Running Head: Physical Activity in COPD After Hospitalizations
Funding Support: Dr. Prieto-Centurion was funded by National Institutes of Health grants (K23HL130524 and R25HL126146).
Date of Acceptance: September 13, 2019
Abbreviations: chronic obstructive pulmonary disease, COPD; interquartile range, IQR; incremental shuttle walk test, ISWT; Patient-Reported Outcomes Measurement System, PROMIS; standard deviation, SD; body mass index, BMI; kilograms per square meter, kg/m2; forced expiratory volume in 1 second, FEV1; number of participants with missing information, m
Citation: Prieto-Centurion V, Casaburi R, Coultas DB, et al. Daily physical activity in patients with COPD after hospital discharge in a minority population.
Chronic Obstr Pulm Dis. 2019; 6(4): 332-340. doi:
http://doi.org/10.15326/jcopdf.6.4.2019.0136
Introduction
Low physical activity is common in patients with chronic obstructive pulmonary disease (COPD) and is associated with increased morbidity and mortality.1-3 Pulmonary rehabilitation after hospital discharge has been shown to improve multiple outcomes in patients with COPD, but its impact is limited due to low levels of participation.4,5 A recent study of Medicare patients found that less than 3% of patients start pulmonary rehabilitation within 12 months of hospital discharge and that approximately 90% of them do not complete it.6 Limited availability of pulmonary rehabilitation programs, as well as transportation and financial difficulties have been identified as common barriers.7,8 Minority and low-income patients with COPD have more barriers to participation in pulmonary rehabilitation programs and have a higher likelihood of poor outcomes after hospital discharge.9,10 Physical activity promotion interventions may be feasible and pragmatic for underserved patients with COPD recently discharged from the hospital, but evidence for their effectiveness is lacking. To inform the design of a home-based physical activity promotion program for patients with COPD recently discharged from a minority-serving hospital, we conducted a cohort study to evaluate objectively measured levels of daily physical activity and patient-reported outcome.
Methods
This was a 12-week, prospective cohort study of patients with a physician diagnosis of COPD recently hospitalized (≤ 12 weeks since hospital discharge) for respiratory symptoms at an academic medical center and minority-serving institution located in Chicago, Illinois. As less than 2% of patients with COPD enroll in pulmonary rehabilitation after hospital discharge, we selected a 12-week enrollment window after hospital discharge to identify a feasible timeframe for participants to initiate a home-based physical activity promotion program.6 Additional eligibility criteria included physical ability to walk and no medical contraindications to participation, as determined by the patient’s physician. Electronic health records were screened to identify hospitalized patients with a diagnosis of COPD or patients attending the outpatient clinics who had been recently hospitalized. Written informed consent was obtained from all study participants. The study was approved by the Institutional Review Board at the University of Illinois at Chicago.
Daily physical activity was recorded over a 12-week period using either wrist-based (Fitbit Charge HR) or “clip-on” (Fitbit Zip) Bluetooth-enabled pedometers, which allow remote physical activity data collection.11,12 Clip-on pedometers were preferentially used for patients in whom there was a concern about accuracy of wrist-based pedometers (e.g., use of a rolling walker that limited hand motion during normal walking).13 Daily physical activity was measured as the mean daily step counts over each 7-day period. At least 4 days per week with wearing time ≥ 8 hours were required for a valid assessment.14 Presence of heart rate data and intra-day time gaps between steps was used to calculate the pedometer wear time.
