Running Head: Stress and Acute Care Use in COPD
Funding support: Trisha M. Parekh is supported by the 5T32HL105346-07 grant from the National Heart, Lung, and Blood Institute. Mark T. Dransfield is supported by the 1K24HL140108 grant from the National Heart, Lung, and Blood Institute.
Date of acceptance: February 4, 2020
Abbreviations: chronic obstructive pulmonary disease, COPD; social determinants of health, SDH; University of Alabama, UAB; emergency department, ED; forced expiratory volume in 1 second, FEV1; adjusted odds ratio, AOR; confidence interval, CI; socioeconomic status, SES; forced vital capacity, FVC; Perceived Stress Scale, PSS; modified Medical Research Council, mMRC; COPD Assessment Test, CAT; body mass index, BMI
Citation: Parekh TM, Cherrington AL, Bhatia S, et al. The association of low income and high stress with acute care use in COPD patients. Chronic Obstr Pulm Dis. 2020; 7(2): 107-117. doi: http://doi.org/10.15326/jcopdf.7.2.2019.0165
Online Supplemental Material: Read Online Supplemental Material (345KB)
Note: Part of this work was presented as an abstract at the American Thoracic Society 2019 International Conference in Dallas, Texas.
Introduction
In the next decade, chronic obstructive pulmonary disease (COPD) is projected to surpass ischemic heart disease as the leading cause of hospitalizations in the United States.1 Interventions developed to reduce COPD hospitalizations and re-hospitalizations have had only modest success and have largely focused on pharmacologic and non-pharmacologic treatments, clinical care processes, and discharge bundles,2 with a notable absence of focus on the social determinants of health (SDH). SDHs are defined as “the conditions in which we work and live” and include factors such as income, education, social support, transportation, access to health care, housing stability, and food security.1 SDHs and their associated health-risk behaviors account for 80% of the modifiable contributors to health outcomes.3,4 Disparities related to SDHs are clearly evident in COPD, where individuals of low socioeconomic status (SES) are more likely to smoke and have a higher frequency of exacerbations, greater disease severity, and increased mortality.5,6,7 Low SES individuals also frequently face other disadvantages of SDHs including poor access to health care, unstable housing, food insecurity, lack of transportation, and poor social support, all of which can contribute to chronic stress.8
Increased levels of psychological stress in individuals with inflammatory diseases including coronary artery disease, HIV, auto-immune diseases, and asthma have been associated with increased prevalence,9 progression,10 and exacerbation of disease.11 In asthma, maternal prenatal stress, work stress, and childhood stress have been associated with childhood asthma, poorer asthma control and quality of life, and increased risk for exacerbation following an acutely stressful event.11,12,13 However, there have been few studies that evaluate correlates of stress with outcomes in COPD. In a longitudinal study of healthy women, psychological distress was a predictor of chronic bronchitis (adjusted odds ratio [AOR] 2.00, 95% confidence interval [CI] 1.16–3.46), breathlessness (AOR 3.02, 95% CI 1.99–4.59), and decline in forced expiratory volume in 1 second (FEV1) (AOR 1.62, 95% CI 1.13–2.32) over a 3-year period.14 The prevalence of psychological distress is high in COPD, nearing 60% in a small cohort of hospitalized COPD individuals (n=92).15 A small clinical trial assessing the effects of a 12-month trial of montelukast therapy on individuals with perceived stress found that those with high stress (n=15) had higher levels of leukotriene B4, interleukin-8 and tumor necrosis factor-a compared to those with low stress (n=5), the levels of which were significantly lowered after therapy in the high stress group.16
Stress research has investigated the role of perceived stress in other inflammatory diseases17 however, there is limited research on the association of perceived stress with health outcomes in COPD. This information would be particularly valuable in the low-income population who frequently experience chronic stress and often use smoking as a coping mechanism,18 who may have higher levels of basal cortisol and catecholamines,19 and who contribute disproportionately to overall COPD disease burden and health care utilization.5 We hypothesized that in individuals with COPD: (1) there is an association between increased levels of perceived stress and higher frequency of acute care use, (2) those with high stress are more likely to be affected by disadvantages of SDHs, including low income, compared to those with low stress, and (3) there is an association between low income + high stress individuals and acute care use.
