Running Head: COPD Self-Management to Impact Quality of Life
Funding support: This work was supported by grants K24HL138150 and R01HL140486 from the National Institutes of Health, Roberto Benzo, principal investigator.
Date of Acceptance: February 28, 2022 │ Published Online: March 8, 2022
Abbreviations: chronic obstructive pulmonary disease, COPD; standard deviation, SD; forced expiratory volume in 1 second percent predicted, FEV1%pred; Self-Management Ability Scale-30, SMAS-30; Chronic Respiratory Questionnaire, CRQ
Citation: Benzo MV, Novotny P, Benzo RP. Adding granularity of COPD self-management to impact quality of life. Chronic Obstr Pulm Dis. 2022; 9(2): 277-284. doi: http://doi.org/10.15326/jcopdf.2021.0277
Introduction
Self-management is considered an essential aspect in chronic obstructive pulmonary disease (COPD) care as it is independently related to health care utilization and quality of life.1,2 Building self-management abilities may empower patients to adopt a lifestyle that agrees with their preferences and values, to become more confident to deal with COPD, and to use health care services more efficiently. In addition, improving quality of life through self-management is one of the leading goals in treating and rehabilitating people with COPD.3
However, there is a knowledge gap on which specific self-management abilities are associated with important aspects of quality of life in COPD like dyspnea, fatigue, emotions, and the confidence to live with COPD (mastery). The 2021 Global Initiative for Chronic Obstructive Lung Disease guidelines3,4 and previous Cochrane Reviews2 identify the need for more granular details on SM to address specific aspects of quality of life. For example, while we know that using an action plan to address an exacerbation is significant for self-management of COPD,2 we do not have granular details on what specific self-management behaviors are associated with improvement in specific quality of life domains. Practices like health coaching and pulmonary rehabilitation could use this valuable information to tailor the self-management programs. Building confidence in specific tasks to improve self-management is at the core of behavior change theory.5
The current approach to self-management is discussing a variety of topics relevant for living with COPD. We hypothesize that specific self-management behaviors are associated with well-defined aspects of living with COPD like dyspnea, fatigue, emotion regulation, and the mastery to live with COPD. Therefore, we aimed to investigate the association of the specific self-management behaviors derived from items of the Self-management Ability Scale-30 (SMAS-30) with the 4 domains of quality of life of the Chronic Respiratory Questionnaire (CRQ)6: dyspnea, fatigue, emotions, and mastery, in a large and well-characterized cohort of patients with moderate to severe COPD. We envision that the presented information may help address self-management more specifically depending on the patient's main problem and move beyond a general approach to self-management.
Methods
The data analyzed represent the baseline assessment of stable patients (no exacerbation in the last 3 months) with moderate to severe COPD that was repurposed from an archival dataset of 3 National Institutes of Health-funded studies for home-based pulmonary rehabilitation (National Heart, Lung, and Blood Institute HL140486, HL138150, HL142933).
Outcomes
The 4 domains of the CRQ (dyspnea, fatigue, emotion, and mastery) were the dependent variables of the models presented. Dyspnea and fatigue are the most common symptoms in COPD patients. The emotion domain refers to how the patient emotionally copes with his chronic conditions, limitations, and changes in social roles. Mastery of the disease is essentially the confidence to manage COPD effectively. The CRQ is a well-validated 20-question disease-specific quality of life inventory asking patients to answer questions using a rating scale of 1 to 7, with higher ratings indicating less symptom impairment regarding the 4 domains.6
The SMAS-30 asks patients to rate on a Likert scale how often they engage in specific activities or how much they agree with various facets of self-management. It includes 6 core abilities (subscales) of self-management: (1) take initiative, refers to being self-motivated in realizing aspects of well-being, (2) invest in resources for long-term benefits, (3) maintain variety in resources, (4) ensure resource multifunctionality (serve multiple dimensions of well-being), (5) self-efficacy in the management of the resources and achieving well-being, and (6) maintain a positive frame of mind. The questionnaire is valid in the COPD, elderly, and frail populations,7 has good internal consistency, reliability, and has demonstrated validity in COPD research.8
A linear regression model was used to define the association of the quality-of-life domain (dependent variables), and the independent predictors included age, lung function (forced expiratory volume in 1 second percent predicted [FEV1% predicted]), gender, and the items of the SMAS-30. The model selection was done using lasso shrinkage methods.9,10 We used LASSO models to find the most parsimonious/robust models possible to avoid overcrowded models that may not inform. Each dependent variable was modeled separately by starting with all the independent predictors in the model and allowing the lasso method to select the best predictors of the dependent variable. Models were validated using bootstrap resampling with 5000 replications. Variables selected in at least 70% of the replicates are included in the final model, and estimates are based on the mean values over these bootstrapped replications.
