Running Head: COPD and Sleep Apnea: O2VERLAP Findings
Funding Support: The study was funded by the Patient-Centered Outcomes Research Institute contract PPRND-1507-3166.
Date of Acceptance: December 8, 2021 │ Published Online: December 15, 2021
Abbreviations: chronic obstructive pulmonary disease, COPD; obstructive sleep apnea, OSA. continuous positive airway pressure, CPAP; Patient-Centered Outcomes Research Institute, PCORI; Patient-Powered Research Networks, PPRNs; COPD Foundation, COPDF; American Sleep Apnea Association, ASAA
Citation: Sullivan J, Pasquale C, Clark B, et al. Outcomes important to patients diagnosed with both COPD and sleep apnea: findings from the O2VERLAP study focus groups. Chronic Obstr Pulm Dis. 2022; 9(1): 45-54. doi: http://doi.org/10.15326/jcopdf.2021.0268
Online Supplemental Material: Read Online Supplemental Material (268KB)
Introduction
The goals and activities of disease management can be different for patients and providers. Oftentimes, providers tend to be more focused on objective clinical parameters (e.g., test results) while patients are more focused on subjective factors (e.g., how they feel and function during the day). This is perhaps even more true when patients are dually diagnosed. Patients who are diagnosed with both chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea (OSA) are often referred to as having overlap syndrome.1 OSA is prevalent in at least 10%–15% of patients diagnosed with COPD.2 The prevalence rate of OSA is similar in patients with COPD as in the general population; individuals with both of these conditions who do not use OSA therapy at night during sleep have an increased risk of death and more hospitalizations from acute exacerbations, demonstrating the importance of OSA treatment.3
The first-line therapy for OSA patients is continuous positive airway pressure (CPAP). CPAP provides pressure to the airway to act as a pneumatic “splint” to keep the airway open during sleep.4 Overlap syndrome may be clinically distinct from either COPD or OSA alone. Patients with overlap syndrome have a worse prognosis compared with patients with only COPD or OSA for several reasons that have important implications for treatment and outcome.5 Studies that have examined the efficacy of CPAP therapy for overlap syndrome have shown that CPAP use is associated with improved walking capacity6 and longer survival in COPD patients who are hypercapnic,7 and that higher levels of CPAP adherence are associated with better outcomes.3 However, of the ~80% of patients who initially accept CPAP therapy, most patients fall into a partial use pattern of 3–5 hours per night.8,9 Adherence with long-term oxygen use has a parallel story; it is beneficial the more it is used but adherence is less than optimal,10 ranging from 45% to 70%. This evidence highlights the importance of providing this patient population the tools necessary to improve use of their prescribed medical device therapies.
There are several outcomes related to both COPD and OSA that are routinely measured by researchers and clinicians, but few studies to date have asked which of these outcomes are important to overlap syndrome patients. Additionally, few studies to date have focused on better understanding overlap syndrome patient CPAP therapy barriers and facilitators. One qualitative study focused on the role of partners, finding that to the extent that partners were involved and supportive of therapy, use of CPAP therapy tended to be better.11 Another focused on the communication patterns between health care personnel and patients during the initial CPAP visits, finding that there were certain aspects of communication that better facilitated patient-centered communications.12 And another qualitative study focused on studying CPAP use trajectories, finding that there seemed to be 2 unique pathways: a route of devotion, which was described as the pathway whereby patients tended to experience immediate benefits and became devoted, regular users of CPAP; and a route of negotiation, which was described as the pathway characterized by lower perceived benefits and, therefore, more irregular use patterns.13 While these studies all provided various insights in CPAP use factors, none directly investigated defined barriers and facilitators of CPAP use.
The study team had an opportunity to investigate both CPAP use facilitators and barriers and outcomes important to patients using qualitative methods as part of the O2VERLAP Study, which was funded by the Patient-Centered Outcomes Research Institute (PCORI) under the Patient-Powered Research Networks (PPRN) Research Demonstration Project mechanism. The goal of projects funded by this mechanism was to support the PCORI PPRNs in conducting comparative clinical effectiveness research on questions that are important to, and inclusive of, patients and other stakeholders.
The study team’s first task was to conduct a series of focus groups with overlap syndrome patients about their experiences with CPAP therapy. More specifically, the goal was to better understand important patient-centered outcomes, treatment barriers, and treatment facilitators so that the study team could develop and refine a peer-led, web-based coaching intervention, which was the focus on the main scientific study of the O2VERLAP project. The goal of the intervention of the larger scientific study was to improve therapeutic adherence and patient-centered outcomes in individuals with COPD and OSA.
