Running Head: COPD Outcomes at VA vs non-VA Hospitals
Funding Support: Supported by a National Institutes of Health grants T32HL144909 (SLL), K24HL132008 (PKL), K12HL137940 (LJS), UL1TR001881 (RGB), and K23HL130524 (VPC).
Date of acceptance: April 26, 2021│ Published online: May 11, 2021
Abbreviations: chronic obstructive pulmonary disease, COPD; U.S. Centers for Medicare and Medicaid Services, CMS; Veterans Health Administration, VHA; Veterans Affairs, VA; confidence interval, CI
Citation: LaBedz SL, Krishnan JA, Chung YC, et al. Chronic obstructive pulmonary disease outcomes at Veterans Affairs versus non-Veterans Affairs hospitals. Chronic Obstr Pulm Dis. 2021; 8(3): 306-313. doi: http://doi.org/10.15326/jcopdf.2021.0201
Introduction
Randomized clinical trials of various interventions designed to reduce hospital readmissions in patients with chronic obstructive pulmonary disease (COPD) have demonstrated inconsistent results, including reductions in readmissions,1,2 an increase in the risk of readmissions or emergency department visits,3 and an increase in the risk of death4 compared to usual care. Results of these and other clinical trials in COPD5 suggest that efforts to reduce readmissions may be variably successful depending on the intervention, patient population, and health care setting.
In the last decade, the U.S. Centers for Medicare and Medicaid Services (CMS) and the Veterans Health Administration (VHA) have prioritized reducing avoidable readmissions. Among Medicare beneficiaries, an observational study found that the implementation of CMS financial incentives to reduce 30-day readmissions in patients hospitalized for heart failure or pneumonia was associated with significant increases in 30-day post-hospital mortality.6 These increases in mortality were primarily driven by patients who were not readmitted. In contrast, among U.S. veterans hospitalized for heart failure, readmission rates declined while mortality rates remained stable.7 Little is known about the relative performance of Veterans Affairs (VA) hospitals and non-VA hospitals on COPD readmissions and mortality following the implementation of policies8,9 intended to incentivize hospitals to reduce COPD readmissions.
The primary objective of this study was to characterize 30-day readmission and mortality rates of patients hospitalized for COPD at VA and non-VA hospitals. Given the potential for harm when hospitals implement strategies to reduce readmissions, we also examined the association between readmission and mortality rates across all U.S. hospitals and separately in VA and non-VA hospitals. Moreover, we examined the association between readmission and mortality rates according to various hospital characteristics to determine whether the association is consistent across different hospitals. Preliminary results were presented at the May 2020 American Thoracic Society International Conference.10
Methods
Hospital-level risk-standardized 30-day readmission and mortality rates in both VA and non-VA hospitals were obtained from CMS Hospital Compare and included Medicare beneficiaries hospitalized for COPD over a 3-year period from July 1, 2015 to June 30, 2018.11,12 Risk-standardized readmission and mortality rates accounted for patient age, comorbid conditions, and indicators of frailty.12,13
We further classified non-VA hospitals according to teaching status, safety-net status, and urban versus rural location. The data required to classify hospitals using these characteristics were obtained from the 2015 Final Rule Impact File14 and were not available for VA hospitals and non-VA critical access hospitals15 since they do not receive reimbursement adjustments under the CMS Inpatient Prospective Payment System. Teaching hospitals were defined16 as having a resident-to-bed ratio > 0. Safety-net hospitals were defined as hospitals in the top quartile of the CMS Disproportionate Share Hospital patient percentage, consistent with previous studies.17 Urban or rural designation by CMS was determined by the core-based statistical area in which the hospital is located.18
Comparisons between VA and non-VA hospitals were evaluated using t-tests and 95% confidence intervals. Associations between hospital-level readmission and mortality rates were evaluated using linear regression models in all hospitals and within VA and non-VA strata. We report the beta coefficient with its 95% confidence interval (CI) to quantify the relationship between the hospital-level readmission and mortality rates. Effect modification by VA/non-VA status and by hospital characteristics was tested using an interaction term in separate linear regression models. If effect modification by hospital characteristic was present, we conducted additional stratified analyses. A 2-tailed p-value <0.05 was considered significant. Analyses were performed using R (version 3.6.0, Vienna, Austria).