Methods
This study was a survey-based study of individuals with COPD at the University of Alabama at Birmingham (UAB). The UAB Institutional Review Board approved the study. Written consent was obtained from all participants and they received a $25 incentive for completing the survey.
Participants and Study Setting
Participants were included in the parent study if they had a clinical diagnosis of COPD and pulmonary function testing consistent with the diagnosis (FEV1/forced vital capacity [FVC] ratio < 0.70) and were able to read and write in English. We recruited participants from pulmonary clinics as well as the Lung Health Research Center at UAB between July 2017 and September 2018. Participants were initially screened through electronic medical records for spirometry results consistent with COPD prior to being approached for enrollment in the study. After confirming eligibility and providing consent, participants were asked to independently take a written survey that assessed various social and medical determinants of health. A study coordinator was available to answer questions if needed. For the current study, participants were included if they had complete data regarding income and stress level.
Income/Stress Groups
Participants were categorized into 2 groups based on stress level: (1) high stress and (2) low stress. Stress level was assessed by Cohen’s Perceived Stress Scale (PSS), a 10-item Likert scale instrument that is widely used in stress research (Cronbach's Alpha coefficient 0.78 from prior study; score range 0-40)20,21 and assesses perceived stress level over the prior month. We defined stress levels based on the median split of the cohort, a method used in seminal stress studies evaluating susceptibility to respiratory virus research,20,22 such that low stress individuals had a score of 0–16 while the high stress group consisted of scores of 17–40. Income was defined by the median split of income, such that low-income individuals reported < $2000 monthly total family income (approximately 200% of the 2018 federal poverty level)23 and high-income individuals reported ≥ $2000 income. Participants were categorized into 4 groups based on income and stress level: (1) high-income + low stress, (2) low-income + low stress, (3) high-income + high stress, and (4) low-income + high stress.
Definition of Covariates
Demographic characteristics, comorbidities, illicit drug use, and smoking history were self-reported. Level of dyspnea was assessed by the modified Medical Research Council (mMRC) dyspnea scale with a score of “0” indicating “breathless with only strenuous exercise” and a score of “4” indicating “too breathless to leave the house or breathless when dressing.”24 COPD-related symptoms were assessed by the COPD Assessment Test (CAT), an instrument with a score range of 0–40 with a higher score indicating worse symptoms.25 The Test of Adherence to Inhalers instrument assessed medication adherence.26 Transportation was assessed by the question “How do you usually get to your clinic appointments (own private vehicle, other private vehicle, public transport, walk/bike)?” Social support was assessed by the Social Support Survey which evaluates emotional support, tangible support, affection, positive interaction, and overall functional support.27 Food insecurity was assessed by the 6-item U.S. Household Food Insecurity Survey Module.28 The Ross Neighborhood Disorder scale was used to measure neighborhood disorder, with a higher score indicating increased disorder.29 Perceived discrimination was assessed by the Williams Everyday Discrimination Scale.30
Outcome Measures
Our primary outcome was acute care use which was defined as a COPD-related emergency department (ED) visit or hospitalization in the 2 years prior to study enrollment. Acute care use was self-reported with answers to the following questions: “In the last 2 years, how many times have you visited the ED (without a hospitalization) for your COPD?” and “In the last 2 years, how many times have you been hospitalized for your COPD?” Our primary outcome was dichotomous and included (1) no COPD-related ED visit or hospitalization and (2) one or more COPD-related ED visits or hospitalizations.
