Running Head: COPD10usa Abstracts
Funding support: The COPD10usa 2017 conference was supported by Boehringer Ingelheim, Mylan, Sunovion and Grifols pharmaceutical companies.
Citation: Yawn BP, Thomashow B. Abstract presentations: COPD10usa 2017. Chronic Obstr Pulm Dis. 2017; 4(4): 305-319. doi: http://doi.org/10.15326/jcopdf.4.4.2017.0162
Introduction
The COPD10USA Conference was held in Chicago in July 2017, and was the fourth in the series of biennial conferences begun in collaboration with our partners from Birmingham, United Kingdom who have held similar conferences for over 20 years. Featuring a faculty of the nation’s top chronic obstructive pulmonary disease (COPD) experts across all groups-- physicians, researchers, patients and caregivers-- the conference provided opportunities for education, interaction, collaboration and guiding future research. The more than 500 attendees also represented the entire spectrum of individuals involved in the lives and care of people with COPD. A highlight of the program was discussion of the recently released National COPD Action Plan supported through the National Institutes of Health, and particularly the National Heart Lung and Blood Institute, and focusing on the steps needed to make the goals of that plan a reality for COPD care in the United States.
The conference’s sessions covered new and emerging COPD topics as well as bringing new perspectives to old issues. Drs. Meilan Han and George Washko discussed “Early COPD” presenting findings on people with symptoms but normal lung function and assessment of airway anatomy as a COPD precursor. Updates were presented on recently published clinical trials including SUMMIT, FLAME, COPDGene and LOTT. Our first pro/com debate from Stephanie Christenson, MD and Prescott Woodruff, MD, was a lively presentation on “Asthma, COPD and ACOS—Does it Matter”. Other topics included biomarkers and digital biomarkers, pulmonary rehabilitation and its widespread under use, the team approach to care and “COPD—A Changing Therapeutic Paradigm”. The conference ended with outstanding reviews of the Future of COPD Care:“Can we get there by translational medicine?” from Steve Rennard, MD; “Precision Medicine” by Avrum Spira, MD; and “Innovation” by Jean Wright, MD.
An evening tribute to John Walsh, COPD patient, advocate, spokesperson and driving force behind much of the national and international recognition and attention given to COPD was a joyous and moving celebration. John was co-founder of the COPD Foundation and is greatly missed but his leadership and guidance continues to push forward action surrounding COPD.
As in previous conferences, poster presentations were an important part of the conference and aimed at providing opportunities for younger researchers and those outside academic centers to present their important and innovative work. The following are the abstracts from those posters.
NOTE: The following abstracts have NOT been edited but are presented here in their original format, as presented by the authors at COPD10usa 2017.
Claims-Based Assessment of Inhaled Corticosteroid (ICS) Use in Patients With COPD and Comorbid Conditions
Srinivas Annavarapu1 Seth Goldfarb1 Chad Moretz1 Andrew Renda2 Rakesh Luthra3 Shuchita Kaila3
1Comprehensive Health Insights Inc.
2 Humana Inc.
3 Boehringer Ingelheim Pharmaceuticals Inc.
Background:
2017GOLD guidelines recommend the use of ICS containing therapies only in highly symptomatic patients with COPD at high risk of exacerbations. ICS use in patients with COPD is associated with an increased risk for pneumonia, diabetes, and reduced bone density.
Objective:
Assess the proportion of patients with COPD and comorbid pneumonia, diabetes, osteoporosis, and/or heart failure that receive ICS containing therapies, stratified by COPD-hospitalization history.
Methods:
A retrospective study using data from a large US health plan was conducted including patients aged 55-89 years who were continuously enrolled for 12 months pre- and post-COPD diagnosis (index date) from 1/1/2010 to 12/31/2013. Four groups were formed for all patients and newly diagnosed patients: no comorbidities (pneumonia, diabetes, osteoporosis, or heart failure), ≥ 1comorbidities, and with or without pneumonia in the 12-month pre-index period. Patients were also stratified by presence of pre-index COPD-hospitalizations. Proportion of patients on ICS therapy was compared (chi-square) in the 12-months post-index period, among patients receiving at least one COPD maintenance medication.
Results:
21,503 patients with COPD were identified, of whom 11,188 (52.0%) had ≥ 1 comorbidities, with 2,142 (10.0%) having pneumonia. Proportions of patients with and without comorbidities receiving ICS was similar (72.6% and to patients without comorbidities (72.2%, p=0.5203). 77.0% of patients with pneumonia received ICS, significantly higher than patients without pneumonia (71.9%, p<0.0001). Similar ICS use was observed for diabetes, osteoporosis and HF. 71.3% of patients without pre-index COPD-related hospitalizations received ICS. Among patients without pre-index COPD-related hospitalizations, proportions of patients with or without comorbidities receiving ICS were similar (71.2% and 71.4%, p=0.7459) while a significantly higher proportion of patients with pneumonia compared to without received ICS (74.7% and 71.0%, p=0.0109). Among patients newly diagnosed with COPD, a similar proportion of patients with and without comorbidities (70.6% and 69.8%, p=0.3452), and patients with and without pneumonia (72.2% and 70.0%, p=0.1643) received ICS.
Conclusions:
A large proportion of patients with COPD and comorbidities including pneumonia received ICS. A majority of these patients did not have a history of COPD-related hospitalizations. These findings highlight the potential overuse of ICS in patients with COPD and specific comorbidities, and may not align with GOLD treatment recommendations.
Pseudomonas Aeruginosa Impact on Severity of Bronchiectasis
Choate R, MPH1 Mannino DM, MD1 Aksamit T, MD2 Bronchiectasis and NTM Research Registry Consortium,* Stone G, PhD3
1 Department of Preventive Medicine and Environmental Health, University of Kentucky, Lexington, Kentucky
2Pulmonary Disease and Critical Care Medicine, Mayo Clinic, Rochester, Minnesota
3Grifols
Background:
Bronchiectasis is a disease characterized by dilated bronchi leading to mucus collection and recurrent infections of the airways. Chronic infections in patients with bronchiectasis commonly increase number of exacerbations and/or hospitalizations. Pseudomonas Aeruginosa (PA) is one of the most frequently isolated pathogens in sputum of patients with bronchiectasis and some other chronic pulmonary diseases.
Objective:
The objectives of this study are to determine the prevalence of PA in non-CF bronchiectasis patients and to determine the independent impact of PA on hospital admissions, exacerbations, lung function and severity of bronchiectasis.
Methods:
This study used baseline data from the Bronchiectasis and NTM Research Registry (BRR). Prevalence of PA was calculated using one or more positive bacterial results. Hospital admissions and exacerbations frequencies were calculated using responses of the patients at baseline about the number of admissions and exacerbations they had in the past two years. Modified Bronchiectasis Severity Score (BSI) and modified FACED were used to categorize the severity of bronchiectasis. The results for categorical variables were reported by frequencies and proportions, and for continuous variables as mean ± SD. Values between the groups were compared using t-test/ ANOVA or non-parametric Wilcoxon-Mann-Whitney for continuous variables, and Chi-squared for categorical variables. Statistical analyses were carried out using SAS 9.4.