Results
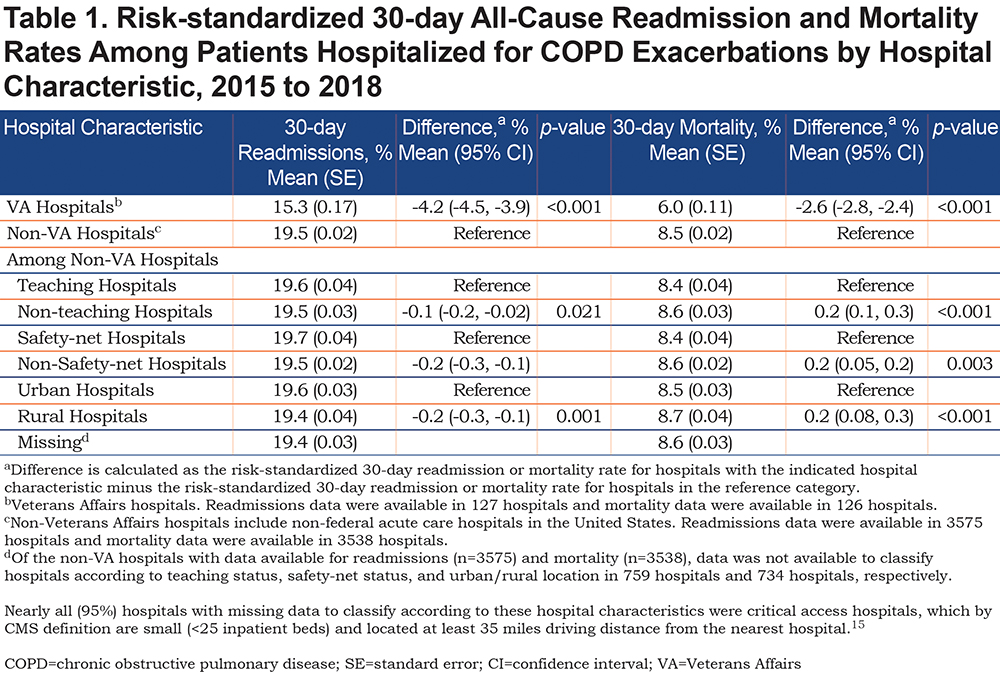
The mean (range) risk-standardized 30-day readmission rates were 15.3% (11.8% to 20.2%) at 127 VA hospitals and 19.5% (15.8% to 26.1%) at 3575 non-VA hospitals (Table 1). The mean (range) risk-standardized 30-day mortality rates were 6.0% (3.2% to 10.5%) at 126 VA hospitals and 8.5% (4.9% to 14.3%) at 3538 non-VA hospitals. VA hospitals had a 4.2% lower (95% CI -4.5% to -3.9%; p-value<0.001) mean readmission rate and 2.6% lower (95% CI -2.8% to -2.4%; p-value<0.001) mean mortality rate compared to non-VA hospitals. Among non-VA hospitals, those classified as non-teaching hospitals, non-safety-net hospitals, and rural hospitals had significantly lower readmission rates and higher mortality rates compared to teaching hospitals, safety-net hospitals, and urban hospitals, respectively.
