Running Head: COPD Chronic Care Management Collaborative
Funding Support: This work was not funded.
Date of Acceptance: March 21, 2022 | Published Online: March 23, 2022
Abbreviations: chronic obstructive pulmonary disease, COPD; emergency department, ED; Centers for Medicare and Medicaid Services, CMS; Hospital Readmissions Reduction Penalty program, HRRP; performance improvement, PI; academic medical centers, AMC; transitions of Care, TOC; baseline, BL; remeasure, RM; electronic health record, EHR; respiratory therapist, RT; obstructive sleep apnea, OSA; best practice alert, BPA; long-term acute care, LTAC; short-acting beta2-agonist, SABA; inhaled corticosteroid, ICS; pulmonary function test, PFT; Epic Systems Corporation, EPIC; heart failure, HF; primary care provider, PCP; frequently asked questions, FAQ; skilled nursing facility, SNF; extended care facility, ECF; acute exacerbation of COPD, AECOPD
Citation: Press VG, Randall K, Hanser A. Evaluation of COPD chronic care management collaborative to reduce emergency department and hospital revisits across U.S. hospitals. Chronic Obstr Pulm Dis. 2022; 9(2): 209-225. doi: http://doi.org/10.15326/jcopdf.2021.0273
Online Supplemental Material: Read Online Supplemental Material (268KB)
Introduction
Chronic obstructive pulmonary disease (COPD), a chronic, progressive disease of the lungs, affects at least 16 million Americans,1,2is a leading cause of disability,3,4 and is the fourth leading cause of death in the United States.2 While COPD can be managed with effective interventions, patients often do not receive appropriate or timely treatment, leading to worse clinical outcomes, high resource utilization (e.g., emergency department (ED) visits and hospitalizations), and high costs.5,6 In 2010, this disease cost over $30 billion each year in health care expenses in the United States, and costs were expected to reach nearly $50 billion by 2020.2 The majority of costs are related to acute care utilization, including ED visits and hospitalizations,5,6 many of which are considered preventable.7 Early (30-day) hospital readmissions, of which COPD is the third-leading cause among the Medicare patient population, are particularly considered to be preventable due to their proximity to the index admission.8
There are a myriad of reasons why these early COPD readmissions might occur, including inadequate in-hospital treatment for the initial exacerbation and/or insufficient transition of care interventions to help support patients after discharge.1,9-14 With respect to the former, one study of inpatient quality of care found that only one-third of patients received “ideal” care for their COPD exacerbation.9 With respect to the latter, studies show patients have inadequate skills for using respiratory inhaler devices critical for delivering medications to control symptoms;10 additionally, studies have shown that effective teaching strategies can be provided during hospitalization and can reduce these early hospital readmissions.11-14
To address these excessive early readmissions after admission for COPD exacerbations, the Centers for Medicare and Medicaid Services (CMS) initiated a Hospital Readmissions Reduction Penalty (HRRP)7 for COPD as of fiscal year 2014. Hospitals across the United States sought opportunities to implement evidence-based practices to improve the quality of care and reduce excessive readmissions after hospitalization for COPD.15Multiple single site studies have been conducted, with varying success. One reason that hospitals might fail to show improvements is lack of on-site expertise in identifying and/or implementing effective interventions and/or lack of on-site expertise on how to evaluate program metrics effectively.16,17 Therefore, to aid hospitals with translating existing evidence of effective strategies into practice in a supported environment, Vizient, Inc., developed a COPD performance improvement collaborative to support enrolled hospitals through program/intervention implementation with opportunities for simultaneous subject matter expert-provided education on evidence-based interventions and implementation approaches and mentoring and peer-support sessions. This report aims to share the results and lessons learned from the multi-site collaborative.
Methods
Setting and Design
Vizient, the setting for the collaborative, is a health care performance improvement company, serving more than half of the health care organizations across the United States. As part of Vizient’s network, the Performance Improvement (PI) Collaboratives program provides evidence-based research and collaboration to address challenges across the health care continuum, resulting in organizations’ improved performance. The COPD Chronic Care Management Collaborative was 1 of 16 Vizient PI collaboratives offered in 2020. These PI collaboratives focus on connecting health care organizations committed to improving together by exchanging ideas, knowledge, and experience to advance patient care. Improvement collaboratives use an evidence-based PI model that incorporates components of Lean, "plan-do-study-act," and Six Sigma’s “define-measure-analyze-improve-control,” etc., complementary to other methodologies used by enrolled hospitals. Topics for the collaboratives are obtained via surveys of Vizient members annually. Based on feedback from the Vizient membership, a PI collaborative was developed to examine, improve, and support the intervention implementation of COPD programs among Vizient members.
