Running Head: GOLD-Discordant Prescribing of Triple Therapy
Funding Support: This study was sponsored by Boehringer Ingelheim Pharmaceuticals, Inc., and performed by Optum. The authors received no direct compensation related to the development of the manuscript. Boehringer Ingelheim Pharmaceuticals, Inc., was given the opportunity to review the manuscript for medical and scientific accuracy as well as intellectual property considerations.
Date of Acceptance: January 26, 2022 │ Published Online: February 2, 2022
Abbreviations: long-acting beta2-agonist, LABA; long-acting muscarinic antagonist, LAMA; inhaled corticosteroid, ICS; Global initiative for chronic Obstructive Lung Disease, GOLD; chronic obstructive pulmonary disease, COPD; Medicare Advantage with Part D, MAPD; triple therapy, TT; standard deviations, SDs; gastroesophageal reflux disease, GERD; short-acting beta2-agonist, SABA; short-acting muscarinic antagonist, SAMA; phosphodiesterase, PDE; confidence interval, CI; commercial, com; odds ratio, OR
Citation: Bhatt SP, Blauer-Peterson C, Buysman EK, Bengston LGS, Palli SR. Trends and characteristics of Global Initiative for Chronic Obstructive Lung Disease guidelines-discordant prescribing of triple therapy among patients with COPD. Chronic Obstr Pulm Dis. 2022; 9(2): 135-153. doi: http://doi.org/10.15326/jcopdf.2021.0256
Online Supplemental Material: Read Online Supplemental Material (258KB)
Introduction
In 2018, 9.7% of U.S. adults aged 45 or above had a diagnosis of chronic obstructive pulmonary disease (COPD), an increase from 8.9% in 20111; still, a substantial proportion of affected people remain undiagnosed.2 Historically, evidence-based recommendations for the treatment of COPD have been provided by the Global initiative for chronic Obstructive Lung Disease (GOLD).3 Maintenance therapy includes inhaled long-acting bronchodilators (long-acting muscarinic antagonists [LAMAs], long-acting beta2-agonists [LABAs]) as monotherapy or in combination, or with inhaled corticosteroids (ICSs).3 The GOLD document further recommends that pharmacological escalation to triple therapy (LAMA+LABA+ICS in free-dose [open triple therapy] or fixed-dose [closed triple therapy] combinations) should be reserved exclusively for the most severe COPD patients with a history of exacerbations (≥2 moderate and/or ≥1 severe) and whose symptoms are not controlled on LAMA/LABA maintenance therapy.4,5 Although clinical trials support advancement in these cases to triple therapy, concerns remain about the chronic use of ICSs and their association with an increased risk of pneumonia,3 diabetes/poor control of diabetes, cataracts, and mycobacterial infection, including tuberculosis.
Real-world observational studies of clinical practice have demonstrated increased prescribing of triple therapy6,7,8 since 2004. Furthermore, multiple claims-based retrospective studies have reported up to 60% of patients as being prescribed triple therapy contrary to GOLD recommendations, including initiation as first-line therapy and/or with insufficient exacerbation history.6,7,9 The most recent of these studies observed patients receiving maintenance COPD medications from 2013 to 2017, before the closed triple therapy option9 became available in September 2017. No real-world studies have since reported on the temporal prescribing patterns of triple therapy among patients with COPD and how closed triple therapy may have impacted triple therapy prescribing.
The objectives of this study were to: (1) describe COPD patients in the United States initiating triple therapy during the period 2014 to 2018 with no history of maintenance therapy (maintenance-naïve) and/or insufficient exacerbation history (exacerbation-discordant) stratified by open and closed triple therapy; and (2) determine factors associated with GOLD-discordant prescribing when both open and closed triple therapy were available.
Methods
Study Design and Data Source
A non-interventional retrospective analysis was conducted using de-identified administrative data between January 1, 2013, and December 31, 2018 (study period including baseline and identification periods) from the Optum Research Database and included medical and pharmacy claims with linked enrollment data for enrollees in commercial and Medicare Advantage with Part D (MAPD) health care plans. The Optum Research Database contains data representing more than 73 million unique patients, including approximately 20% of the commercial-insured and 20% of the Medicare-insured population of the United States. The distribution of age, gender, race, and geographic region is aligned with the overall U.S. commercial and Medicare insured populations, respectively.