Results:
Almost a quarter of the patients (24.1%) had one or more bacterial cultures positive for PA. A higher proportion of patients with PA reported having pulmonary exacerbations in the past two years (77.4% vs 57.5%, p<.0001) compared to PA-negative patients, with a greater mean number of pulmonary exacerbations (2.1 (SD=2.8) vs 1.3 (SD=2.4) respectively, p<.0001) in the past two years. About a third (33.3%) of the patients positive for PA had been hospitalized for pulmonary illness in the past two years compared to only 18.1% of those with negative PA cultures (p<.0001). PA-positive patients had greater average number of hospital admissions in the past two years compared to PA-negatives (0.7 (SD=1.7) vs. 0.3 (SD=0.8), p<.0001). There was significant impact of PA on lung function (FEV1) in patients with bronchiectasis (FEV1(L): mean (SD)= 1.7 (0.7) vs. 2.0 (0.7), p<.0001; FEV1(% predicted): mean(SD)=66.7 (21.5) vs. 73.8 (21.2), p<.0001).
Baseline data from 994 patients were used to assess the severity of bronchiectasis using modified BSI score. PA-positive patients had significantly greater proportion of high BSI scores (60.0%) compared to PA-negatives(29.5%), p<.0001. Mean modified BSI score in patients positive for PA was 7.0 compared to 9.9 in patients without PA, p<.0001. Data from 839 patients at baseline were available to estimate severity of bronchiectasis using modified FACED. Similarly, to BSI score, significantly higher proportions of patients with PA had severe bronchiectasis (18.4% vs. 3.3%), p<.0001. There were no significant changes in the results after excluding PA variable from the modified BSI score or FACED.
Conclusions:
Our study found estimated prevalence of PA in non-CF bronchiectasis patients of 24.1% in the BRR registry. PA-positive patients had significantly greater average number of exacerbations and hospitalizations, and higher modified BSI and FACED scores. Further research is recommended to better understand the impact of PA on outcomes in patients with bronchiectasis.
Funding source:
This study was funded by Grifols
Acknowledgement:
* Dorreen Addrizzo-Harris1, Timothy R. Aksamit, MD2, Alan Barker, MD3, Charles L. Daley, MD4, M. Leigh Anne Daniels, MD, MPH5, Edward Eden, MD6, Radmila Choate, MPH7, Angela DiMango, MD8, Kevin Fennelly, MD9, David E. Griffith, MD10, Margaret M. Johnson, MD11, Michael R. Knowles, MD5, David Mannino, MD7, Mark L. Metersky, MD12, Peadar G. Noone, MD5, Anne E. O’Donnell, MD13, Kenneth N. Olivier, MD, MPH9, Matthias A. Salathe, MD14, Kevin L. Winthrop, MD, MPH3, 15, Byron Thomashow, MD8, Gregory Tino, MD16, Gerard M. Turino, MD6
1New York University School of Medicine, New York, New York
2Pulmonary Disease and Critical Care Medicine, Mayo Clinic, Rochester, MN
3Department of Pulmonology, OHSU School of Medicine, Portland, OR
4Division of Mycobacterial and Respiratory Infections, National Jewish Health, Denver, CO
5University of North Carolina at Chapel Hill, Chapel Hill, NC
6Icahn School of Medicine, Mt Sinai West and Mt Sinai St Luke’s Hospitals, Mt Sinai, NY
7Department of Preventive Medicine and Environmental Health, University of Kentucky, Lexington, KY
8Columbia College of Physicians and Surgeons, Center for Chest Disease, New York, NY
9National Heart Lung and Blood Institute, NIH, Bethesda, MD
10University of Texas at Tyler, Tyler, TX
11Mayo Clinic Florida, Pulmonary and Critical Care, Jacksonville, FL
12Division of Pulmonary and Critical Care Medicine, University of Connecticut School of Medicine, Farmington, CT
13Georgetown University Medical Center, Washington, DC
14University of Miami Miller School of Medicine, Miami, FL
15Department of Infectious Disease, OHSU School of Medicine, Portland, OR
16University of Pennsylvania Perelman School of Medicine, Philadelphia, PA
Efficacy of an mHealth Integrated Care Program Post Pulmonary Rehabilitation for COPD Patients: A Pilot Randomized Control Trial
B. Jiménez Reguera1 E. Maroto López2 M. López Martín3 L. Juarros Monteagudo4 N. García Gutiérrez4 M. Sánchez4 J. Rodríguez Hermosa5 A. Montero Pacios5 J. Vilaro Casamitjana6* S. Fitch7
1 Lovexair Foundation. Facultad de fisioterapia Universidad CEU San Pablo de Madrid - Madrid (Spain),
2 Lovexair Foundation. Área de Pacientes, Innovación Tecnológica y Formación de la Fundación Lovexair - Madrid (Spain),
3 Hospital Universitario de la Princesa - Madrid (Spain),
4 Hospital 12 de Octubre - Madrid (Spain),
5 Medical Research Institute (IdISSC) Hospital Clínico San Carlos – Madrid (Spain),
6 FCS Blanquerna, Physical Activity and Health Research Group (SAFE). Ramon Llull University - Barcelona (Spain)
7 Fundación Lovexair. President
Background:
Pulmonary rehabilitation (PR) is the most efficient nonpharmacological
intervention for COPD. However, maintaining its effectiveness for a long period of time is still a challenge. The lastest research show that a solution to this problem may be the use of mobile phones and other Wireless technology in medical care (mHealth). The aimof this project is to evaluate the efficacy and effectiveness of an mHealth integrated care program (MHICP) carried out on patients after conventional PR, to continue its benefits.
Method:
After an ambulatory PR program of 8 weeks duration, COPD patients were randomly allocated to a conventional follow up control group (CG) or MHICP Intervention Group (IG)
The protocol, in both groups, followed 4 evaluations: start, post PR, 8 and 12 months. Pulmonary Function, quality of life (SGRQ, EUROQOL-5D, EQ visual analogue scale and CAT), exercise tolerance (6MWT), dyspnoea (mMRC), adherence and perception (CAP-Physio) were assessed along with standard measures.
The IG followed a daily-care program which consisted of the following: introduction to basic digital literacy, using an app for patient- reported outcomes (PRO), self-care techniques, physical activity and behavioural & motivational support with an educator guidance and monitoring via a clinical platform and telephone/messaging support.
Results:
A total of 44 COPD patients, 21 oxygen therapy users, from 3 Madrid Hospitals at stages GOLD II, III, IV (59% male) were included (23 CG and 21 IG). FEV1 46.2(16.5) vs 40.2(11.1), CG and IG respectively. The multivariate analysis showed significative differences between groups in CAT (p<0.0001); SGRQsimpt (p<0.0001); EQ visual analogue scale (p=0.016) and 6MWD (p=0.004). Finally, the IG patients presented more adherence and good perception of the program (p<0.05, both).
Conclusions:
We conclude that a long term mHealth integrated care program, indicates effectiveness and efficacy, to maintain and improve the physiological effects and quality of life in COPD patients after pulmonary rehabilitation.