We focused the analysis on the specific items of the SMAS-30 to provide very granular information on specific self-care actions associated with the CRQ domains dyspnea, fatigue, mastery, and emotions. Every SMAS-30 item consists of a single quotation, as seen in the results section, that were analyzed as independent predictors of CRQ domains. Within the SMAS-30, these items are grouped into the self-management core abilities. However, we did not use the self-management core abilities in the analysis, but instead, the individual items were used to provide the highest granularity to inform potential self-management interventions.
Results
A sample of 512 stable patients with moderate to severe COPD were part of this analysis. The results reflect baseline measures before any intervention started. The age mean (standard deviation [SD]) was 69.6 (9.9) and gender distribution was 54% female, 46% male. The FEV1% predicted mean (SD) was 42.2 (19.0), CRQ total score mean (SD) 17.2 (4.3), CRQ dyspnea domain mean (SD) 4.3 (1.4), CRQ fatigue mean (SD) 3.7 (1.2), CRQ emotional function mean (SD) 4.7 (1.2), CRQ mastery mean (SD) 4.6 (1.4), and CRQ physical score mean (SD) 4.0 (1.2).
The Lasso models found specific behaviors and abilities from SMAS-30 items associated with each particular domain of CRQ (Table 1). Furthermore, all CRQ domains have a positive association with the specific self-management items found significant in the models, as the self-management item improves, the CRQ domain also improves.
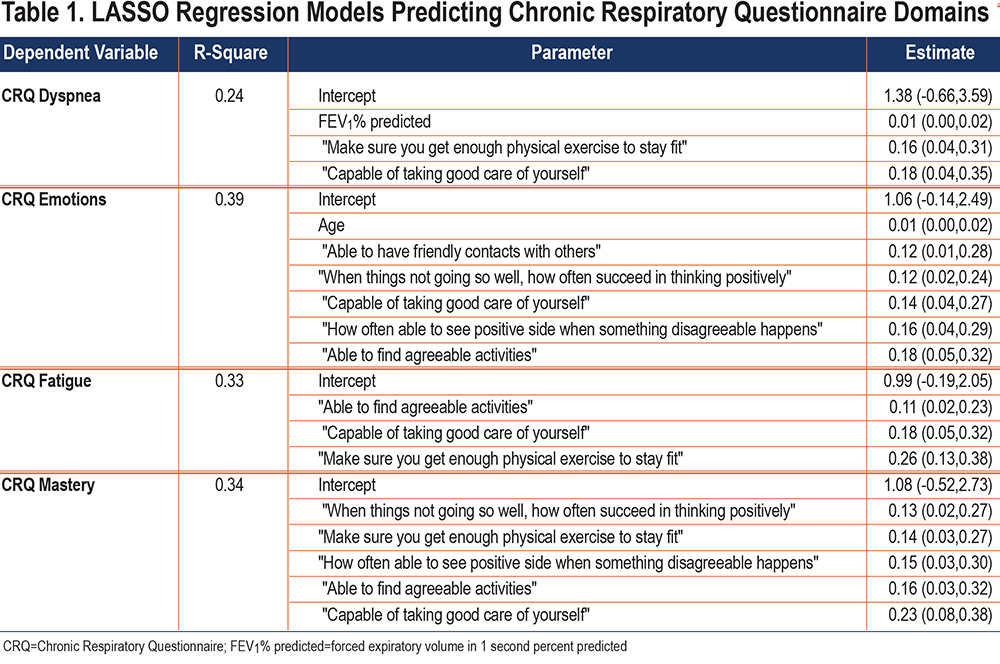
Dyspnea was associated with self-management abilities of investment behavior and self-efficacy. These items included "make sure to do enough exercise to stay fit" and "capable of taking good care of yourself."