Statistical Analysis
We initially analyzed participants based on the 2 stress groups. Characteristics of participants in each group were compared using chi-square tests of association or t-tests as appropriate. A multivariable logistic regression model evaluated the association between stress and acute care use adjusted for demographic factors, smoking status and FEV1 as they are known to impact exacerbations. Inclusion of additional confounders was limited by our sample size. The magnitude of association was described as AOR with an accompanying 95% CI. We then used descriptive statistics to evaluate characteristics of SDHs between low and high stress groups. We performed an interaction analysis with median stress level * median income in determining acute care use which was not significant (OR, 95% CI, 0.75, 0.17–3.32). However, because stress can manifest differently in low-income populations who generally have higher levels of stress and fewer resources to effectively cope with stressors,8 we were interested in examining characteristics of the cohort in groups categorized by income and stress level. We analyzed the binary status of income and stress (4 groups) with descriptive statistics and comparison statistics, using one-way analysis of variance or Kruskall Wallis as appropriate, with p values generated from these tests. Finally, a multivariable model evaluated the association between the composite income + stress variable and acute care use. We used SPSS v.25 for all statistical analysis. All hypothesis testing was 2-sided with significance set at p <0.05.
Results
Of the 233 individuals who met spirometry criteria, 173 were approached and 148 consented to participate in the parent study. Those who were not approached were missed due to time constraints with only 1 study member performing recruitment. Of the 143 participants who completed the survey, 126 had complete income and stress data and were