The Impact of Integrated Respiratory Care Coordination on Patients in Primary Care
Michael W. Hess, BS, RRT1 Kelly N. Becker, MSN, FNP-BC
1Western Michigan University Homer Stryker M.D. School of Medicine
Contact Information: 1000 Oakland Drive, Kalamazoo, MI 49008; phone: 269-348-2841;email: michael.hess@med.wmich.edu
Funding Sources:
None
Abstract:
COPD patients often experience gaps in knowledge and access to care for many reasons. Both the latest iteration of the Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (the “GOLD recommendations”) and the NHLBI COPD National Action Plan call for enhanced care coordination and patient education leading to improved self-efficacy, in an attempt to close these gaps. However, little evidence currently exists to demonstrate the impact these programs have on quality of life, psychosocial metrics, or other patient-centered functional outcomes.
The WMU School of Medicine has integrated a respiratory therapist/COPD educator directly into their urban primary care clinic to act as a consultation resource, a patient educator/navigator, and care facilitator. As this clinic also serves as a resident physician training program, the presence of a “COPD clinic” on premises has the potential to be a demonstration model for the development of future medical home-type primary care practices as these clinicians complete their residencies and establish their careers. It is anticipated that this program will also serve as a research engine to support and promote the adoption of various care coordination, education, and access standards for primary care providers throughout the United States healthcare system.
This poster will examine the impact that personalized care management provided by a respiratory therapist has on quality of life as measured by COPD Assessment Test™ (CAT), evaluations of inhalation device technique, social/community engagement, and other metrics. While this is a relatively new program, it appears to already be increasing access to resources like pulmonary rehabilitation, and having a positive impact on certain measures, as well as demonstrating to physicians that respiratory therapy is a valuable resource outside of the traditional inpatient setting.
Effect of Gender and Menopause on Coronary Artery Calcium in the COPDGene Study
Amena Keshawarz, MPH, Dawn L. DeMeo, MD, MPH, Marilyn G. Foreman, MD, MS, Sharon Lutz, MPH, PhD, Kendra A. Young, MSPH, PhD, Elizabeth Regan, MD, PhD, John E. Hokanson, MPH, PhD, Matthew J. Budoff, MD, Gregory L. Kinney, MPH, PhD
Contact: amena.keshawarz@ucdenver.edu; 303-724-8789
University of Colorado Anschutz Medical Campus, 1775 Aurora Ct., Aurora, CO 80045
Funding: R01 HL 089859, R01 089897
Introduction:
Severe COPD is associated with increased risk of coronary artery calcium (CAC), a measure of subclinical atherosclerosis strongly associated with cardiovascular disease (CVD). Sex differences in the risk of CAC and CVD exist; they are also present in COPD, as women may be more susceptible to developing severe, early-onset COPD than men. Because both CAC and COPD differ by sex and COPD is associated with increased risk of CAC, we examined whether differences in CAC by sex persist in individuals with COPD. Secondly, because CVD risk in women further increases following menopause, we assessed if there is a difference in CAC by menopause status in women with COPD.
Methods:
The COPDGene study is a prospective, multicenter study focusing on COPD in a cohort of men and women (mean age 70 ± 9 and 69 ± 9 years, respectively) with at least 10 pack-years of smoking history. Logistic regression was used to compare the presence of CAC at the Phase 1 study visit in participants who did not report a prior diagnosis of CVD (n=3,941). COPD severity was assessed by GOLD 2011 classification. Menopausal status at the time of CAC measurement was derived using self-reported menopause status and age of menopause collected at the Phase 2 study visit. We first compared the odds of any CAC presence in men and women with and without COPD. We then compared the odds of any CAC presence in pre-menopausal and post-menopausal women with and without COPD.
Results:
Female sex was associated with significantly lower odds of CAC (OR=0.46, 95% CI: 0.40, 0.54) in NHW women compared to men regardless of COPD severity. African American women with COPD (GOLD stages 2-4) and preserved ratio impaired spirometry (PRISm) still saw an overall protective effect compared to men, but this was not statistically significant (OR=0.73, 95% CI: 0.48, 1.13 and OR=0.70, 95% CI: 0.41, 1.20 respectively). The final model was adjusted for age, smoking history, comorbidities, and the interaction between gender, race, and COPD severity.
Post-menopausal status was associated with CAC in univariate analysis (OR=2.75, 95% CI: 2.10, 3.60). However, after adjustment in the final model for age, smoking history, comorbidities, and time in menopause, this association is mitigated (OR=1.01, 95% CI: 0.71, 1.43). Further stratification to compare individuals with COPD (GOLD stages 2-4) to individuals without COPD showed that there was no difference in CAC between pre-menopausal women with COPD compared to those without COPD (OR: 1.77, 95% CI: 0.91, 3.46). However, post-menopausal women with COPD had slightly increased odds of CAC compared to controls (OR: 1.61, 95% CI: 1.22, 2.12).
Conclusion:
These analyses show that sex differences in CAC persist in individuals with severe COPD. NHW women particularly see a protective effect against CAC as compared to men. Additionally, odds of CAC are similar regardless of self-reported menopause status of women in this cross-sectional sample. However, among post-menopausal women only, COPD is associated with increased odds of CAC compared to individuals without CAC.
Psychological Factors Among COPD Patients: Relations With Smoking Status and COPD Symptom Impact
Amanda R. Mathew, PhD, Susan Yount, PhD, Ravi Kalhan, MD, MS, Brian Hitsman, PhD
Northwestern University Feinberg School of Medicine
Background:
Chronic obstructive pulmonary disease (COPD) is a tobacco-related disease associated with several comorbid conditions, including elevated rates of depression and anxiety. Psychological factors that commonly underlie nicotine dependence, depression, and anxiety may represent novel treatment targets, but have not yet been examined among COPD patients. We assessed three psychological factors – anxiety sensitivity (AS; fear of anxiety-related sensations), distress intolerance (DI; inability to withstand distressing states), and anhedonia (Anh; diminished sense of pleasure or interest) – in relation to smoking status, COPD symptom impact, and negative response to COPD symptoms.
Methods:
We conducted a single-session laboratory assessment with 40 COPD patients (20 current smokers and 20 former smokers). All participants completed self-report measures of psychological factors (Anxiety Sensitivity Index, Distress Intolerance Index, and Snaith-Hamilton Pleasure Scale, respectively), COPD symptom impact (COPD Assessment Scale), response to COPD symptoms (Breathlessness Catastrophizing Scale), and general anxiety and depression symptoms (PROMIS-Depression and Anxiety short forms).
Results:
Participants were older adults (66.7 + 6.8 years; 21 men, 19 women) with moderate levels of COPD symptom impact (CAT score 16.6 + 6.7). Current vs. former smokers reported higher levels of AS (19.0 vs. 9.9; p=.01) and marginally higher levels of DI (16.1 vs. 11.5; p=.07). In univariate regression models, AS, DI, and Anh were each associated with greater COPD symptom impact (β’s .31-.64; all p’s<.05). Each factor was also positively associated with breathlessness catastrophizing (β’s .36-.67; all p’s<.05). Only AS remained a significant predictor of COPD symptom impact (β=.36, p=.03) and breathlessness catastrophizing (β=.31, p=.04) after adjusting for general depression and anxiety symptoms.
Conclusion:
Preliminary findings show that AS and DI are higher among current vs. former smokers and all three psychological factors are positively associated with COPD symptom impact and negative response to symptoms. AS showed unique associations with COPD functioning even after adjusting for general depression and anxiety symptoms, perhaps because it specifically indexes risk for negative reactions to bodily sensations such as shortness of breath. AS may be an important target for behavioral interventions to improve symptom burden and quality of life among COPD patients.