The emotional function was associated with self-efficacy and a positive frame of mind. Specific items for self-efficacy are "able to have friendly contact with others," "capable of taking good care of yourself," and being "able to find agreeable activities." For positive frame of mind, items included "when things are not going so well, how often do you succeed in thinking positively" and "how often are you able to see the positive side of things when something disagreeable happens."
Fatigue was positively associated with the self-efficacy item "capable of taking good care of yourself" and investment behavior items "able to find agreeable activities," "capable of taking good care of yourself," and "make sure to do enough exercise to stay fit."
Mastery of disease was positively associated with a positive frame of mind, investment behavior, and self-efficacy. Positive frame of mind items included "when things are not going so well, how often do you succeed in thinking positively" and "how often are you able to see the positive side of things when something disagreeable happens." Investment in behavior items were "make sure to get enough exercise to stay fit," "finding agreeable activities," and the self-efficacy item "capable of taking good care of yourself."
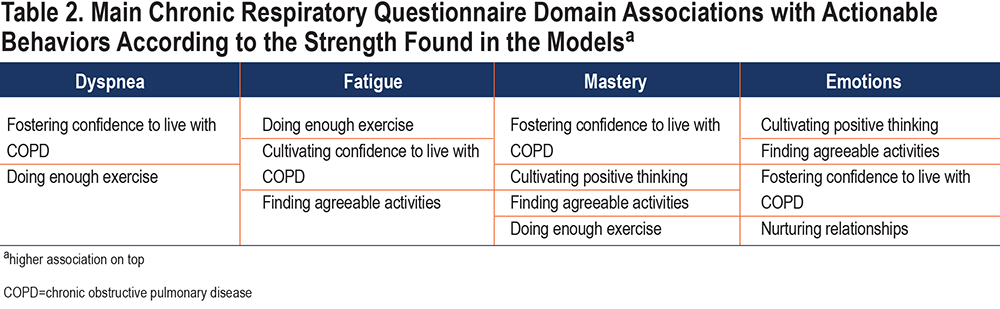
We further categorized the significant actionable behavior independently associated with the 4 CRQ domains (Table 2).
Discussion
We found a positive and significant association between specific self-management abilities with clinically meaningful quality of life aspects in patients with COPD. Our findings may inform the knowledge gap of what self-management abilities need to be addressed to target the most common COPD symptoms. The novelty of this report are the actionable behaviors that health professionals can promote when tailoring a behavior change intervention like pulmonary rehabilitation or health coaching (Table 2). For example, cultivating positive thinking patterns in patients with COPD who deal with difficult emotions. We believe that findings like the one presented here will amplify the scope of the individualized therapy programs.