COPD Collaborative Overview
The COPD Collaborative enabled and offered participating hospitals and health care organizations to collectively work on improving patient navigation through various care access points, patient outcomes and disease education, awareness, and overall support for the COPD patient population. The Collaborative was a multi-month, PI-focused initiative with bimonthly virtual meetings focused on education from subject matter experts and peer-to-peer networking.
In June 2019, Vizient convened a planning committee including 2 subject matter experts (VP and RG) from health care systems along with internal stakeholders to develop and finalize the Collaborative project’s scope. The team was comprised of health care administrators, nurses, and medical experts. The program was designed to provide 6 educational webinars on topics relevant to developing, implementing, and evaluating COPD readmission reduction interventions. The 6 monthly talks were provided by 1 of 2 subject matter experts (VP or SG) and included the following topics: medication management, patient education and self-management, interprofessional care teams, technology innovation for COPD readmission reduction, population health management, post-hospital strategies, and post-acute and community support. These educational webinars were each followed by a corresponding networking webinar. The 6 peer-to-peer, networking, hour-long meetings focused on enrollees discussing their progress updates and receiving expert coaching from the subject matter expert(s).
Project Focus and Collaborative Goals
This Collaborative focused on assisting multiple sites with the implementation of effective COPD care management strategies, standard practices, and evidence-based protocols to help reduce disease progression, process variation, and COPD-related emergency department revisits and readmissions. The Collaborative was comprised of 2 parts, and members could participate in either part or the entire collaborative. Part 1: Points of Access focused on improving effective care management and care access to reduce disease progression leading to ED visits and readmissions; and Part 2: Standardized Care explored the leading strategies to incorporate standard practices of care and protocols to reduce process variation and medical errors. The Collaborative’s goals included: (1) increase COPD-patient engagement, education, and long-term self-management, (2) establish community and post-acute care partnerships to increase patient support and effective transitions of care, (3) identify population health management strategies to prevent, monitor, and stabilize COPD, and (4) improve interprofessional team collaboration, COPD-related knowledge, and standardization of workflows and processes.
Site Recruitment and Participation Requirements
Sites were recruited from the Collaborative Program membership that includes nearly 300 members, with over 1000 participating academic medical centers (AMC) and community hospitals. Project recruitment included targeted outreach, marketing in a Vizient monthly newsletter, and hosting an informational webinar to inform program participants of the upcoming project focus, participation requirements, and expected benefits. The COPD Chronic Care Management Collaborative had 47 unique organizations enroll and participate in the 6-month project. Collaborative participation requirements included identifying 3 team members for each enrolled organization, completing a project charter, joining bimonthly virtual meetings for the education and peer-networking sessions, and delivering a progress update. Teams were also required to submit baseline and follow-up remeasure outcome and process metric data.
Intervention Characteristics
Given the variation among health care settings, each site could choose to implement the intervention(s) that they identified through their own formal or informal needs assessment as filling a gap in care quality for patients hospitalized with COPD as they transition home to avoid revisits. Teams submitted their charters, which outlined their chosen interventions based on their needs assessment results within the first month of participation (September 2019). Sites were to report on their identified interventions and the metrics by which they would evaluate their interventions. Examples of interventions included: (1) develop a core interdisciplinary COPD team; (2) identify, assign risk, and track COPD patients; (3) train the trainers for effective patient education; (4) standardized discharge; (5) transition and post-acute processes;( 6) referrals to pulmonary rehabilitation; and/or (7) implement COPD care pathways (among others).
Measurement and Analysis
Participants were asked to submit performance data for 2 outcome measures and 1 process measure. Performance results were submitted twice, once at baseline and a second submission for the remeasure time-period. The outcome metrics assessed participants’ rate of 30-day COPD-related ED visits and hospital readmissions. Process improvement was evaluated by measuring population reach of an intervention as a proxy for impact. Reach was defined as the number of unique individuals affected by a program initiative (e.g., percentage of patients with COPD who received spirometry testing, pulmonary referral, 7-day follow-up appointment, etc.). Cost data were financially quantified using the Agency for Healthcare Research and Quality’s standardized per event cost estimate for 30-day, all-payer, all-cause readmissions.18 Annualized avoided costs were financially quantified by estimating the average cost of an inpatient readmission. The results for the cost avoidance values and number of events avoided were annualized to reflect a 12-month timeframe. The interventions studied varied across the enrolled sites. Examples of interventions and their measures included: (1) the percentage of patients with COPD who received a spirometry test, (2) pulmonary rehabilitation referral, and (3) follow-up appointment within 7 days (among others). Qualitative data on barriers and facilitators were collected through the bimonthly peer-to-peer networking sessions systematically via pre-meeting submitted progress update slides and end-of-session polling and are summarized with quotes below. Descriptive statistics were performed to summarize quantitative data using means, medians, standard deviations, interquartile ranges, and proportions.