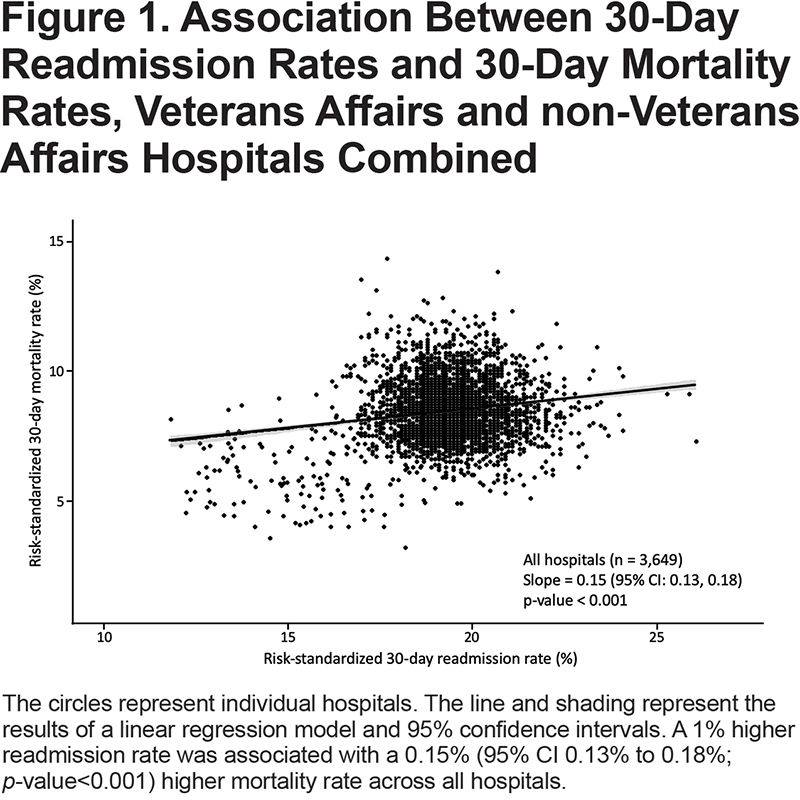
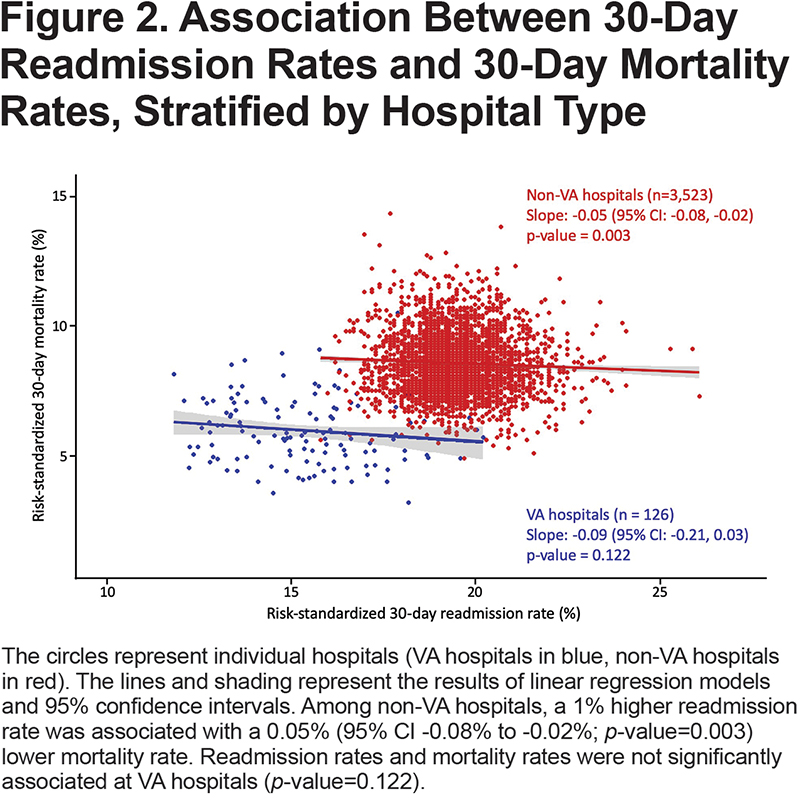
Data for both readmission and mortality rates were available in 126 VA hospitals and 3523 non-VA hospitals. When VA and non-VA hospitals were aggregated, higher readmission rates were associated with significantly higher mortality rates (Figure 1) and VA/non-VA status did not modify the association (interaction p-value=0.44). However, in analyses stratified by hospital type, higher readmission rates were associated with significantly lower mortality rates among non-VA hospitals (Figure 2), with 50 fewer deaths per 1000 more readmissions. A similar, but non-significant inverse association was observed among VA hospitals.