Confidence (self-efficacy) to deal with COPD was independently and significantly associated with all symptoms/domains (Table 1). The practical interpretation of that finding is critical. It is important to address the confidence of the specific self-management actions or goals. Asking the patient, "how confident are you to ..." is a critical question for any behavior change, and it showed here in this well-characterized cohort of COPD patients. Discussing aspects as the effort needed and the sustainability in the face of obstacles5,11 are important and appropriate. Patients with high confidence in coping with their chronic diseases have a heightened sense of control over their lives.12
Dyspnea
The items that showed to be significantly and positively associated (same direction) with dyspnea CRQ scores were doing enough exercise to stay fit and the sense of mastery of taking good care of themselves (Table 1). Exercise is a critical factor for why traditional pulmonary rehabilitation has been universally effective.13 Our finding confirms the previous report on the importance of self-efficacy (confidence) to deal with dyspnea as a success factor in pulmonary rehabilitation.14
Emotions
Self-management activities that were found to be significantly and positively associated with emotional function were: doing exercise, confidence to deal with COPD, finding agreeable activities, and positive thinking (Table 1). Exercise is a universally well-known self-care behavior that helps manage stress and depression15 and the cornerstone of the traditional pulmonary rehabilitation, and perhaps the reason why pulmonary rehabilitation improves depressive symptoms in COPD.16
Our finding in positive thinking supports our previous report17 and may broaden the options to treat patients with COPD and distressed emotions beyond pulmonary rehabilitation, counseling, and pharmacotherapy. Positive emotions may broaden cognition and behavioral repertoires and build resources that support coping and flourishing.18
The Positive emotions, Engagement, Relationships, Meaning and Accomplishment model (PERMA) may represent a meaningful framework for positive psychology interventions to enhance positivity and hope.19-21
We interpret the association found between emotional function and finding an agreeable activity related to the concept of "optimal experience or flow." When people do activities that they love, they are completely in the present moment, oblivious to anything else.22 In the flow state, the attention shifts to the task at hand, allowing symptoms and limitations to fade.21
Another key component associated with emotions revealed in this analysis is nurturing (active effort) supportive relationships. Our results confirm and extend the previous report about the need to address the quality of relationships and caregiving to improve difficult emotions (anxiety/depression).23,24
Fatigue is the second most common symptom in COPD,25 and was found to be associated with doing enough exercise, finding agreeable activities, positive thinking, and self-care. The positive association of fatigue with positive thinking is certainly novel for COPD and represents an addressable self-management behavior in patients with fatigue.26 COPD patients commonly believe they are not capable of exercising or doing activities of daily living.27
Mastery in dealing with COPD was associated with doing exercise, positive thinking, and confidence (self-efficacy), all powerful skills aimed at sustained well-being.28
Our results extend previous reports indicating that patient-tailored self-management programs are preferable to pre-defined rigid ones, which might contribute to non-adherence.29 Targeting behavior change by trying different self-management activities to improve a specific symptom takes time; it is proven that longer self-management interventions are more likely to improve outcomes.30,31 Health literacy and patient activation are important while incorporating specific self-management abilities.32 In addition, having various self-management options with an appropriate degree of guidance facilitates disease-specific health behavior change and effective self-management.33
Limitations
Our findings do not imply causality. Improving items found significant does not necessarily translate into enhancing the associated outcome. In addition, we did not include the phenotype exacerbation in the models. Our sample consisted of primarily White participants; however, given the sample size, the robustness of the models, and the adjustment to the meaningful covariates for COPD (age, gender, predicted FEV1%), we believe that the models are generalizable to that population. More efforts are needed to recruit a diverse race and ethnicity sample.
Conclusions
We identified specific self-management abilities associated with meaningful and common symptoms in patients with COPD from a very large and well-characterized cohort of patients.
In all, we provide granularity for addressing COPD symptoms during self-management intervention like pulmonary rehabilitation, chronic care management programs, and health coaching. Fostering positive thinking and nurturing relationships represent promising aspects of self-management to explore that may impact the life of COPD patients.
Acknowledgments
Author contributions: RB and MB were responsible for the manuscript's analysis, interpretation, and drafting. PN provided statistical analysis and interpretation of results. RB was primarily responsible for the study design and critical revisions. All listed authors approve this final version and agree to be held accountable for all aspects of the work.
Data availability: Individual, de-identified participant data (including data dictionaries) will be shared if requested to answer a well-specified question, proposed analysis, and reporting plan.
Declaration of Interest
The authors report no conflict of interest.