Results
Site Enrollment and Characteristics
The Collaborative ran from September 2019 to February 2020, with Part 1 running September 2019 to November 2019 and Part 2 running December 2019 to February 2020. Of the nearly 300 members, 47 members enrolled. Of the enrolled sites, 33 joined for the entire Collaborative (Parts 1 and 2), 3 joined for Part 1 only, and 11 joined for Part 2 only. Sites represented the diverse U.S. geographical regions with 8 participating across the Southeast, 4 from the Southwest, 21 from the Midwest, 12 from the Northeast Coast, and 2 from the Northwest Coast. Hospitals ranged from small (<250 [34–240] beds, 22 hospitals), to medium (>250- ≤500 [251–451] beds, 15 hospitals), to large (>500 [536–3000] beds, 10 hospitals). There was at least one hospital site representing urban, rural, and suburban settings, and hospital sites comprised a mix of AMC and community-based systems.
Outcomes
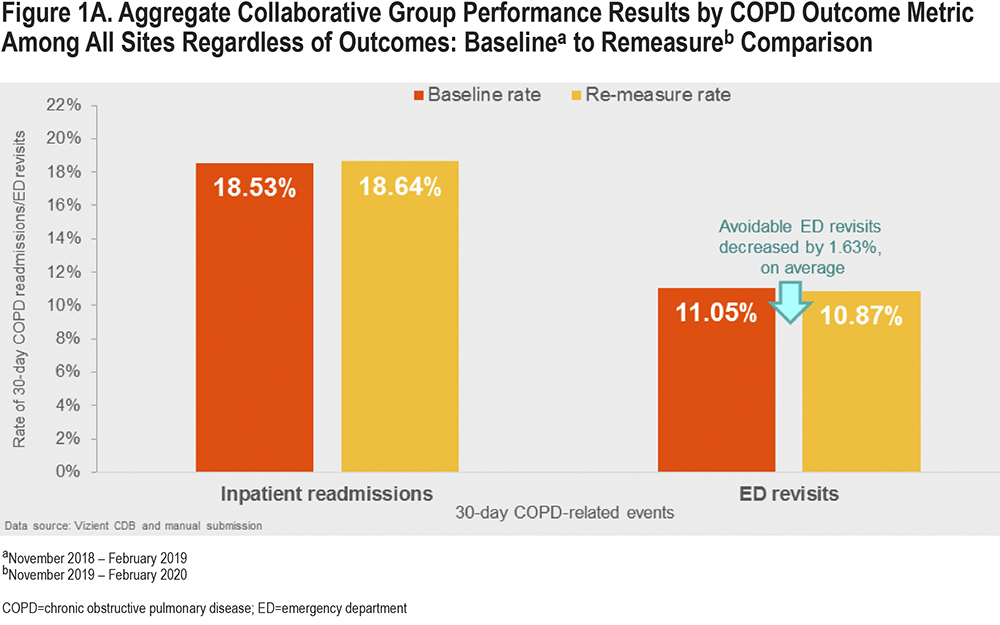
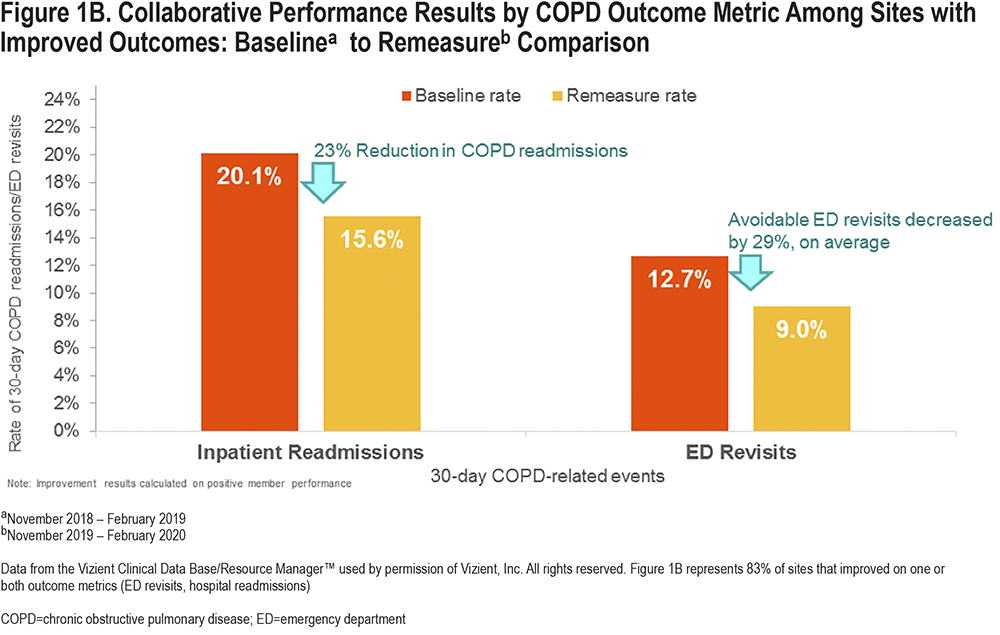
Outcome Measures: Overall, of participating sites who submitted data (n=23/47), the majority (83%, n=19/23) of sites reduced their rate of COPD-related ED revisits and/or hospital readmissions. Of the 23 sites reporting data, 5 reduced both ED revisits and hospital readmissions, while 7 each reduced only ED revisits or hospital readmissions (Table 1, Figure 1a and 1b, Figure 2a and 2b). There were only 4 teams (of those who submitted data) who did not improve in either outcome metric (ED and readmissions). Overall, among all 23 sites, the change in ED visits went from 11.05% to 10.87% (mean 29% [range -4% to -61%]); among the 7 sites that had reductions in ED visits, the reduction was from 12.7% to 