Funding:
This research was supported by the NIH National Center for Advancing Translational Sciences (UL1TR001422).
Corresponding Author:
Amanda R. Mathew, PhD, Northwestern University Feinberg School of Medicine, 680 North Lake Shore Drive, Chicago IL 60611; Phone: 312-503-1343; Email: Amanda.mathew@northwestern.edu
Individual and Neighborhood Determinants of Adherence to Pulmonary Rehabilitation in Chronic Obstructive Pulmonary Disease
Gabriela R. Oates, PhD,* Bryant W. Hamby, MA, Irena Stepanikova, PhD, Sara J. Knight, PhD, Surya P. Bhatt, MD, Jason Hitchcock, MBA, BSN, Christopher Schumann, MA, Mark T. Dransfield, MD
*Division of Preventive Medicine, University of Alabama at Birmingham, MT 623, 1717 11th Avenue South, Birmingham, AL 35205; phone: 205-975-7940; goates@uab.edu
Background:
Adherence to pulmonary rehabilitation (PR) is low. Previous studies have focused on clinical and demographic predictors of PR completion, with little attention to socio-environmental factors. We aimed to identify social determinants of adherence to PR in COPD patients.
Methods:
Data were obtained from a prospectively maintained database of COPD patients (N=455) who had attended an outpatient PR program from 1996 to 2013. Individual-level variables included age, sex, race, BMI, smoking status, pack years, baseline 6-minute walk distance (6MWD: <150, 150-249, ≥250), comorbidities, depression, and prescribed PR sessions (≤20, 21-30, >30). Adherence, calculated as a ratio of attended-to-prescribed sessions, was coded as low (<35%), moderate (35-85%), and high (>85%). Area-level measures aggregated to Census tracts, proxies for neighborhoods, were obtained from the 2000 and 2010 U.S. Census after geocoding patients’ residential addresses. A socioeconomic disadvantage index, constructed from 15 candidate variables through exploratory factor analysis with orthogonal VARIMAX rotation, included 6 factors with loading >0.5: poverty, public assistance or food stamps, households without vehicles, cost burden (>30% income toward housing), unemployment, and minority population. Multivariate regression models were adjusted for clustering on Census tracts.
Results:
26% of patients had low adherence, 23% were moderately adherent, and 51% highly adherent. Relative to high adherence, low adherence was associated with smoking, lower functional status, more comorbidities, and more prescribed PR sessions, while moderate adherence was associated with more prescribed PR sessions and higher socioeconomic disadvantage. In the best fitted joint model of individual and neighborhood characteristics, smoking more than tripled the relative risk of low adherence (p<0.01), while each increase in 6MWD category decreased it by 72% (p<0.01) and 82% (p<0.001), respectively. Each decile increase in the neighborhood socioeconomic disadvantage index increased the risk of moderate vs high adherence by 12% (p<0.01).
Conclusions:
Health status and socioeconomic disadvantage impact patients’ ability to attend PR over extended periods of time. While smoking and low functional capacity are predictors of low adherence, socioeconomic disadvantage is a predictor of moderate adherence. Interventions to improve adherence to PR should consider the different pathways of suboptimal adherence. Future research should test approaches to mitigate the negative impact of economic hardship on adherence
This project was supported by grant number K12HS023009 from the Agency for Healthcare Research and Quality.
Symptom Burden Among Patients Reporting Nontuberculous Mycobacteria (NTM): Findings from the COPD Foundation Survey
Pravosud V,1 Mannino DM,2 Choate R,1 Prieto D,3 Malanga E,3 Zhang Q,4 Aksamit T5
1College of Public Health, University of Kentucky, Lexington, Kentucky
2Department of Preventive Medicine and Environmental Health, University of Kentucky, Lexington, Kentucky
3COPD Foundation, Washington, DC.
4Insmed Incorporated, Bridgewater, New Jersey
5Pulmonary Disease and Critical Care Medicine, Mayo Clinic, Rochester, Minnesota
Background:
The burden of symptoms that patients with nontuberculous mycobacterial lung disease (NTMLD) or infection can experience remains underreported. These data may contribute to design future investigations of individuals diagnosed with NTM infection or disease.
Objective:
To determine the proportion of patients with NTMLD who reported symptoms and quality of life impairments. We also sought to determine the proportion of patients reported being troubled by these symptoms or impairments.
Methods:
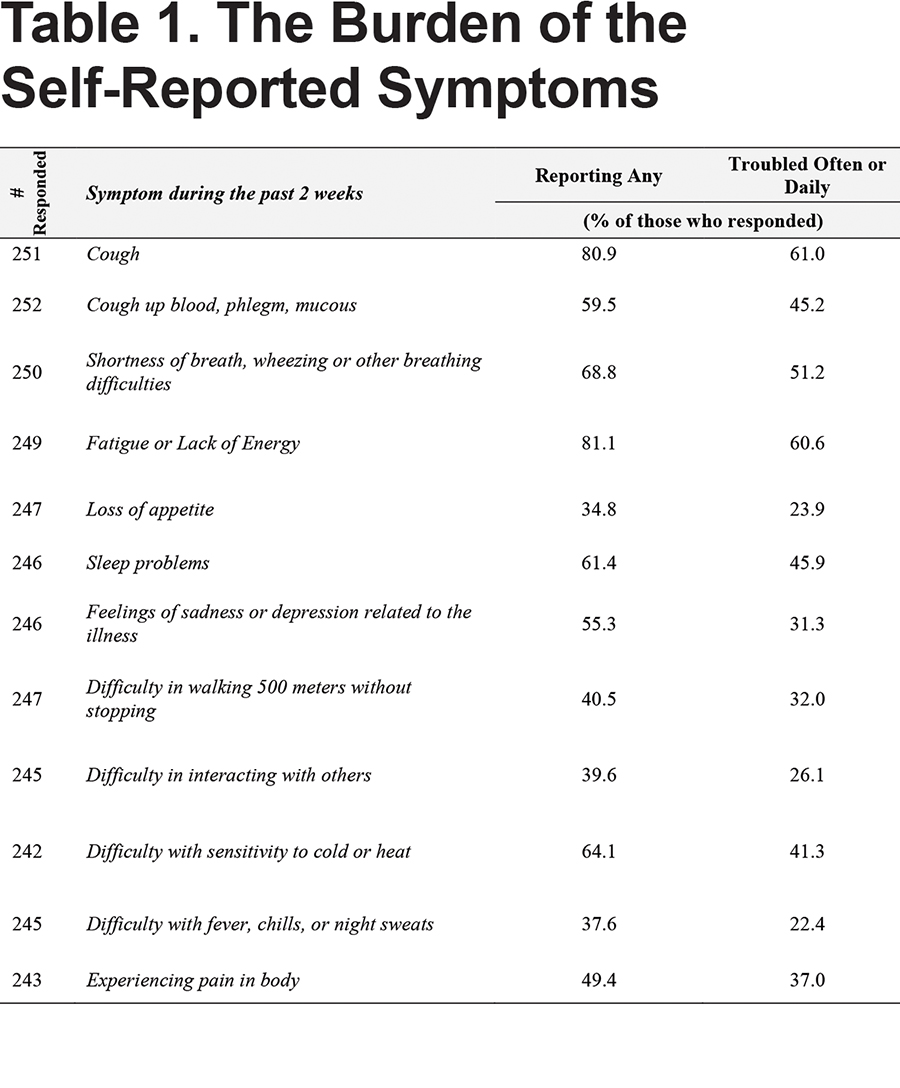
The COPD Foundation developed the website BronchandNTM360social based on their COPD360 social community. The “Burden of NTM Survey” was developed by the COPD Foundation and posted on the website from September 12, 2016 through January 11, 2017. Respondents were limited to those patients reporting that they had been diagnosed with NTMLD. The survey participants were asked about experiencing twelve symptoms during the past two weeks including cough, cough up blood/phlegm/mucous, fatigue or lack of energy, sleep problems, feelings of sadness or depression related to illness, difficulty in walking 500 meters without stopping, difficulty in interacting with others, difficulty with sensitivity to cold or heat, difficulty with fever, chills, or night sweats, and experiencing body pain. The survey participants were also asked about taking any medication to treat their NTMLD, their age group, gender, residence, duration of living with NTMLD, and experiencing selected comorbidities.
