Running Head: Aerosolized therapy during the COVID-19 pandemic
Funding support: No funding support was involved in the writing of this report.
Date of acceptance: May 26, 2021 │ Published online: June 4, 2021
Abbreviations: severe acute respiratory syndrome coronavirus 2, SARS-CoV-2; coronavirus disease 2019, COVID-19; airway clearance techniques, ACTs; Centers for Disease Control and Prevention, CDC; personal protective equipment, PPE; pulmonary nontuberculous mycobacteria, pNTM; health-related quality of life, HRQoL; nontuberculous mycobacteria, NTM; positive expiratory pressure, PEP
Citation: McShane PJ, Philley JV, Prieto DA, Aksamit TR. Global attitudes of health care providers about aerosolized airway clearance therapy in bronchiectasis patients during the coronavirus disease 2019 pandemic. Chronic Obstr Pulm Dis. 2021; 8(3): 319-325. doi: http://doi.org/10.15326/jcopdf.2021.0214
Online Supplemental Material: Read Online Supplemental Material (311KB)
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the novel human coronavirus that is responsible for the coronavirus disease 2019 (COVID-19) pandemic, is transmitted by person-to-person contact. Transmission occurs primarily by inhalation of respiratory droplets, but fomite transmission has also been identified.1 Airway clearance techniques (ACTs), such as those required by bronchiectasis patients, are likely to generate higher load infectious particles, theoretically putting health care personnel at an increased risk for infection. The Centers for Disease Control and Prevention (CDC) has published special infection control considerations for aerosol-generating procedures. They recommend, when feasible, to minimize the use of procedures or techniques that might produce infectious aerosols and to minimize the number of people in the operating or procedure room to reduce exposures. If such procedures are deemed necessary, use of all personal protective equipment (PPE), such as N95 or equivalent higher-level respiratory or facemasks, eye protection, gloves, and gown, is recommended.2
ACTs include directed cough, forced expiratory maneuvers, active cycle of breathing, positive pressure devices with oscillation, and high frequency chest wall oscillation.3 Nebulized mucolytic and/or bronchodilator solutions are commonly added adjuncts to ACTs3 and are, therefore, included as ACTs in this discussion. ACTs are an essential component in the management of bronchiectasis and pulmonary nontuberculous mycobacteria (pNTM) lung disease patients. ACTs improve symptoms and health-related quality of life (HRQoL) and reduce exacerbation frequency.4,5 The exact risk of infectious transmission generated by ACTs is unknown. There are limited data describing the risk of coronavirus transmission during the 2003 SARS outbreak, but the applicability of this data in the COVID-19 pandemic is only theoretical. In the context of this uncertainty, health care workers are in a position of balancing the necessity of airway clearance techniques with the probable increased risk of SARS-CoV-2 transmission that these techniques impose. The survey presented here describes concerns of health care practitioners who care for bronchiectasis patients with known or suspected COVID-19 regarding the use of airway clearance techniques in various clinical and home settings.
Recognizing the importance of airway clearance in the management and treatment of bronchiectasis patients, we sought to identify concerns related to airway clearance techniques during the COVID-19 pandemic and whether the survey respondents’ institutions had implemented any policies specific to airway clearance in the context of the COVID-19 pandemic.
Methods
A single electronic survey was conducted in April 2020 and was widely disseminated throughout several global networks: the U.S. Bronchiectasis and NTM Research Registry, the European Multicentre Bronchiectasis Audit and Research Collaboration (EMBARC), the Australian Lung Foundation network, the NTM Information and Research Network, and the Japanese Bronchiectasis Registry Network. Practitioners of various levels of clinical care completed the survey, including medical doctors, nurses, and respiratory therapists who care specifically for patients with bronchiectasis, with and without pNTM infections. The survey focused on practitioners’ concerns related to use of ACTs and the risk of coronavirus transmission and further queried the practitioners’ subjective assessment of their patients’ adherence to ACTs in the context of the COVID-19 pandemic. The survey was divided in sections to allow for responses to refer specifically to the inpatient setting, the outpatient clinic setting, and the home setting. The survey is available in the online supplement.
This anonymous survey was targeted toward health care providers and did not include any personal identifiable information or health information. Health care providers were made aware of the intent to publish the results of the survey prior to initiation of the survey. At the time that this survey was conducted, surveys that were anonymous and targeted solely at health care providers were assumed to be exempt and were not submitted to an institutional review board for an exemption determination.