9%. Overall, among all 23 sites, there were not reductions in hospital readmissions (18.53% to 18.64%; mean 29% [range -4% to -61%]); among the 7 sites that saw reductions, the readmission rate went from 20.1% to 15.6%. There was a signal that sites with greater participation in the Collaborative were more likely to have improved results. Overall, 68% (n=13/19) of sites with improvements in ED and/or hospital revisits had participation greater than 80%. Among sites with decreased ED visits, 71% (n=5/7) had ≥80% participation. Among sites where rehospitalization decreased, 71% (n=5/7) had 100% participation. Among sites where both ED visits and rehospitalization decreased, 60% (n=3/5) had >80% participation. Among those sites that did not see decreases in ED visits or hospitalizations (n=4) only 50% (n=2/4) had participation >80%.
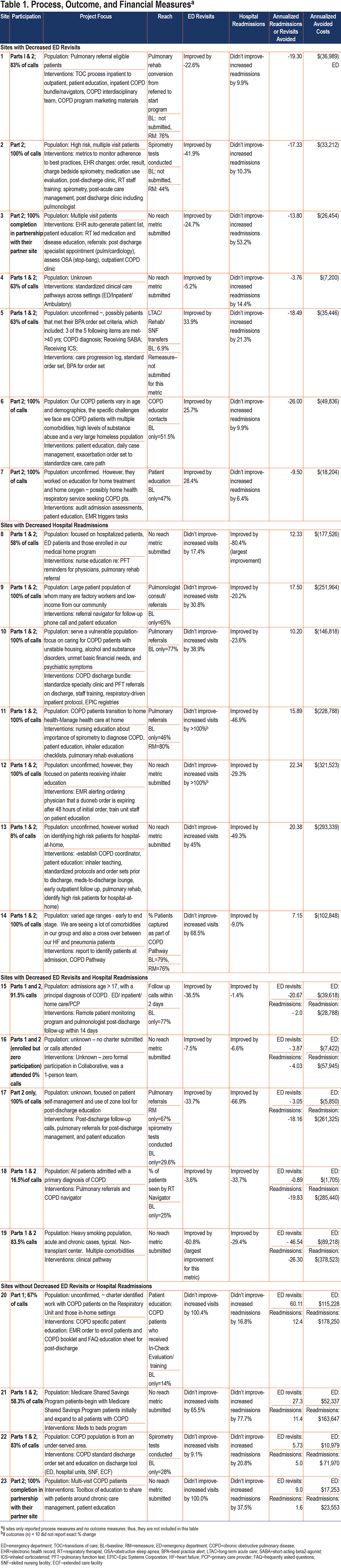
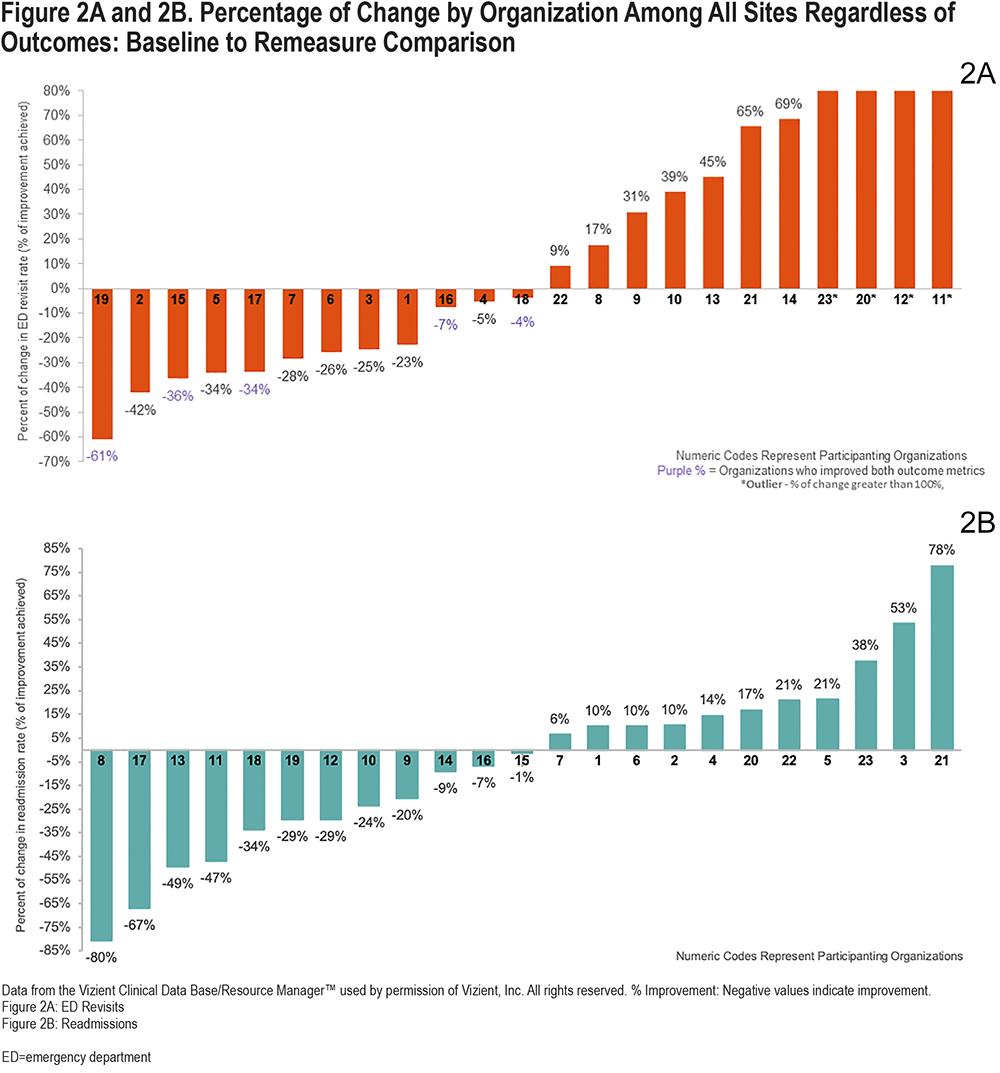
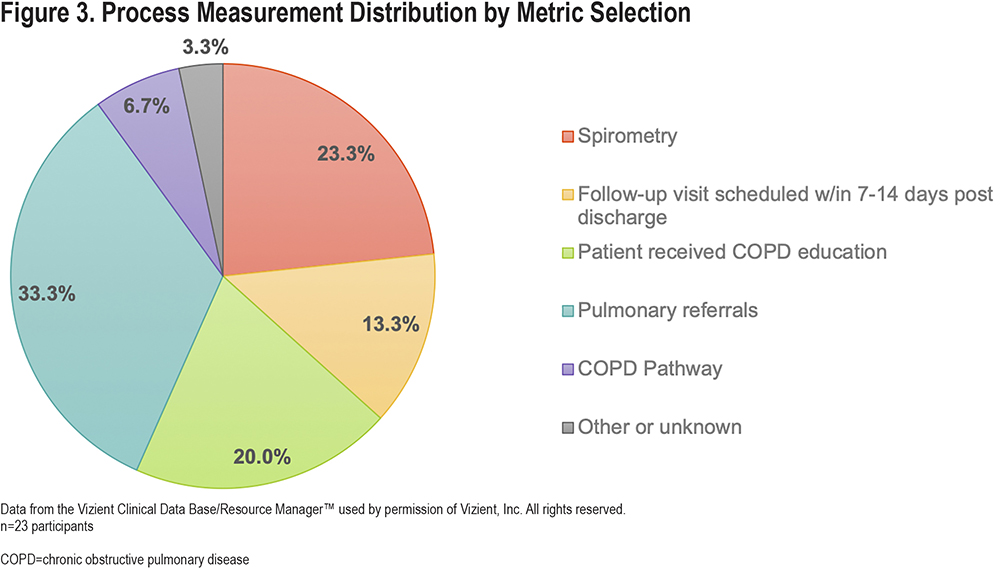
Process Measure: The mean reach, across the 20 hospitals reporting reach for their most successful measure, at baseline reach was 35.2% (SD=26.7%; 17=hospitals) and at follow-up was 73.8% (SD=18.3%; n=6 hospitals). (Table 1) High performers (top quartile/25%) all participated in both Parts 1 and 2 and attended an average of 94% of monthly calls and were a mix of community and AMC facilities and bed size and had a mean reach of 81%. Low performers (bottom quartile/25%) attended an average of 50% of monthly calls, most of whom were community-based hospitals, with varying bed sizes (staffed beds), and had a mean reach of 9.82%. Teams who were above average but not in top 25% attended 100% of monthly calls and were comprised of both community and