Running Head: 3rd World Bronchiectasis Conference Abstracts
Citation: O’Donnell AE, Aksamit TR. Abstracts: 3rd World Bronchiectasis Conference. Chronic Obstr Pulm Dis. 2018; 5(4): 302-323. doi: http://doi.org/10.15326/jcopdf.5.4.2018.0132
Introduction
The 3rd World Bronchiectasis Conference was held at Georgetown University in Washington, D.C., on July 12-14, 2018. The meeting brought together the expertise of the U.S. Bronchiectasis Research Registry and the European Bronchiectasis Registry principal investigators, as well as experts from Canada, Asia, Australia and New Zealand. This program benefited the entire health care team who care for patients with bronchiectasis and nontuberculous mycobacterial lung infections (NTM) including pulmonologists, infectious disease physicians, pharmacists, nurses and respiratory care practitioners.
This gathering of the international community of participants highlighted an authentic world bronchiectasis conference as an extension of the previous 2 World Bronchiectasis Conferences in Milan, Italy in 2017 and Hannover, Germany in 2016. The burgeoning amount of research interest, much needed development of clinical trials, and support of international collaborative work attests to progress made in the past several years awakening the new age of research and clinical work involving bronchiectasis and nontuberculous mycobacterial lung disease.
With nearly 300 attendees, the conference was a focused, cutting-edge gathering of the world’s experts on bronchiectasis and NTM. Original work spanning basic science to clinical investigations were featured during the conference presentations as well as abstracts included in this publication. Highlights included recent advances in research on disease mechanisms in bronchiectasis, including new understandings on the role of inflammation, infection and the microbiome. Clinical topics included sessions on the diagnosis and treatment of bronchiectasis and NTM infections, including small group, case-based presentations specifically aimed at understanding the role of airway clearance, anti-inflammatory treatments and antibiotics.
On Saturday morning, July 14th, the program focused on the management of patients with NTM lung infections. This session was well attended by pulmonologists and infectious disease practitioners who treat patients with these challenging infections. Saturday afternoon offered a halfday workshop solely focused on patients, with educational presentations featuring ways to manage their condition and learn more about bronchiectasis and NTM infections.
Much appreciation is given collectively to the large number of patients, staff, clinicians, researchers, and industry partners involved in making this conference possible. Without the generous time, effort, and support provided, progress towards advancing the science and actively addressing the current gap in knowledge would not be possible. As a result of the 3rd World Bronchiectasis Conference we can look forward optimistically to the opportunities at hand for continuing this international enthusiasm and scientific inquiry, and, most importantly, positively impacting the lives of patients with bronchiectasis and NTM lung disease.
NOTE: The following abstracts have NOT been copyedited but are presented here in their original format, as presented by the authors at the 3rd World Bronchiectasis Conference July 12-14, 2018.
High Frequency Chest Wall Oscillation Physiotherapy as Part of a Bundle of Care Results in Reduced Hospitalizations and Stability of Lung Function in Non-CF Bronchiectasis
Authors: Powner M. Jordan, DO; Denay P. Kirkpatrick, CRNP; Andrew B. Nesmith; Jessica K. Nichols, BSN; George M. Solomon, MD
University of Alabama at Birmingham, Birmingham, AL
Background:
Non-CF Bronchiectasis is characterized by recurrent exacerbations, for which there are limited therapies. High frequency chest wall oscillation therapy (HFCWO) has been shown to improve symptoms; however, there is limited data on improvements of clinical outcomes. This study sought to understand the efficacy of a care bundle, which included early initiation of HFCWO.
Methods:
This retrospective cohort was treated per clinic algorithm if patients experienced >2 exacerbations in the previous 12 months. All patients were treated with an algorithm consisting of nebulized bronchodilators, mucolytics, macrolides, and HFCWO. Patients were eligible for entry upon initiation/receipt of HFCWO device. Baseline lung function was defined as the mean of all values in the 12 months prior to initiation.
Results:
43 patients were analyzed and found to meet study criteria. The mean age was 60.7 years (78% female), and 19% had Pseudomonas aeruginosa. The baseline FEV1 was 1.85 ± 0.60L, which remained stable at 1-year post enrollment (1.89 ± 0.60 L, p=NS), as well as FVC. No significant reduction was observed in the total antibiotic courses, but the frequency of severe exacerbations requiring hospitalization reduced after bundle treatment (1.3 ± 1.0 vs. 0.46 ± 0.81, post, p<0.0001).
Conclusions:
We demonstrate stabilization of lung function after treatment and significant reductions in the number of severe exacerbations requiring hospitalization. The nature of the study does not limit investigator bias about the need for hospitalization, however. Since the present study is retrospective, we are planning prospective study of the role of HFCWO/bundle.
Pulmonary Rehabilitation in Bronchiectasis – Program Components, Outcomes and Insurance Billing Codes
Authors: Shane S. Blake; Gerilynn A. Connnors, BSRT; James Lamberti, MD; Kimberly Palczynski
Inova Fairfax Hospital, Fairfax, VA
Background:
The 2013 American Thoracic Society (ATS)/European Respiratory Society (ERS) Statement in Pulmonary Rehabilitation (PR) documented the positive outcomes of PR in Bronchiectasis to include improvement in exercise. The special consideration for airway clearance techniques in pulmonary rehabilitation was advised. An opportunity exits to increase physician referrals of Bronchiectasis patients to PR and for PR programs in the United States to treat Bronchiectasis patients by understanding the insurance billing codes and special considerations. PR is a standard of care for COPD and the Bronchiectasis patients also deserve this adjunct treatment. The purpose of this abstract is to note how the components of comprehensive PR can result in improved outcomes for the Bronchiectasis patient. Understanding the insurance billing codes in Pulmonary Rehabilitation will allow this special group of patients to be treated.
Methods:
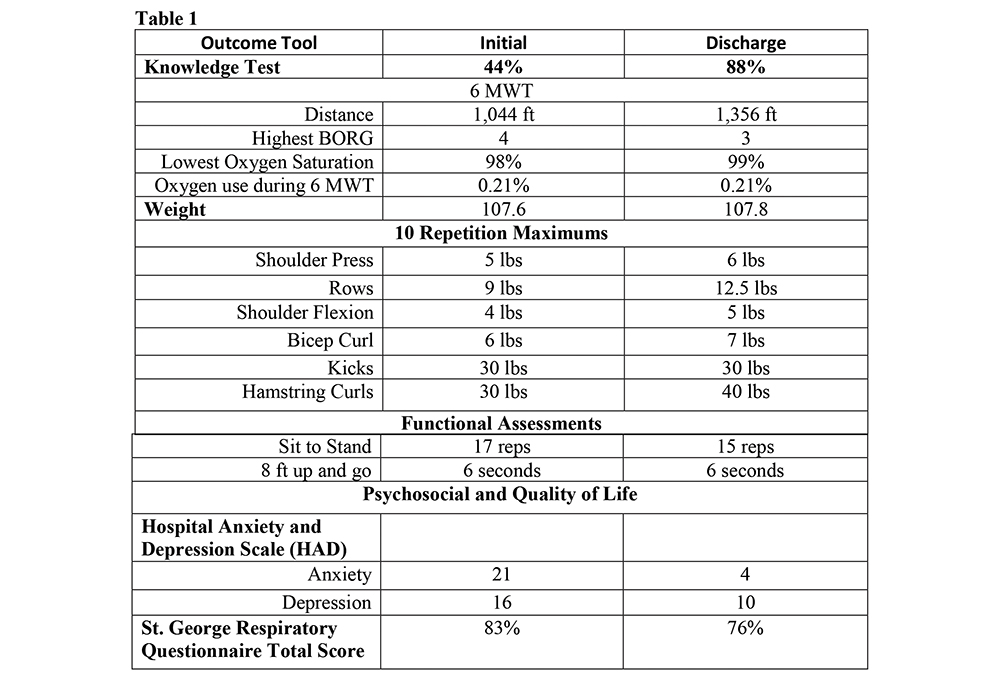
Retrospective Analysis of the PR initial- and discharge outcome tools for a Bronchiectasis patient that completed a 9 week, 3 times a week comprehensive PR program was done. The comprehensive components of PR included: assessment, education, therapeutic exercise, psychosocial intervention and long term adherence. The insurance billing codes used for the PR treatment was G0237 (therapeutic procedure strength and endurance), G0238 (other respiratory procedure, individual) and G0239 (other respiratory procedure, group).
Results:
The Bronchiectasis patient attended the 9 week Inova Fairfax Hospital PR program completing 24 of the 26 therapeutic exercise sessions and 9 of the 9 education-training sessions. The table below reports the PR outcomes.
Conclusions:
Exercise tolerance and quality of life can be improved in the Bronchiectasis patient referred to a comprehensive PR program.
The Comparison of Bronchiectatic Lung Disease in Different Ages
Authors: Adi Dagan, MD; Ori Efrati, MD; Amir Onn, MD
Sheba Medical Center, Tel-Hashomer, ISRAEL
Background:
Bronchiectasis is chronic irreversible dilation of bronchi prevalent in all ages, caused by inherited and acquired disorders. Aim: To compare epidemiology, etiology and management between different age groups.
Methods:
99 patients were collected and divided into three groups: under 18 years, young adults 18-40, and elders above 40.