included in the current study. Table 1 displays the baseline characteristics of the study participants by stress group. The high stress group was more likely to be < 65 years old and female. No differences in race, current smoking, years of smoking, BMI, dyspnea, or lung function (FEV1%) by stress group were observed. There are no significant differences in comorbidities between the low and high stress groups, including anxiety and depression, with the exception of obstructive sleep apnea, which was higher in the high stress group (27% versus 11.5% in low stress; p = 0.03). The high stress group more frequently rated their health as “poor” and experienced lower quality of life as assessed by the CAT (mean score 24.9 versus 19.8; p < 0.001). Those with high stress had a higher incidence of overall use of acute care services in the prior 2 years (acute care use frequency, mean [standard deviation (SD)]: 2.59 [3.9] versus 0.86 [1.44]; p = 0.001). Results from our multivariable regression model revealed that those who experienced high stress had a 2.5-fold increased adjusted odds of acute care use (AOR, 95% CI, 2.51, 1.06–5.98) compared to low stress individuals after controlling for demographic and clinical factors (Table 2).
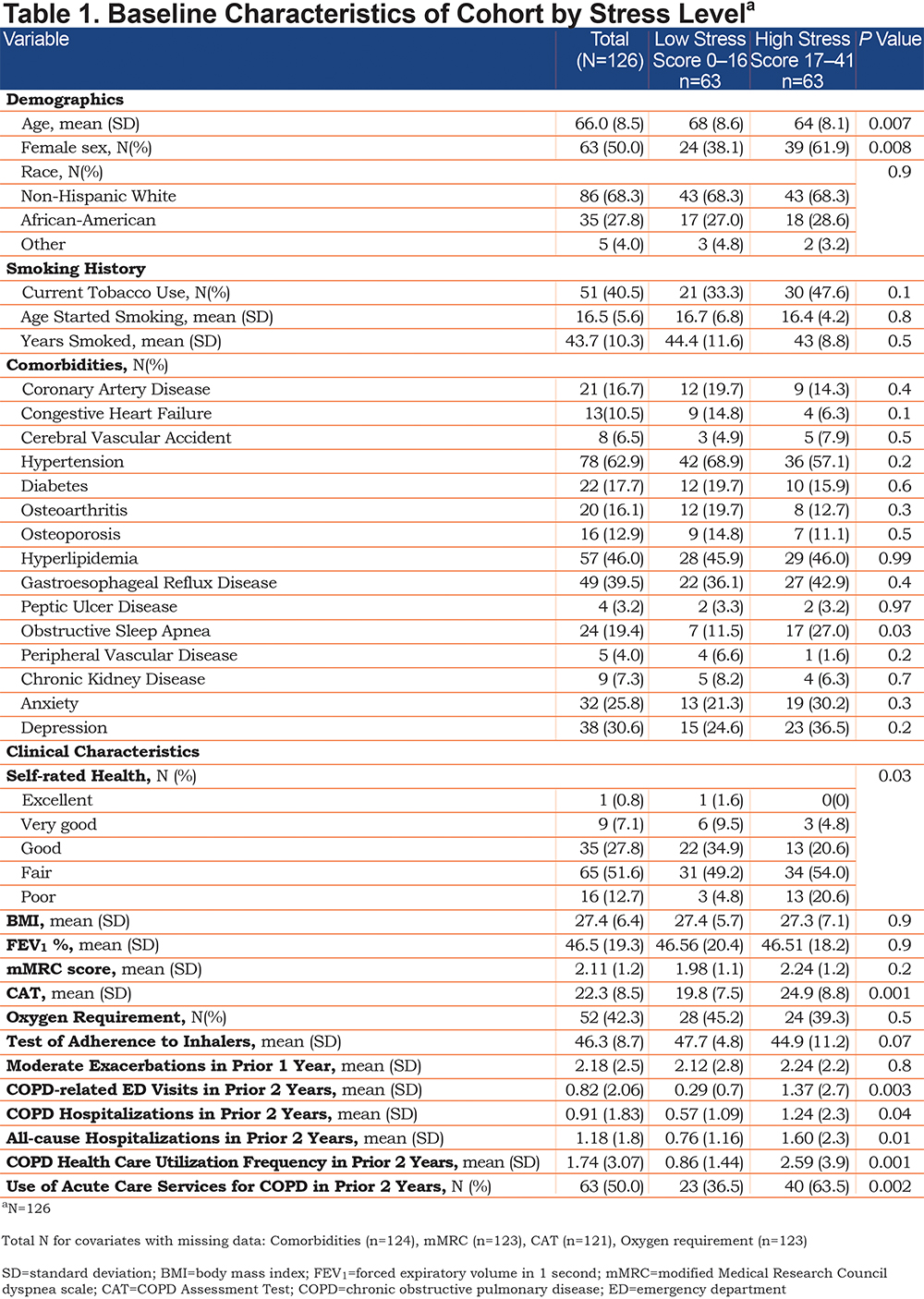
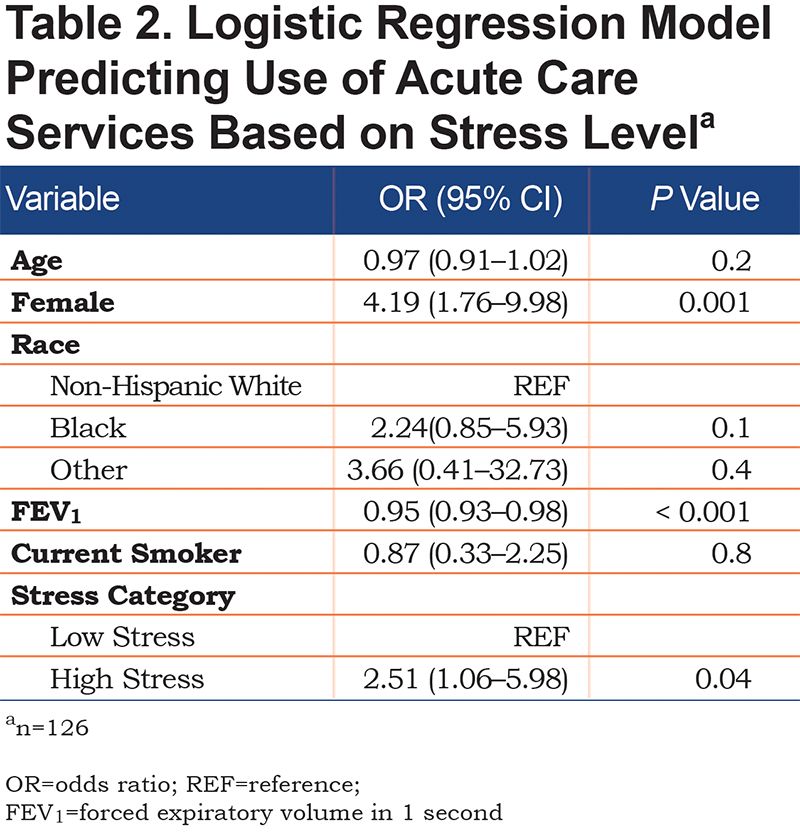
Table 3 displays the SDH characteristics of the low and high stress groups. Those who experienced high levels of stress had lower monthly income as well as difficulty affording mental, dental, and specialist care. The high stress group also had higher levels of neighborhood disorder and illicit drug use. There were no significant differences in social support although scores were numerically higher (more social support) in all components of the Social Support instrument for those with lower stress. Mean PSS score in the high stress group was 22.1 (SD 4.1) while mean PSS in the low stress group was 9.6 (SD 4.6).
