-tailed correlations were then adjusted for age, and sex. To reduce false positives due to multiple comparisons, we have further adjusted the raw p-values for a global false discovery rate (FDR) of less than 10%.19 This method adjusts up the significant values for individual proteins to ensure that the expected number of false positives among positive results is no more than 10%, which is a common practice in high-throughput data analysis.
Pathway analysis of proteins correlated with PD15/TLC and/or its slope was performed using the UniProt number and Homo sapiens Reactome pathway analysis software.20
Results
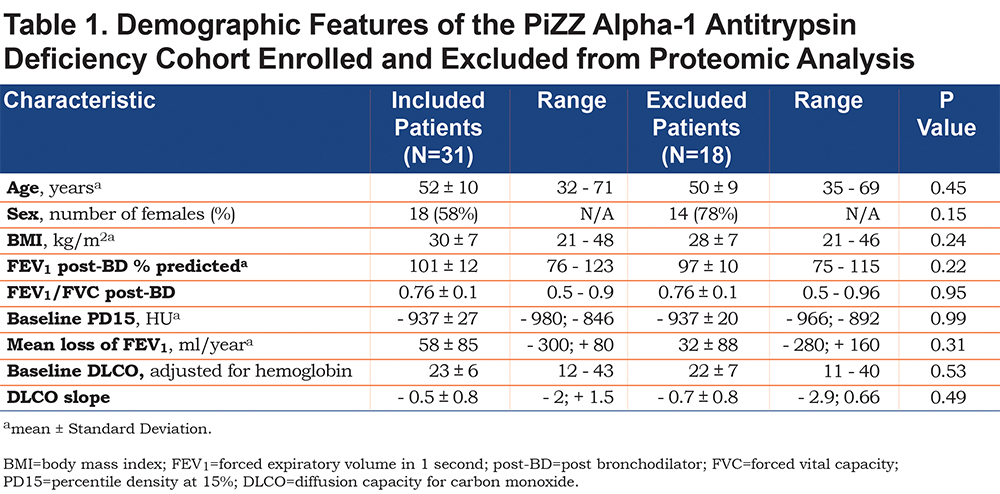
The 31 eligible PiZZ participants had a mean age of 52 ± 10 years, a body mass index (BMI) of 30 ± 7 kg/m2 (39% had BMI in the obese range), FEV1/ forced vital capacity (FVC) post-BD of 0.76 ± 0.1, post-BD FEV1 of 101 ± 12% predicted, baseline DLCO adjusted for hemoglobin 23 ± 6, and baseline PD15 of -937 ± 27 Hounsfield units (HU). A slight majority of participants were women (58%). No differences in baseline characteristics between the 31 included and the 18 excluded participants were found (Table 1). There were changes in radiographic and spirometric measurements over the 3-year study course, verifying progression of emphysema. Annual changes included a decline of FEV1 of 58 ± 85 ml/year, decline of PD15 of 4 ± 13HU/year, increase of CT volume (CT TLC) of 80 ± 371 ml/year, decrease of PD15/ CT TLC of 0.75 ± 4.4 HU/ml/year, decline in DLCO of 0.5 ± 0.8, and rise in post-bronchodilator TLC measured by lung volumes of 212 ± 600 ml.
Exacerbation questionnaires at the baseline visit revealed that 47% of individuals had at least one exacerbation in the preceding year. However, over the 3 years of observation, only 51% had one or more events. A bivariate analysis of FEV1 slope and PD15 slope adjusted for TLC in 31 individuals confirmed a significant association between spirometry and CT measures. However, adjustment for age and sex, extinguished the significant correlation between FEV1 decline and emphysema progression (p=0.21 after adjustment). Baseline emphysema showed wide variation among participants at baseline. All but 5 individuals had emphysema present, as defined by PD15 ≤ -910 HU, with a range of PD15 of -966 HU to -892 HU. Three of 5 participants with no emphysema by this definition were extremely obese (BMI>39), potentially affecting PD15 measurements.