Methods
The protocol was limited in scope to the conduct of 3 focus groups with the express purpose of identifying outcomes important to patients with both COPD and OSA, as well as identifying treatment barriers and facilitators. Details about the participants, recruitment methods, focus groups methods, and qualitative analysis are provided next. The study and methods were approved by Western IRB (Puyallup, Washington).
Description of Participants
Patients who had been diagnosed with both COPD and OSA were included. Participants were either current or recent past users of the primary therapeutic medical device for each condition, namely: supplemental oxygen and CPAP, respectively. Participants who reported using only 1 device were considered for inclusion in the focus groups on an individual basis.
Recruitment
Several types of recruitment were employed. The study team reached out to members of both the COPD Foundation (COPDF) (Miami, Florida and Washington, DC) and the American Sleep Apnea Association (ASAA) (Washington, DC) to inform them about these focus groups. The potential participants were notified of the study either verbally or electronically through posts to community online forums or through email. Online websites and forums included COPD360social®, the COPDF Facebook page, COPDF-related patient advocacy groups on Facebook, and the ASAA Facebook page. Any interested individuals were invited to participate in the focus groups by calling a toll-free phone number for more information. The electronic nature of the recruitment strategy allowed other study partners to easily share the approved recruitment messages with their own constituents. In all cases, potential focus group participants were directed to contact the COPDF’s study coordinator for more information. Only institutional review board (IRB)-approved messaging and scripts were used. For direct email, only 1 contact attempt was made. All recruitment materials were in English only.
Types of Focus Groups
The study team conducted 3 separate focus groups using the following modalities: (1) teleconference (audio only), (2) in-person, and (3) web-based platform. There were multiple reasons for using these 3 kinds of focus groups: to avoid limiting the amount of data collected, the study team’s short time frame, the limited mobility of participants, and as an opportunity to compare the usefulness of modes which, in comparison to in-person focus groups, are preferable for many reasons, including increased accessibility, timeliness, and improved resource allocation. Further, because the main study was national in scope, we realized an opportunity to begin practicing digital recruitment methods that would be used in the larger study, which was applicable to teleconference and web-based platform focus groups.
The focus groups differed only in communication modality: (1) the teleconference focus group was conducted via telephone, (2) the in-person focus group was conducted by a moderator physically located in the same room with the participants, and (3) the web-based platform focus group was conducted using the COPDF’s COPD360social platform, both in real-time and asynchronously, using a moderator-led private chat room.
There was a fair amount of discussion and time spent deciding how to optimally run the web-based platform focus group. The team decided to run an initial 2-hour synchronous (i.e., real-time) group where study team members engaged with participants in real-time. The initial 2-hour period was immediately followed by a 72-hour period of possible asynchronous communication; during the initial 2 hours, participants were made aware of the opportunity to provide more information over the following 3 days. The participants were encouraged to return and answer questions or provide follow-up responses at their convenience.
The study team planned to have between 5 and 8 participants in all the live focus groups to allow for substantive participation. The basis for this decision was focus group best practices, which recommends that fewer than 5 participants may limit the conversation and yield poor data while more than 10 can be unwieldy.14 The in-person focus group had 4 participants, the phone focus group had 5 participants and the web-based focus group had 8 participants.
Number of Focus Groups
It is well known that it takes more than 1 focus group on any one topic to produce valid results.14 The commonly accepted number of groups is usually 3 or 4. This is the rationale that was used to decide to run a total of 3 separate focus groups.
Focus Groups Methods
In-person and Telephone: All focus group participants were consented verbally over the phone and sent copies of the study’s IRB-approved consent information sheet. Focus group participants were introduced by first name and ground rules were established by the moderator and participants. Focus groups lasted approximately 90 minutes and were audio-recorded. Audio recordings were then transcribed for analysis. A brief questionnaire was given prior to the start of the in-person focus groups to assess participant demographics and to capture current therapeutic medical device characteristics. The telephone participants completed the same survey online via SurveyMonkey prior to participation.
Web-based Platform: The participation instructions used for the in-person and telephone-based focus groups were also applied in the web-based focus group. This focus group took place over 3 consecutive days after being live (i.e., interactions occurring in real-time) for a period of approximately 90 minutes. The text of the conversations was captured online via a private discussion forum and then converted into transcript format, similar to the in-person and phone focus groups.