Results
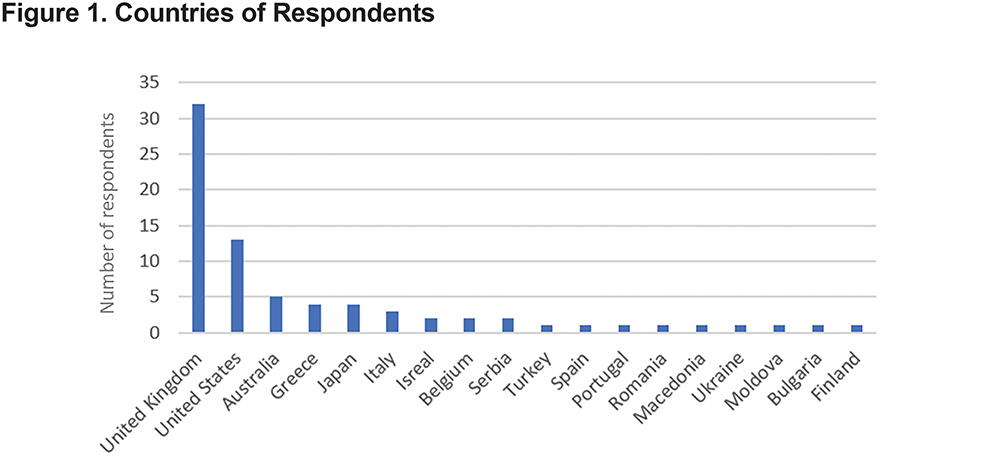
Seventy-six practitioners from 18 different international locations participated in the survey. Figure 1 shows the locations of the respondents. A total of 86.8% of the respondents were medical doctors. The remaining 13.2% of respondents were made up of respiratory therapists, registered nurses, PhDs, and research coordinators. Half (38/76) of the respondents had treated patients with either bronchiectasis or nontuberculous mycobacteria (NTM) lung disease, or both, who also had tested positive for COVID-19. The types of ACTs utilized are shown in Table 1. When practitioners were asked to estimate the percentage of their bronchiectasis or NTM lung disease patients who they thought were actively using prescribed ACTs regardless of COVID-19 status, only 22.6% of the practitioners reported that over 80% of patients were adherent to the prescribed regimen. Forty-three percent of the practitioners estimated between 50% and 79% of their patients were adherent, and 32.1% of practitioners estimated that less than 50% of patients were adhering to prescribed airway clearance regimens. Seventy-nine percent of practitioners reported that their institution had begun using telehealth (phone or video visits) in response to the COVID-19 pandemic, and 93% of those whose institutions started using telehealth had already personally conducted a patient visit via telehealth.

Inpatient Health Care Setting
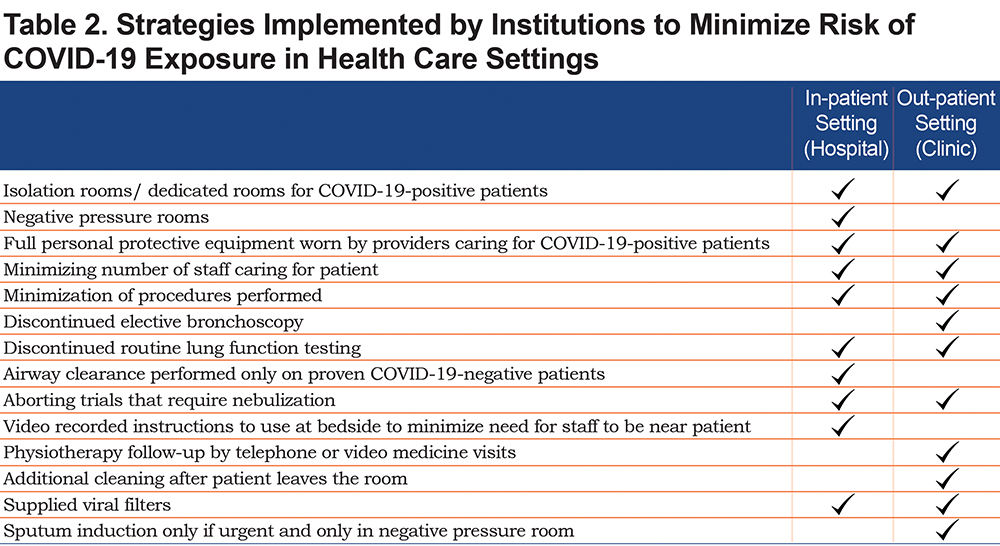
In response to the question, “Do you have any concerns about bronchiectasis and/or NTM lung disease patients with known or suspected COVID-19 performing aerosol generating procedures such as airway clearance techniques or diagnostic testing in an inpatient setting (e.g., hospital),” 85.3% percent of the respondents affirmed that they had concerns about the safety of inpatient ACTs, diagnostic tests, or both. The most frequently cited concern was directed cough and active cycle of breathing techniques (90.2%). Chest percussion/postural drainage (66.7%), positive expiratory pressure device use (72.5%), and high frequency chest wall oscillation (51.0%) were all cited as concerning by the respondents. Of those who had concerns regarding airway clearance techniques in the inpatient setting, 52% reported that their institution had implemented policies to enable COVID-19-positive patients to perform ACTs without putting others at risk. Table 2 shows reported strategies implemented by institutions in the inpatient and outpatient setting to minimize risk of COVID-19 exposure. These strategies were reported in an anonymous and free text fashion within the survey. Nine respondents, or 13.0%, expressed no concerns regarding aerosol-generating procedures with 1 of them indicating that all COVID-19 positive patients at his/her institution were isolated.