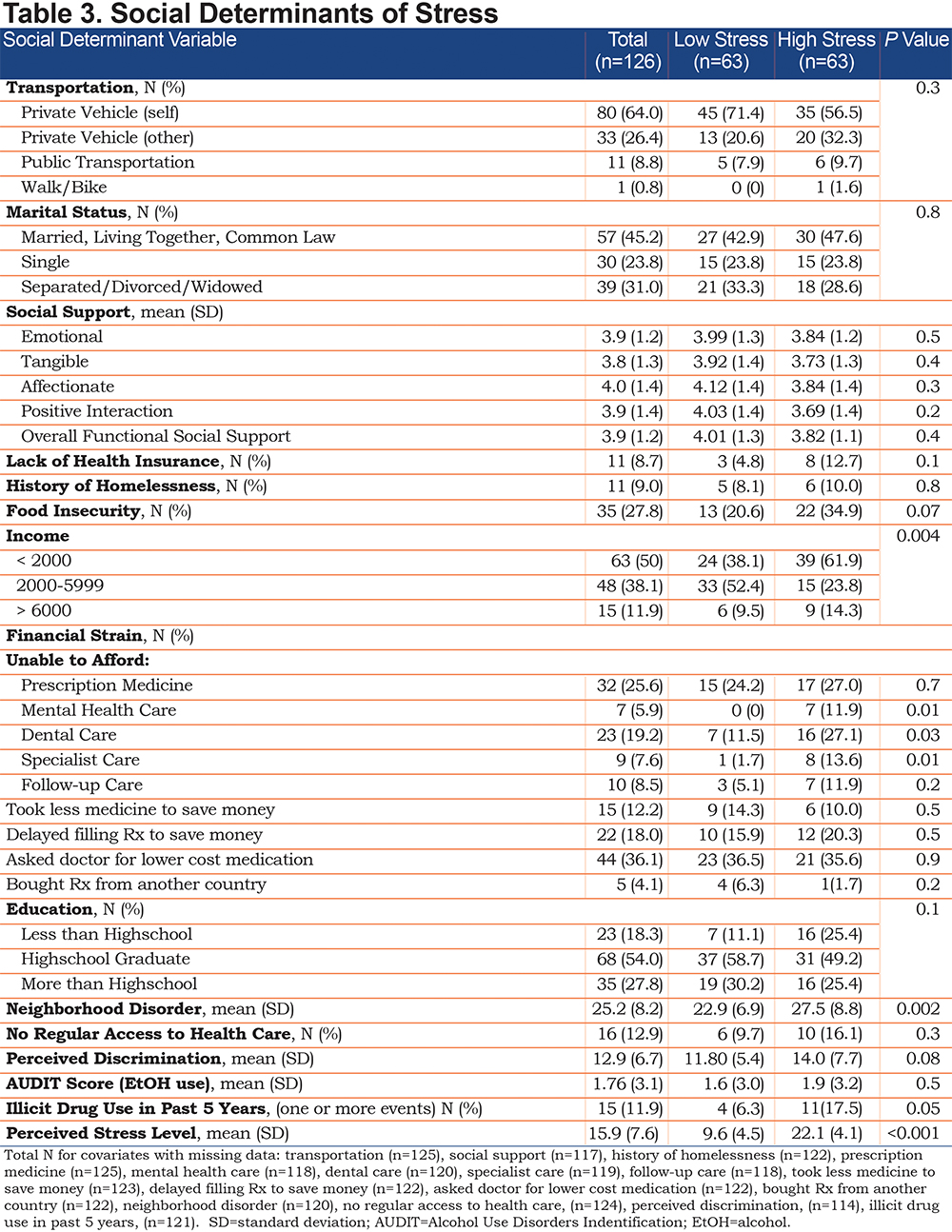
Supplemental Table 1 (in the online supplement)provides descriptive data of baseline characteristics of the 4 income + stress groups. The low-income + high stress group was more likely to be young, active smokers with a poor quality of life. Both high stress groups had high COPD acute care use frequency however, the low-income + high stress group had the highest number of individuals who utilized acute care services (Figure 1).The SDH characteristics of the 4 income + stress groups are displayed in Supplemental Table 2 (in the online supplement). The low-income + high stress group was least likely to own a car, have health insurance, or have education above high school. They were most likely to experience food insecurity, perceive discrimination, have a history of drug use, and live in neighborhoods with high levels of disorder. The high stress + high-income group was most likely to be married or living together. The low-income groups had lower social support scores compared to high-income groups and had difficulty accessing health care regularly. Compared to the low-income + low-stress group, those with low-income + high-stress were unable to afford prescription medicine, and mental, dental, specialist, and follow-up care.
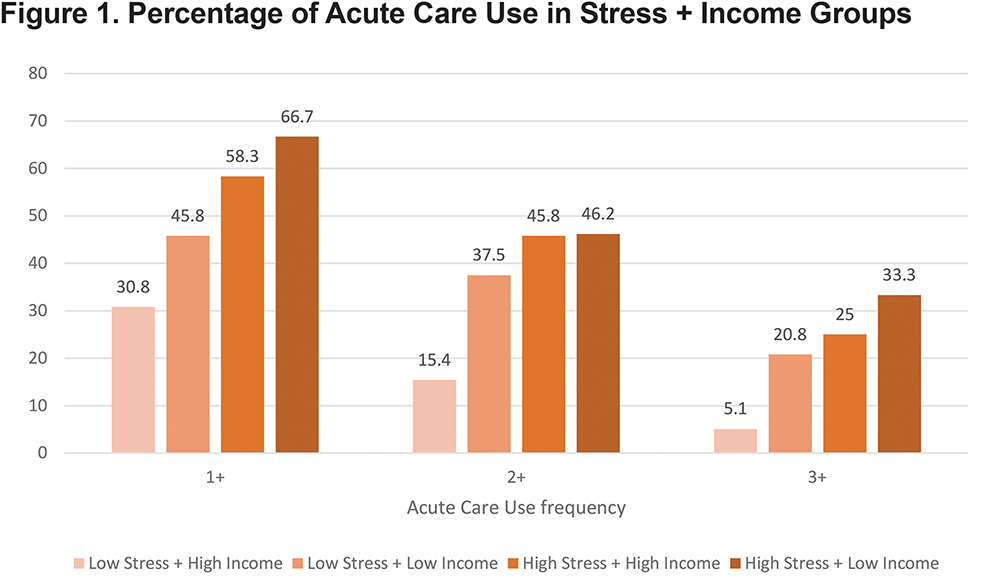
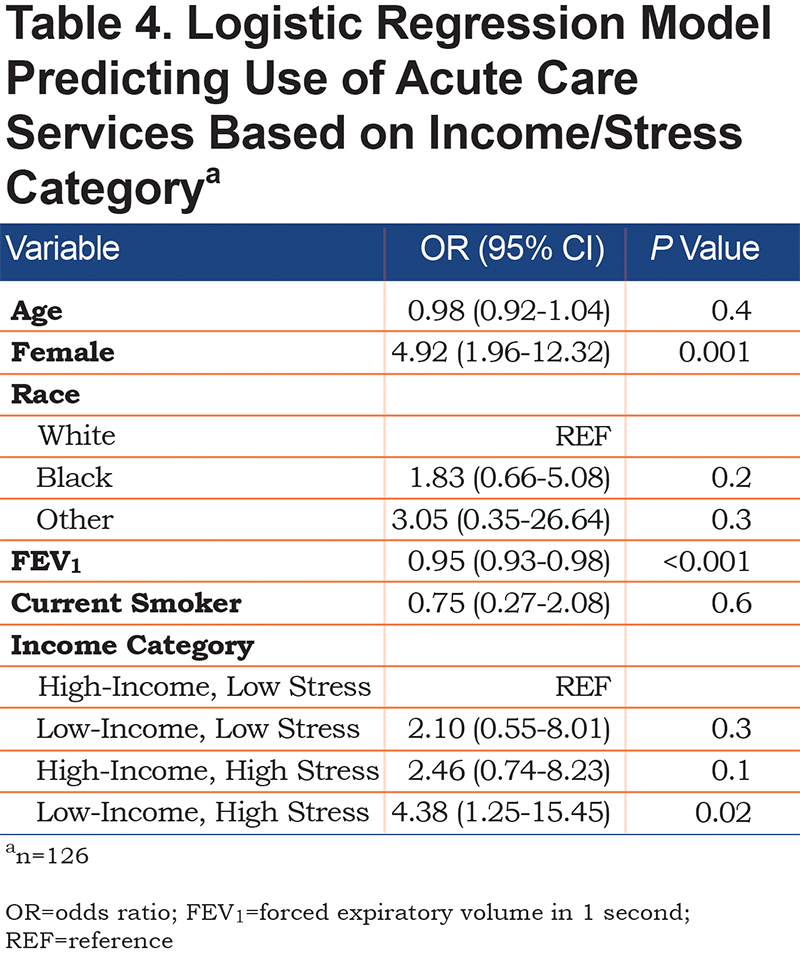
Results from the multivariable logistic regression model for use of acute care services in the past 2 years are shown in Table 4. Compared to low stress/high-income individuals, those who experienced low income/high-stress had a 4-fold increased association with acute care use (AOR, 95% CI, 4.38, 1.25–15-45) after controlling for demographic and clinical factors.
Discussion
Our study highlights the association between COPD-related acute care use and high perceived stress, particularly in those who experience high stress and have a low monthly income. We found that compared to low stress, high stress more than doubled the odds of using acute care services, with 4-fold increased odds in those with both low income and high stress. Our study also provided a comprehensive description