Results:
Male predominance found in the pediatric group opposed to females in the elders. No differences found in symptomatology, apart from hemoptysis which prevailed in the two adult groups. History of childhood hospitalizations (50%, 30%, and 8%) and recurrent pneumonia (65%, 45%, and 22%) were higher among children. Haemophilus in sputum prevailed in the pediatric group (50%, 30%, and 22%) whereas Pseudomonas in the elderly group (20%, 37%, 42%). Mycobacteria and Aspergillus isolation also increased with age. PFTs showed no difference by age groups. 80 patients had bilateral and 19 single sided diseases without differences in lobar distribution by age or etiology. Post-infectious bronchiectasis was common (37%) among children, whereas in young adults 27% had post-infectious and 27% PCD. In the elder group the common etiology (27%) was idiopathic. Management with physiotherapy and hypertonic saline was similar in all ages. No differences were found in treatment, tailored individually to the patients, including preventive therapy with Azithromycin. However inhaled corticosteroid use was higher in children while long acting beta agonists, oral steroids and inhaled antibiotics prevailed in adults.
Conclusions:
Different age groups should undergo similar investigation and management protocols; therefore, younger patients should be added to the registries and clinical studies.
A Passport for Patients with Non-Cystic Fibrosis Bronchiectasis: A Qualitative Investigation of Patients’ Beliefs and Expectations
Authors: Anthony G. De Soyza, MD, PhD; Paul M. McCallion, PT
Newcastle Upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, UNITED KINGDOM
Background:
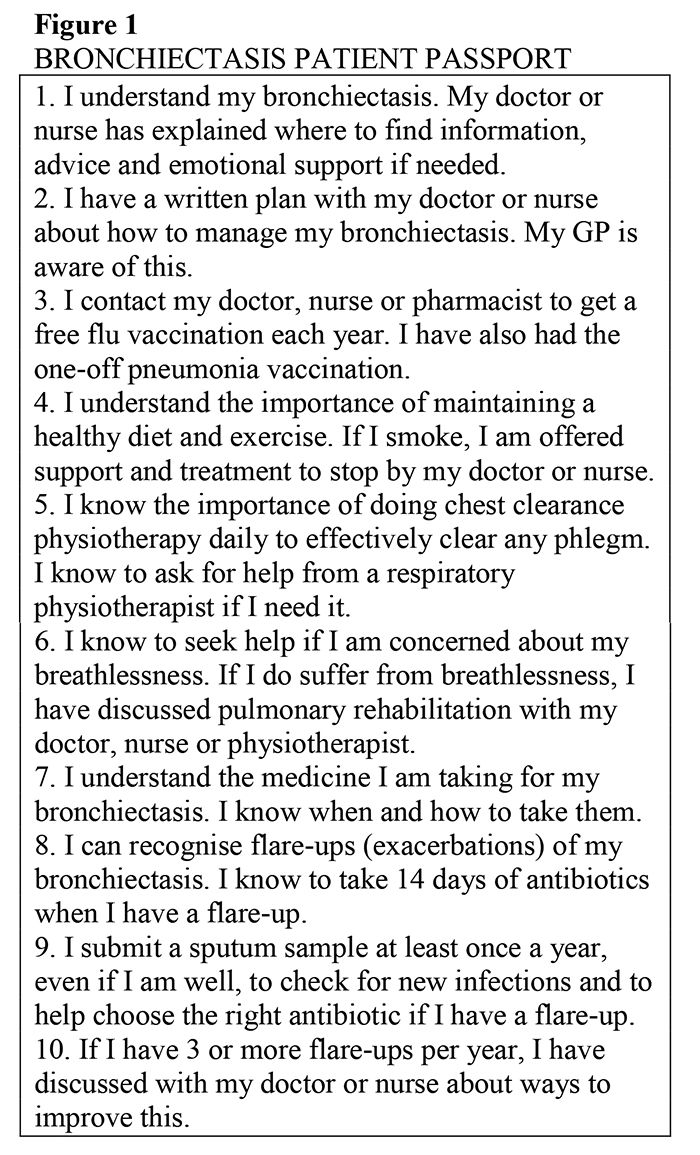
Bronchiectasis is a chronic lung condition characterised by irreversible airway dilatation. There are many key management principles necessitating a need for patient education and understanding of their condition as soon as possible after diagnosis Previous research has demonstrated patients with bronchiectasis feel more confident self-managing their condition after receiving information in a specialist clinic. A draft information resource called the bronchiectasis patient passport was developed by a multi-disciplinary team including expert physicians, physiotherapists and patient / carers. We aimed to assess patient and carer views on challenges in bronchiectasis care and define their views on a draft patient passport and how this might help future patients.
Methods:
Eleven participants were recruited for focus groups. Focus groups were conducted, digitally recorded and transcribed verbatim The data were analysed using Thematic Analysis
Results:
Three themes were identified: Interactions with Health Care Professionals, Self-Management and Beliefs about the Passport Patients expressed the importance of being under a specialist clinic; having a single point of contact, continuity of care and access to multi-disciplinary team services. Most patients demonstrated good knowledge of their disease and self-management strategies. Patients felt the passport would be useful for newly diagnosed patients Suggestions for alterations to the passport were discussed and implemented.
Conclusions:
This study showed patients felt the passport was a useful information resource. Future research should include implementing the passport within the clinical setting and using outcome measures to assess its usefulness in patient knowledge and self-management of their bronchiectasis.
Clinical, Functional and Microbiologic Characteristics of Patients with Co-Existence COPD and Bronchiectasis: Comparison to COPD or Bronchiectasis Alone
Authors: Katerina Dimakou, MD, PhD; Georgios Drivas, MD; Georgios Hillas, MD, PhD; Maria Kaponi, MD, MBA; Sofia Koukidou, MD
5th Respiratory Department, Sotiria Chest Hospital, Athens, GREECE
Background:
Bronchiectasis often coexist with COPD and contribute to disease severity. The aim was to study the characteristics of patients with COPD and Bronchiectasis (BE) and compare to COPD without BE and BE without COPD in a Greek cohort
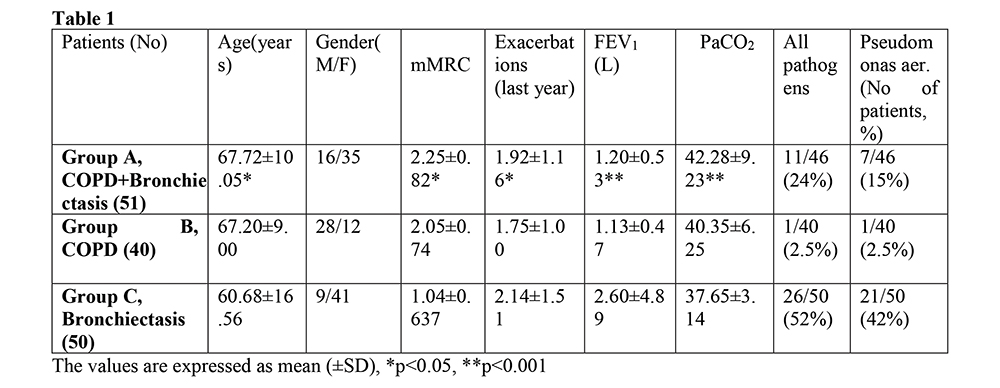
Methods:
Three groups of patients were studied prospectively: Group A (COPD+BE), group B (COPD) and group C (BE). Symptoms, exacerbations/year, lung function, sputum culture, arterial blood gases and number of lobes involved with BE on HRCT were recorded.
Results:
51 patients were included in group A (16 male), 40 in group B (28 male) and 50 in group C (9 male). Patients with COPD+BE comparing to BE alone were older (p=0.028), had worse dyspnea (p=0.03), lower FEV1 (p<0.001) and higher PCO2 (p<0.001). Comparing to COPD alone they had a higher rate of exacerbations (p=0.028) and Pseudomonas aeruginosa growth in sputum
Conclusions:
Our findings suggest that patients with COPD and Bronchiectasis are more severe than those with only COPD or Bronchiectasis. In COPD patients, the presence of pathogens, especially Pseudomonas may indicate the co-existence of Bronchiectasis.
The Clinical Impact of Self-Reported Symptoms of Chronic Rhinosinusitis in Adults with Bronchiectasis
Authors: Janet L. Bondarenko, PT1; Brenda M. Button, PhD1; Annemarie L. Lee, PhD2; Caroline H. Nicolson1
1Alfred Health, Melbourne, AUSTRALIA; 2Monash University, Melbourne, AUSTRALIA
Background:
Chronic rhinosinusitis (CRS) affects between 44% and 72% of adults with bronchiectasis and has been linked to increased disease severity according to spirometry. However, the impact of self-reported symptoms of CRS and health-related quality of life (QOL) is unclear. This study aimed to 1) establish the relationship between symptoms of CRS, HRQOL and health status and 2) identify predictors of HRQOL in adults with bronchiectasis and symptoms of CRS.
Methods:
Measures of HRQOL included the Quality of Life–Bronchiectasis (QOL-B) Questionnaire, Leicester Cough Questionnaire (LCQ) and Bronchiectasis Health Questionnaire (BHQ). Symptoms of CRS were evaluated by the Sinonasal Outcome Test-22 (SNOT-22) and the Total Nasal Symptom scores for 12 and 24 hours (TNSS12 and TNSS24). Disease severity was assessed using the Bronchiectasis Severity Index (BSI).