Data Handling
The phone and in-person focus groups were audio recorded. The conversations were moderated in such a way as to keep participants anonymous. First names only were used to converse and to moderate the discussion. Recordings were submitted to a contract vendor for transcription, (Rev.com, Inc., San Francisco, California) and all personal health information, though it may have been discussed anonymously, was redacted from the records. The conversations from the online focus group were transcribed into a document and securely sent to Dr. Stepnowsky for analysis.
Qualitative Analysis
Qualitative analysis was conducted using thematic analysis, which consisted of coding the data through transcript review for potential conceptual categories. The initial categories were based on the project-specific focus group questions that the study team created for the Moderator Guide. The study team applied 2 types of codes for analysis: (1) deductive codes that represented expected themes, as identified by our stakeholders and from the medical literature, were applied to the data; (2) inductive codes that emerged organically were applied to the data. Emergent themes were identified based on recurrence, which is how frequently they were mentioned or discussed in the transcripts. Similarities and differences of the themes observed were documented.
The observed themes were developed into a codebook. The codebook included the name of each code, an operational description of the codes, notes regarding the inclusion and exclusion criteria for each code, as well as examples of each code in use. The use of the codebook was based on a recently published article.11 Coding was undertaken with reference to the codebook. Coded data was analyzed to provide a count of the most common phrases and to understand their links to each theme. This allowed the study team to build concepts grounded in the data to explain the observed phenomena and to have a shared understanding of the meaning and context of each theme and code. The transcripts were coded independently by 2 coders. The median intercoder reliability was 0.95 (95% confidence interval , 0.92 to 0.98) as measured by Cohen’s kappa. Differences in coding were discussed and resolved by consensus. After identifying all themes, final codes were applied to the transcripts to summarize the final themes and relevant quotes using Dedoose qualitative analysis software.15 A commonly used outcome metric is a count of the frequency of each code. Dedoose provides functionality to create a word cloud, which is a data visualization method to graphically show the most frequently used coded words and/or phrases.
Focus Group Questions
Online data supplement 1 provides the script used to begin each focus group and the list of questions used to engage participants in the discussion. The questions were designed to generate the kinds of discussions that can yield information that will be important for the goals of the subsequent larger scientific study, including both a focus on outcomes important to patients and a discussion of barriers and facilitators of device use. The questions started more generally and then became more specific.
Results
Focus Group Date and Duration
All synchronous discussions lasted about 90 minutes and were scheduled for midday EST to accommodate different time zones. This time of the day was selected because alertness levels tend to be best for this patient group during this time period. The online focus group remained open for comments after the synchronous portion for 72 hours and was considered the asynchronous portion of the online focus group.
Recruitment Methods
All recruitment was accomplished through established COPD and OSA patient communities. Interested individuals were directed to call or email the COPDF study research coordinator. Recruitment messaging and graphics were all submitted to Western IRB for approval prior to engagement. The COPDF and ASAA both used various online communities to promote the focus groups after receiving IRB approval, including: COPD360social, COPDF Facebook page, COPDF Twitter account, ASAA Facebook page, and ASAA Twitter account. Facebook was the primary and most successful source of social media recruitment. The focus groups were promoted organically for about 7 days and then utilized Facebook’s option for boosting posts and placing an advertisement.
Participant Demographics
The recruitment period was approximately 25 days (including weekends), during which time approximately 50 inquiries were received. Of the 50 inquiries received, 17 individuals were able to participate in the focus groups.
The average age of participants was 65 years old, 12 (70%) were female and 5 (30%) male, and 88% of the participants were White. The average household income of participants was $35,000–$50,000 annually. These demographics are consistent with those who are known to have the overlap syndrome. Most individuals reported that it was difficult to manage their financial needs on an annual basis with their reported household income. The participants’ average level of education was a completed high school diploma or GED with some college or vocational training. One hundred percent of participants used CPAP devices at night and 47% used both supplemental oxygen and CPAP devices at night. Only 52% of participants reported using their CPAP device as prescribed and only 75% of supplemental oxygen users reported using their oxygen therapy as prescribed.
Qualitative Data Analysis
Facilitators and Barriers. Table 1 provides a summary of the code counts while the full coding table is provided in online data supplement 2. The codes are summarized across the 3 focus groups. Interestingly, the most codes were from the telephone (40) and online (32) focus groups, while the in-person (16) focus group had fewer (~50%) excerpts coded. Table 1 shows the codes which have a count of 3 or more. The following facilitators had a count of 2: addition of humidifier, decreased energy, napping, and feeling refreshed in the morning. The following barriers had a count of 2: dryness, inconvenience when traveling, and “don’t want to put CPAP back on after getting up during the night.”