of the SDH characteristics seen in COPD individuals, data which is not frequently found in existing literature. In comparing the 4 income + stress subgroups, our study highlights the potentially modifiable factors that distinguish the low-income + low-stress group from the low-income + high-stress group, including access to health insurance, transportation, safe neighborhoods, and food security, which may inform the integration of social care into health care for these groups.31
Due to the design of our study, we cannot draw conclusions of causality between stress and acute care use. However, there are several theoretical mechanisms that may explain bidirectional relationships between acute care use and perceived stress. ED visits and hospitalizations may cause increased stress for multiple reasons. Acute care use visits disrupt daily routine and are, by nature, indicative of a deterioration of one’s health. A longitudinal study found that individuals with moderate COPD who had frequent exacerbations (≥ 3 per year) had a greater decline in quality of life compared to those with infrequent exacerbations over the following 2 years.32 Exacerbations have also been associated with impaired work productivity, activity impairment, and, after the second severe exacerbation, a rapid decline in health status.33,34 Themes surrounding exacerbations of feeling “not in charge anymore” and fearing “my last day” emerged from a qualitative study of 14 COPD adults utilizing in-depth interviews.35 The emotional and physical toll of severe exacerbations is also accompanied by significant financial stress. In a large sample of a U.S. managed care population, COPD participants who were frequent exacerbators (2 or more exacerbations per year) in 2008 incurred an average of $7382 in COPD costs.36
Alternatively, increased levels of perceived stress may perpetuate increased acute care use through biobehavioral and psychological mechanisms. Increased stress can increase tobacco use,37 thus increasing the risk of disease progression, exacerbation, and lung cancer in individuals with COPD. In our study comparing 4 low-income groups, those who had low income + high stress had higher rates of smoking compared to those with high income + high stress (67% versus. 