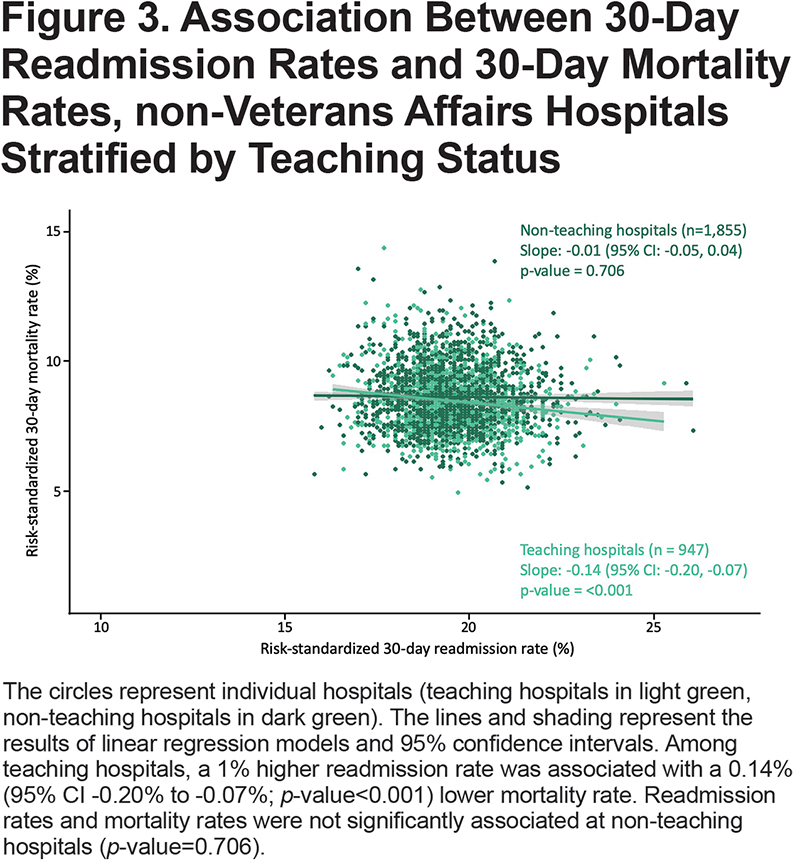
Among the 3523 non-VA hospitals with available data for both readmission and mortality rates, data for teaching status, safety-net status, and urban/rural location were available in 2802 (80%) hospitals. Of the 721 non-VA hospitals without data available to classify according to those hospital characteristics, 687 (95%) were critical access hospitals. Teaching hospital status modified the association between readmission and mortality rates (interaction p-value=0.001) among non-VA hospitals, but this was not observed for other hospital characteristics (p-value for all interactions > 0.5). Among teaching hospitals, we observed 140 fewer deaths per 1000 more readmissions (Figure 3).
Discussion
We found that VA hospitals had lower risk-standardized 30-day readmission and mortality rates in patients hospitalized for COPD compared to non-VA hospitals from July 2015 to June 2018, 3 years following the implementation of policies intended to reduce COPD readmissions.8,9 Among non-VA hospitals, higher readmission rates were also associated with lower mortality rates. The inverse association between readmissions and mortality observed among non-VA hospitals varied according to teaching hospital status.
Our findings extend observations noted prior to and after implementation of policies to reduce readmissions. VA hospitals outperformed non-VA hospitals on mean risk-standardized 30-day readmissions (3.7% lower) and mortality (1.9% lower) in patients with COPD from 2012 to 2015,19 suggesting the gaps in readmissions and mortality may be widening (corresponding values in current report 4.2% and 2.6%, respectively). In an analysis limited to 121 of 306 U.S. hospital referral regions from 2014 to 2017, the risk-standardized 30-day mortality rate in patients with COPD also favored VA hospitals (3.5% lower).20 Several possible explanations for results favoring VA hospitals in patients hospitalized for COPD warrant further investigation, including the availability of post-hospital transitional care services (e.g., arranging follow-up appointment), effects of financial penalties and reimbursement models on resources available to provide high-quality care, and differences in data quality or patient populations unaccounted for in the risk-adjustment models.