Sample Selection
Inclusion Criteria
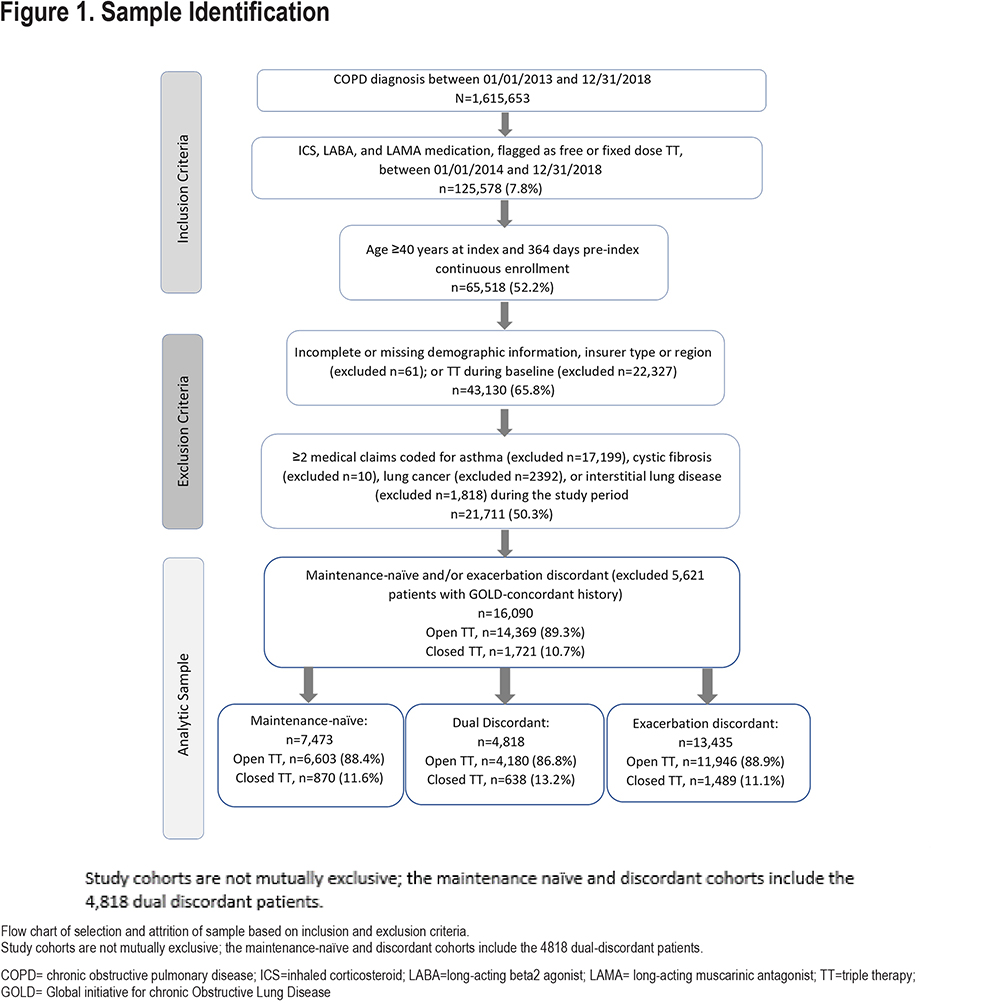
Patients were identified by the presence of ≥1 COPD diagnosis code in any position on a medical claim during the period January 1, 2013, through December 31, 2018 (identification period) (Figure 1). Study eligibility required ≥30 days of overlapping ICS, LAMA, and LABA prescriptions (allowing for a 7-day gap) between January 1, 2014, and December 31, 2018 (study period); the index date was set to the first date that all 3 components were on hand. Patients were categorized as initiating open triple therapy (multiple inhalers collectively containing ICS, LAMA, and LABA) or closed triple therapy (a fixed-dose single triple therapy inhaler containing fluticasone furoate/umeclidinium/vilanterol). Patients aged 40 years or older at index and with continuous medical and pharmacy enrollment for ≥12 months prior to index (baseline period) were retained.
Exclusion Criteria
Patients were excluded if they had ≥2 medical claims with diagnosis code(s) for asthma, cystic fibrosis, interstitial lung disease, or lung cancer; missing demographic information (age, gender, geographic region, or insurance type); or baseline use of triple therapy.
Patients who met the study selection criteria were stratified by their index year. For calendar year 2018, when both open and closed triple therapy were available for the entire year, the latter subpopulation of closed triple therapy was also highlighted.
Cohort Definitions
GOLD-discordant cohorts (not mutually exclusive) were defined according to the 2018 GOLD recommendations10 based on the following criteria evaluated during the 12-month baseline period:
- Maintenance-naïve patients had no evidence of use of ICS, LAMA, LABA and/or their combinations prior to initiating triple therapy.
- Exacerbation-discordant patients had no evidence of severe exacerbation(s) and <2 moderate exacerbations before initiating triple therapy (i.e., were classified as GOLD A/B). Severe COPD exacerbation was defined as an inpatient admission with a COPD diagnosis code in the primary position, or an acute respiratory failure diagnosis code with a non-primary COPD diagnosis code. A moderate exacerbation was defined as an emergency department visit with a COPD diagnosis code in the primary position or an office visit with a COPD diagnosis in any position plus a pharmacy claim for a COPD-recommended antibiotic and/or a pharmacy claim for an oral corticosteroid within ±7 days of the visit. Encounters occurring within 14 days of each other were considered a single exacerbation episode and classified according to the event contributing the highest severity.
- Dual-discordant patients were both maintenance-naïve and exacerbation-discordant.
Study Measures
Baseline patient demographic characteristics and clinical characteristics were obtained from claims. Index medication information included index triple therapy type, active ingredient composition, and the prescribing provider specialty.
Statistical Analyses
Baseline measures were analyzed descriptively for the overall triple therapy-initiating population and the following subgroups of interest: (1) maintenance-naïve, (2) exacerbation-discordant, and (3) dual-discordant. Frequencies and percentages were calculated for categorical variables. Means with standard deviations (SDs) were calculated for continuous variables. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, North Carolina).
Multivariable logistic regression analyses were used to explore the association between receipt of open or closed triple therapy and (1) dual discordance, and (2) maintenance-naïve discordance with GOLD recommendations, adjusting for demographic characteristics, comorbidities, baseline medications, and index provider types. These analyses were restricted to calendar year 2018, when both open and closed triple therapy treatment options were available. The outcome of the first model was dual discordance versus GOLD-appropriate prescribing on one or both criteria among all patients. The outcome of the second model was maintenance-naïve status at the time of open or closed triple therapy receipt stratified by the presence or absence of exacerbation discordance.