Results:
Sixty participants with bronchiectasis (mean[SD] FEV1 73.2[25.5]% predicted) were included. More severe CRS symptoms (according to the SNOT-22 total score) were associated with poorer cough-related QOL (all r>-0.60) and reduced health status (r=-0.401). A higher SNOT-22 total score was moderately associated with poorer physical function (r=-0.518), less vitality (r=-0.631), reduced social function (r=-0.546), greater treatment burden (r=-0.411) and increased severity of respiratory symptoms (r=-0.534). More severe symptoms of CRS were weakly related to a higher BSI (r=0.29). The BSI, SNOT-22 and LCQ total scores were predictors of each of the domains of the QOL-B.
Conclusions:
CRS symptoms have a negative impact on disease-specific and cough-related QOL, are weakly related to disease severity, and predict QOL in adults with bronchiectasis.
Age, Fev1 and Severe Exacerbation Frequency are Major Determinants of Impaired Quality of Life (QoL) for Australians with Bronchiectasis
Authors: Anne Chang, MD, PhD1; Lucy Morgan, MD, PhD2; Dean Mills, PhD3; Enna Stroil-Salama4; Simone Visser, MD2
1Menzies School of Health Research, Casuarina, AUSTRALIA; 2University of Sydney, Sydney, AUSTRALIA; 3University of Southern Queensland, Darling Heights, AUSTRALIA; 4Lung Foundation Australia, Milton, AUSTRALIA
Background:
QoL is often impaired for patients with bronchiectasis. We know less about the association between clinical measures and domains within the bronchiectasis-specific QoL questionnaire (QoL-B).
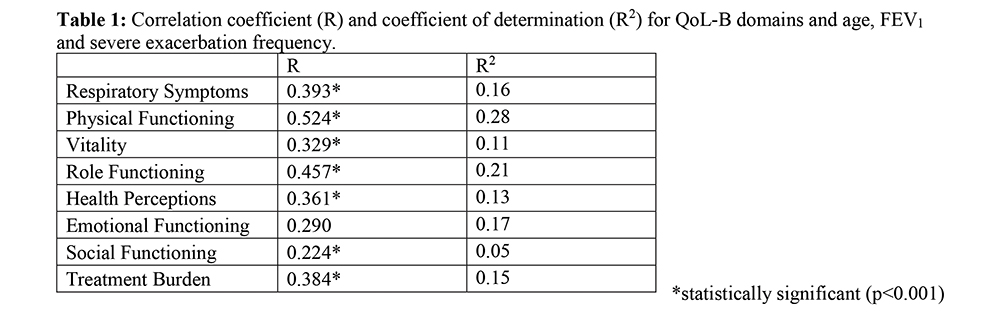
Methods:
Data from adults enrolled within the Australian Bronchiectasis Registry (ABR), who had completed the QoL-B, was used. Spearman’s Rank correlation and stepwise multiple regression analyses were undertaken to assess the association between age, potentially treatable traits [body mass index (BMI), forced expiratory volume in 1s (FEV1 % predicted), Pseudomonas aeruginosa colonisation and severe exacerbation frequency (requiring hospitalisation in the past year)] and QoL-B domains (Respiratory Symptoms, Physical, Role, Emotional and Social Functioning; Vitality, Health Perceptions and Treatment Burden).
Results:
As of June 2018, 968 people have been enrolled in the ABR; 786 adults and 182 children. 359 adult participants (median age 69 years; 83% female) completed the QoL-B survey and had a mean BMI of 25.6+-6 kg/m2, FEV1 of 76.9+-25.7% predicted and 0.5+-1.2 severe exacerbations per year. Age, FEV1 and severe exacerbation frequency predicted poorer QoL. When clustered together, the triad is a surrogate predictor of decreased QoL in all domains except Emotional Functioning (Table 1). BMI and Pseudomonas aeruginosa colonisation had no bearing on QoL.
Conclusions:
Increasing age, FEV1 and severe exacerbation frequency are major determinants associated with impaired QoL for Australian adults within the ABR. This highlights that FEV1 and severe exacerbation frequency are potential targets for improving QoL for patients with bronchiectasis.
Independent Predictors of Primary Ciliary Dyskinesia as the Etiology of Adult Bronchiectasis: Results from the German Bronchiectasis Registry Prognosis
Authors: Roland Diel1; Pontus Mertsch, MD2; Jessica Rademacher, MD3; Felix C. Ringshausen, MD3; Tobias Welte, MD3
1Lungen Clinic Grosshansdorf and German Center for Lung Research, Grosshansdorf, GERMANY; 2Munich University Hospital, Munich, GERMANY; 3Hannover Medical School and German Center for Lung Research, Hannover, GERMANY
Background:
Primary Ciliary Dykinesia (PCD) is a rare genetic disease, which regularly leads to bronchiectasis as disease progresses. Its prevalence as an etiology among adults with bronchiectasis is unknown.
Methods:
We investigated the prevalence of PCD/Kartagener syndrome within the German Bronchiectasis Registry PROGNOSIS and identified independent clinical predictors using multivariate logistic regression analysis.
Results:
Between Jun 2015 and June 2018, 1101 adult subjects with CT-confirmed bronchiectasis were recruited from 38 centers across Germany and across all levels of healthcare (15 private practices, 13 community and teaching hospitals, 10 university hospitals). The mean age (SD) was 59 (15.8) years, 59.3 % were female. Overall, 88 subjects (8.8%) had PCD or Kartagener syndrome as an etiology of bronchiectasis. When ignoring situs inversus the following independent clinical features were identified as clinical predictors of PCD/Kartagener syndrome: upper airway involvement (nasal polyps and/or chronic rhinosinositis (aOR 5.7, 95% CI 3.23–10.12); known bronchiectasis for >15 years (aOR 3.8, 95% CI 2.15–6.61); age <57 years (aOR 3.3, 95% CI 1.74–6.13); radiological involvement of any middle and any lower lobe (aOR 2.7, 95% CI 1.33–5.58); Pseudomonas aeruginosa detected in the past 12 months (aOR 2.1, 95% CI 1.24–3.69); never-smoker (adjusted Odds ratio [aOR] 2.1, 95% confidence interval [CI] 1.16–3.98); and absence of cardiovascular mobidity (aOR 2.1, 95% CI 1.04–4.16).
Conclusions:
Within a representative cohort of adult German patients with bronchiectasis basic clinical data could be identified to support the clinical diagnosis of PCD. Although further diagnostic confirmation is always required, basic clinical information may be utilized to enable earlier diagnosis of PCD.
Comparison Between Culture and Culture Independent Assessment of Bronchoalveolar Lavage Fluid in Bronchiectasis
Authors: Doreen Addrizzo-Harris, MD; Shriram Alapaty, MD; Leopoldo Segal, MD; Imran Suleiman, MD; Benjamin Wu, MD
New York University, New York, NY
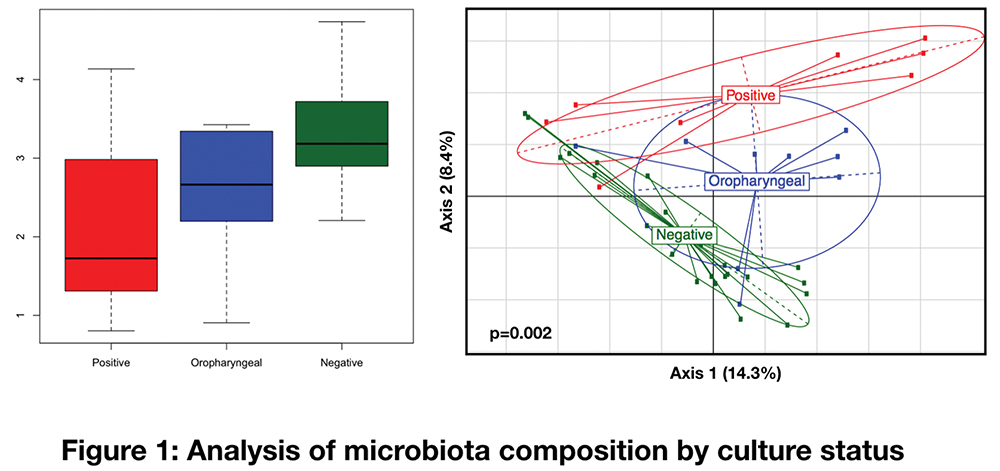
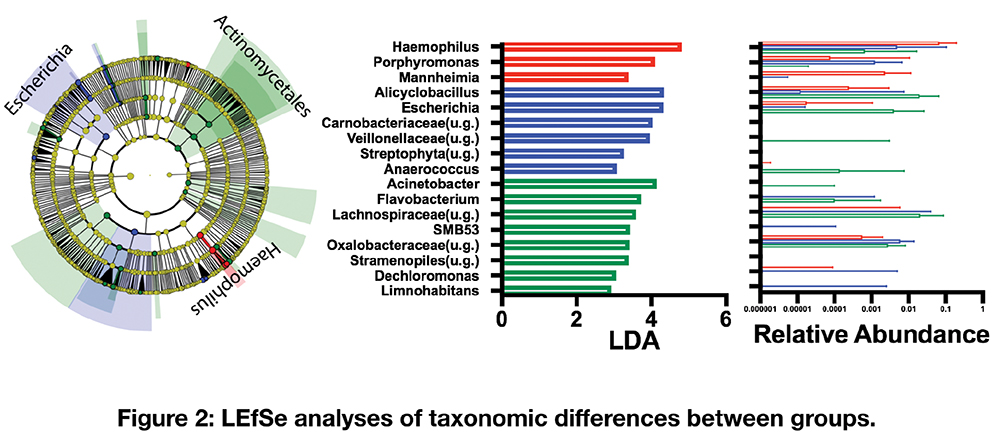
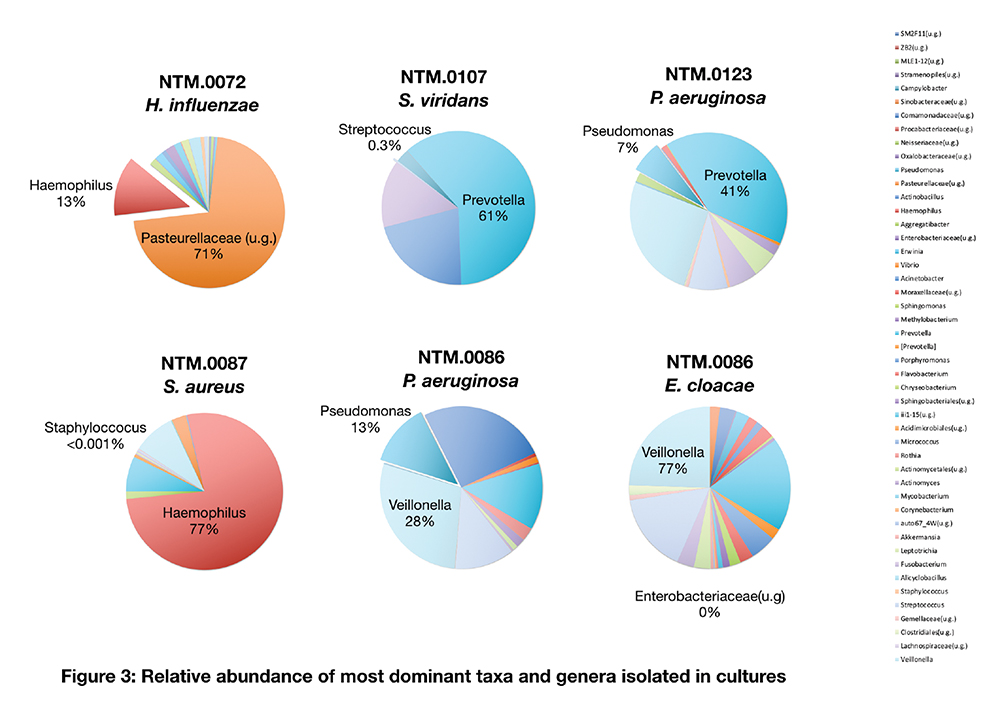
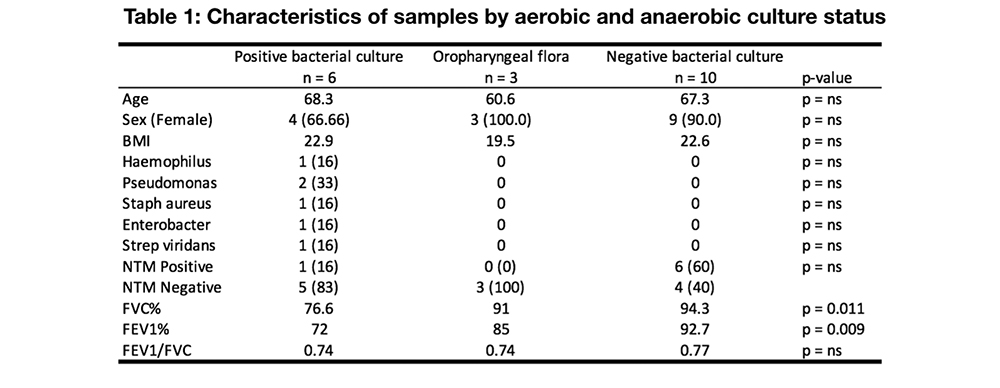
Background:
Recent data suggests that in patients with bronchiectasis, identification of at least one pathogen in chronic infection is about 51%. Here, we compare culture results with culture independent assessment of the lower airway microbiota of patients with bronchiectasis.