AMC hospitals; 60% of hospitals had <250 staff beds and had a mean reach of 54.9%. Teams who were below average, but not in the bottom 25%, attended 55.5% of monthly calls; most were comprised of both community and AMC sites, with a wide range of bed sizes (small <250 to large >1000) and had a mean reach of 22.3%. Beyond reach, sites also followed a range of other process measures that included completion of the following (n=number of sites following this process measure): pulmonary referrals (33.3%), spirometry (23.3%), patient education provided (20.0%), 7-14-day post-discharge follow-up visits (13.3%), COPD pathway (6.7%), other process measure (3.3). (Figure 3)
Financial Outcomes: The aggregate cost avoidance for the teams who reduced ED visits was $351,157 and COPD readmissions equaled $2,534,833. (Table 1). Overall, the Collaborative group avoided 183 ED visits and saved $351,157 and 176 hospital readmissions and saved $2,534,833 in COPD and ED readmission costs. The per-event cost for inpatient readmissions used was $14,394, which reflects the average of Medicare and non-Medicare estimates.18 The per-event cost for ED revisits19 was $1,917, and data were collected from 23 participating organizations over 6 months and annualized. The aggregate performance results for the Collaborative were calculated on positive member performance.
Common Barriers and Challenges
Many organizations experienced barriers and challenges that prevented or delayed successful implementation. The following barriers were reported by Collaborative participants during the project: (1) delays in receiving support or approval for information technology departments to to assist, prioritize, create, and/or complete project requests (electronic health records, report automation, customized forms), n=6; (2) lack of organizational support for COPD program development, growth, support, funding, n=5; (3) difficulty identifying and tracking COPD patients, lack of automation requiring manual processes, n=approximately 25 throughout the Collaborative meeting report-outs; and (4) availability and accessibility to pulmonary rehabilitation—referrals, facilities, partners, transportation, n=3.
Qualitative Feedback: Challenges Among Less Successful Sites
There were challenges by some of the sites, particularly those that did not see improvements. One site noted:
“Due to our leader transition, our group has not had an opportunity to meet. We have not made much progress in 2 areas (increase pulmonary referrals and post discharge appointment).”
Another site had difficulty narrowing the scope and stated:
"I should have made them [goals] less complicated. I am super excited because we are moving along. It has been a “process.” It is nice to see an idea take shape. I had to go back and narrow my ideas a few times. I realized I will have to make this change one small step at a time. I understood the time and need for going through so many steps and committees from developing education and writing policies and education. This process was similar but more complex. I had to look at what I wanted to accomplish and break it into smaller process improvements to get to the end goal. I very much appreciate this learning experience."
Some sites began participating during Part 2 of the Collaborative, and at least one site thought their improvements were less successful due in part to the short duration of their participation.