17%; p < 0.001). It is well-known that low income and education are associated with tobacco use38 and although low-income individuals make similar attempts to quit smoking, their success rates are lower compared to high-income individuals.39 Perceived stress can also impact health outcomes in COPD through biobehavioral mechanisms involving cortisol and inflammatory markers. Under states of chronic stress, a prolonged increase in cortisol, the primary neuroendocrine stress hormone, leads to glucocorticoid resistance, increased levels of inflammatory markers, and increased susceptibility to respiratory viruses, all of which may increase the risk of COPD exacerbations.40,41 Stress can also increase the risk of anxiety and depression, both of which are known to predict poor outcomes in individuals with COPD.42,43 A meta-analysis of 9 prospective studies of the impact of depression and anxiety on future exacerbations found that depression (relative risk, 1.12; 95% CI, 1.02–1.24) and comorbid depression and anxiety (relative risk, 1.18; 95% CI, 1.01–1.38) increase the risk of hospitalizations for acute exacerbations of COPD in severe COPD patients.44 Individuals living in low-SES neighborhoods have more than double the incidence of depression compared to individuals living in high-SES neighborhoods,45 which may indicate that psychological effects of stress may be amplified for low-income individuals.
Our results should be interpreted in light of several limitations. ED visits and hospitalizations were self-reported which may allow recall bias. However, we chose to use patient-reported data as individuals may not consistently use our institution for acute care services, limiting the reliability of electronic medical record data. In addition, self-reported measures of utilization have been shown to have good agreement with administrative data, particularly for acute care utilization.46 These data were also cross-sectional and thus cannot be used to establish causality. We cannot conclude that stress causes acute care