Methods:
Nineteen patients with bronchiectasis underwent bronchoalveolar lavage via bronchoscopy. Fluid was sent for gram stain, aerobic/anaerobic culture, and mycobacterial culture. The microbiome was assessed by 16S rRNA gene sequencing. Alpha, beta, and taxonomic differences were evaluated between groups with different culture results.
Results:
6/19 subjects were culture positive for a pathogen, 3/19 had growth of oral flora, and the remaining showed no growth. Comparison of these three groups revealed lower alpha diversity of the lower airway microbiota of subjects with positive pathogen isolation. Beta diversity analysis based on weighted UniFrac demonstrated significant differences (PERMANOVA p=0.002) supporting compositional differences between the groups. The lower airway microbiota of subjects with culture positive for a pathogen was enriched with Haemophilus and Porphyromonas. Interestingly, in this cohort, none of the pathogens identified by culture was the dominant taxa in the lower airway microbiota.
Conclusions:
Utilizing culture-independent methods, we identified microbiota signatures associated with culture positivity for pathogens (e.g. decreased alpha diversity). However, the dominant taxa of those with culture positivity did not correlate with the bacteria isolated. This data suggests that pathogenesis may be mostly related to functional aspects of each bacteria rather than numeric abundance within the microbial community. In addition, culture independent assessment may provide further insights into the role of organisms that are frequently ignored when relying on culture techniques.
Markers of Non-Cystic Fibrosis Bronchiectasis Disease Severity and Nutrition in the United States Bronchiectasis Research Registry
Authors: Katherine A. Despotes, MD1; Radmila Choate, MPH2; M. Leigh Anne Daniels, MD, MPH1; Peadar G. Noone, MD1; Bronchiectasis Research Consortium3
1University of North Carolina at Chapel Hill, Chapel Hill, NC; 2University of Kentucky, Lexington, KY; 3COPD Foundation
Background:
We sought to determine the relationship between nutrition and health outcomes in non-CF bronchiectasis (NCFB) using data from the US Bronchiectasis Research Registry (BRR), addressing the hypothesis that patients who are underweight have increased markers of disease severity.
Methods:
This was a retrospective, observational, longitudinal study using five-year follow-up data from the BRR. The main inclusion criterion was bronchiectasis confirmed on high resolution CT. Stratified analyses by BMI categories at baseline were performed using SAS v.9.4.
Results:
Out of 496 patients (64.6±13.3 years; 83.27% female) included in the study, at baseline 12.30% (n=61) were underweight (<18.5), 63.91% (n=317) had normal BMI (18.5=BMI<25), 17.34% (n=86) were overweight (25=BMI<30), and 6.45% (n=32) were obese (=30). More men were in the overweight and obese groups (25.58% and 43.75%, p<0.0001). Underweight patients had significantly lower lung function than the other weight groups (FVC 68.76+21.08%, p<0.0001 and FEV1 64.49±22.18%, p=0.0194). Of note, no significant difference existed among BMI groups in exacerbation frequency or hospitalizations. There were few reported patients with hemoptysis requiring intervention (n=4).
Conclusions:
Although US patients with NCFB who are underweight do have lower lung function than normally nourished or overweight patients, lower nutrition does not appear to drive what are considered the main markers of disease severity (hospitalization rates and exacerbations). Compared to the stereotype of the tall, thin, female patient with bronchiectasis, there are more male patients in the overweight and obese categories. The rate of hemoptysis requiring intervention is low compared to patients with cystic fibrosis.
Aspergillus Airway Colonization in Non-Cf Bronchiectasis Patients is not Associated with Disease Severity
Authors: Angela DiMango, MD1; Radmila Choate, MPH2; Bronchiectasis and NTM Research Registry Consortium*
1Columbia University Medical Center, New York, NY; 2University of Kentucky, College of Public Health, Lexington, KY
Background:
Effects of A. fumigatus colonization on health outcomes in non-CF bronchiectasis has not been well established.
Methods:
The Bronchiectasis Research Registry is a database of patients with non-CF bronchiectasis at 13 US sites. 2461 patients were analyzed. This study evaluated baseline demographics, pulmonary function, exacerbation, hospitalization frequency, microbiology, and treatment in patients with confirmed positive vs. negative growth of Aspergillus. Patients with ABPA were excluded. Groups were compared using t-test/Kruskall-Wallis test for continuous and Chi-squared test for categorical variables. Multivariate linear and logistic regressions were used to assess adjusted associations between Aspergillus growth and pre-bronchodilator FEV1 and exacerbation frequency. The significance level was set at 0.05.
Results:
Data from 648 subjects were reviewed. 179 subjects (28%) had documented growth of Aspergillus. Median age was 66.0 years; 81% were women. There was similar use of continuous oral suppressive antibiotics in both groups (35% in positive group and 29% in negative group, p=0.14). There was slightly more aerosolized antibiotic use in the aspergillus negative group (15% vs 9.5%, p=0.08). Macrolide use was 28% overall, similar in both. The use of oral/inhaled steroids was similar in both. Mean pre-bronchodilator FEV1% was 70.7+/-22.5% in the aspergillus negative group and 70.9 +/-20.3% in the positive group(p=0.91). 26% in the aspergillus negative group were hospitalized within 2 years compared with 18% in the positive group (p=0.03) with no difference in number of exacerbations overall.
Conclusions:
Aspergillus colonization in patients with bronchiectasis is not associated with suppressive antibiotic use, steroid use, disease severity or exacerbation frequency.