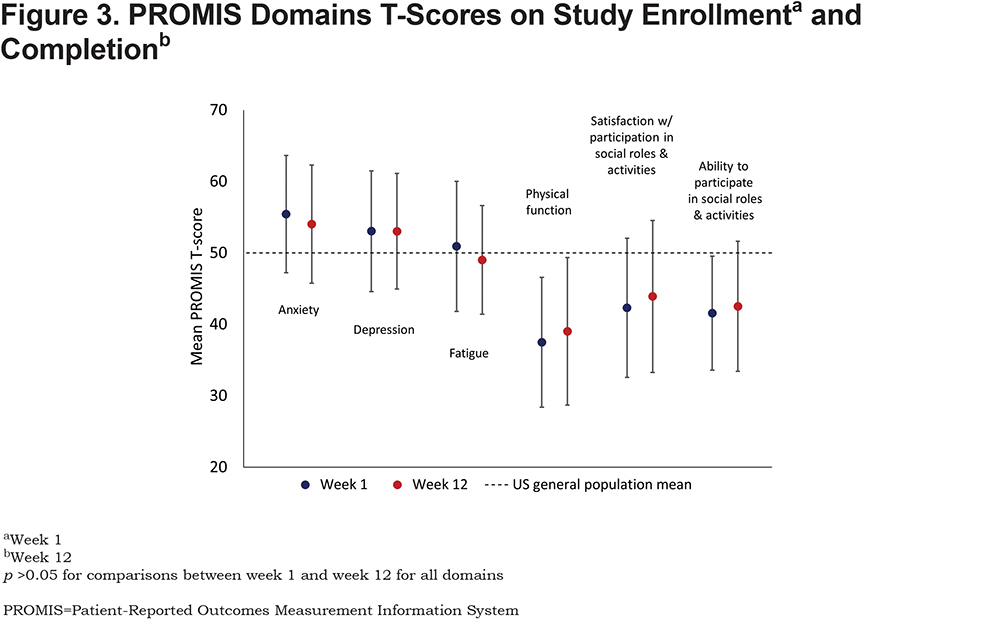
The incremental shuttle walk test (ISWT), a measure of maximal functional exercise capacity, was performed at the enrollment visit.15 Participants also reported on their health care utilization (i.e., all-cause hospitalizations) and multiple domains of health using the Patient-Reported Outcomes Measurement Information System (PROMIS), including physical function, fatigue, anxiety, depression, ability to participate in social roles and activities, and satisfaction with social roles and activities.16 PROMIS scores are standardized such that the U.S. national population has a mean T-score of 50 units with a standard deviation (SD) of 10 units. Higher T-scores indicate more of the concept being measured, i.e., a higher PROMIS fatigue T-score indicates worse fatigue whereas a higher PROMIS physical function T-score indicates better physical function. A difference in T-scores of ≥ 5 units (i.e., 0.5 SD) was considered clinically meaningful.17 Pearson’s r was used to establish correlations between mean daily step counts and time from hospital discharge to study enrollment. Wilcoxon rank sum tests were used to compare differences in mean daily step counts according to health care utilization and functional capacity. Wilcoxon signed rank tests were used to compare time-related changes in patient-reported outcomes. Analyses were performed using STATA software package, release 15.1 (Stata Corp Inc, College Station, Texas).
Results
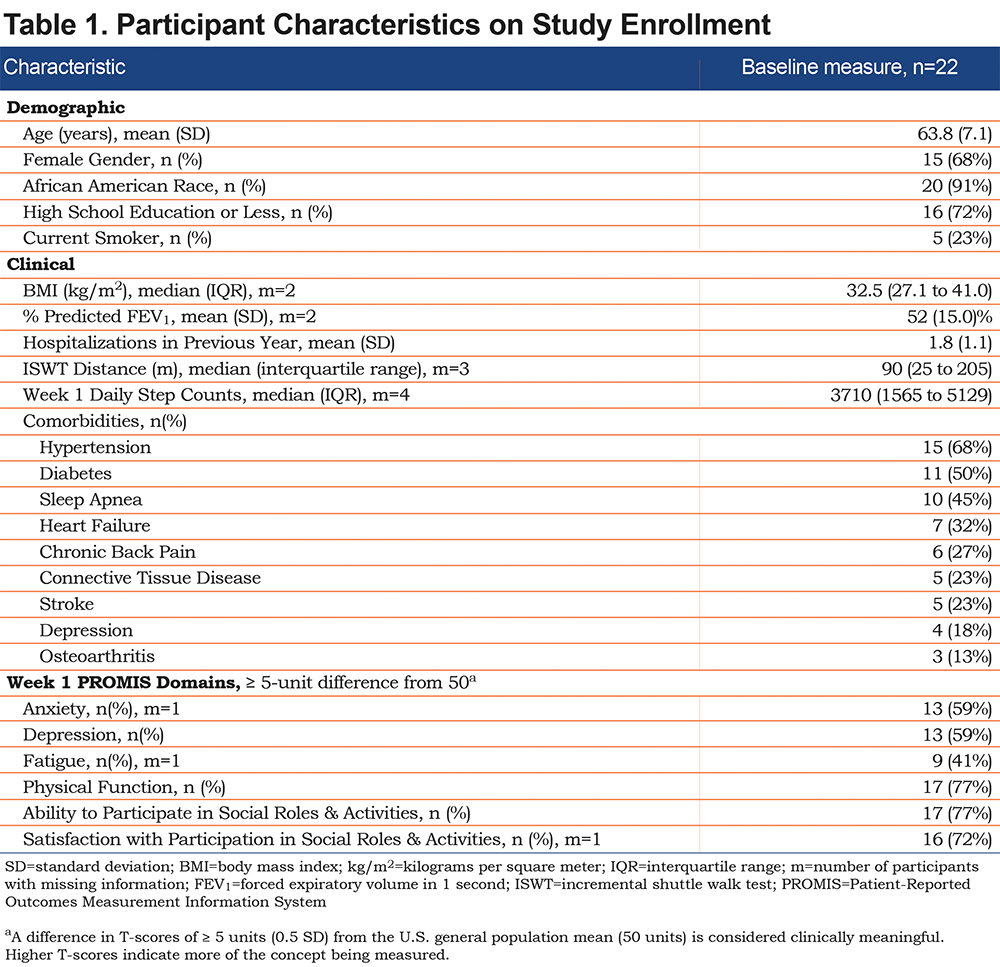