This study used fully de-identified data extracts in a manner compliant with Health Information Portability and Accountability Act regulations. Institutional review board approval was neither required nor sought.
Results
Sample Selection
Among 1,615,653 patients with a COPD diagnosis, 65,518 met the study inclusion criteria and 21,711 remained eligible after exclusion criteria were applied (Figure 1). Of the overall triple therapy study population, 34.4% of patients were maintenance-naïve, 61.9% were exacerbation-discordant, and 22.2% were dual-discordant. The maintenance-naïve and exacerbation-discordant cohorts include the subset of dual discordant patients.
Patient Characteristics
Overall Sample
Triple therapy prescribing appeared to increase year-over-year between 2016 and 2018; patients initiating triple therapy in 2017 and 2018 accounted for 54.1% of the study sample (Table 1).11 In 2018, 1 out of every 3 triple therapy initiators started with closed triple therapy.
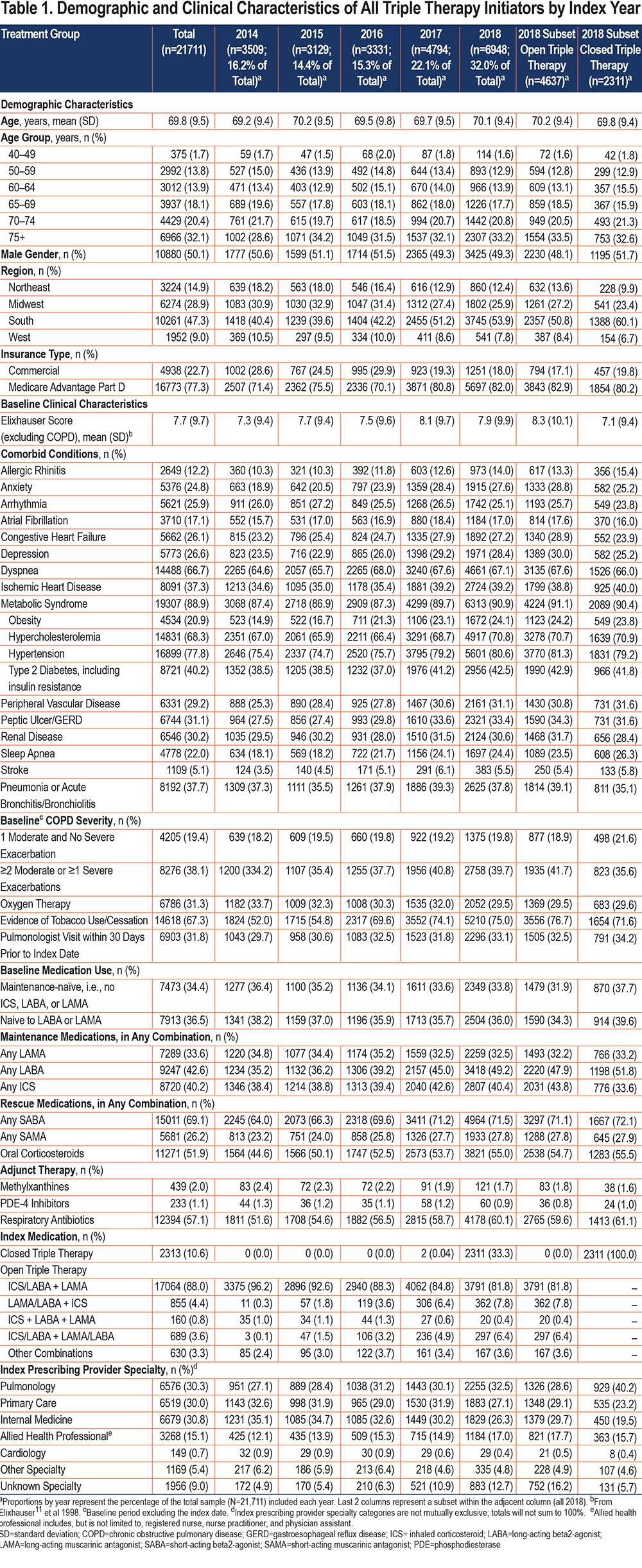
Among the overall triple therapy population, 50.1% of patients were male, and the mean (±SD) age was 69.8 (±9.5) years. ICS/LABA+LAMA was the most common open triple therapy combination. Overall, 34.4% were maintenance-naïve and 61.9% were exacerbation-discordant (i.e., had no exacerbations or only 1 moderate exacerbation history at index). A total of 74.1% were either maintenance-naïve and/or exacerbation-discordant while 22.2% were dual-discordant. Approximately 1 in 5 patients (22.7%) were commercially insured. One in 3 patients (37.7%) had pneumonia and/or acute bronchitis/bronchiolitis during the baseline period. Nearly one-third (31.8%) had a recent pulmonologist visit prior to triple therapy initiation and this specialty’s share of prescribing appears to be increasing over time (Table 1).
Within the closed triple therapy subset, 2 out of 5 index prescriptions were prescribed by pulmonologists (40.2%). Among these patients, 37.6%, 64.4%, and 74.4% of the closed triple therapy starts were found to be maintenance-naïve, exacerbation-discordant, and discordant on at least 1 GOLD triple therapy-specific recommendation, respectively.