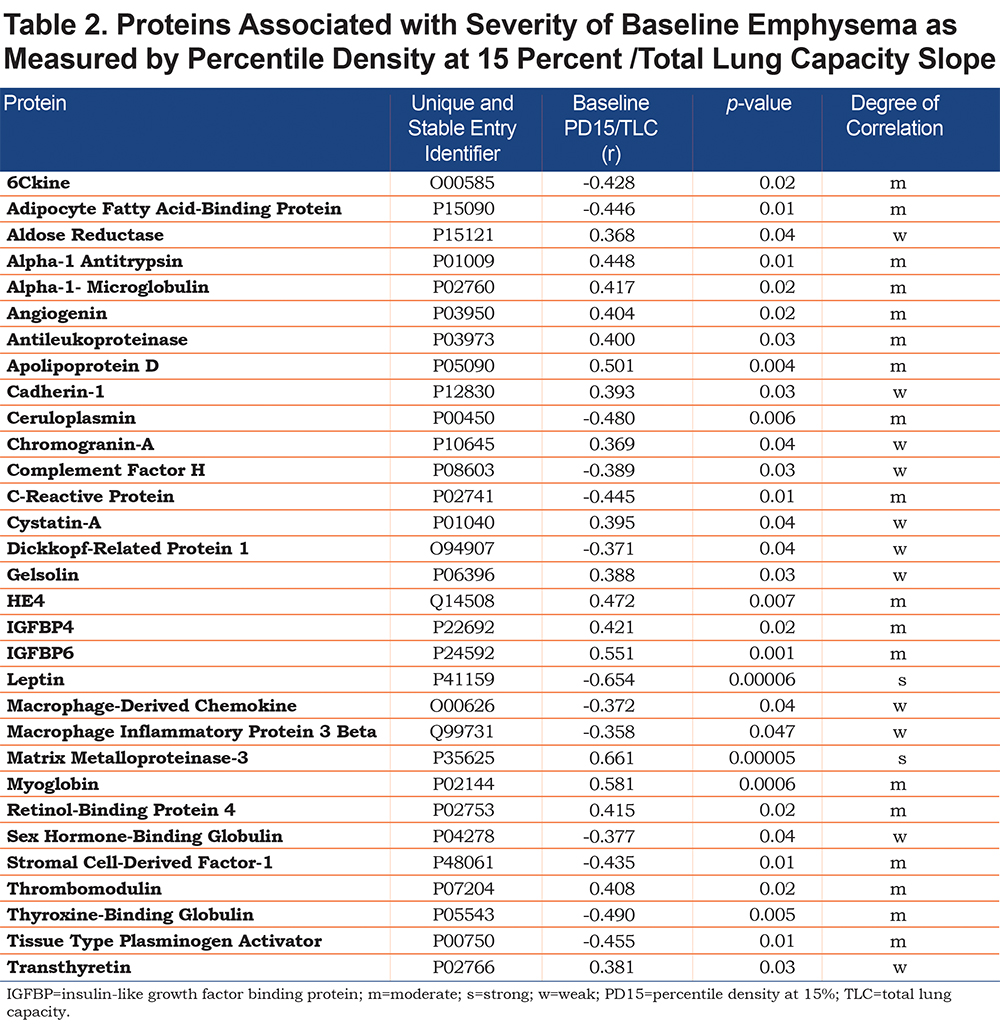
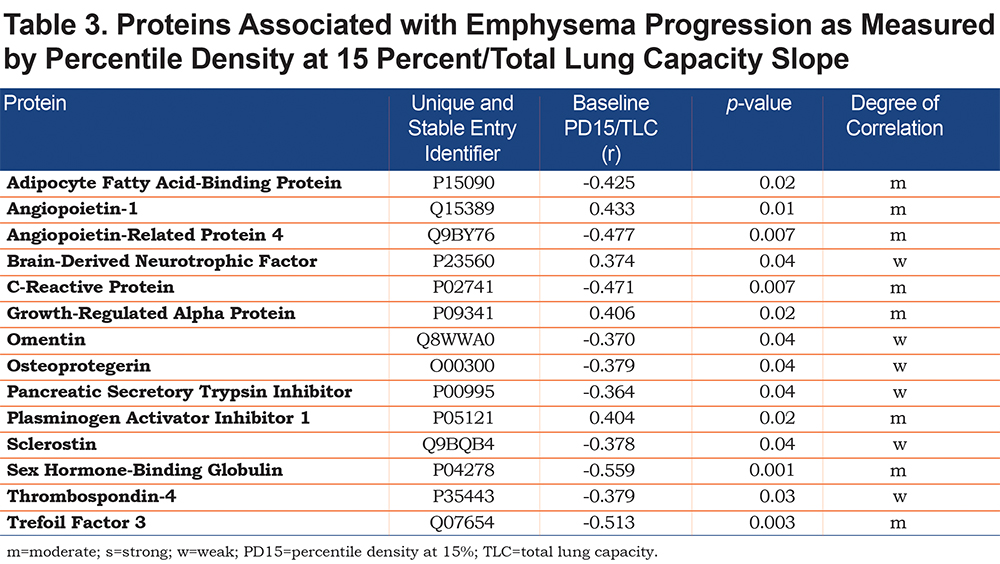
From the 317 proteins evaluated, 31 were associated with baseline emphysema (Table 2) and 14 were associated with emphysema progression (Table 3) when unadjusted for age, sex, and multiple comparisons. Most of these proteins showed a moderate degree of correlation as measured by Pearson product moment correlation. In unadjusted analyses, 3 proteins (C-reactive protein [CRP], adipocyte fatty acid binding protein [AFBP], and sex hormone-binding globulin) were associated with both baseline emphysema and emphysema progression as measured by the PD15/TLC and PD15/TLC slope, respectively (Table 4). Angiopoietin-related