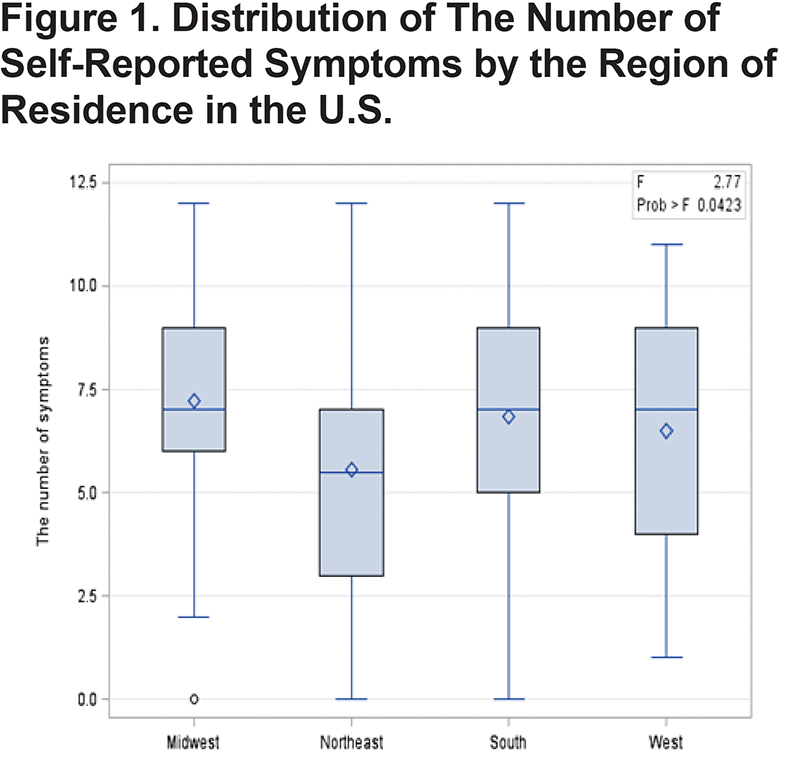
The analysis was carried out using SAS 9.4. Descriptive statistics of the study sample as well as the rank-based nonparametric tests were used to assess whether there were differences in the number of self-reported symptoms among gender and age groups. Moreover, the differences among four U.S. regions were examined for those patients who resided in the U.S. using both the Kruskal-Wallis H test and the analysis of variance. Two-sided p-values ≤0.05 were considered statistically significant.
Results:
Data were available from 266 individuals reporting an NTMLD diagnosis. The majority (95.06%) of respondents were aged 50 or older, of female gender (93.1%), had an on-going NTM lung infection (73.9%), were living with NTMLD for more than 5 years (55.7%).
The Kruskal-Wallis H test indicated that there were no statistically significant differences between the medians of the number of self-reported symptoms neither between women and men (χ2= 1.4436, p= 0.2296) nor between two age groups of less than or equal/more than 50 years old (χ2= 2.9870, p= 0.0839).
For the subsample of the U.S. patients only (n=235), statistically significant differences (χ2= 8.7104, p= 0.0334) among the medians of the number of self-reported symptoms were observed among four U.S. regions representing the place of residence. Also, those patients who were from the Midwest had reported a higher mean number of symptoms (μ=7.1), followed by patients from the South region (μ=6.8), the West (μ=6.5), and finally from the Northeast region (μ=5.5).
Conclusions:
The findings of this study suggest that there were no significant gender or age differences in the medians for number of self-reported symptoms, whereas statistically significant differences were observed among the U.S. patients from different geographical regions. The symptom burden among patients is high, with many patients reporting symptoms that bother them frequently.
Funding Source:
BronchandNTM360social was funded by an unrestricted grant from Insmed.
Acknowledgement:
The NTM survey was developed by the COPD Foundation with input from Amy Leitman and Susan Wisliceny from NTM Info & Research and from Insmed.
Medication Use as a Measure of Severity: Findings from the COPD Foundation NTM Social Survey
Pravosud V1 Mannino DM2 Choate R1 Prieto D3 Malanga E3 Zhang Q4 Aksamit T5
1College of Public Health, University of Kentucky, Lexington, Kentucky
2Department of Preventive Medicine and Environmental Health, University of Kentucky, Lexington, Kentucky
3COPD Foundation, Washington, DC
4Insmed Incorporated, Bridgewater, New Jersey
5Pulmonary Disease and Critical Care Medicine, Mayo Clinic, Rochester, Minnesota
Background:
Understanding how nontuberculous mycobacterial lung disease (NTMLD) can affect a patient remains under investigated. The information about the factors which may be associated with the burden of symptoms can be used for future development of interventions for NTMLD patients.
Objective:
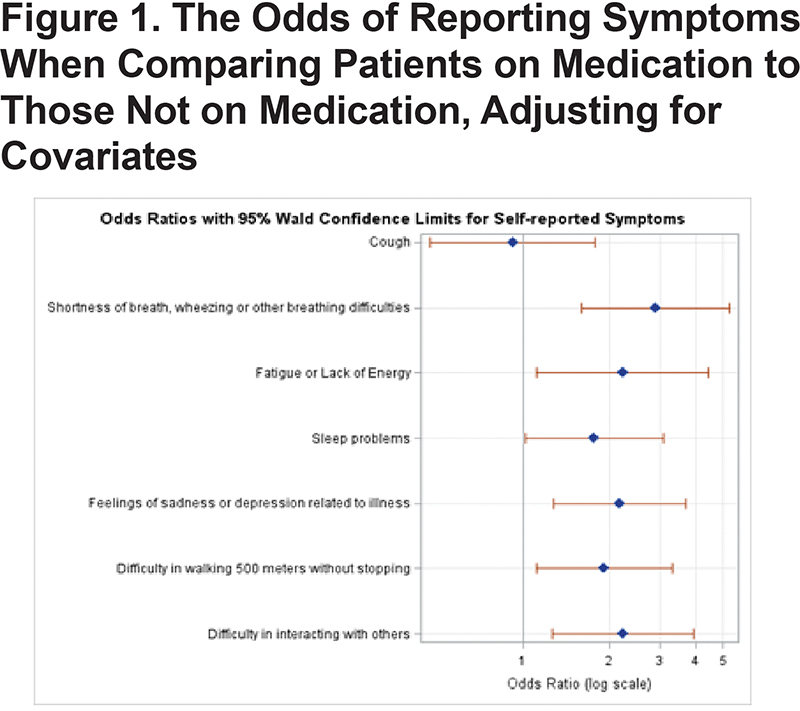
We hypothesize that among patients who report NTMLD, those currently on medication report a higher symptom burden and quality of life impairment than those not currently on medication.