Dual-Discordant Cohort
Among the patients who were dual-discordant, 56.4% were male (Table 2). The mean (±SD) age was 69.0 (±9.9) years with the largest proportion of patients (30.3%) in the 75+ year age group. Over a quarter of this cohort was commercially insured; 29% had a baseline diagnosis of pneumonia or acute bronchitis/bronchiolitis. Approximately 1 in 4 (26.6%) of these patients had a recent pulmonologist visit.
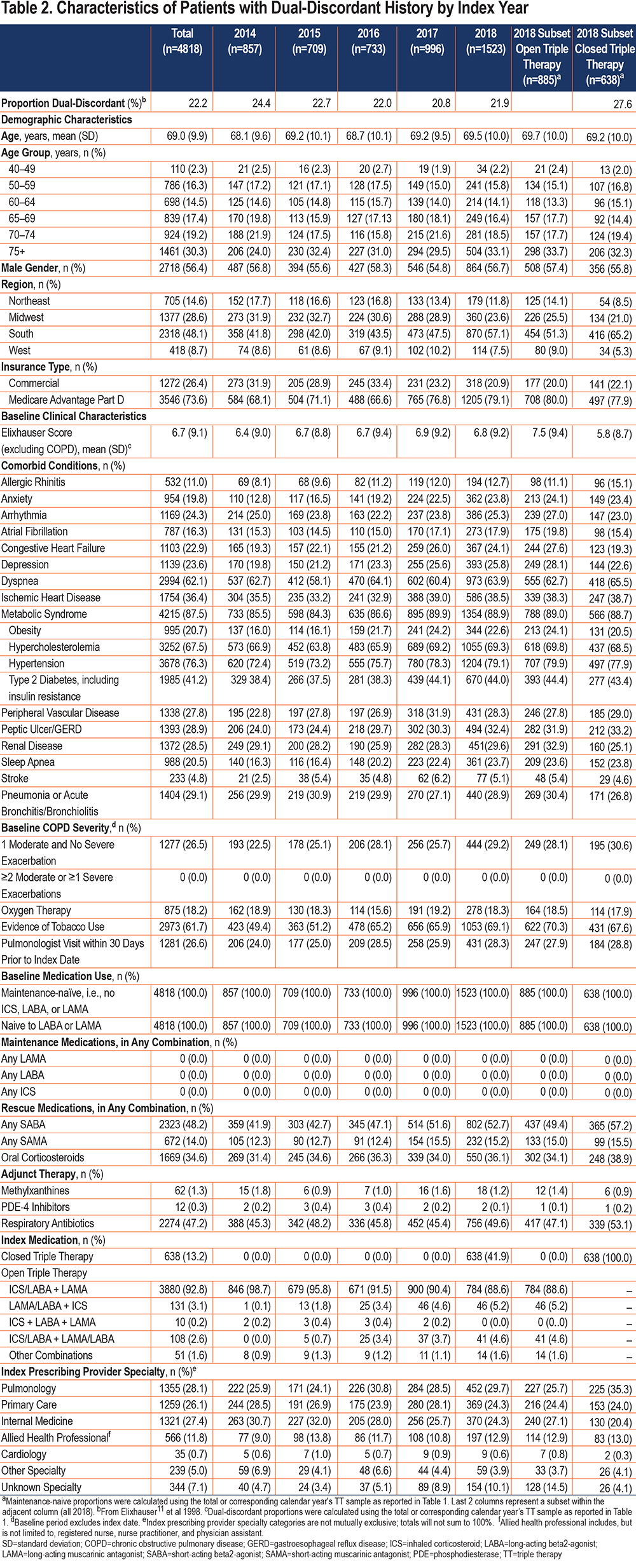
Among closed triple therapy patients, 27.6% were dual-discordant; these 638 patients represented 41.9% of the dual-discordant triple therapy initiators in 2018. A total of 35.3% of the closed triple therapy dual-discordant patients were prescribed by pulmonologists, followed by primary care (24.0%) and internists (20.4%).
Maintenance-Naïve Cohort
Among the maintenance-naïve patients, 53.5% were male, and the mean (±SD) age was 69.5 (±9.8) years; the largest proportion of patients (32.1%) were in the 75+ year age group (Table 3). Approximately 1 in 4 patients (24.2%) were commercially insured. A total of 41.3% of patients had a history of pneumonia or acute bronchitis/bronchiolitis diagnoses and 35.5% were classified as GOLD C/D. Approximately one-third (32.8%) visited a pulmonologist in the prior month and 24.8% were prescribed their index triple therapy by this specialist type. However, internists were the most frequent prescribing type (32.9%) within this group.