protein 4 showed a moderate correlation (r=-0.477, p=0.007) with emphysema progression. CRP and AFBP correlated strongly with BMI.
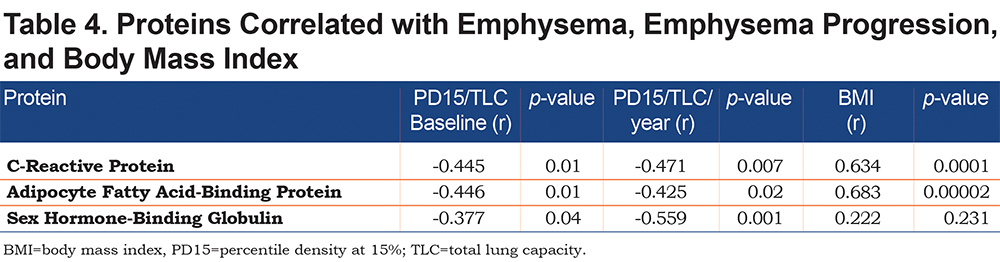
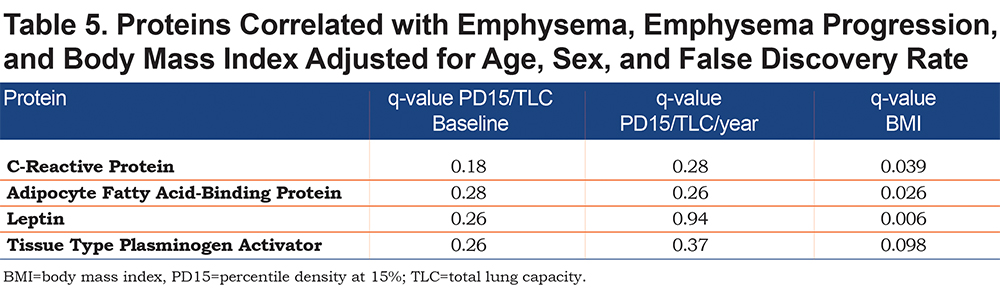
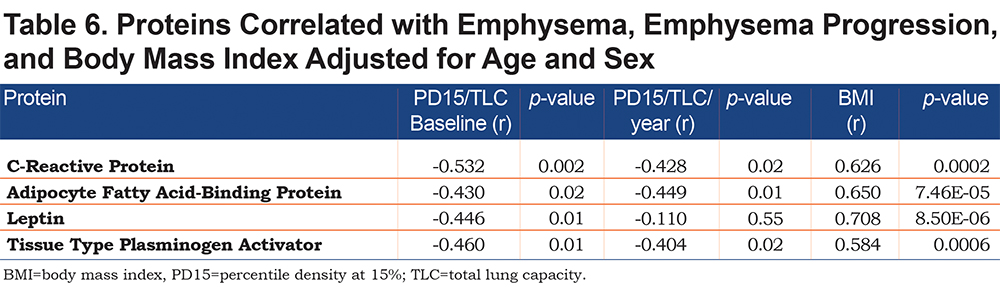
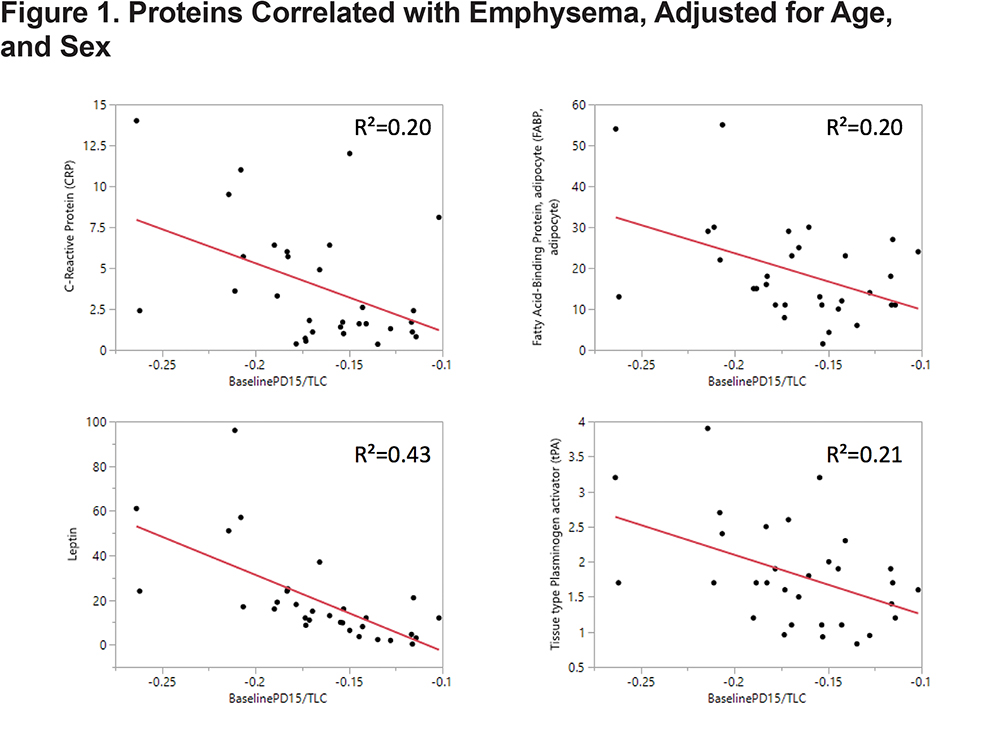
CRP, AFBP, leptin, and tissue plasminogen activator (tPA) were found to be significantly associated with BMI after controlling for multiple comparisons at global FDR < 10% and adjusting for age and sex (Table 5). If these proteins were not adjusted for multiple comparisons, all 4 were statistically significantly associated with baseline emphysema and all but leptin were associated with emphysema progression after adjustments were made for age and sex (Table 6 and Figure 1). In summary, the adjustment for multiple comparisons caused the strength of the associations of CT-measured emphysema with biomarkers to lessen such that none correlated with CT measures of emphysema (q value range 0.18-0.94).
Discussion
In individuals with rare diseases such as AATD, large, prospective, controlled, clinical trials are difficult to perform. Therefore, characterizing the correlation between biomarkers and important clinical features is of paramount importance, as the availability of reliable biomarkers might limit the size of required clinical trials and inform emphysema research about biologically relevant pathways.