*Bronchiectasis and NTM Research Registry Consortium: Doreen Addrizzo-Harris, MD1; Timothy R. Aksamit, MD2;Alan Barker, MD3;Charles L. Daley, MD4;M. Leigh Anne Daniels, MD, MPH5; Edward Eden, MD6; Radmila Choate, MPH7; Angela DiMango, MD8; Kevin Fennelly, MD9; David E. Griffith, MD10; Margaret M. Johnson, MD11; Michael R. Knowles, MD5; David Mannino, MD7; Mark L. Metersky, MD12; Peadar G. Noone, MD5; Anne E. O’Donnell, MD13; Kenneth N. Olivier, MD, MPH9; Matthias A. Salathe, MD14; Andreas Schmidt, MD14; Byron Thomashow, MD8; Gregory Tino, MD16; Kevin L. Winthrop, MD, MPH3, 15
1New York University School of Medicine, New York, NY; 2Pulmonary Disease and Critical Care Medicine, Mayo Clinic, Rochester, MN; 3Department of Pulmonology, OHSU School of Medicine, Portland, OR; 4Division of Mycobacterial and Respiratory Infections, National Jewish Health, Denver, CO; 5University of North Carolina at Chapel Hill, Chapel Hill, NC; 6Icahn School of Medicine, Mt. Sinai West and Mt. Sinai St Luke’s Hospitals, Mt. Sinai, NY; 7Department of Preventive Medicine and Environmental Health, University of Kentucky, Lexington, KY; 8Columbia College of Physicians and Surgeons, Center for Chest Disease, New York, NY; 9National Heart Lung and Blood Institute, NIH, Bethesda, MD; 10University of Texas at Tyler, Tyler, TX; 11Mayo Clinic Florida, Pulmonary and Critical Care, Jacksonville, FL; 12Division of Pulmonary and Critical Care Medicine, University of Connecticut School of Medicine, Farmington, CT; 13Georgetown University Medical Center, Washington, DC; 14University of Miami Miller School of Medicine, Miami, FL; 15Department of Infectious Disease, OHSU School of Medicine, Portland, OR; 16University of Pennsylvania Perelman School of Medicine, Philadelphia, PA
Microbial Spectrum of Sputum in Patients (Pts) with Bronchiectasis (Be) in Stable Phase
Authors: Kateryna Bogatska, MD1; Valeriia Dmytrychenko, MD2; Kateryna Gahynova, MD, PhD2; Tetyana Kireyeva, MD1; Tetyana Pertseva, MD, PhD1
1Dnipropetrovsk Medical Academy of the Ministry of Health of Ukraine, Department of Internal Medicine, Dnipro, UKRAINE2; Dnipropetrovsk Medical Academy of the Ministry of Health of Ukraine, Department of Occupational Diseases and Clinical Immunology, Dnipro, UKRAINE;
Background:
The aim of the study was to determine the pathogens in sputum of stable patients with non-cystic fibrosis BE and evaluate their susceptibility to antimicrobial agents.
Methods:
Twenty women with BE were examined. The diagnosis of BE was confirmed by computed tomography. Isolation and identification of pathogens was carried by sowing on nutrient media. Susceptibility to antimicrobial agents was determined by disc-diffusion method.
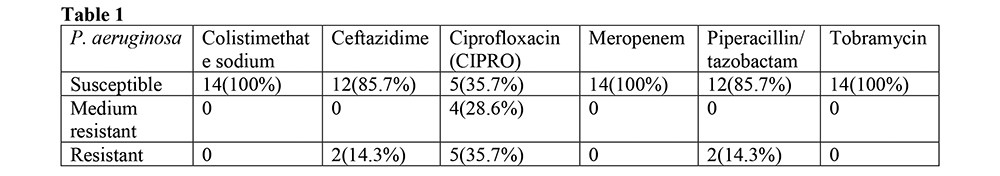
Results:
The age of pts was 51.0±4.3 years. 17 samples of sputum were obtained (purulent– 6 (35.3%), mucopurulent – 8 (47.1%), mucosalivary – 3 (17.6%)). At least one pathogen microorganism was detected in 14 (82.4%) samples. The combinations of pathogens were found in 3 (21.3 %) pts. The most common was P. aeruginosa – 14 (100%) alone or in combination with M. catarrhalis 1 (7.1%), K. pneumoniae 1 (7.1%) and A. fumigatus 1 (7.1%). Susceptibility profile of P. aeruginosa strains (strs) performed in table 1. There are 2 (14.3%) strains that were resistant to more than one group of antimicrobial (pyperatsyllyn/tazobactam, ceftazidime and CIPRO) and 7 (50.0%) showed pathogen resistance to only one drug (CIPRO).
Conclusions:
1. The most common pathogen in sputum of stable patients with BE is P. aeruginosa. 2. More than 64 % of the P. aeruginosa strains were resistant to variety of antibiotics, most frequently – to CIPRO. 3. In accordance with recent guideline antimicrobial therapy must be done for all BE patients with P. aeruginosa. This study allow to suggest that this treatment should be rather definitive than empiric.
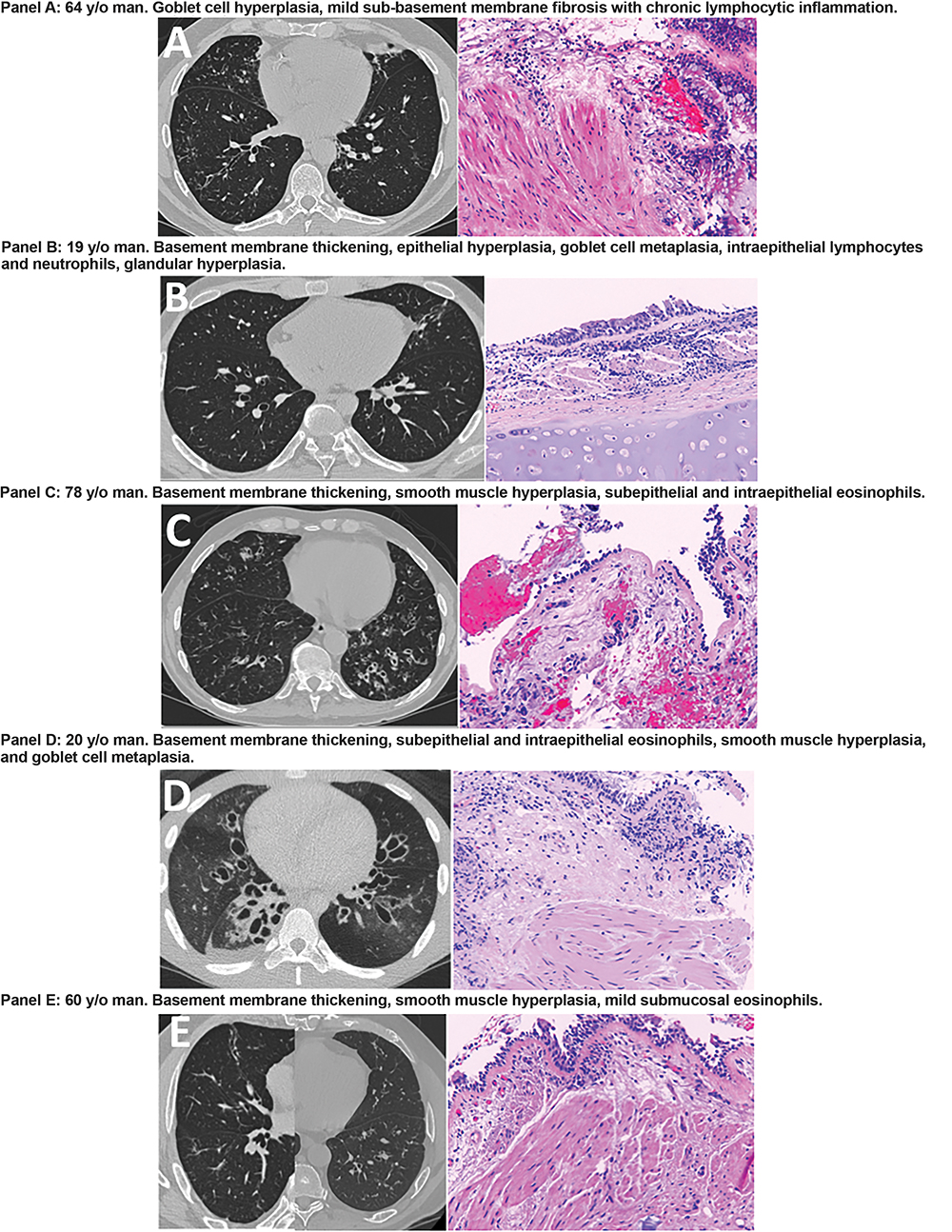
Histopathologic Manifestations of Idiopathic Bronchiectasis in an Endobronchial Biopsy Based Series
Authors: Sarah E. Gray, MD; Kyle D. Hogarth, MD; Aliya N. Husain, MD; Pamela J. McShane, MD
University of Chicago
Background:
Endobronchial biopsies (EBBx) have not been in the utilized in the systematic evaluation of bronchiectasis, and their role in the management of bronchiectasis is unknown.
Methods:
Patients had idiopathic bronchiectasis based on presence of dilated airways on HRCT, daily productive cough, exertional dyspnea and fatigue, and a history of bronchiectasis exacerbations. Patients underwent previously described systematic evaluation to exclude other causes of bronchiectasis. EBBx was performed using HRCT to guide biopsies in the area of bronchiectasis involvement.