use or that acute care use causes stress based on the results of our study. Nonetheless, the results call for further complex investigations of the relationship between stress and acute care use. Our sample size was small, which limited the number of covariates we could include in our models. There are also many variables that contribute to stress which were not collected in our study, and thus could not be included in our model. A major strength of our study lies in the detailed collection of SDH data for COPD patients. To our knowledge, there are no known databases that have collected this granular level of data, despite the national recognition of its importance in influencing health outcomes.47 However, the use of multiple comparisons does increase the risk of Type 1 errors, therefore results should be interpreted with caution.
The results from our study highlight a relationship between stress and acute care use in individuals with COPD, particularly those who are vulnerable and may lack the tangible and emotional resources needed to cope with stressful events. Longitudinal studies are warranted to determine the temporal relationship between stress and acute care use, the results of which may inform the design of readmission reduction interventions.
Acknowledgements
Author Contributions: All authors (TMP, SBP, JMT, BT, SB, ALC, YK and MTD) have substantially contributed to the study design, data analysis and/or interpretation, and writing and editing of the manuscript prior to its submission. All authors have significantly contributed to the intellectual content of the article and have given final approval of the version to be published.
Declaration of Interest
TMP, SBP, JMT, BT, SB, YK and ALC have nothing to declare. MTD reports grant funding from the American Lung Association, the National Institutes of Health, the Department of Defense, and the Department of Veterans Affairs; consulting fees from AstraZeneca, GlaxoSmithKline, Mereo, PneumRx/BTG, Pulmonx, and Quark; contracted clinical trials from AstraZeneca, Boston Scientific, Boerhinger Ingelheim, Gala, GlaxoSmithKline, Nuvaira, PneumRx/BTG, Pulmonx, and Yungjin.