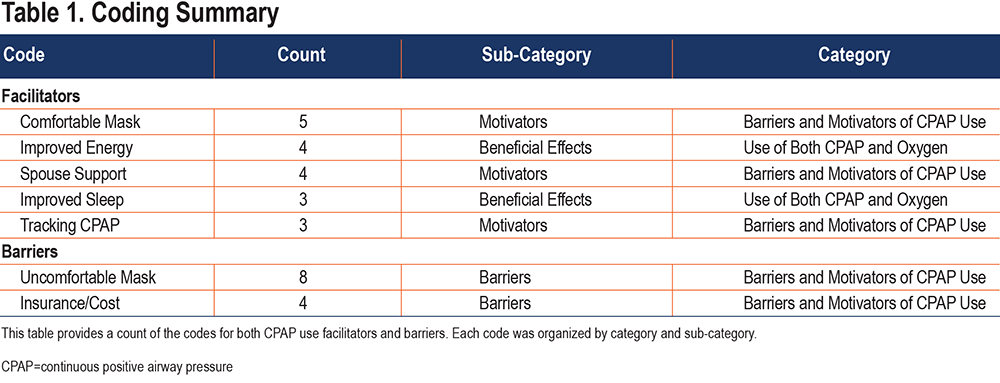
Interestingly, the role of the mask had a large impact for the participants as both a CPAP use barrier and facilitator. When participants described barriers or problems with therapy, they focused primarily on the mask, its poor fit and how uncomfortable it felt to wear. On the other hand, a comfortable mask was identified by other participants as the most important facilitator of CPAP therapy. Perceived benefit in the form of improved energy and improved sleep were other key facilitators. Having a supportive spouse or partner was another identified important facilitator. Several participants also found the tracking of their CPAP data via phone applications (i.e., apps) to be an important facilitator as well. Other key barriers, beyond an uncomfortable mask, included nasal dryness resulting from CPAP use and the cost of care maintaining a functioning CPAP device and related insurance issues.
Another coded aspect which might indicate poor mask fit and is also a cause of discomfort, is the perceived ability to breath with a mask on. It is important to note that there is often an adjustment period when first using a CPAP mask that, regardless of mask fit, requires users to overcome an initial sensation of asphyxiation or perceived breathing cessation when using the mask. This may be the case when a person is first diagnosed with OSA and becoming acquainted with CPAP therapy or when an experienced user is transitioning to use a new or different style CPAP mask. All of our focus group participants were seasoned CPAP therapy users.
Figure 1 shows a word cloud for the codes across the 3 focus groups. This word cloud included all coded items, including those from the discussion on the intervention format options.
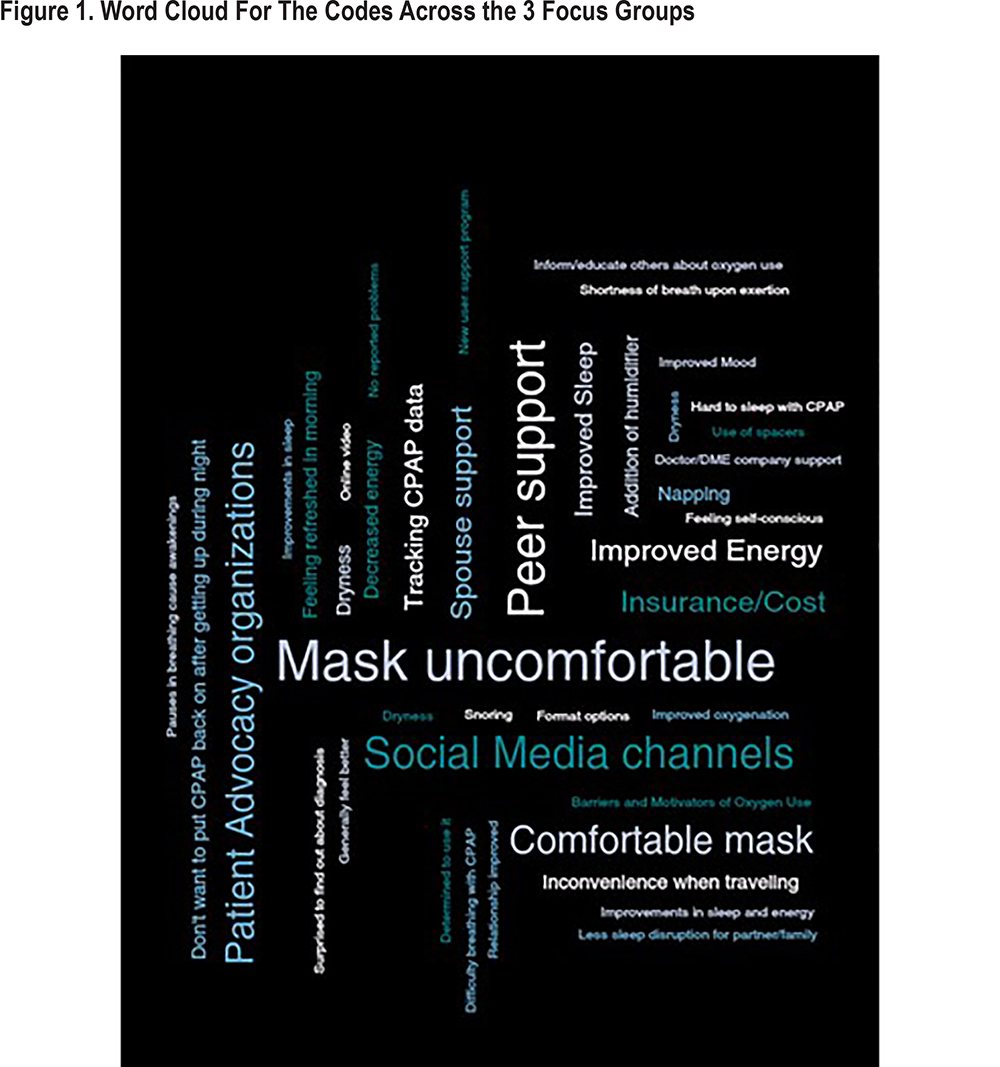
Intervention Format. In terms of intervention format options, participants were overall enthusiastic about obtaining peer support, which they communicated in various ways as being perceived as a method that is more tailored and customizable to their individual circumstances as compared to receiving support from members of their clinical care teams. They expressed the difficulty in obtaining the feedback that they needed within the clinical care system. The kind of feedback that they sought was related to general support and understanding for living day in and day out with OSA and COPD, and needing to use a treatment device on a nightly basis. While the clinical care team excelled in their technical expertise, peers were described as being more helpful with psychosocial support and empathy. A full list of the codes related to the intervention can be found in the online data supplement 2. Of note, peer intervention (count=7), social media channels (count=6), and patient advocacy organizations (count=5) were all listed as important sources of information about CPAP therapy.
