Running Head: Follow-up and COPD Readmissions
Funding Support: This research is not funded.
Date of Acceptance: November 30, 2018
Abbreviations: acute exacerbation of chronic obstructive pulmonary disease, AECOPD; chronic obstructive pulmonary disease, COPD; International Classification of Diseases, ICD; Charlson Comorbidity Index, CCI; odds ratio, OR; confidence interval, CI; Nationwide Readmissions Database, NRD
Citation: Budde J, Agarwal P, Mazumdar M, Braman SS. Follow-up soon after discharge may not reduce COPD readmissions. Chronic Obstr Pulm Dis. 2019; 6(2): 129-131. doi: http://doi.org/10.15326/jcopdf.6.2.2018.0149
Introduction
Visiting an outpatient provider shortly after hospital discharge for acute exacerbation of chronic obstructive pulmonary disease (AECOPD) may help prevent hospital readmissions. A retrospective cohort study of fee-for-service Medicare beneficiaries1 showed a significant reduction in hospital readmissions in those with a visit within 30 days. However, patients more likely to attend a follow-up visit were receiving care at nonteaching, for-profit, and smaller-sized hospitals, potentially indicating a source of bias. The benefit of rapid follow-up has been shown to be greatest among patients with multiple comorbidities.2 The purpose of this study was to determine whether a physician visit soon after discharge from a large, urban, academic hospital was associated with a lower risk of 30-day all-cause readmission in chronic obstructive pulmonary disease (COPD) patients, especially in those with multiple comorbidities.
Methods
We retrospectively examined electronic health records of all AECOPD-related hospitalizations at an urban, academic medical center for patients 40 years of age or older between June 2011 and June 2016. The diagnosis of AECOPD was based on International Classification of Diseases (ICD) 9-CM or ICD-10-CM coding. Hospitalizations were excluded if they resulted in transfer to another hospital, in-hospital mortality, discharge to hospice care, or discharge against medical advice. The study was approved under IRB-16-00808.
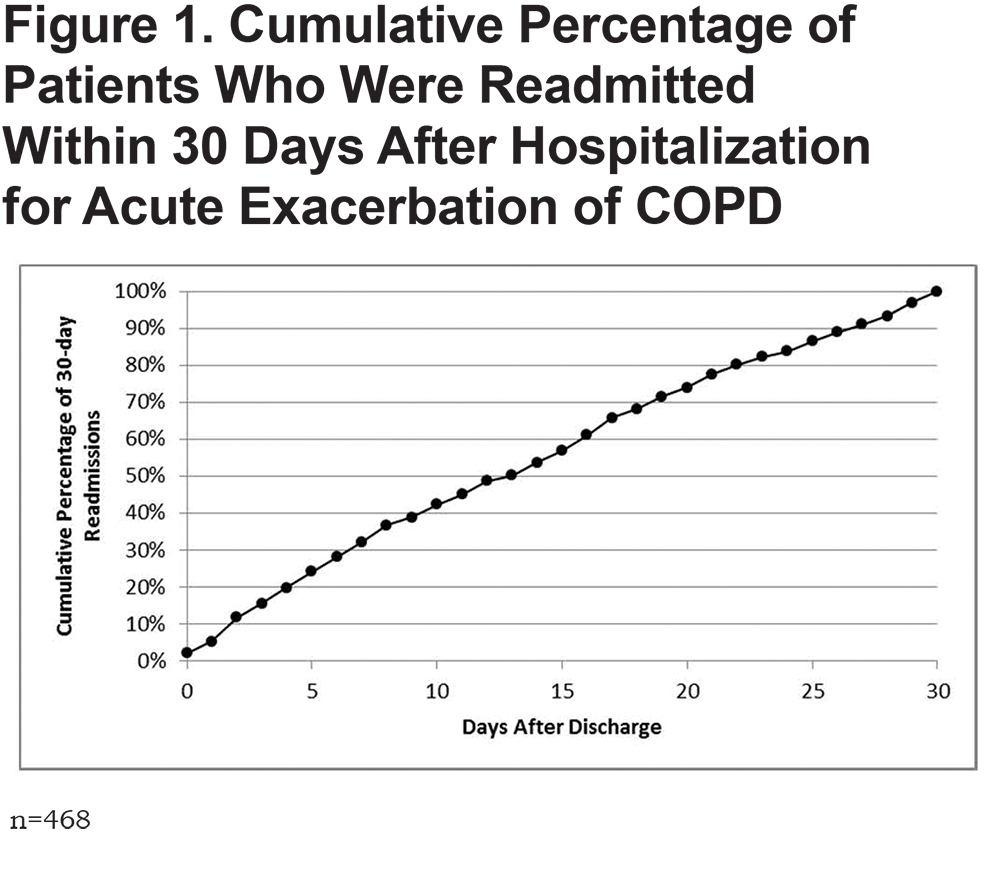
The primary outcome of interest was all-cause 30-day readmission following an index hospitalization; a patient could have multiple index hospitalizations. Follow-up visit was defined as a visit to a primary care provider or any medical subspecialist within 10 days of discharge. Adjusted generalized linear mixed models were estimated to explore whether age, race, gender, primary payer, smoking status, alcohol use, number of chronic conditions as defined by the Charlson Comorbidity Index (CCI),3 and presence of a follow-up visit were associated with readmission risk. The cumulative proportion of 30-day readmissions occurring each day after discharge is calculated. We looked for effect modification by CCI, which was chosen a-priori. A 2-tailed P-value of 0.05 was considered significant. All analyses were conducted using Statistical Analysis Software version 9.4.