Methods:
The COPD Foundation developed the website BronchandNTM360social based on their COPD360 social community. The “Burden of NTM Survey” was developed by the COPD Foundation and posted on the website from September 12, 2016 through January 11, 2017. The analysis was limited to those patients reporting a diagnosis of NTMLD and compared those not on therapy to those currently on therapy. The survey participants were asked about experiencing different symptoms during the past two weeks (yes/no), taking any medication to treat their NTMLD (yes/no), their gender, duration of living with NTMLD (less than 1 year, 1 to less than 2 years, 2 to 5 years, more than 5 years), experiencing other lung illnesses or infection such as bronchiectasis, COPD/emphysema, cystic fibrosis, or asthma. The survey participants were divided into two age categories (<50 or ≥50).
The analysis was carried out using SAS 9.4. Based on the fact of being on or off medication to treat NTMLD, bivariate analyses, such as Pearson χ2 tests, were conducted to identify differences in the number of individuals having reported such symptoms as cough, fatigue or lack of energy, sleep problems, feelings of sadness or depression related to illness, difficulty in walking 500 meters without stopping, difficulty in interacting with others. The multivariable logistic regression models were carried out with seven symptoms as separate outcomes of interest, and taking any medication to treat NTMLD as the main predictor.
Results:
Of the 266 patients reporting NTMLD, 129 were currently on medication and 129 were not on medication (8 did not answer this question). After adjusting for age, gender, duration of living with NTMLD, and comorbidities, patients on medication had statistically significantly larger odds of reporting of shortness of breath, wheezing or other difficulties (OR=2.9, 95% CI: 1.6-5.3), fatigue or lack of energy (OR=2.2, 95% CI: 1.1-4.5), sleep problems (OR=1.8, 95% CI: 1.01-3.1), feelings of sadness or depression related to illness (OR=2.2, 95% CI: 1.3-3.7), difficulty in walking 500 meter without stopping (OR=1.9, 95% CI: 1.1-3.3), and difficulty in interacting with others (OR=2.2, 95% CI: 1.3-3.9), as compared to those who were off medication (Figure). Cough was similar in the two groups.
Conclusions:
In this database, patient currently on medication reported more symptoms, probably reflecting a higher disease severity among those requiring therapy.
Funding Source:
BronchandNTM360social was funded by an unrestricted grant from Insmed.
Acknowledgement:
The NTM survey was developed by the COPD Foundation with input from Amy Leitman and Susan Wisliceny from NTM Info & Research and from Insmed.
Meta-analysis of LAMA/LABA Versus Iiotropium Using U.S.-Approved Dosages for COPD
Riju Ray1 MeiLan Han2 Jason Foo3 Chaienna Morel3 Beth Hahn1
1GSK, Research Triangle Park, NC, USA
2University of Michigan, Ann Arbor, MI, USA 3Mapi Group, Houten, The Netherlands
Rationale:
The use of fixed dose dual bronchodilators (LAMA/LABA) is increasing in the US; yet, limited research has been conducted to examine how they perform as a group compared with frequently used LAMA monotherapy. Several (network) meta-analyses have been conducted to inform comparative efficacy of these therapies; however, the analyses included dosages not approved in the US and did not include data for new therapies. The purpose of this study is to assess the relative efficacy of LAMA/LABA versus tiotropium (TIO) for US-approved dosages in patients with moderate to severe COPD.
Methods:
A systematic review of the literature was conducted November 2016, following the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines to identify published RCTs comparing selected therapies in patients with COPD. The key study design details, patient characteristics and outcomes were extracted and recorded. Six endpoints were considered and evaluated at 24 weeks: change from baseline in trough forced expiratory volume in 1 second (FEV1 trough as measured by percentage of responders), total score and response to the St. George’s Respiratory Questionnaire (SGRQ) (defined as achieving a minimal clinically important difference of a reduction from baseline in SGRQ total score of at least 4 units), average reduction in rescue medication use (daily number of puffs), and incidence of serious and total adverse events.
Results:
A total of 5,683 citations were identified with the search strategies in Medline, EMBASE, Cochrane and DARE databases. Abstract screening resulted in the exclusion of 5,177 abstracts with an additional 491 publications excluded during full text screening. A total of 7 trials from 15 publications with 4,630 subjects were included in the meta-analysis. Two additional studies reporting relevant data for LAMA/LABA versus TIO were included even though they were published after the search date (November 28, 2016), bringing the total number of trials to 9 (ITT = 6,101). Both fixed and random effects models were employed and model selection for each endpoint was data-driven.
The results of the base-case analysis for trough FEV1 at 24 weeks showed that there was a 66mL improvement for LAMA/LABA therapies compared with tiotropium. The therapies did not differ in SGRQ response rate; however, LAMA/LABA demonstrated a 1.05 point improvement in SGRQ total score compared with tiotropium. There was a reduction in rescue medication use of 0.47 puffs per day for LAMA/LABAs compared with tiotropium. There were no significant differences between the medications in the incidence of total adverse events or serious adverse events.
Conclusions:
Dual bronchodilators demonstrate an increase in lung function, as measured by trough FEV1, and a reduction in rescue medication compared to tiotropium with no additional increase in adverse events.
Funding:
This study was funded by GlaxoSmithKline (GSK study number HO-17-17522).
Use of an Electronic Medical Record-based Algorithm to Improve Care for Inpatients with Asthma or COPD Exacerbation
Susan Russell, MD, Bernadette Cuasay, RN, Sean Kane, MBA, and Ravi Kalhan, MD
Northwestern University
Contact: s-russell4@northwestern.edu
Background:
Inpatient care for patients with asthma and chronic obstructive pulmonary disease (COPD) often deviates from established guidelines, which has contributed to unacceptable outcomes for these populations. In recent years financial penalties tied to readmission rates have motivated institutions to improve processes of care for obstructive lung disease, but to date no study has demonstrated long term efficacy in impacting rate of exacerbation or mortality. Therefore, at our institution we formulated an electronic medical record (EMR) based screening algorithm to identify asthma and COPD patients for both inpatient consultation and outpatient follow up to improve delivery of care.
Methods:
Retrospective study. EMR based algorithm was formulated based on previous ICD-10 or DRG diagnosis codes for asthma or COPD as well as orders for oral corticosteroids and scheduled nebulizer therapy. Chart review performed by a midlevel provider on patients identified by daily EMR based report confirmed asthma or COPD exacerbation prior to inpatient consultation for optimization of therapy. At time of discharge a follow up appointment was scheduled within 2 weeks either with an attending or midlevel provider in outpatient Pulmonary clinic. Readmission rates prior to implementation of this care plan on September 1, 2016 were compared with previous values.