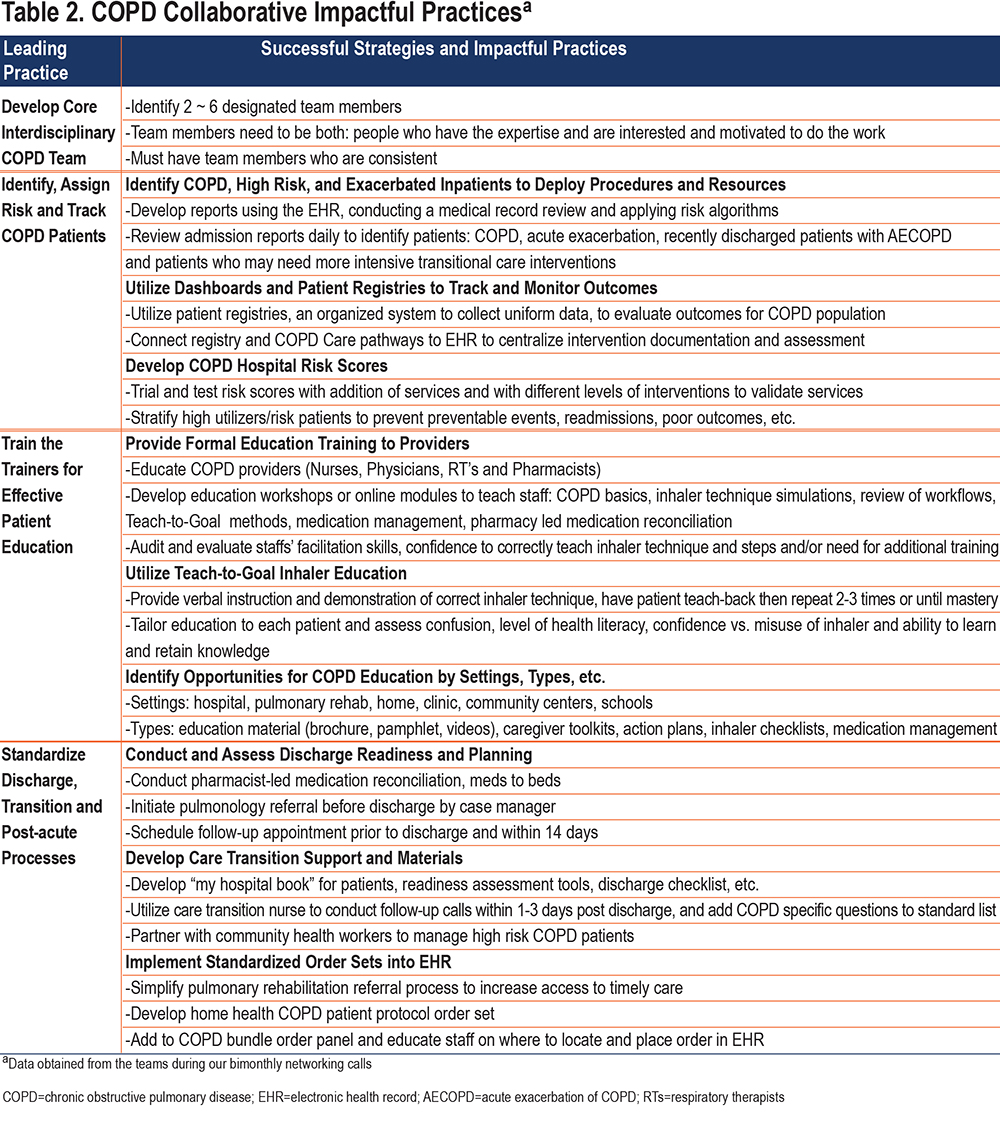
Common Impactful Practices
There were 4 key impactful practices identified by the member sites throughout the Collaborative work and their project updates/progress reports. These included the need to: (1) develop a core interdisciplinary COPD team; (2) identify, assign risk, and track patients with COPD; (3) “train the trainer” education for effective patient education; and (4) standardize the discharge, transition, and post-acute processes. (Table 2)
Discussion
The Vizient COPD Collaborative was able to demonstrate improved utilization outcomes and cost savings by supporting diverse U.S. hospitals to develop and implement COPD readmission reduction programs. The majority of sites reduced ED visits and/or readmissions and the Collaborative overall saved over $2.5 million from avoided acute care utilization. Sites that more fully participated in the Collaborative were more likely to see positive outcomes.
The reduction in ED visits and/or hospital readmissions for patients with COPD realized through this Collaborative is encouraging. Since CMS identified billions of excess costs in potentially avoidable hospital readmissions,7 efforts across the United States have driven to identify and implement successful interventions to reduce these costly events.15-17 The introduction of the CMS HRRP for COPD led to specific efforts to rapidly develop and identify best practices,7 as evidence of effective readmission-reduction interventions was quite limited at the time of policy initiation.20 Several literature reviews and individual interventions have sought to help identify and curate these data.15,17,21 However, most site-specific interventions have lacked power to identify statistically significant readmission reductions,16,17,21 and one randomized study actually found negative results.22 This emerging evidence has been discouraging.