Results
There were 2653 index hospitalizations, 17.7% of which resulted in a 30-day readmission. In the multivariate analysis, patients with CCI ≥ 2 were more likely to be readmitted2 as compared to those with lower index (odds ratio [OR] = 2.4, 95% confidence interval [CI] 1.5, 3.9). A total of 644 individuals (24.3%) had follow-up within 10 days of discharge. Of the 30-day readmissions, 42% occurred within 10 days of discharge [Figure 1]. Attending a follow-up visit was not associated with 30-day readmission risk (adjusted OR 1.14; 95% CI 0.89, 1.47), even among patients with CCI ≥ 2 (OR = 1.09; 95% CI 0.84, 1.40).
Discussion
We did not find an association between early physician follow-up and risk of 30-day readmission. A study using the Nationwide Readmission Database (NRD)4 showed that early readmission for AECOPD was associated with Medicaid payer status, lower household income, and higher comorbidity burden, all common to the population served by large urban academic hospitals. In the NRD study, 29.9% of readmissions were within the first 7 days; in ours, 32% occurred by day 7. This high proportion of patients admitted within the first week suggests that an intervention targeted at early follow-up may already be too late.
We did confirm that comorbidity burden is a predictor of readmission risk. However, predictors of readmission also include socioeconomic status and education level.5 These are difficult targets for short-term intervention. This study is a reminder of the need for a comprehensive approach to COPD.6 While short-term follow up may benefit some patients, interventions such as patient/caregiver education, pulmonary rehabilitation, advice on smoking cessation, inhaler use, and an exacerbation action plan, are likely the best approach to reduce readmission risk.1
1. Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010; 170(18):1664-1670. doi: https://doi.org/10.1001/archinternmed.2010.345
2. Jackson C, Shahsahebi M, Wedlake T, DuBard CA. Timeliness of outpatient follow-up: an evidence-based approach for planning after hospital discharge. Ann Fam Med. 2015;13(2):115-122. doi: https://doi.org/10.1370/afm.1753
3. Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676-682. doi: https://doi.org/10.1093/aje/kwq433
4. Jacobs DM, Noyes K, Zhao J, et al. Early hospital readmissions following an acute exacerbation of COPD in the Nationwide Readmissions Database. Ann Am Thorac Soc. 2018;15(7):837-845. doi: https://doi.org/10.1513/AnnalsATS.201712-913OC
5. Eisner MD, Blanc PD, Omachi TA, et al. Socioeconomic status, race and COPD health outcomes. J Epidemiol Community Health. 2011;65(1):26-34. doi: https://doi.org/10.1136/jech.2009.089722 jech-2009
6. Braman SS. Hospital readmissions for COPD: we can meet the challenge. Chronic Obstr Pulmon Dis. 2015;2(1):4-7. doi: https://doi.org/10.15326/jcopdf.2.1.2015.0130