Results:
Readmission rates (any cause) decreased over the study period from 15.5% in September-December quarter of 2016 to 9.9% in September –December quarter of 2017. When analyzed by type of exacerbation, asthma decreased from 10.5% to 7.1% and COPD from 17.6% to 11.6%. Results did not reach statistical significance. Further review of patients with DRG diagnosis codes of asthma or COPD exacerbation following discharge revealed that >90% of patients were identified by the EMR report during their inpatient stay.
Conclusions:
EMR based screening algorithms can correctly identify patients with asthma or COPD exacerbation during their inpatient stay. This information can effectively be used to facilitate guideline based care and timely outpatient follow up.
Funding Source:
none
Pulmonary Consultation During and Following Hospitalization for Acute Exacerbations of COPD Results in Improved Patient-Centered Outcomes in a Large, Integrated Health Care System.
P.F. Simonelli, MD, PhD1 Diane Francis, BS2 Mary Anne Vitunac, RN3 Mary Connell, CRNP4 Amanda Staskiel4
1Depts. Pulmonary/Critical Care Medicine
2Quality Metrics & Analytics
3Quality and Safety
4Health Information Technology, Geisinger Health System, 100 North Academy Ave., Danville, PA. 17822
Abstract Text:
Geisinger Health System adopted a ProvenCare® protocol for the management of severe COPD exacerbations (AE COPD) beginning in 2013. Like other established ProvenCare® protocols, the COPD protocol was developed to implement evidence-based best practice care, to assure consistency and avoid unwarranted variation, and to measure outcome in relation to included metrics. In-hospital management is effected by using a standardized order set, and management for 90 days after discharge is initiated by transition of care planning. Allowance is made to tailor an individual patient’s care, so specific orders can be altered or discontinued at the discretion of the admitting physician. In-patient Pulmonary consultation is included routinely in the ProvenCare® COPD protocol for all AE COPD patients to help assure the accuracy of the diagnosis of COPD, and to assist in the management and transition of care planning by the hospitalist teams. By protocol, all AE COPD patients should be seen within 30 days in post-hospital discharge follow-up in the Pulmonary Clinic. We sought to determine whether patient outcomes were changed when patients were seen in Pulmonary consultation during, after, or both during and after a hospitalization for AE COPD. We examined the data covering a one-year period beginning in April 2016 during which 629 patients were entered in the ProvenCare® COPD protocol, accounting for six hospital locations within the Geisinger system. Of these, 420 (66.7%) were seen by Pulmonary in consultation during the hospitalization, 199 (31.6%) were seen by Pulmonary within 30 days following discharge, 147 (23.3%) were seen both during and following the hospitalization, and 157 (24.9%) were not seen by Pulmonary. The readmission rates measured at 30 and 90 days were improved when seen by Pulmonary during the hospital stay, decreasing by 23.5% and 26.2%, respectively, in comparison with those who were never seen by Pulmonary. Similarly, the corresponding readmission rates decreased by 39.1% and 40.3%, respectively, for those who were seen both during and after the hospitalization. The rate of follow-up care within seven days of discharge within the patient’s primary clinic was consistent across the groups (58-79%), and did not fully account for this difference. Being seen by Pulmonary while hospitalized increased the likelihood of being evaluated in the Pulmonary Clinic after discharge from 35.0% to 66.0% (88.5% increase). Measurement of spirometry following discharge for those who never had COPD confirmed by pulmonary function testing increased from 5.1% to 70.5% when patients were seen in hospital by the Pulmonary consultant, and to 84.4% when patients were also seen by Pulmonary after discharge. Other patient-centric metrics, including antibiotic stewardship, patient and family education by the Respiratory Therapy Dept., and Clinical Nutrition consultation were all increased when patients were seen by Pulmonary when hospitalized (increased by 32.9%, 39.7%, and 57.9%, respectively). The hospital LOS was increased modestly when comparing those seen and not seen in Pulmonary consultation (3.49 vs. 4.07 days). These data provide support for the added value of engaging Pulmonary consultation during and after hospitalization for AE COPD with regard to several patient-centric outcome metrics.
Living Well With COPD
Pamela K Storrs RN, MSN, CMSRN, Angela Lambert RN, BSN, CMSRN
Winchester Medical Center- Valley Health, 1840 Amherst St., Winchester, VA, 22601 Contact: pstorrs@valleyhealthlink.com; 540-536-4479
Abstract Text:
In 2014, Centers for Disease Control and Prevention (CDC) reported that Chronic Obstructive Pulmonary Disease (COPD), was the third leading cause of death in the United States and almost 15.7 million Americans (6.4%) reported that they have been diagnosed with COPD. COPD prevalence rate varies per state but Virginia’s rate is 5.7-6.4% and West Virginia’s is 7.6-12.3%1. COPD also has a financial bearing to institutions. In 2015, Centers for Medicare and Medicaid Services (CMS) included COPD in its Readmission Reduction Program (HRRP) 2. October 2015, our facility, chose COPD as one of their Bundled Payments for Care Improvements (BPCI).
In late 2014, approval was obtained and implementation of a comprehensive COPD program began in March 2015. The Living Well with COPD program, which incorporates an inpatient and an outpatient component, uses a multidisciplinary approach that embraces Global Initiative for Chronic Lung Disease (GOLD) standards. According to the GOLD guidelines prevention of exacerbations is key and exacerbations can often be prevented with smoking cessation, influenza and pneumococcal vaccination, as well as knowledge of current therapy3. Our program centers on the concepts of: consistent education across the care continuum, symptom management, use of evidence based treatment protocols, connection to resources, medication assistance, and smoking cessation.
Inpatients are seen by the COPD nurse. During their time in the hospital the focus is on educational deficits leading to hospitalization and directing them to outpatient education. COPD GOLD guidelines suggest that patients with an exacerbation be on triple inhaler therapy. Therefore, the COPD nurse guides the physician in ordering the right medications and works with the patient on affordability, compliance, and technique. In 2015 only 30.7% of patients were being discharged on triple therapy, in 2016 that number increased to 54.8%. 2017 is currently 64.4%.
The outpatient COPD nurse works in a variety of ways in providing education to interested patients. One on one education, classes, and TeleHealth are all offered free of charge. Our data shows that patients who take interest in their health care are reducing their readmissions. 2016 demonstrated a 71.4% reduction in 90-day post readmission rates compared to 90 day pre readmission rates for patients after their first COPD outpatient visit.
The program empowers people to take control of their disease before they’re hospitalized to preserve lung function and live better longer. The overall goal is to improve the quality of life for patients with COPD and reduce admissions to the hospital.
1.Centers for Disease Control and Prevention at http://www.cdc.gov/copd/index.html (September 16, 2016), accessed 10/3/2016.
2.Centers for Medicare and Medicaid Services at https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html (4/18/2016), accessed 10/3/2016
3.Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. GOLD 2014.