However, the more promising results of this COPD Collaborative may shed light onto pragmatic practices to encourage hospitals to continue to improve the quality of care for patients with COPD through intervention implementation. A key aspect included in this Collaborative that may have been missing was mentored implementation of interventions across U.S. hospitals. Mentored implementation is the use of dedicated expertise to aid clinical sites and their clinical site leads through the process of implementing quality improvement interventions in real-time.23This approach has been used in several prior studies with success at improving medication reconciliation and transitions of care from hospital to home.24,25
Affirming the potential impact of mentored implementation on successful intervention implementation and effectiveness among sites participating in this COPD Collaborative is the finding that both the acute care utilization (outcome measures) and reach (process measure) of programs that more fully participated were improved compared to those that were not able to participate as fully. Participation cannot necessarily indicate cause/effect, but this association may signal that participating in a Collaborative or other form of mentored intervention implementation may support successful intervention implementation and ultimate outcomes.
Overall reach doubled across sites. However, within site pre-to-post data were limited, as some sites only reported at the baseline period while others only reported at the remeasure period, and about one-third did not report any reach results, limiting conclusions that can specifically be drawn about specific improvements in reach by sites and their intervention. Future work in this area should obtain more robust reach data to identify the impact of reach on programs’ utilization and cost outcomes.
In addition to improvements in outcome and process measures around health care utilization and reach, cost-savings were also realized. The Collaborative saved an estimated $2.5 million annualized from a 4-month data collection period to a 1-year performance period among the sites that decreased acute care utilization. Prior evaluations of cost-savings have had more mixed results.16,26 Therefore, while Collaboratives and mentored implementation approaches in general are resource heavy, requiring investment by participating hospital sites and expertise to lead the Collaborative and/or mentored approach could pay off with a non-trivial return on investment.
In addition to the promising findings and insights provided by this Collaborative, the evaluation has some limitations. By design, the Collaborative did not randomize sites, and each site chose their respective intervention(s). Further, interventions were implemented at each site simultaneously over the duration of the Collaborative without piloting at a single site first. This was due to the fact that sites were implementing established evidence-based interventions and/or best practices and were more focused on obtaining Collaborative implementation and evaluation support than testing novel interventions. In addition, participation bias may be present, both in joining the Collaborative and in participation throughout the Collaborative, such that sites that signed up and more fully engaged may have been more likely to have success even without the Collaborative. However, the average number of Vizient sites that participate in collaboratives is 33, so our participation rate overall was above average (with 47 participating sites). Further, around half of the sites did not provide complete data; these missing data may bias our results, however, we presented data and figures to represent the findings as transparently as possible. Additionally, interventions across the sites were not standardized, which could limit generalizability or the results. However, the focus of this Collaborative is to aid hospitals in implementing quality improvement initiatives, rather than test specific interventions. Hence, the findings that greater participation in the Collaborative sessions was associated with improved outcomes support this concept. Future work that includes randomization of sites to collaboratives/mentored implementation versus site-only implementation with more fully complete quantitative and qualitative data reporting could better identify the impact of these types of collaborative or mentored implementation strategy interventions that realize improved patient outcomes and cost-savings.
Despite these limitations, the Vizient COPD Collaborative was able to demonstrate improved outcomes and cost savings by supporting diverse U.S, hospitals to develop and implement COPD readmission reduction programs. A majority of sites saw reduced ED visits and/or readmissions and the Collaborative overall could potentially have saved over $2.5 million from avoided acute care utilization based on the calculated savings. With the CMS HRRP continuing for the foreseeable future, ongoing financial pressures will continue to galvanize hospital efforts to reduce preventable and costly acute care utilization. Lessons from this Collaborative may assist U.S. hospitals with this endeavor. Future work can further elucidate important evidence around the impact of collaboratives to support implementation of quality improvement initiatives.
Acknowledgements
Author contributions: VGP, KR, and AH conceptualized this study, helped design the study, interpreted the data, assisted with data collection and analyses, as well as drafted and revised the manuscript. All authors reviewed and approved the final manuscript. They agree to be accountable for all aspects of the work.
We want to thank all the participating Vizient sites. We also want to acknowledge Raghav Gupta, MD, FCCP, a subject matter expert who provided some of the educational sessions for the Collaborative. We also want to thank the Vizient PI Collaboratives program. Finally, we would like to thank Mary Akel for her assistance with the manuscript submission.
Declaration of Interest
Dr. Press reports receiving honorarium for her work with the Vizient Collaborative. In addition, she reports consulting for Humana and receiving grant funding from the National Institutes of Health, the American Medical Association, and the American Lung Association. Neither Mrs. Hanser nor Mrs. Randall report any conflicts of interest.