Twenty-two patients were enrolled at a median (interquartile range, [IQR]) of 14 (7 to 29) days after hospital discharge (Table 1). Participants had a mean (SD) age of 63.8 (7.1) years, were predominantly women (68%), African American (91%), and had no more than a high school education (72%). Nine participants were rehospitalized and 3 died during the follow-up period. Comorbidities were common among the participants, including those associated with chronic pain (45% reported connective tissue disease, osteoarthritis or chronic back pain) or limited mobility (23% reported a previous stroke). Additionally, some of the comorbidities reported by participants have symptoms that can either overlap with or exacerbate COPD (e.g., heart failure, perception of dyspnea in patients with comorbid depression). Participants had a median (IQR) ISWT distance of 90 (25 to 205) meters. On enrollment, the majority of participants reported physical function (77%), ability to participate in social roles and activities (77%), and satisfaction with social roles and activities (72%) T-scores significantly lower than the U.S. general population.
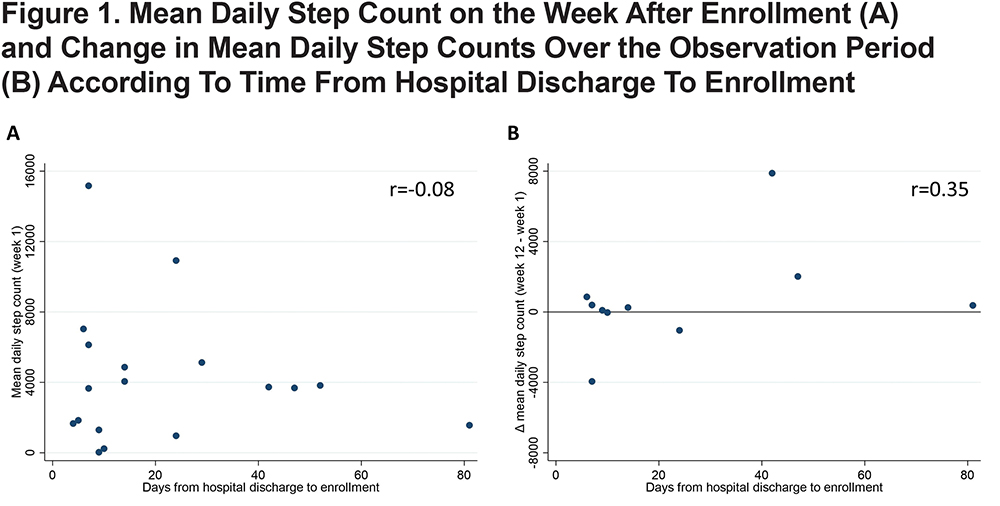
The median daily step count (IQR) in the first week after enrollment (week 1) was 3710 (1565 to 5129) steps. The median within-person change in daily step count (IQR) from week 1 to week 12 was 314 (-30 to 858) steps (p=0.28). In addition, the within-person correlation of week-to-week daily step counts was high (r ≥ 0.75), indicating limited variability in daily physical activity over the 12 weeks of observation. Time from hospital discharge to enrollment was not correlated with mean daily step counts on week 1 (r= -0.13; Figure 1, Panel A) and only weakly correlated with the change in mean daily step counts from week 1 to week 12 (r= 0.37; Figure 1, Panel B).