Patient-Centered Outcomes: It was very clear from the transcripts that a disturbed night’s sleep results in a less than optimal ability to function the following day, and for several individuals, a very difficult time functioning the next day. Some used the expression “not being able to get out of bed.” Others used the phrases “not being able to do the kinds of activities that I want to do” and “not having the energy I need during the day.” Many participants mentioned the need to take naps the following day to manage their fatigue, which cut into time available to do typical day-to-day activities. In total, 15 out of 17 expressed the importance of daytime functioning as the most important outcome of managing their OSA.
Patient Perspectives: A qualitative analysis would not be complete without a summary of some of the patients’ thoughts and comments pulled out in their entirety. Online data supplement 3 contains a list of quotes and comments from individual participants of the focus groups on a variety of issues.
Discussion
The 3 focus groups were designed to gain a better understanding of the use of medical devices (CPAP and supplemental oxygen therapy) in the treatment of COPD and OSA. Participants were clearly affected by both COPD and OSA and all were using the medical devices to some degree. However, the focus group discussions of these 2 main devices clearly indicate participants felt they had a very good handle on their use of oxygen therapy but were relatively unsatisfied by their experiences with CPAP therapy. And it is important to point out that the group of patients in our focus groups reported using CPAP regularly and having very good daytime functioning. The study team was surprised by the predominant focus of the discussions on CPAP therapy relative to oxygen therapy. This observation was also reflected in the participants’ self-reported adherence for each therapy type, with 52% of the 17 participants using their CPAP device as prescribed and 75% of the 8 oxygen users using their oxygen therapy as prescribed. However, this group of patients proved to be quite resilient and adaptable as quite a few reported being able to adapt to CPAP therapy and derive a benefit after some personal trial and error. Even the most successful participants had stories to tell about their experiences, whether it be their perseverance in mask selection and comfort or negotiating with their insurance companies and/or durable medical equipment providers. While all new CPAP users have an adjustment period when starting to use therapy, what clearly distinguished this group of focus group participants was that none stopped using therapy despite the difficulties that they encountered.