Results:
Age at time of biopsy was 19 to 78. Four patients had no clinical history of asthma; one patient reported intermittent chest tightness but had borderline methacholine provocation responsiveness. FEV1 ranged from 38 to 98 percent predicted. On EBBx, three patients had smooth muscle hyperplasia along with subepithelial, intraepithelial, and submucosal eosinophils. The remaining two patients had goblet cell hyperplasia and intraepithelial lymphocytes and neutrophils. Basement membrane thickening was identified in 4 patients. In two of the three patients (aged 60 and 78) with eosinophils, inhaled corticosteroids were associated with clinical improvement in symptoms.
Conclusions:
Endobronchial eosinophils were more common than expected based on clinical history. Based on these results a diagnosis of concomitant asthma was made in three of five patients. This case series demonstrates the potential utility of EBBx in the evaluation of bronchiectasis.
The Association of Stenotrophomonas Maltophilia with Patient Characteristics and Outcomes in Bronchiectasis
Authors: Mark Metersky, MD1; Radmila Choate, MPH2;
1Health University of Connecticut School of Medicine, Farmington, CT; 2University of Kentucky, College of Public, Lexington, KY;
Background:
Stenotrophomonas maltophilia is a Gram negative non-fermenting rod sometimes cultured from patients with bronchiectasis. Another non-fermenter, Pseudomonas aeruginosa, is associated with unfavorable outcomes in patients with bronchiectasis and cystic fibrosis (CF). S. maltophilia may be associated with unfavorable outcomes in CF, but there are no data addressing this issue in bronchiectasis. We used the United States Bronchiectasis Research Registry (BRR) database to determine if S. maltophilia is associated with unfavorable outcomes in patients with bronchiectasis.
Methods:
Retrospective analysis of patients from the BRR with non-CF bronchiectasis, comparing baseline patient characteristics and selected outcomes among patients with a baseline culture growing S. maltophilia with: 1. patients whose baseline cultures grew no pathogens; 2. patients whose baseline cultures grew only pathogens other than S. maltophilia and P. aeruginosa; 3. patients whose baseline cultures grew P. aeruginosa but not S. maltophilia.
Results:
Among 1287 patients, 46 (4%) grew S. maltophilia at baseline. Patients who grew S. maltophilia were more likely to have had an exacerbation or to have been hospitalized for pulmonary disease during the prior two years than patients who had not grown S. maltophilia or P. aeruginosa. At the one year follow up visit, patients who had grown S. maltophilia were more likely to have been hospitalized for pulmonary disease. Generally, patients with S. maltophilia were similar to those with P. aeruginosa.
Conclusions:
Patients who had grown S. maltophilia tended to have more severe disease than patients who grew neither S. maltophilia nor P. aeruginosa.
Autoimmunity to Bactericidal/Permeability-Increasing Protein in Chronic Airway Infection of Bronchiectasis and Cystic Fibrosis Patients
Authors: Sladjana S. Gardner, PhD1; Rachel E. Meagher1; William F. Rigby, MD1; Jomkuan Theprungsirikul1; Kevin L. Winthrop, MD, PhD2
1 Geisel School of Medicine, Dartmouth College, Hanover, NH; 2Oregon Health Sciences University-Portland State University, School of Public Health, Portland, OR
Background:
Recurrent infection with Pseudomonas aeruginosa affects bronchiectasis (BR, ~65%) and cystic fibrosis (CF, ~80%) patients and is associated with deteriorating lung function, morbidity, and mortality. The extraordinary permissiveness of BR and CF airways for P. aeruginosa is not understood. Autoantibodies to bactericidal/permeability increasing protein (BPI) have been reported in CF patients in association with P. aeruginosa. The precise relationship between P. aeruginosa infection and autoimmunity to BPI is unclear.
Methods:
Antibodies to BPI and to P. aeruginosa were measured in sera from two BR cohorts (n=58), a longitudinal retrospective BR cohort (n=34), and two adult and one pediatric CF cohorts (n=79) by ELISA and/or immunoblot. Antibody avidity and IgG subclass were investigated.
Results:
Across all cohorts, autoantibodies to BPI (BR 52-56%, adult CF 45-53%) were detected specifically in patients with an antibody response to Pseudomonas aeruginosa. Notably, anti-BPI IgG did not associate with Nontuberculous Mycobacterium (NTM) infection in BR, nor were they detected in pediatric CF patients. Anti-BPI IgG and anti-P. aeruginosa antibody titers tracked together over time. Anti-BPI IgG demonstrated as high avidity as anti-P. aeruginosa LPS and -tetanus toxoid IgG. Anti-P. aeruginosa LPS antibodies were mainly of the IgG2 subclass (88%) while anti-BPI autoantibodies were primarily of the IgG1 subclass (88%).
Conclusions:
Large subpopulation of BR and adult CF patients develop autoantibodies to BPI. Autoreactivity to BPI develops in the context of the immune response to P. aeruginosa, independently of CFTR. Antibody avidity and IgG subclass usage suggest that anti-P. aeruginosa and anti-BPI antibodies arise via different mechanisms.
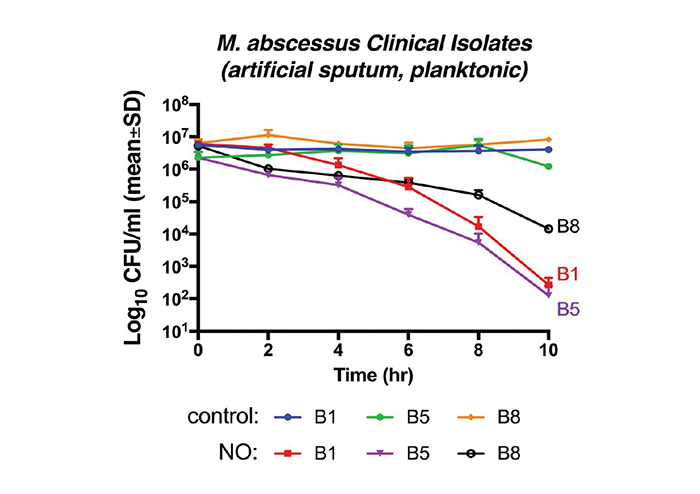
High-Dose Inhaled Nitric Oxide as a Potential Therapy Against Mycobacterium Abscessus Lung Infection in Cystic Fibrosis
Authors: Kristijan Bogdanovski1; Abdi A. Ghaffari, PhD2; Kenneth N. Olivier, MD, MPH1; Joas L. da Silva, PhD1; Adrian M. Zelazny, PhD3
1National Heart, Lung and Blood Institute, NIH, Bethesda, MD; 2AIT Therapeutics Harrison, NY; 3NIH Clinical Center, Bethesda, MD
Background:
Mycobacterium abscessus (MAB) is an emerging, multidrug-resistant (MDR) nontuberculous mycobacterium (NTM) with limited treatment options. Exogenous high-dose nitric oxide (NO) has anti-bacterial activity against a broad-spectrum of bacterial species, including Mycobacterium smegmatis. In this study, we investigate whether high-dose NO exhibits antibacterial activity against MDR MAB strains in vitro.
Methods:
A continuous horizontal-flow NO delivery system was used to treat MAB with specific doses of NO. Time-kill assay was performed in saline, 7H9, or artificial sputum media (106 CFU/mL in 2mL) to assess NO bactericidal activity against MAB. Samples were cultured on 7H11 agar every 2hr followed by CFU analyses.
Results:
Treatment at 250ppm and 400ppm NO achieved 100% kill in B1 strain cultured in saline after 6hr and 2hr, respectively. In artificial sputum, time-kill curves for B1, B5, and B8 strains revealed 4.2, 4.0, and 2.8 Log10 reductions, respectively, following 10hr treatment with 250ppm NO. The absolute values of MAB time-kill curve slopes, calculated by a non-linear regression model, were significantly higher in treated group (250ppm NO) compared with the controls (B1 p=0.013; B5 p=0.0008, B8 p=0.0011). All controls were treated with medical air only under the same conditions.
Conclusions:
These findings demonstrate the antibacterial activity of exogenous 250ppm NO against MDR MAB clinical isolates in vitro. In our opinion, further evaluation of inhaled NO therapy as a potential anti-mycobacterial agent in NTM lung infections is warranted.
Figure 1
Health-Related Quality of Life in Bronchiectasis Patients with Nontuberculous Mycobacterial Disease
Authors: Kieren Brown, MD1; Lucy Burr, MD2; Enna Stroil-Salama3; Lucy Morgan, MD, PhD4; Rachel Thomson, MD, PhD1
1Gallipoli Medical Research Institute, University of Queensland, Brisbane, AUSTRALIA; 2Mater Hospitals and Health Services, South Brisbane, AUSTRALIA; 3QLD Lung Foundation Australia, Milton, AUSTRALIA; 4Concord Repatriation General Hospital, Concord, AUSTRALIA
Background:
Pulmonary nontuberculous mycobacterial (NTM) infection is an increasingly recognised cause of morbidity, health care utilisation and impaired health-related quality of life.
Methods:
This study compares bronchiectasis patients with and without pulmonary NTM infection enrolled in the Australasian Bronchiectasis Registry (ABR). The Primary outcome was a comparison of Quality of life Questionnaire - Bronchiectasis (QOL-B) scores. NTM treatment status, Pseudomonas (PsA) co-infection, gender, exacerbation frequency and BMI were included in sub analyses.