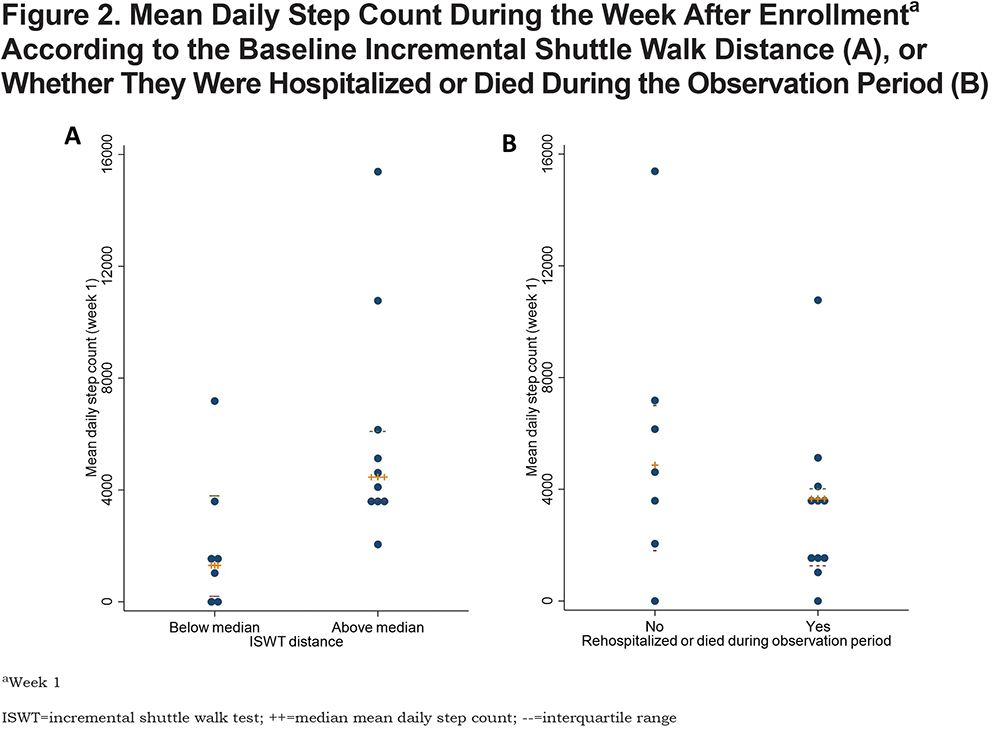
Mean daily step counts during week 1 were significantly lower among participants with ISWT distances below the median value than those with distances above the median (1230 versus 4459 steps per week, p=0.02; Figure 2, Panel A). Mean daily step counts during week 1 were also lower among participants who were rehospitalized or died during the study period than those who were not, although this difference was not statistically significant (3660 versus 4864 steps per week, p=0.26; Figure 2, Panel B). Compared to week 1, there was no significant difference in any of the PROMIS domains T-scores at week 12 (p >0.05 for all measures; Figure 3).
Discussion
In predominantly African American patients with COPD, recently discharged from the hospital, we observed a wide range of mean daily step counts, but without significant within-person change over the 12-week observation period. These patients had a high rate of poor clinical outcomes following hospital discharge. In addition, they had low functional exercise capacity as measured by the ISWT (age-adjusted normal ISWT distance for 60-69-year-old individuals is 788m).18 The observed mean daily step counts and ISWT distance was more than the minimal clinical important difference (1100 steps per day and 47.5 meters, respectively) and lower than that observed in previous studies of patients with stable COPD.19-22 A high proportion of participants also reported limited physical or social health, as recorded by several PROMIS domains, without any significant change over the observation period. We did find an association between higher ISWT distance and higher mean daily step counts. This observation is consistent with the concept that physical conditioning, a physiologic characteristic, is a significant determinant of a behavior, daily physical activity, in this population.