Baseline PD15 values in our cohort (N=47) were -937 ± 25 HU, which is abnormal even in comparison to smoking participants with normal gas trapping.21
In individuals with AATD and preserved lung function, our unadjusted analysis showed that of 317 proteins assessed, 31 proteins were associated with baseline emphysema extent and 14 proteins were correlated with its progression. Only 3 of these 42 proteins correlated both with baseline emphysema extent and its progression: CRP, AFBP, and sex hormone-binding globulin. These 3 proteins are not related in pathway analysis; however, each has a previously described connection to emphysema.22-26
One of the important questions in the field of COPD and emphysema is whether the longitudinal change in FEV1 correlates with the emphysema progression measured by PD15 utilizing CT. In our cohort of 31 individuals followed for 3 years we found no association between decline in spirometry and CT emphysema measures in analyses adjusted for age and sex. More importantly, once corrected for age, sex, and multiple comparisons, striking associations between CT features and CRP, AFBP, leptin, and tPA with BMI were found. This finding is significant as we previously found that obesity (BMI>30) was associated with more exacerbations in this cohort of individuals.23 Exacerbations are important patient-reported outcomes and are known to negatively affect COPD individuals and portend poor prognosis.24 Our study lacked sufficient power for formal statistical pathway analysis. However, proteins correlated with PD15/TLC or its slope were often interrelated with broad connections to known pathways of emphysema pathogenesis. These involved complement activation, retinoic acid transport, wingless-related integration site (WNT) signaling, pathways of hemostasis, and chemokine production. As discussed below, some of the pathways involved in metabolism of lipids and lipoproteins were also overexpressed.
CRP has been proposed as a biomarker for COPD because of clinical associations with FEV1, exacerbations, comorbidities, hospitalization risk, and mortality.22-24 Biochemically, CRP promotes complement fixation and may scavenge nuclear material from damaged circulating cells. In addition, CRP has several functions associated with host defense. The complement cascade is critical in connecting the innate and adaptive immune response and has been studied in COPD.25 Because CRP has been extensively studied in cardiac disease as a risk factor biomarker, the lack of specificity for emphysema will be an issue in further advancing this observation toward the clinic.
AFBP is a lipid transport protein in adipocytes which binds both long-chain fatty acids and retinoic acid. Given the long history of interest in retinoic acid therapy and alveolar growth, the association with rate of emphysema progression is interesting.
TPA plays an important role in tissue remodeling and degradation, by converting plasminogen to plasmin. Prior research confirms that the tPA levels are predictive of cardiovascular events26 and recent publications reveal the potential of fibrinolytic agents as treatments for chronic respiratory diseases.27
Also, earlier analyses revealed that exacerbation frequency is increased in obese individuals with AATD.23 In this exploratory analysis, we found that some proteins had very strong correlations with BMI (CRP and AFBP). This association is not surprising as some view obesity as a chronic inflammatory state that further perpetuates many chronic diseases. In a clinical context, the prevalence of obesity is disproportionately high in individuals with COPD28 and the cause and consequences of this association remains speculative. To date, studies investigating the impact of obesity on mortality in COPD individuals suggest that obesity is associated with a 30%-34% increase in relative risk of all-cause mortality in individuals with mild or moderate COPD compared to individuals with normal weight and comparable disease severity.29 How much of the associated mortality from high BMI is from COPD comorbidities and how much may be from an impact on emphysema progression remains unknown. Recent analysis of the Behavioral Risk Factor Surveillance System data collected by the Centers for Disease Control and Prevention confirmed that comorbidities are commonly present in COPD individuals.30
Body composition abnormalities with higher measurements of adiposity are related to greater functional limitations, particularly in women.31 One of the reasons that obesity may be associated with worse outcomes in COPD may relate to systemic inflammation.32 In the Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) cohort, patients exhibiting high circulating levels of 6 inflammatory biomarkers had worse health outcomes and were more obese compared to non-inflamed individuals.33 In our study, metabolism of lipids and lipoproteins were implicated by finding different expression of adipocyte fatty acid-binding protein, aldose reductase, and angiopoietin-related protein 4. Angiopoietin-related protein 4 plays a role in several plausible AATD-associated COPD pathways34 involving inflammation, lipid metabolism, and metabolic dysregulation. Therefore, linkage between lipid transport and systemic inflammation in COPD 35 is supported by these observations in the well-phenotyped QUANTUM-1 cohort of AATD individuals.
Sex hormone-binding globulin was also associated with emphysema and its progression, although the degree of correlation was smaller. This molecule has been associated with androgen binding and could participate in emphysema pathogenesis by altering the clearance rate of steroid hormones. We are unaware of other pathway associations for COPD.