Results:
Of 968 ABR enrolled patients, 320 (completed minimum data set) were selected for analysis, including 32 patients (10.0%) with active NTM infection and 48 (15.0%) with previous NTM infection. 67 (20.9%) had current or previous NTM treatment. Patients were of similar mean age (NTM current 72 years vs never NTM 68.52) and FEV1 % predicted (82.90 vs 76.57; p=0.435). Female patients dominated both groups (75.0% vs 71.6%); NTM patients had lower BMI (22.34 vs 26.66; p=0.011) but had similar frequency of exacerbations (0.88/year vs 1.40/year; p=0.192) and hospital admissions (0.53/year vs 0.50/year; p=0.986). Colonisation with PsA was greater in those with past NTM (29.2%) compared to current NTM (18.8%) and never NTM (23.8%). ANOVA comparison of means found no differences in QOL-B scores between NTM patients and those who had never had NTM, in all domains.
Conclusions:
QOL-B in patients with bronchiectasis does not appear to be influenced by NTM infection status in this Australian cohort. The lack of details of NTM disease severity and treatment status, particularly time since treatment completion, may have influenced findings.
Colonization with Pseudomonas Aeruginosa as a Predictor of Future Nontuberculous Mycobacteria Isolation
Authors: Timothy R. Aksamit, MD1; Amanda E. Brunton, MPH2; Sarah A. Siegel, MPH2; Kevin L. Winthrop, MD, MPH2
1Mayo Clinic, Rochester, MN; 2Oregon Health Sciences University-Portland State University, School of Public Health, Portland, OR
Background:
In a longitudinal analysis of 1,826 patients with non-cystic fibrosis bronchiectasis (NCFB) enrolled in the national US Bronchiectasis Research Registry (BRR), 63% were co-infected with nontuberculous mycobacteria (NTM). Among subjects with cultures collected during the baseline enrollment period, isolation of Pseudomonas species and Staphylococcus aureus was significantly less in patients with NTM versus patients without NTM. We therefore seek to understand the role of colonization with non-NTM microorganisms as predictors of NTM isolation.
Methods:
Bacterial and mycobacterial culture results were analyzed for patients with both baseline and annual follow-up data. We focused on three groups: 1) patients with at least one Pseudomonas aeruginosa isolate during the baseline window, but no documented history of NTM and no NTM isolates; 2) patients with at least one P. aeruginosa isolate and at least one NTM isolate during the baseline window; and, 3) patients with neither P. aeruginosa nor NTM isolates during the baseline window.
Results:
Over a five year follow-up period, group 1 isolated NTM on average less than group 2 (8.6% vs. 28.3%). Among patients with neither P. aeruginosa nor NTM isolates (group 3), mean NTM isolation was 15.4%. Mean prevalence of P. aeruginosa over the same follow-up period was 58.5%, 46.8%, and 39.9% respectively. At baseline, the distribution of NTM species within group 2 was predominantly M. avium intracellulare (67.5%), followed by M. abscessus (17.5%), and M. kansasii (1.3%).
Conclusions:
We found NCFB patients infected with P. aeruginosa without NTM may be associated with a lesser chance of NTM acquisition.
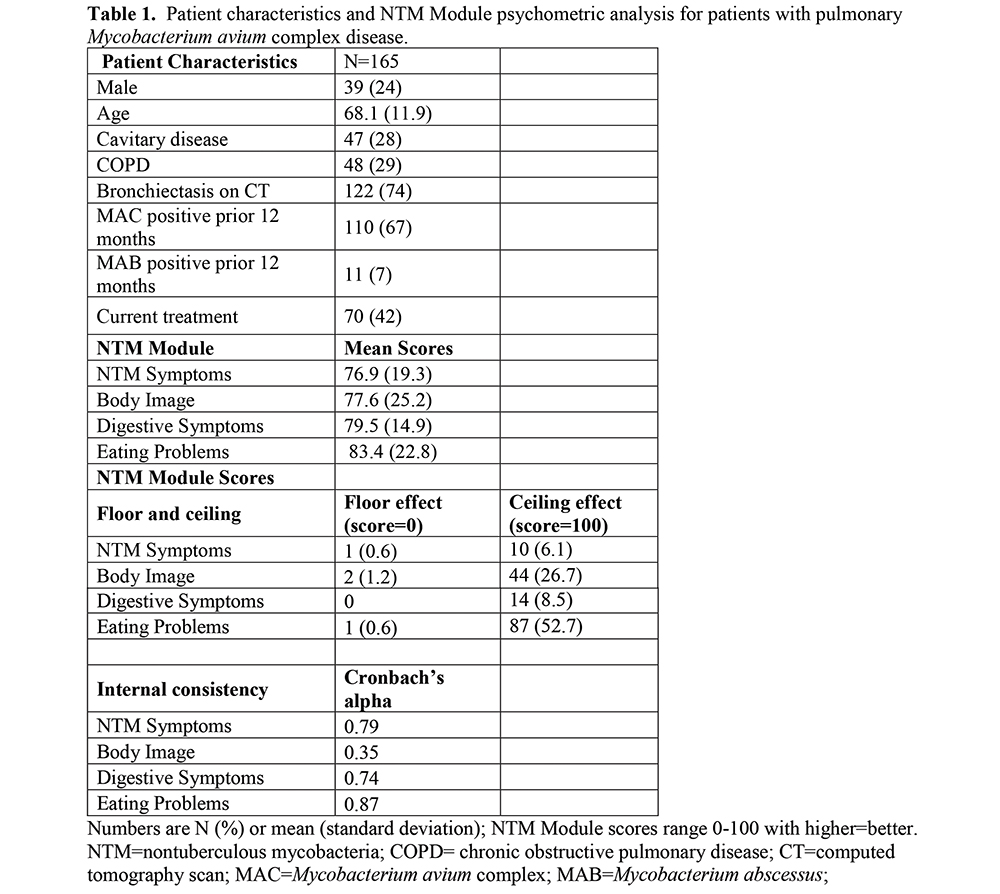
Psychometric Analyses of the NTM Module: First Patient-Reported Reported Outcome Measure for Pulmonary Nontuberculous Mycobacterial Disease
Authors: Emily Henkle, PhD1; Alexandra L. Quittner, PhD2; Greg Ranches, MD1; Kevin L. Winthrop, MD, MPH1
1Oregon Health Sciences University-Portland State University, School of Public Health, Portland, OR; 2Nicklaus Children’s Research Institute, Miami, FL
Background:
Patient-reported outcomes (PROs), including health-related quality of life (HRQoL), provide measures of key symptoms, daily functioning, and treatment response from the patient’s perspective. Here we describe psychometric properties of the recently developed NTM Module.
Methods:
This cross-sectional analysis included patients in the Northwest NTM Biobank with pulmonary M. avium complex (MAC) disease, who completed the NTM Module and had their clinical history abstracted from chart review. The NTM Module represents critical NTM symptoms; three other domains were mentioned by individuals with NTM as being affected by their infection (Body Image, Digestive Symptoms, and Eating Problems). Psychometric analyses included floor and ceiling effects and internal consistency. Test-retest reliability was calculated using intraclass correlation coefficients (ICCs) on a subset who completed a second administration 14 +/-1 days later.
Results:
A total of 165 patients were included. Domain scores were standardized (0-100; higher indicates better functioning). Scores ranged from 77 for NTM Symptoms to 83 for Eating Problems. Ceiling effects were noted for Body Image and Eating Problems. Internal consistency was very good for NTM Symptoms (Cronbach’s alpha 0.79), Digestive Symptoms (0.74), and Eating Problems (0.87), but was poor for Body Image (0.35). The ICC for test-retest reproducibility in 27 patients ranged from 0.72 (Body Image) to 0.94 (Eating Problems), which is excellent.
Conclusions:
The NTM Module generally performs well as a valid PRO for pulmonary MAC disease, although Body Image may be dropped. Further longitudinal evaluation of the NTM Module is needed to examine changes over time and response to treatment.
Lady Windermere’s Dudemere? Pulmonary NTM in Men
Authors: Jennifer H. Ku, MPH; Gregory Ranches, MD; Sarah A. Siegel, MPH; Kevin L. Winthrop, MD, MPH
Oregon Health Sciences University-Portland State University, School of Public Health, Portland, OR
Background:
Pulmonary non-tuberculous mycobacterial (NTM) disease occurs frequently among tall, thin women with pectus defects and/or scoliosis. This phenotype, dubbed Lady Windermere disease, is also found among men with pulmonary NTM disease.
Methods:
We performed an institution-wide electronic medical record search between 2003 and 2017. Thirty-two non-CF bronchiectatic males with NTM disease were identified using the ATS/IDSA criteria and compared with three comparator groups matched on age (±3 years): (1) 20 healthy males; (2) 15 male bronchiectasis patients without NTM; and (3) 33 bronchiectatic females with NTM.
Results:
Cases were 69 years of age at median (range 30, 94), mostly non-Hispanic white (84.4%), and had a median BMI of 22.6 (range 17.6, 35.3), significantly lower than bronchiectatic male patients without NTM [27.3 (range 18.4, 40.3), p=0.04] and healthy males [26.1 (range 21.2, 38.2), p=0.002]. Most common disease-causing species was mycobacterium avium-intracellulare complex (84.4%). Since consultation at OHSU, 22 (68.8%) received therapy for a median 90.0 weeks (range 10.9, 255.9). Mild deformity based on Haller Index in cases (15, 46.9%) was less common than in female bronchiectatic patients [25 (75.8%), p=0.02]. Kyphoscoliosis in cases (20, 62.5%) was more common than healthy males [8 (40.0%) p=0.045] and male bronchiectatic patients without NTM [4 (26.7%), p = 0.03].