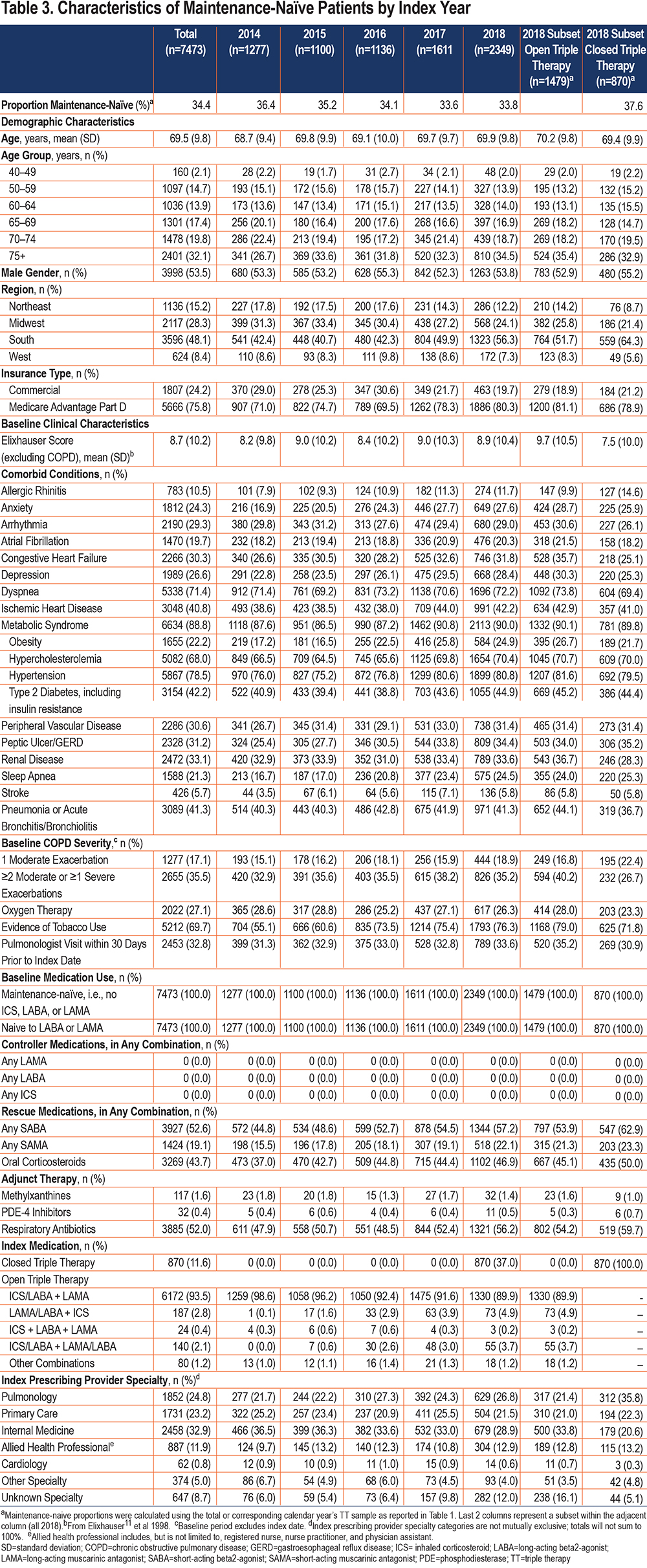
A total of 37.0% of the 2018 maintenance-naïve starts belonged to closed triple therapy . Among the maintenance-naive closed triple therapy subset in 2018, pulmonologists were the largest prescribing group (35.9%).
See Supplementary Table S1 in the online supplement for results on patients with exacerbation-discordant history as the indicator of discordance with GOLD recommendations.
Multivariable Analyses: Predictors of Discordant Prescribing
Odds of Dual-Discordant Prescribing
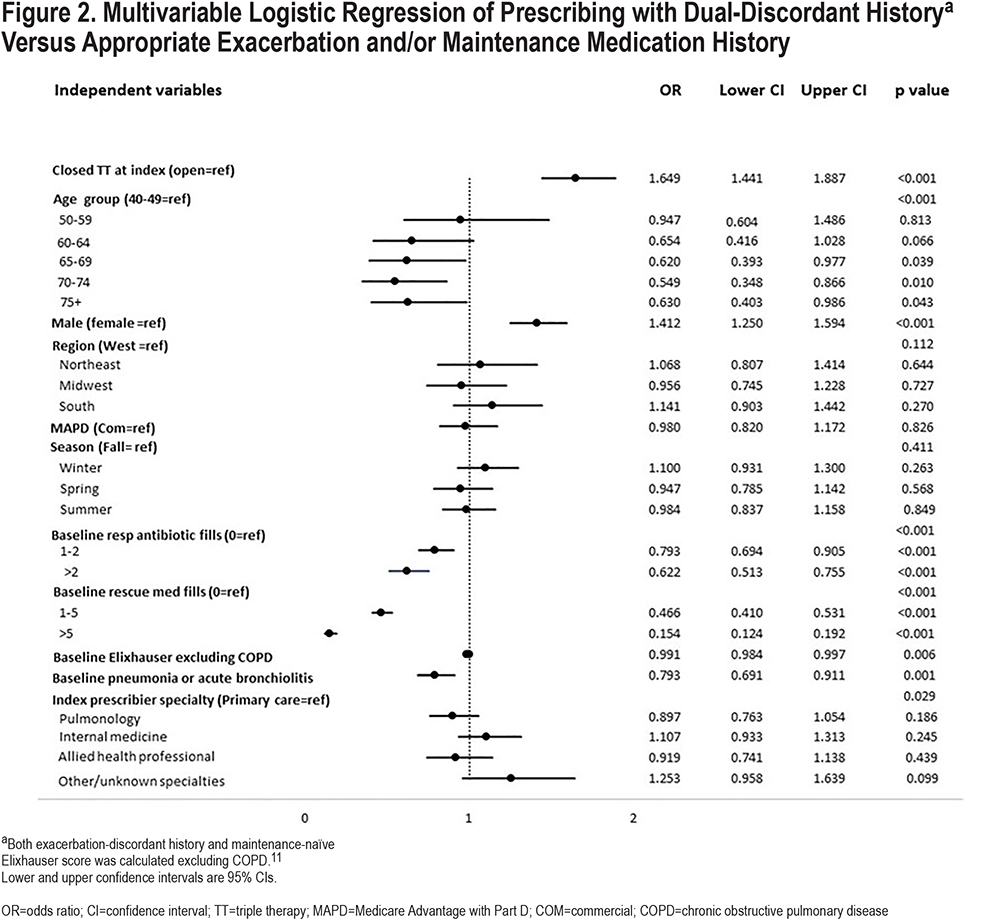
Figure 2 displays the multivariable logistic regression results of dual-discordant history (versus appropriate prescribing per at least 1 criterion). When patients initiated closed triple therapy, as compared with open triple therapy, the odds of being dual-discordant were 65% higher (95% confidence interval [CI]: 1.44–1.89; p<0.001). Males had 41% increased odds (95% CI: 1.25–1.59; p<0.001) of being discordant on both criteria versus females. Conversely, the adjusted odds of discordance with both GOLD criteria were lower among patients with baseline respiratory antibiotic or rescue medication use as compared to those with no respiratory-related antibiotic or rescue medication use, respectively (global p<0.001) (Figure 2). Similarly, the odds of dual discordance were also lower (odds ratio [OR]: 0.79, CI: 0.69–0.91; p<0.001) among patients with a history of pneumonia or acute bronchiolitis versus patients with no such history. The adjusted odds of dual discordance varied significantly across prescribing providers when compared to primary care providers (global p=0.029) but was not associated significantly with any particular index medication prescribing provider specialty (each p>0.05, for pulmonology, internal medicine, allied health, or other/unknown specialties).
Odds of Maintenance-Naïve Status Among Patients with Exacerbation-Discordant History
Among all exacerbation-discordant patients, those receiving closed triple therapy had 1.61 times (95% CI: 1.39–1.88; p<0.001) greater odds of also being maintenance-naïve at treatment initiation, as compared with those receiving open triple therapy (Figure 3). In addition, the adjusted odds of being maintenance-naïve differed significantly based on prescribing provider (global p<0.001); specifically, the odds were 17% lower for pulmonologists (OR: 0.83; 95% CI: 0.70–1.0; p=0.048), while internists were 26% higher (OR: 1.26, 95% CI: 1.04–1.53; p=0.017), versus primary care prescribers, respectively. Significant variation was also observed by age group: specifically, patients ≥65 years of age