Outpatient Clinic Setting
Regarding airway clearance in the outpatient setting, 89.7% of respondents expressed concerns about patients with bronchiectasis and/or NTM lung disease with known or suspected COVID-19 infection performing ACTs, diagnostic testing, or both. Directed cough and active cycle of breathing was the most commonly cited concern from 88.9% of responders. The majority of responders also expressed concern about other techniques: chest percussion/postural drainage, 73.3%; positive expiratory pressure (PEP) without oscillation (e.g., Thera-PEP), 80.0%; PEP with oscillation (flutter or acapella device), 62.2%; and high frequency chest wall oscillation, 51.1%. Only 6 (8%) responders expressed no concern about known or suspected COVID-19 patients performing airway clearance techniques in an outpatient setting. Eighty-four percent of responders indicated that they recommend patients modify their environment (e.g., use a designated room) before performing airway clearance in an outpatient setting. Discontinuation of all airway clearance until COVID-19 was cleared was indicated as a recommendation by 11.4% of responders and 6.8% indicated that they advise patients to continue airway clearance as usual. Regarding outpatient diagnostic procedures, 85.7% of practitioners reported concern about both sputum induction and bronchoscopy. Only 66.7% of these responders indicated that their institution implemented a policy and/or procedure for the outpatient clinic setting to minimize risk of COVID-19 transmission during airway clearance.
Home Setting
In contrast to the majority of practitioners expressing concern about patients with known or suspected COVID-19 performing airway clearance in either the hospital or outpatient clinic setting, only 39.6% of responders expressed concern over the same patients performing these techniques at home. Of those who did report concern about airway clearance in the home, directed cough and/or active cycle of breathing was cited by 100% of the respondents. Discontinuation of airway clearance until patients recover from COVID-19 was indicated as a recommendation by 19.1% of responding practitioners. A total of 85.7% of respondents recommended that patients modify their environment while performing airway clearance, e.g., performing airway clearance in isolation, in a designated room, or outside.