The other 39 proteins that were associated with either baseline emphysema extent or emphysema progression play roles in many pathways that have been previously implicated in emphysema pathogenesis. Associations with programmed cell death showed activity for apoptotic signaling that has been well studied in emphysema.36 We also found strong signals for retinoic acid transport. Although clinical trials of all-trans retinoic acid have proved negative37 the retinoid cycle has been implicated in COPD pathogenesis. In this context, 2 proteins in our analysis regarded the retinoid cycle: retinol-binding protein 4 and transthyretin, both with significant correlations to baseline emphysema (of moderate and strong degrees).
Very little is known about the types of inflammatory events and their initiation, especially in early onset emphysema. In this regard, our finding that some chemokine receptors and chemokines were associated with emphysema extent raises the possibility that they contribute to the pathogenesis of emphysema. The associated proteins in this study include 6Ckine, stromal cell-derived factor-1, macrophage inflammatory protein 3 beta, growth-regulated alpha protein, and macrophage-derived chemokine.
Linkages to autoimmunity have been studied extensively in clinical and experimental COPD.38 Proteins involved in WNT signaling (sclerostin and dickkopf-related protein 1) were moderately expressed, as was metalloproteinase 3, a metalloproteinase previously identified to play a role in AATD-related emphysema.39
The hemostatic protein fibrinogen is the first serum biomarker validated in the COPD Biomarkers Qualification Consortium40 and has known involvement in hemostatic pathways.41 Fibrinogen reflects both COPD severity and progression by association with adverse clinical outcomes (e.g., exacerbation, hospitalization, and mortality) and is now a drug development tool in COPD. We saw significant upregulation (negative correlation with PD15/TLC) for tissue type plasminogen activator and downregulation of its inhibitor plasminogen activator inhibitor 1, signaling a pro-thrombotic state associated with emphysema.
This study has several limitations. First, the sample size was small and included only 31 individuals of the 49 participants originally enrolled in the study. The fact that included participants did not differ from excluded participants regarding demographic features lessens concerns about selection bias. Second, the associations reported were based on single measurements but not serial measures. Furthermore, the extent of inter-individual and intra-individual variation in the biomarker protein measurements in COPD patients is currently unclear. Few exacerbations were seen over the 3 years of the study, limiting correlations with this clinical outcome. Obesity with BMI >40 was present in 4 of 31 individuals and can impact CT density independent of chest restriction by radiation scatter. As such, though our findings are provocative and novel, their validity and generalizability will require replication in other cohorts.
Variation in CT measurement of lung volumes posed a challenge in this study, as it has characteristically in other studies of individuals with AATD.5 Our study used state-of-the-art techniques to control CT acquisition, which have not materially advanced since 2008 when the images in this study were obtained. Although new methodologies that allow registration of the same segments during inspiration and expiration to differentiate between small airways disease and emphysema are available, these were not used in this study as they have not been fully validated.42
Projects designed for discovery of novel biologic pathways that impact clinical disease are high risk with the hope of high reward. The challenge with rare disease cohorts such as AATD is that validation cohorts are limited and data are costly to acquire. Recognizing that validation of these findings is needed before routine use of these biomarkers in clinical trials can be endorsed, our findings are novel and, we believe, promising.
Conclusions
Prior publications confirm that PiZZ AATD individuals are at increased risk for developing COPD compared to the normal population and typically develop emphysema at a younger age, especially if exposed to tobacco smoke. We have shown that baseline CT density varies widely in the QUANTUM-1 cohort, which includes individuals with advanced emphysema despite normal lung function tests and some individuals with normal lung density as measured by densitometry. In addition, these preliminary data suggest that, at baseline, there is poor correlation between the rate of FEV1 decline and the radiographic presence of emphysema.
In this cohort of AATD individuals, leptin, CRP, AFBP, and tPA were associated with baseline emphysema and all but leptin were associated with emphysema progression after controlling for age and sex. Strong correlations of these proteins with BMI were also found after adjustments for multiple comparisons were made.