were less likely (OR range: 0.47–0.56) to be maintenance-naïve compared to their 40-49-year-old counterparts (each p<0.05). Patients with ≥1 fill of baseline rescue medication use had greater odds of maintenance-naïve status (global and pair-wise p<0.001) than patients with no rescue medication. Odds of being maintenance-naïve were 61% higher for patients with baseline dyspnea (95% CI: 1.39–1.86; p<0.001) than non-dyspnea patients. Similarly, patients with a history of pneumonia or acute bronchiolitis had 50% greater odds of being maintenance-naive (95% CI: 1.28–1.77, p<0.001).

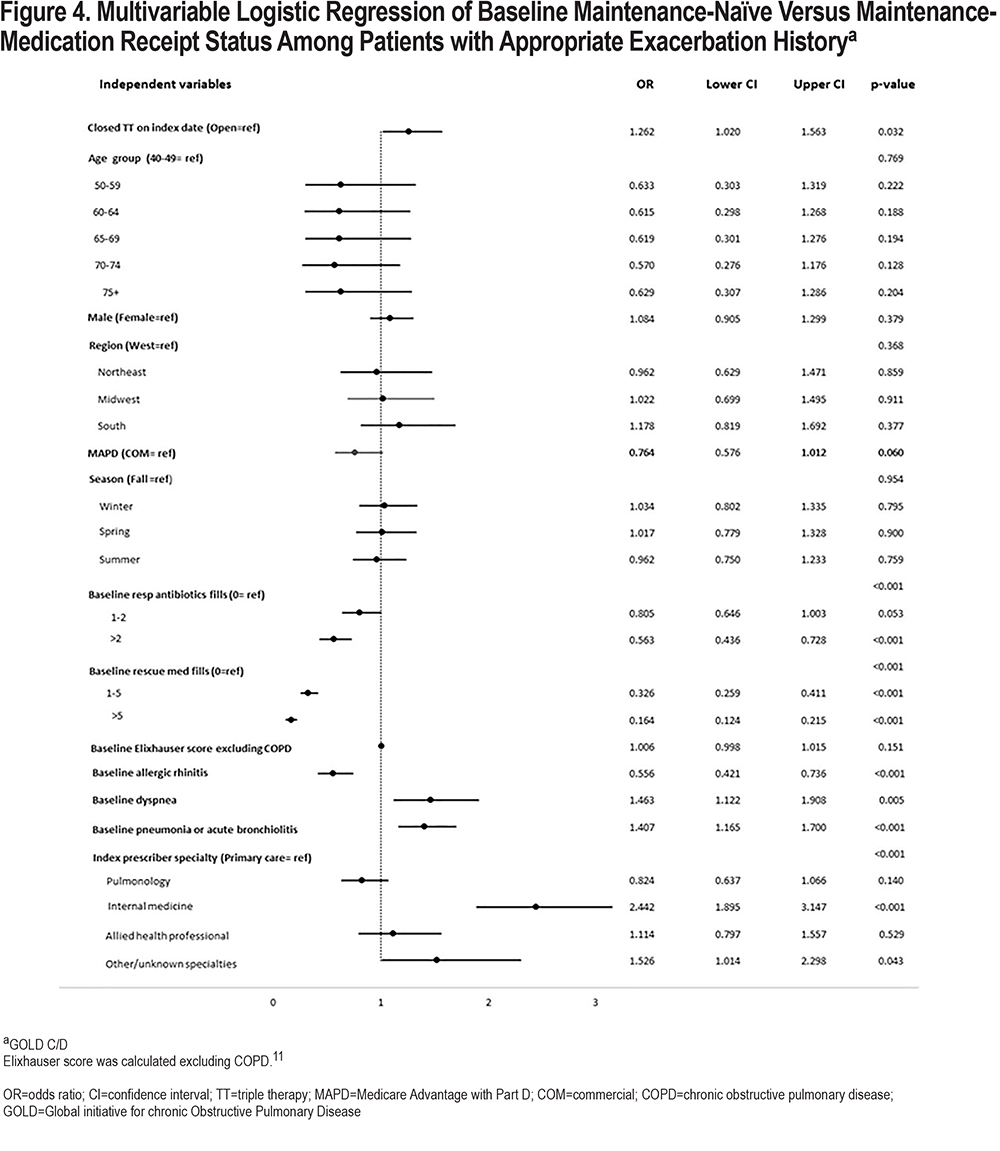
Among GOLD C/D patients (i.e., those who had baseline severe and/or multiple moderate exacerbations, and thus, prescribing was not discordant with GOLD), the adjusted odds of being maintenance-naïve were higher when closed triple therapy was initiated (OR: 1.26, 95% CI: 1.02–1.56, p=0.032) (Figure 4), as compared with open triple therapy. Significant differences in adjusted odds of being maintenance-naïve were also observed among patients with specialty prescribing providers (global p<0.001); specifically, the odds were more than 2 times higher (OR: 2.44, 95% CI: 1.90–3.15; p<0.001) when patients were prescribed triple therapy by internal medicine practitioners versus primary care providers. Patients with a history of rescue medication use also had higher odds of being maintenance-naïve (global and pair-wise p<0.001). Similarly, the odds of being maintenance-naïve were 41% higher among patients with baseline pneumonia or acute bronchiolitis (95% CI: 1.17–1.70, p<0.001) than among patients who did not have baseline pneumonia or acute bronchiolitis. Conversely, patients with appropriate exacerbation history were less likely to be maintenance-naïve if they had comorbid allergic rhinitis (OR: 0.56, 95% CI: 0.42–0.74; p<0.001).
Discussion
To our knowledge, this is the first real-world study to examine a large sample of patients with COPD who initiated triple therapy, and the extent of their misalignment with GOLD recommendations, especially given the entry of closed triple therapy formulation(s) to the market. Specifically, the study evaluated patients who lacked prior exposure to maintenance inhaled therapies (maintenance-naïve) or did not meet the GOLD requirements for exacerbation history (exacerbation-discordant) prior to triple therapy initiation, or both (dual-discordant). Among 21,711 patients with COPD initiating triple therapy between 2014 to 2018, 34.4% were maintenance-naïve and 61.9% were exacerbation-discordant (i.e., classified as GOLD A/B); 22.2% were dual-discordant — i.e., they had both types of GOLD-discordant histories. We also found that 74.1% were either maintenance-naïve and/or exacerbation-discordant. Conversely, only 25.9% of patients were prescribed triple therapy in accordance with GOLD recommendations. Examining 2018 triple therapy initiators specifically, 31.9% and 58.3% of the open triple therapy starts were maintenance-naïve and exacerbation-discordant versus 37.6% and 64.4% of the closed triple therapy starts for the same measures. Previous retrospective U.S. studies have shown similar findings regarding GOLD-discordant prescribing of triple therapy . Substantial proportions (58%–80%) of COPD patients on triple therapy were found to have GOLD-discordant prescribing of this regimen for the same timeframe.9,12 Li and colleagues observed that 60% of mostly Medicare patients prescribed triple therapy between 2012 and 2014 had no exacerbations or only a mild one, not requiring hospitalization, prior to escalation.6 Simeone et al found that 60%–75% of patients receiving triple therapy between 2009 and 2013 had only mild or moderate disease.7 This suggests that despite efforts to increase awareness about appropriate prescribing, triple therapy prescribing has been and continues to be excessive and contrary to GOLD recommendations.
Between 2008 and 2015, while COPD diagnosis rates among people aged 40 and older decreased, overall maintenance drug usage increased.13 Concurrently, spending attributable to bronchodilators and maintenance therapy also increased between 2008 and 2015.13,14 While this study was limited in its exploration of non- triple therapy maintenance therapies, the overprescribing trends of triple therapy reported in previous published literature6,7 support our conclusions. The launch of closed triple therapy may have also further contributed to higher triple therapy use. Even adjusting for potential confounders, we found that closed triple therapy initiators were more likely than their open triple therapy counterparts to be discordant on both GOLD criteria. Additional data are needed to confirm these findings and whether the closed triple therapy launch has had a longer-term impact on GOLD-discordant prescribing. While this study was not designed to identify the reasons underlying the higher rate of GOLD-discordant prescribing with closed triple therapy, it could be hypothesized that the ease-of-use of a single inhaler “umbrella treatment” may have contributed to the worsening of ongoing GOLD-misaligned care patterns. There may also be some uncertainty about individual patients having COPD and/or asthma as underlying disease.