Discussion
This survey of global attitudes provides a snapshot of current thoughts and opinions of health care practitioners who care for bronchiectasis and/or pNTM patients with known or suspected COVID-19 regarding the use of ACTs in both health care and home settings. Half of the respondents in this survey had treated patients with COVID-19. Active cycle of breathing and PEP with oscillation were the most commonly used modes. Interestingly, less than a quarter of practitioners estimated that the majority (more than 80%) of their patients were using prescribed ACTs and approximately one-third of practitioners estimated that airway clearance was being performed in less than 50% of patients. This low confidence in patient use of airway clearance regimens is not necessarily the effect of COVID-19. Prior to the COVID-19 era, a study performed to determine independent predictors of adherence to therapy in bronchiectasis patients revealed that only 41% of patients were adherent to airway clearance.6
There was almost ubiquitous concern about the safety of airway clearance in both inpatient and outpatient health care settings (85% and 89.7%, respectively). In contrast, only 39.6% of respondents felt concern about the use of airway clearance in the home. The majority of practitioners indicated that they recommend their patients perform airway clearance in a modified environment and 11.4% reported advising patients to stop all airway clearance until the virus had cleared. The latter observation is concerning given that ACTs result in symptom improvement and improved HRQoL in bronchiectasis patients.5 In addition to improving symptoms and HRQoL, hypertonic saline has been shown to improve lung function in these patients.7
Only about half of the respondents who indicated concern about the safety of airway clearance during the COVID-19 pandemic reported that their institution had implemented policies to enable COVID-19-positive patients to perform airway clearance without putting others at risk in the health care setting. This is a notable finding considering the severity of the current COVID-19 pandemic and could be the result of variable data that came from the 2003 SARS outbreak.
Loeb and colleagues conducted a retrospective cohort study among critical care nurses who worked in critical care units in Toronto during the 2003 SARS outbreak.8 The study analyzed the relative risk of infection for 23 different patient care activities and included 43 nurses who worked at least 1 shift in a critical care unit where there was a patient with SARS. Of the 43 nurses, 8 became infected. The activity with the highest relative risk of SARS transmission was manipulation of the oxygen mask (RR 9.00, confidence interval [CI] 1.25 – 64.89), followed by suctioning prior to intubation (RR 4.20, CI 1.59 – 11.14). Nebulizer treatments were associated with a relative risk of transmission of 3.24 (CI 1.11 to 9.42). The study concluded that SARS transmission can occur with exposure to respiratory secretions or activities that generate aerosols but also found a nearly 80% risk reduction with consistent use of masks (surgical or N95).
In another retrospective cohort study, Raboud and colleagues analyzed 624 health care workers who provided care to confirmed SARS patients during which time activities performed included airway clearance types of procedures.9 Twenty-six of the 624 individuals contracted SARS. Of the 598 health care workers who did not develop SARS, 47 (8%) performed chest physiotherapy, 38 (6%) performed sputum sample collection and 9 (2%) administered a nebulizer treatment. These percentages were not statistically significant compared to health care workers who performed the same activities and did develop SARS: chest physiotherapy performed by 1 (4%) of the health care workers, sputum sample collection by 4 (15%) of the workers, and nebulizer treatments that were administered by none (0%).
Wong and colleagues analyzed factors affecting transmission of SARS to medical students who contracted SARS after performing a bedside clinical assessment of an index SARS patient.10 The index patient had been treated with a bronchodilator via jet nebulizer 4 times per day, lasting 30 minutes each time. While 1 of the 9 students who developed SARS performed a bedside assessment after nebulizer treatments had been initiated, 6 of the 10 students who contracted SARS had performed a bedside assessment of the index patient on the day before nebulizer treatments had started, confirming that transmissibility was not dependent on delivery of nebulized treatments.
These studies are few in number and were limited by small cohort size, but they provide data that can inform our current approach to performing airway clearance during the current COVID-19 pandemic. The current survey is likewise limited by sample size, but it reveals the concerns that the majority of practitioners feel towards airway clearance techniques during the ongoing pandemic, the lack of uniform policies set forth by institutions, and the heterogeneity of strategies that practitioners have taken to minimize risk.
This survey has additional limitations. Although the survey was conducted at a peak of the COVID-19 pandemic (in April 2020), due to availability of testing at the time, we were not able to ascertain the percentage of respondents’ patients who were COVID-19 positive. Furthermore, we were not able assess if COVID-19 positive status affected patient adherence to the prescribed airway clearance regimens. Caution is clearly justified in administering ACTs in a patient suspected of having COVID-19, but the importance of maintaining airway clearance in a bronchiectasis patient is notwithstanding. Minimizing bronchiectasis symptoms, improving HRQoL, and preserving lung function in bronchiectasis will be more important than ever. Airway clearance, therefore, must be continued despite its attendant risks assuming adequate precautions including, but not limited to PPE, are used. As we move forward through this era of COVID-19 and beyond, research into ways to reduce infection transmissibility while maintaining airway clearance is of utmost importance to maintain the health of our bronchiectasis patients.
Declaration of Interest
The authors have no conflicts to report.