While analysis of CRP and leptin in COPD is ongoing,22,43,44 the observation regarding AFBP may prompt investigation regarding the regulation of systemic glucose and lipid metabolism in the pathogenesis of COPD. Similarly, more research investigating plasminogen activation in COPD is needed. Such investigations could suggest promising targets for COPD therapy.
Acknowledgements
The original 2008 QUANTUM-1 Investigators of the Rare Lung Disease Consortium:
National Institutes of Health Rare Lung Diseases Consortium Sponsor: Former Office of Rare Disease Research--Director, Steve Groft, PharmD (retired). Administered by: former National Center for Research Resources--Director, Barbara Alving, MD(retired), Elaine Collier, MD, Carl Hunt, MD; Data Management and Monitoring Center: University of South Florida--Director, Jeffrey Krischer; Rare Lung Diseases Consortium Leadership: Director, Bruce Trapnell, MD Co‐director, Frank McCormack, MD, DSMB Chair, Robert Senior, MD; Data Management Coordinating Center, Pediatrics Epidemiology Center: University of South Florida, Principal Investigator: Jeffrey Krischer, PhD, Personnel: M. Abbondondolo, F. Badias, M. Colouris, D. Cuthbertson, K. Grant, H. Lee, K. Paulus; Brigham and Women's Hospital, Harvard Medical School: Principal Investigator, Edwin K. Silverman, MD, PhD; Personnel: F. .Jacobson, MD, D. DeMeo, MD, L. Kaufman, J. Medeiros, E. Schwinder; Cleveland Clinic Foundation: Principal Investigator, James K. Stoller, MD, MS; Personnel: D. Faile, M. Meziane, MD; University of Cincinnati/Cincinnati Children's Hospital Medical Center: Principal Investigators, Bruce Trapnell, MD, and Frank McCormack, MD; Personnel: W. Blower, A. Brody, D. Lagory, R. McKay, B. Kinder, C. Meyer, T. Roads, M. Stamper, L. Young, W. Zhang. Translational Research Trials Office Personnel: J. Bailey, J. Dahlquist, R. Dosani, M. Hodgson, P. Kaiser, L. Korbee, M. Kuhlmann, S. McMahan, E. Turner, S. Uber; Medical University of South Carolina: Principal Investigator, Charlie Strange, MD; Personnel: Tatsiana Beiko, MD; James Ravenel, MD; A. Finley, S. Kumbhare, M. Kokosi, D. Woodford; National Jewish Health: Principal Investigator, Robert A. Sandhaus, MD, PhD; Personnel: K. Brown, G. Cosgrove, G. Downey, S. Frankel, J. Swigris, D. Kervitsky, M. Morrison, E. Perez, J. Schroeder; Oregon Health and Science University: Principal Investigator, Alan Barker, MD; Personnel: K. Kennie, S. Primack; University of Florida: Principal Investigator: Mark Brantly, MD; Personnel: L. Gilbert, P. Schreck, A. Leong, F. Rouhani; QUANTUM-1 Core Radiologists: Cincinnati—Cristopher Meyer, MD, and Alan Brody, MD; Vancouver--Harvey Coxson, PhD; QUANTUM-1 Statistician: Hye‐Seung Lee, PhD; Alpha-1 Foundation: Adam Wanner, MD
Declaration of Interest
TB has received grants from the CHEST Foundation and the Alpha-1 Foundation. MGJ, AVA and CA have nothing to declare. HOC reports grants from Spiration Inc., and personal fees from Samsung, outside of the submitted work. JLB, SES, CLW, LMS, AB, MB, RAS and EKS have nothing to declare. JKS is a consultant to: Grifols, Shire, CSL Behring, Arrowhead Pharmaceuticals and reports research funding from the National Institutes of Health, the Alpha-1 Foundation, and CSL Behring. He is also a member of the Board of Directors of the Alpha-1 Foundation and a member of the Medical and Scientific Advisory Committees of the Alpha-1 Foundation and the COPD Foundation. BT has nothing to declare. CS has grants with Adverum, the Alpha-1 Foundation, CSL Behring, Grifols, and Baxalta/Shire and has consulted for Grifols, Adverum and CSL Behring in alpha-1 antitrypsin deficiency and has an equity interest in Abeona.