Feedback from the O2VERLAP study’s Stakeholder Advisory Board indicated that overlap syndrome patients who are prescribed and use both medical device therapies (i.e., supplemental oxygen therapy and CPAP therapy) may represent an overall less well group (i.e., higher rates of comorbidities) and, therefore, comprise a relatively small percentage of potential participants in our larger study. We found, based on the 3 focus groups that were conducted, that not only do quite a few individuals use both therapies, but that they are able to manage their COPD and OSA quite well. Several participants expressed their belief that they felt the best during the day if they used oxygen therapy at night in conjunction with CPAP therapy. Several participants who are not currently prescribed or using supplemental oxygen therapy mentioned that they feel they would benefit from a prescription and were motivated by our discussions to pursue this with their health care provider.
Resolve: The best word the study team could find to describe the spirit of what our focus group participants were communicating in the focus groups in balancing the CPAP facilitators and barriers was “resolve.” Listening to the stories of patients who have managed their OSA and COPD for many years, the study team heard that the ones who managed their medical conditions most successfully had the resolve to use their medical device therapies regularly and to troubleshoot problems and find solutions. One definition of resolve is a “firm determination to do something” and in this case, it is to manage sleep apnea on a regular basis and work through CPAP problems and issues so that daytime functioning is maximized. The level of resolve and determination exhibited by the participants in our focus groups was remarkable.
Format of Intervention: One of the themes that came through was that the participants felt that clinical staff are often limited in terms of the amount of time that can be spent with patients, and that the use of other resources helped to fill this gap. Other resources included friends, family, community support, and social media support. Each participant was open to the type of intervention that the study team was planning for the main study. Only 2 participants said that they would prefer to get all of their medical information from a physician or provider in the clinical care context. A total of 15 out of 17 participants indicated that they would trust and rely on the type of intervention that we were planning. Importantly, several individuals made the distinction of obtaining information from the internet versus patient advocacy organizations (they used phrases like, “from COPD Foundation” “or when I visit 360” [short for COPD360social]). Of note, participants were not asked specifically to compare information sources they sought out, nor were they asked specifically about patient advocacy organizations, which we believe helps to provide more credence to this kind of finding from the focus groups.
Patient-centered Outcomes: It was very clear that a disturbed night’s sleep resulted in a less-than-optimal ability to function the following day with overlap syndrome patients, and for several individuals, a very difficult time functioning the next day. Many participants mentioned the need to take naps the following day to manage their fatigue, which cut into time available to do typical day-to-day activities. The predominant theme expressed by the participants was a focus on next-day functioning. This finding helped inform the primary aims of the main O2VERLAP study by increasing the importance of the measurement of daytime functioning.
Limitations
The focus groups were reliant on identifying patients from each of the medical condition’s patient advocacy organizations. It could be that individuals identified through these channels are somehow more motivated and able to take on challenges, given that they already were in some way associated with the organizations. Note, this statement is not meant to imply that the participants were active with the organizations; they were not. The study is also potentially limited by the sample size associated with each focus group type. It may be that had we run more focus groups with greater numbers that the findings would have been slightly different. That said, from quantitative studies of factors associated with CPAP use, mask comfort tends to be one of the top factors found. This means that the findings of this study are consistent with the findings of patients with sleep apnea only.
Summary
The study has found that the most important outcome to overlap syndrome patients is daytime functioning. It has also identified important CPAP facilitators and barriers as well as intervention formats important to, and preferred by, patients. In addition, it was clear from the groups that effective use of CPAP was a key factor in next day functioning and was described by most as being more important than the use of oxygen therapy. All of these findings were incorporated into the main O2VERLAP study. Importantly, the study team decided to primarily focus on CPAP therapy and changed the methods of the study to obtain and utilize CPAP adherence and efficacy data. The project was funded as part of the PCORI-funded Patient-Powered Research Network Demonstration Project mechanism, and the study team is finding that the inclusion of patients and other relevant stakeholders at study outset can improve research process and quality.
Acknowledgements
We would like to acknowledge the help of the COPDF state captains and the ASAA for their efforts in helping to recruit participants for this study.
Declaration of Interest
There are no conflicts of interest to report.