These observations have implications for the design of programs to improve physical activity and outcomes following hospital discharge in patients with COPD. First, although these patients have variable levels of physical activity after hospital discharge, a large majority of patients reported limited physical and social functioning. Therefore, to be responsive to the needs of these patients, physical activity promotion programs need to be flexible to allow participation of patients with markedly different levels of physical activity on enrollment. Second, given the high prevalence of comorbidities and high baseline risk of poor clinical outcomes in this population, close collaboration with the patients’ health care providers is essential to address any potential changes in clinical status. Third, as we did not observe a significant association between daily physical activity and the time from hospital discharge to enrollment, patients who are beyond the immediate post-hospital discharge period may still benefit from physical activity promotion programs. The immediate post-hospital discharge period can be chaotic for many patients and their caregivers as they attempt to return to their normal routine.23 Additionally, although the risk for rehospitalization or death is highest within the first weeks after hospital discharge, this risk remains elevated for at least 1 year.24 Flexible timelines for enrollment in post-hospitalization physical activity promotion programs may allow inclusion of patients who otherwise may not have been able to participate. Third, although ISWT distance allows insight into the mechanisms by which a physical activity promotion program works, its implementation in clinical studies adds significant burden as participants usually need to attend in-person study visits for outcome collection. As mean daily step counts, remotely collected by wireless pedometers, were significantly associated with ISWT distance, they could serve as a behavioral marker of intervention progress.
The principal strength of this study is that we used validated and scalable measures to concurrently collect data on functional capacity, daily physical activity and patient-reported outcomes in a population at high risk for adverse outcomes. The study’s main limitation is the relatively small sample size. It is possible that a larger sample size would have allowed us to detect differences in daily physical activity in sub-groups of patients, such as those likely to be rehospitalized during the observation period, or to characterize the study population in more detail, such as identifying comorbidities associated with lower levels of physical activity. However, the sample size is within the generally recommended number of participants for early pilot studies and it provides important feasibility data for the design of physical activity promotion programs specific to this population.25,26 Another study limitation is that, as described in the methods section, participants in whom there was a concern about the accuracy of wrist-based pedometers were provided with clip-on pedometers. A recent systematic review found that Fitbit devices worn on the wrist or torso can, in the majority of cases, provide step count measurements comparable to research-grade accelerometers or pedometers. However, it is possible that between-person differences in mean daily step counts observed in the present study are partly due to differential accuracy between pedometers.27 Last, observations were conducted in patients discharged from a single minority-serving institution and may not be applicable to other populations of patients with COPD. However, this represents the first such characterization of an underserved and relatively understudied population. Additional studies would be needed to establish the baseline characteristics of other populations to design physical activity promotion programs targeted to their needs.
In conclusion, this cohort study showed daily physical activity levels to be highly variable among patients with COPD recently discharged from the hospital, but with little within-person change over a 12-week period. These observations highlight the need for the development of flexible physical activity promotion programs that can address the needs of a heterogeneous patient population.
Acknowledgements
We thank the patients and clinicians who assisted in the implementation of the study. We also thank members of the independent Data and Safety Monitoring Board (Sherita Chapman-Smith, MD; Kerri Morgan, PhD, and Meghan Lane-Falls, MD, MSHP).
Author Contributions: VP had full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. VP contributed to the study conception, data acquisition, analysis and interpretation, writing and revision of the manuscript. RC, DBC, MK, JM, and CSR contributed to the study conception, data interpretation, writing and revision of the manuscript. JJL and AMT contributed to the data acquisition and analysis, writing and revision of the manuscript. JK contributed to the study conception, data analysis and interpretation, writing and revision of the manuscript.
Declaration of Interest
Dr. Prieto-Centurion reports receiving grants from the National Institutes of Health/National Heart, Lung, and Blood Institute during the time of this study. Dr. Krishnan reports grants from the National Institutes of Health/Patient-Centered Outcomes Research Institute not related to this study and Dr. Tan reports a grant from the National Institutes of Health. All other authors have nothing to declare.