Conclusions:
In male pulmonary NTM patients, kyphoscoliosis was more common than healthy males or bronchiectatic males without NTM; mild deformity was also common but less common than female bronchiectatic NTM patients. Further comparison in larger studies is needed to ascertain whether these phenotypes are characteristic of males with NTM disease.
Treatment of Refractory Mycobacterium Abscessus Lung Infection with Inhaled Intermittent Nitric Oxide
Authors: Sandra D. Macdonald, RN1; Kenneth N. Olivier, MD, MPH1; Ann M. Peterson, PhD2; Mark V. Rimkus, RT3; Chevalia J. Robinson, RN1
1National Heart, Lung and Blood Institute, NIH, Bethesda, MD; 2NIH Clinical Center, Bethesda, MD; 3AIT Therapeutics, Harrison, NY
Background:
Mycobacterium abscessus is an increasing problem particularly in cystic fibrosis (CF). Antibiotics are often ineffective and poorly tolerated. Prior studies suggest nitric oxide (NO) may have direct antimicrobial activity against lower airway pathogens including mycobacteria.
Methods:
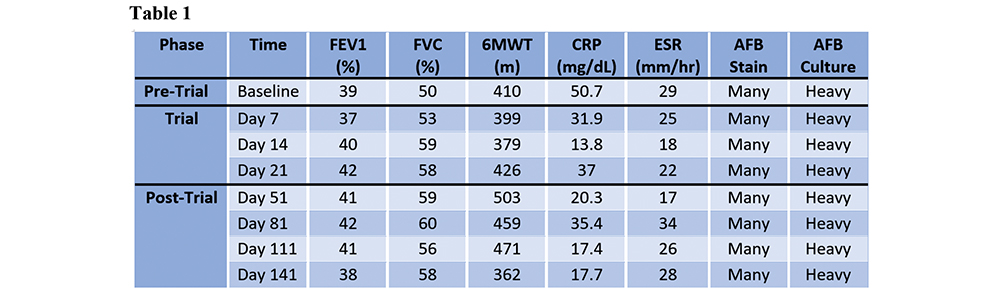
A 25 year old CF patient with an 8 year history of chronic M. abscessus unresponsive to multiple antibiotics and with deteriorating lung function was treated with intermittent, inhaled nitric oxide added to background antibiotics. The NO was administered via a novel, portable generator at 160ppm for 30 minutes 5 times/day for 2 weeks followed by 3 times/day for 1 week. Continuous SpO2, methemoglobin (MetHb), FiO2, NO, and NO2 were monitored with each treatment. Lung function, 6 minute walk (6MWT) distance, quality of life (CFQ-R), and sputum mycobacteriology were assessed before, during, and after NO treatment.
Results:
The patient tolerated the treatments well with MetHb levels never above 5.2% and stable SpO2 levels. Improvements were noted in FVC, 6MWT, and inflammatory markers (Table 1). No significant decreases in M. abscessus by smear or culture were seen. CFQ-R scores demonstrated large improvements including physical, vitality, health perceptions and respiratory domains. Following therapy she was able to complete her college degree and obtain a job.
Conclusions:
Inhaled nitric oxide was associated with clinical but not microbiologic improvement in a CF patient with refractory M. abscessus infection and may be a viable treatment option. Additional studies of optimal dosing are underway.
Vitamin D Deficiency Increases the Risk of Pulmonary Nontuberculous Mycobacteria in Cystic Fibrosis
Authors: Keira A. Cohen, MD; Mark T. Jennings, MD; Matthew N. Santos; Aniket Sidhaye, MD; Yuqing Sun, PhD
Johns Hopkins University School of Medicine, Baltimore, MD
Background:
Cystic fibrosis (CF) markedly increases the risk of pulmonary nontuberculous mycobacteria (NTM) infection and disease. Vitamin D is important for host control of Mycobacterium tuberculosis, but to date, few studies have explored the relationship between Vitamin D deficiency and NTM infection. Due to pancreatic exocrine insufficiency, individuals with CF are at high risk for Vitamin D deficiency, however, whether or not Vitamin D deficiency is an independent predictor of NTM infection in CF has not been explored. This study investigates the epidemiological and clinical risk factors for NTM infection with a focus on Vitamin D deficiency in this uniquely at risk population.
Methods:
We conducted a retrospective study of adults with CF cared for at the Johns Hopkins CF Center between January 2006 and December 2016. Routine serum measurements of Vitamin D 25-OH D3 were categorized as sufficient, mildly, moderately and severely deficient. A respiratory culture positive for NTM was the primary outcome measurement. Multivariable logistic regression and time-dependent Cox proportional hazards analyses were performed.
Results:
153 individuals were included in our study cohort. After adjusting for age, gender, BMI, CF-related diabetes, baseline pulmonary capacity and pseudomonas infection, we found that both moderate and severe vitamin D deficiency were significantly associated with increased risk of NTM infection in adults with CF.
Conclusions:
Vitamin D deficiency is associated with increased risk of pulmonary NTM infection in adult individuals with CF. Future investigation should explore whether or not aggressive Vitamin D repletion strategies can prevent NTM infection and disease in CF.
Perception for Risk and Disease Severity of NTM Lung Disease – Physician Survey in Germany, UK, Italy, France and The Netherlands
Authors: Marko Obradovic, PhD1; Roald van der Laan, PhD1; Jakko van Ingen, MD, PhD2; Dirk Wagner, MD, PhD3
1Insmed, Bridgewater Township, NJ; 2Radboud University Medical Centre, Department of Medical Microbiology, Nijmegen, THE NETHERLANDS; 3Universitätsklinikum Freiburg, Zentrum für Infektiologie und Reisemedizin & Centrum für Chronische Immundefizienz, Freiburg, GERMANY
Background:
Bronchiectasis is one of the strongest risk factors for nontuberculous mycobacteria (NTM) lung disease The objective of this study was to measure current perception of NTM risk and disease severity by physicians treating adult non-CF bronchiectasis patients (NCFB).
Methods:
An online survey with 280 physicians who spend at least 80% of their time in hospital setting and treated at least 10 adult NCFB patients in the previous 12 months was conducted in Germany, UK, Italy, France and the Netherlands.
Results:
87% of respondents (range 77-93%) consider adult NCFB patients to be at particular risk of contracting NTM. 53% of respondents (range 36% [Italy] - 68% [UK] estimated that less than 20% of NCFB patients will contract NTM, 28% of respondents were not able to estimate that risk. The risk of contracting NTM was ranked as average compared to other micro-organisms. Most respondents (88%) were aware that NTM lung disease when left untreated can lead to severe consequences, including progressive worsening of respiratory function, increased morbidity and more frequent hospitalizations. Approximately 13% (range 7% [Germany] - 22% [France]) of physicians did not see NTM lung disease having a significant impact on mortality risk.
Conclusions:
The results indicate that physicians treating adult NCFB patients are aware of the association between bronchiectasis and the risk of NTM lung disease. Majority of physicians perceive that NTM lung disease can lead to severe health consequences, although a minor part of physicians do not see that it lead to significant increase in mortality.
Screening for NTM Lung Disease in Adult Non-CF Bronchiectasis Patients – Physician Survey in Germany, UK, Italy, France and The Netherlands
Author(s): Marko Obradovic, PhD1; Roald van der Laan, PhD1; Jakko van Ingen, MD, PhD2; Dirk Wagner, MD, PhD3
1Insmed, Bridgewater Township, NJ; 2Radboud University Medical Centre, Department of Medical Microbiology, Nijmegen, THE NETHERLANDS; 3Universitätsklinikum Freiburg, Zentrum für Infektiologie und Reisemedizin & Centrum für Chronische Immundefizienz, Freiburg, GERMANY
Background:
Nontuberculous mycobacteria (NTM) lung disease has been increasing globally with bronchiectasis being a strong risk factor. The objective of this study was to evaluate the current screening practices of physicians for NTM disease in adult patients with non-CF bronchiectasis (NCFB).
Methods:
We conducted an online survey with 280 physicians treating adult non-CF bronchiectasis patients in Germany, UK, Italy, France and the Netherlands. Respondents had to spend at least 80% of their time in the hospital setting and manage N10 adult NCFB patients in previous 12 months.
Results:
85% (range: 80-88%) of surveyed physicians tested at least some of their NCFB patients for NTM infection. In total 51% (range: 40% [France] - 70% [Netherlands]) of NCFB patients managed by these respondents were tested for NTM infection and 17% of those (range: 8% [Netherlands] - 21% [Germany]) - were stated to have tested positive. The NTM infection was mostly suspected by physicians due to radiology exams or physical features of the lung (82%). Close to half of NCFB patients are tested for NTM on diagnosis or initial presentation. 64% of respondents (range: 52-76%) test for NTM in at-risk patients with NCFB at least once per year. Only 38% (range: 24-66%) of physicians test for NTM infection before initiating a macrolide monotherapy.
Conclusions:
Physicians need to be educated to screen patients with NCFB for NTM infection before initiating macrolide monotherapy. Recommendations for NTM-screening in these patients need to be validated, and further research on risk factors associated with NTM infection is warranted.