Blended Learning Theory as Framing Device in the Development of a Comprehensive COPD Program for Respiratory Therapists
Blevins, J1 Crout D1 Wheeler DM2
1Adult Respiratory Therapy Department, Medical University of South Carolina, Charleston SC
2 Pediatric Respiratory Therapy Department, Medical University of South Carolina, Charleston SC
Background:
Blended Learning Theory (BLT) is a process of incorporating discreetly tailored learning strategies to evolve a meaningful highly adaptive learning experience to achieve qualitative and quantitative learning outcomes. BLT gives us the potential to provide personalized learning in the creation of a curriculum that meets the needs of individual learners, (therapists, patients etc.) Illeris’s model of BLT rests on assumption that we share in the creation of BLT namely: the adult learner must hold the perception that the material or the curricula has meaning for the achievement of their individualized goals.
The Program:
The COPD Readmission Reduction Program utilizes Blended Learning Theory to enhance patient and family engagement. Patient education is divided into four approximately twenty-minute segments. Each segment includes an evidence-based didactic portion, in-room instructional video, and a scripted dialogue with the patient. Subject matter focuses on anatomy and physiology of COPD, correct MDI and spacer use, breathing techniques, and trigger avoidance, as well as the completion of a COPD Action Plan. Each session requires the patient to demonstrate learning via teach-back.
Total Educational Opportunities:
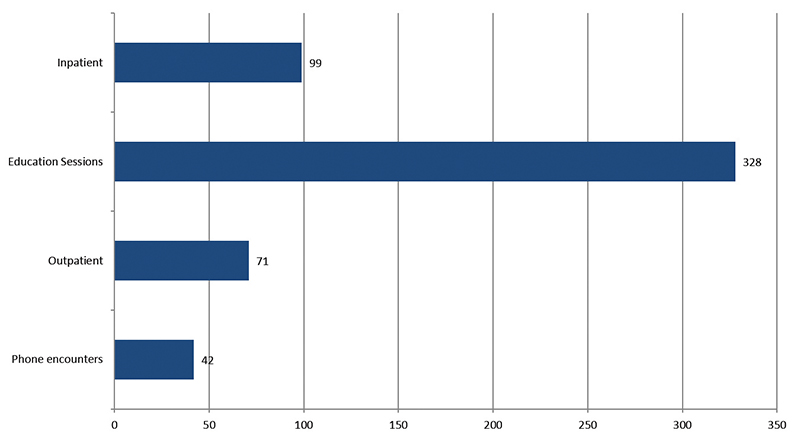
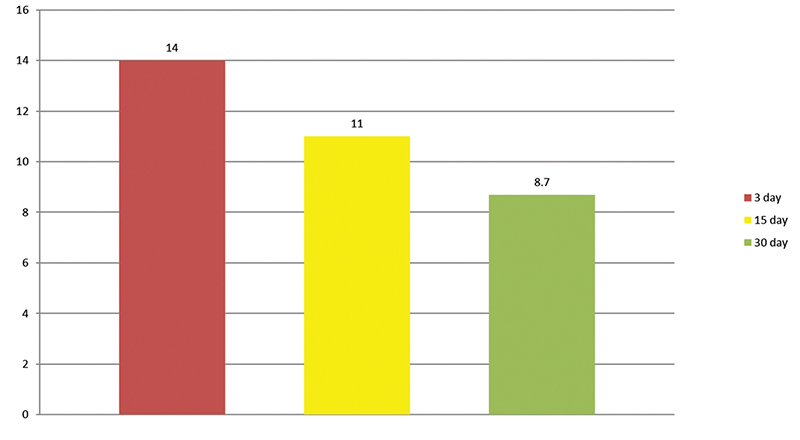
CAT Scoring:
Conclusion:
BLT has become increasingly popular. Learning and teaching methods within this theoretical frame are supported by a large variety of didactic, simulation, online and face-to-face interventions. The adult learner will take as much or as little responsibility for their learning as they want to. The intention of this program is to increase the realization of learning in a context specific fashion through to a highly meta-cognitive self- regulated process. This process will rest on the highly context sensitive BLT platform.
References:
Dick, W., Carey, L. & Carey, J. O. (2009) The Systematic Design of Instruction. 7th edn, Pearson Merrill, Upper Saddle River, NJ.
Dziuban, C., et al., (2006) ‘Blended learning enters the mainstream’, in The Handbook of Blended Learning, eds C.
J. Bonk & C. Graham, Wiley, San Francisco, CA, pp. 195– 208.
Bruner, J. (1996) The Culture of Education, Harvard University Press, Cambridge, MA.
The Cognitive Impact of a Mobile Engagement Program on COPD Patients with Alpha-1 Antitrypsin Deficiency
Richard D. Stachel, DSc, MBA1 Benedict B. Hilldorfer, MS2 Valerie M. Villanueva, PhD2 Louis A. Musante, MLS2
1Robert Morris University, 6001 University Blvd., Moon Township PA, 15108
2echo HEALTHCARE, 1801 Oakhurst Court. Allison Park, PA 15101
Funding Sources:
None
Background:
COPD is the third leading cause of death in the USA. With an annual healthcare cost of $32 billion, there is an urgent need for novel solutions to address the underlying drivers of the high cost of care; two of which are low adherence rates, and re-hospitalization. The widespread adoption of mobile devices presents a unique opportunity to empower patients through daily interactions that leverage both mobile learning and positive behavioral reinforcement in order to improve patient Subjective Well Being (SWB) and Quality of Life (QoL). We present a study that introduces the Thrive Learning Platform (developed by the Affective Computing Company - tACC), which used Ecological Momentary Assessment (EMA) to improve positivity and SWB in order to analyze if that improvement led to higher adherence rates and enhanced QoL.
Methods:
A cohort of 96 patients with Alpha-1 Antitrypsin Deficiency-Associated COPD were enrolled in an 8-week patient engagement program covering topics such as positivity, mindfulness, gratitude, and coping. Patients received short multimedia experiences (lessons) delivered via text message or email from the Thrive Learning Platform twice daily. Each lesson was composed of text, images, questions, and small calls-to-action that took 30-60 seconds to complete. The content was designed to first present validated concepts - such as coping strategies - before reinforcing these concepts through patient practice. Patients’ SWB was measured before and after the program using the modified Differential Emotions Scale (mDES) developed by Barbara Fredrickson (Frederickson et. Al., 2003). Similarly, patients’ QoL was measured before and after the program using the Short Form-12 (SF-12) Health Survey.
Results:
The overall participation rate was 75% over the two-month program with no significant difference between text message and email delivery modalities. Analysis indicated a significant increase in SWB scores (p < 0.01) between pre- and post-program mDES evaluations and a small but insignificant improvement in QoL scores (p = .586 and p = 0.441) between pre- and post-program SF-12 evaluations. Furthermore, 61.5% of patients reported an increase in self-awareness after participating in the program.
Discussion:
In this study, we demonstrate the utility of using the Thrive Learning Platform to deliver short multimedia experiences, which engage patients through daily interactions. Throughout the eight-week program we observed a strong patient participation rate (75%), as well as an overall increase in reported self-awareness (61.5%). While we saw a significant increase in SWB scores (p < 0.01) before and after the program, this was not reflected in a statistically significant increase in QoL scores (p = .586 and p = 0.441) nor an improvement in adherence (χ = 0.701).
Existing medical literature of chronically ill patients suggests that an increase in patient SWB leads to improvement in patient QoL. Furthermore, improvements in QoL are correlated with a decreased risk of hospitalization. This “correlative chain” implies that it is feasible to develop programs with clinical end points that include reductions in patient hospitalization.