A systematic review and meta-analysis of randomized controlled trials comparing open and closed triple therapy concluded that there were no differences between the 2 formulation approaches with respect to exacerbations, FEV1, and quality of life.15 While it has been theorized that a single inhaler triple therapy may help improve treatment adherence versus multiple inhalers, this is yet to be documented.16,17 Observed pathways of escalation to triple therapy and associated outcomes are quite diverse among the retrospective studies performed to date.18 More U.S.-based, real-world analyses are needed to provide guidance and awareness for prescribers, especially taking into account individualized therapy choices based on symptoms and function.19
Nonetheless, GOLD-discordant triple therapy prescribing has been substantial and has been observed before closed triple therapy was available.20 Lack of access to specialists21,22 and low spirometry testing may be contributing to the problem of non-triple therapy maintenance inhalers’ underuse in some cases and leading to triple therapy overprescribing for others. This study observed that generalists are engaged in GOLD-discordant triple therapy prescribing on a larger scale than pulmonologists. Approximately 75% of patients who were maintenance-naïve were initiated on triple therapy by non-pulmonologists. Similarly, 65% of patients who had dual-discordant prescribing, were initiated into triple therapy by primary care, internal medicine, and allied health care providers. For GOLD A/B group patients, multivariable analyses showed that the adjusted odds of being maintenance-naïve were lower for patients whose index triple therapy was prescribed by a pulmonologist as compared with those prescribed by primary care physicians. Furthermore, GOLD C/D group patients whose triple therapy was prescribed by internal medicine specialists had 1.44 times greater odds of being maintenance-naïve. It is possible that patients with COPD are not referred to specialists frequently enough. Despite many published efforts to provide clarification on COPD treatment options,4,23,24,25 it is possible that more efforts to inform prescribers would be helpful in their determination whether to prescribe triple therapy or non- triple therapy alternatives. Alternatively, increased payer guidance or restrictions on closed triple therapy, like those observed in other countries26 may need to be pursued to curtail excess triple therapy use.
Limitations
Health care claims offer a rich source of information on health and health care patterns in large samples of patients. However, claims-based studies may be limited by their inherent nature. Because claims are generated for the express purpose of billing, rather than research, they may be subject to miscoding and missing information. As to medication use, there is no way to know if a patient used a physician sample or another patient’s medication.
They also lack certain clinically relevant data, such as lung function measures and smoking status, and symptom data that could classify patients by COPD severity and be potential confounders for predicting GOLD-discordant triple therapy initiation. Not all possible courses of chronic airflow limitation were restricted; for example, patients with bronchiectasis or previous tuberculosis may have been included in any cohort. In addition, exacerbations and open triple therapy were defined by established claims-based algorithms yet are subject to misclassification. Defining exacerbations can be limited using claims data, because most mild exacerbations are based on changes in symptomology, which are not captured by claims. In fact, mild exacerbations, usually identified by nebulized budesonide and antibiotics without an outpatient or office visit would be missed.
Furthermore, comparisons between years are only descriptive in nature as statistical testing of changes in discordance were not performed. Finally, the annual proportion of triple therapy initiators was determined without regard for changes in the size of the Optum Research Database during the study period. Some of the apparent increase in the proportion of triple therapy initiators over time may be an artifact of the increasing size of the database.
Conclusions
Triple therapy prescribing appears to have been increasing since 2016. A substantial proportion of patients with COPD who are prescribed triple therapy do not meet GOLD recommendations pertaining to prior maintenance therapy and/or exacerbations. Relative to patients prescribed open triple therapy, those prescribed closed triple therapy were more likely to be dual discordant and naïve to maintenance inhalers. This GOLD-discordant prescribing behavior occurred more often among generalist-specialty prescribers than pulmonologists. These findings support increasing the awareness of GOLD recommendations to counter the continuing overprescribing of triple therapy in individuals with COPD.
Acknowledgments
Author contributions: Authorship criteria conformed to the International Committee of Medical Journal Editors guidelines for authorship. SPB was responsible for data interpretation, implications, manuscript review, and substantial revisions. CB-P was responsible for the acquisition of data, data analysis, and interpretation, and manuscript review and revision prior to submission. EKB was responsible for the acquisition of data, data analysis, and interpretation, and manuscript review and revision prior to submission. LGSB was responsible for conception and/or design of the study, the acquisition of the data, data interpretation, and substantial involvement in the draft and revision prior to submission. SRP was responsible for conception and/or design of the study, the acquisition of the data, data interpretation, and substantial involvement in the draft and revision prior to submission. Writing, editorial support, and formatting assistance was provided by Caroline Jennermann, MS, an employee of Optum, which was contracted and compensated by Boehringer Ingelheim Pharmaceuticals, Inc., for these services. We are grateful to Krista Schladweiler, PhD, (krista.schladweiler@gmail.com) for essential work on this study.
Data sharing: The database utilized for this study contains proprietary elements owned by Optum. Data cannot be broadly disclosed or made publicly available. The disclosure of data to third-party clients requires certain data security and privacy protocols and a standard license agreement including restrictive covenants governing use of the data.
Declaration of Interest
SRP is an employee of Boehringer-Ingelheim Pharmaceuticals, Inc. LGSB, CB-P, and EKB are employees of Optum. SPB was a key opinion leader and consultant for this study. SPB reports serving on advisory boards of GlaxoSmithKline and Sunovion.