Interestingly, we observed a reversal of trends when comparing the association between readmission and mortality in all hospitals and when stratified by VA and non-VA hospital type. This reversal of trends is an example of Simpson’s paradox, a statistical phenomenon that can occur when 1 or more unaccounted factors linked with the outcome are unequally distributed between groups.21 This finding highlights the challenges associated with interpreting administrative data, which lacks important clinical information; it is also relevant from a policy perspective. The Veterans Access, Choice and Accountability Act of 20148 mandated the Secretary of Veterans Affairs to make patient quality and outcome data at VA hospitals publicly available through CMS Hospital Compare.11 This effort to increase transparency and accountability for the VHA was followed by the VA MISSION Act of 2018,22 which further expanded veterans’ access to health care outside the VA health care system. It is of interest to veterans to make informed choices about where to go for health care, and the data provided on Hospital Compare is intended to allow for comparisons between VA and non-VA hospitals. However, our finding of Simpson’s paradox suggests the CMS-derived risk-adjustment models may be inadequate for direct comparisons between VA and non-VA hospitals due to residual confounding. The lack of patient-level data in our study limits our ability to elucidate potential sources of residual confounding, but previous studies have noted that differences in coding practices and in social determinants of health among patients served by different hospitals also contribute to variations in risk-adjusted readmission and mortality rates.23-26 Taken together with our finding that teaching hospital status modified the association between readmissions and mortality, our study builds on existing evidence that variations in hospital readmission rates and mortality rates are likely related to the patients and communities which hospitals serve in addition to the quality of care they provide.
The inverse association between readmission and mortality rates in non-VA teaching hospitals in the current study is consistent with a randomized clinical trial that showed an increased risk of death with an intervention intended to reduce COPD readmissions.4 An observational study also found increases in post-hospital mortality in patients with COPD following implementation of CMS policies to reduce readmissions.27Although this finding may be partially explained by changes in coding practices,28,29 the potential for increases in post-discharge mortality accompanying reductions in readmissions has been reported for other conditions.6 It remains unclear if nationwide efforts to reduce readmissions improved or worsened patient outcomes, but our findings add to a body of literature that calls for re-examining these policies.
Strengths of our study include the use of well-established publicly reported metrics in thousands of U.S. hospitals. Our study also has several limitations. The lack of patient-level data about severity of illness or quality of care limits our ability to explain the observed patterns. Although CMS-derived risk-adjustment models do account for patient age, comorbid conditions, and indicators of frailty, they do not account for other determinants of clinical outcomes such as severity of illness at hospital discharge (e.g., hypercapnia) or adherence to prescribed care (e.g., use of home oxygen therapy for severe hypoxemia). To the extent these factors contribute to case-mix variation across hospitals, there may be residual patient-level confounding when comparing hospital-level outcomes. Also, the CMS risk-adjustment formula for hospital readmissions does not account for deaths that occur during hospitalization or shortly after discharge. Thus, if the risk of readmission differs between those who die and those who survive, hospitals with higher numbers of deaths may have lower “risk-standardized” 30-day readmission rates as a result of selection bias.30 Our analyses, which use hospital-level performance, may not necessarily hold for individual patients (ecologic fallacy). The cross-sectional study design also precludes establishing a causal association between readmissions and mortality.
Further research is needed to understand the patient, hospital, and health system determinants of readmission and mortality following hospitalization for COPD.31 Ongoing efforts to reduce readmissions should address modifiable risk factors that contribute to avoidable readmissions without discouraging appropriate readmissions.
Acknowledgements
Author contributions: SLL, JAK, YCC, and VPC were primarily responsible for the study design, analysis, interpretation and drafting of this manuscript. PKL, LJS, LCF, EMS, RGB, and SB provided substantial contributions to the analysis, interpretation, and critical revisions. All listed authors approve this final version and agree to be held accountable for all aspects of the work.
Declaration of Interest
JAK reports grants from the National Institutes of Health (NIH) and a research contract from the Patient-Centered Outcomes Research Institute outside the submitted work. PKL reports grants from the NIH/National Heart, Lung, and Blood Institute (NHLBI) outside the submitted work. LJS reports grants from the NIH/NHLBI during the conduct of the study. LCF reports receiving an annual stipend for her role as associate editor for Annals of the ATS, during the conduct of the study; grants from the Department of Veterans' Affairs Health Services Research and Development, grants from the American Lung Association, and grants from the NIH/NHLBI outside the submitted work. RGB reports personal fees from GlaxoSmithKline, personal fees from Mylan/Theravance Biopharma, grants from the NIH/National Center for Advancing Translational Sciences, and grants from the NIH/NHLBI outside the submitted work. RGB is employed by the Veterans Health Administration. The submitted work does not necessarily reflect the views and positions of the Department of Veterans Affairs. VPC reports grants from the NIH during the conduct of the study and other from Vertex Pharmaceuticals outside the submitted work. SLL, YCC, EMS, and SB have nothing to disclose.