Running Head: Mild to Moderate Acute Exacerbations of COPD Experiences
Funding Support: This work was funded by Fundação para a Ciência e a Tecnologia under the PhD grant SFRH/BD/147200/2019. This work was also supported by the project “CENTR(AR): pulmões em andamento” via Programa de Parcerias para o Impacto, Portugal Inovação Social through Programa Operacional Inclusão Social e Emprego (POISE-03-4639-FSE-000597), by Fundo Social Europeu through Programa Operacional Regional Centro, and by Programa Operacional Competitividade e Internacionalização (COMPETE 2020 - POCI-01-0145-FEDER-007628; UIDB/04501/2020).
Date of Acceptance: May 4, 2022 │ Published Online Date: May 6, 2022
Abbreviations: acute exacerbation of chronic obstructive pulmonary disease, AECOPD; pulmonary rehabilitation, PR; randomized controlled trial, RCT; Consolidated Criteria for Reporting Qualitative Research, COREQ; Global initiative for chronic Obstructive Lung Disease, GOLD; body mass index, BMI; long-term oxygen therapy, LTOT; COPD Assessment Test, CAT; Web Qualitative Data Analysis, WebQDA; forced expiratory volume in 1 second, FEV1; activities of daily living, ADLs
Citation: Machado A, Almeida S, Burtin C, Marques A. Giving voice to people – experiences during mild to moderate acute exacerbations ofCOPD. Chronic Obstr Pulm Dis. 2022; 9(3): 336-348. doi: http://doi.org/10.15326/jcopdf.2022.0283
Online Supplemental Material: Read Online Supplemental Material (258KB)
Note: Part of this work was presented at the European Respiratory Society International Congress 2021 as an e-poster.
Introduction
Acute exacerbations of chronic obstructive pulmonary disease (AECOPDs) are defined as an acute worsening of respiratory symptoms that result in additional therapy.1,2 A recent proposal on an updated definition of an AECOPD states that these events are characterized by dyspnea and/or cough and sputum that worsens over a period of up to 14 days, possibly accompanied by tachypnea and/or tachycardia, and often associated with increased local and systemic inflammation.3 These events occur on average 0.5–4 times per person/year4,5 and are a major cause of morbidity and mortality (110,000 deaths/year), accounting for 50%–75% of all disease-related costs.1,6-8 AECOPDs lead to a significant decline in individuals’ lung function, exercise performance, and quality of life, and increase their susceptibility to subsequent AECOPDs.1,6,8 The goals of treatment for AECOPDs are, therefore, to minimize their impact and prevent the development of subsequent events.1
Current management of AECOPDs (e.g., pharmacological treatment) is only partly effective, and thus, research on this topic is a well-established priority.9 AECOPDs are heterogeneous in terms of pathobiological mechanisms, severity, and clinical presentation, which leads to different prognoses, management needs, and therapeutic strategies.10-13 People with COPD have reported the need for an increased understanding of the impact of AECOPDs as it appears that physicians have been underestimating it, which may contribute to undertreatment.14 Nevertheless, previous studies have been more focused on people’s interpretation and recognition of an AECOPD than on the experience of the AECOPD itself.15-17 One study14 explored the impacts of moderate AECOPDs from individuals’ perspectives, but its retrospective design (i.e., people recalling the exacerbation experience) may have induced an important recall bias.18,19 Prospective studies on individuals with mild to moderate AECOPDs are needed, since understanding their symptoms, needs, experiences, and feelings can potentially inform treatment strategies.20-22
Pulmonary rehabilitation (PR) is a well-established intervention for the management of stable COPD.1 Evidence for the use of PR in the management of people during and after AECOPDs has been increasing recently.23-25 Nevertheless, quantitative studies have been mainly conducted in hospitalized individuals with AECOPDs, when more than 80% of all AECOPDs are managed on an outpatient basis (i.e., mild to moderate exacerbations)1,26; and qualitative studies have mainly focused on the period following the AECOPD.27,28 Moreover, people with AECOPDs differ from those with stable disease, and currently there are no guidelines on how to conduct PR tailored to individuals’ needs and specificities during an AECOPD.23,25,27,29
Listening to the perceptions of individuals during AECOPDs, understanding their needs, concerns, goals, and expectations is increasingly important to have them involved in a shared decision-making process, and to design and implement PR that is tailored to their preferences.27,30 This person-centered approach could improve the management of AECOPDs and help ensure PR’s effectiveness.27 Thus, this qualitative study aimed to understand individuals’ experiences (i.e., needs, impact, perceptions) during mild to moderate AECOPDs. We also explored their thoughts on PR during an AECOPD as a secondary aim.
Methods
This qualitative study was nested in a randomized controlled trial (RCT)31 evaluating the effectiveness of a PR program during AECOPDs treated on an outpatient basis. The Consolidated Criteria for Reporting Qualitative Research (COREQ)32 was followed. The ethic committees of the Health Sciences Research Unit: Nursing (P618-10/2019), Unidade Local de Saúde de Matosinhos (73/CE/JAS), Centro Hospitalar do Baixo Vouga (15.23-2020) and Administração Regional de Saúde do Centro (85/2018) approved the study. Written informed consent was obtained from all participants prior to any data collection. A phenomenological approach was followed to gain a deeper understanding of the phenomenon (i.e., AECOPDs) through participants’ experiences.33
Participants
A convenience sample was used. Individuals with AECOPDs were consecutively recruited from participants of the RCT between January 2019 and February 2020. Individuals were eligible for the RCT if they were: (1) diagnosed with an AECOPD according to the Global initiative for chronic Obstructive Lung Disease (GOLD)1 criteria, i.e., presenting an acute worsening of respiratory symptoms that resulted in additional therapy (e.g., antibiotics, corticosteroids, bronchodilators); (2) could be included within 48 hours of the diagnosis; (3) managed on an outpatient basis; and (4) able to provide informed consent. Exclusion criteria included: (1) unstable cardiovascular disease, (2) significant musculoskeletal or neuromuscular impairment that precluded the adequate performance of the tests or participation in PR (e.g., amputation, Parkinson’s disease), (3) signs of cognitive impairment, (4) current neoplasia or immunological disease, and (5) any therapeutic intervention in addition to standard of care (i.e., pharmacological treatment). All diagnoses of AECOPD were performed by clinicians at the hospitals and primary care centers involved in the study. At the time of the first coronavirus disease 2019 (COVID-19) lockdown, recruitment stopped since data from individuals with AECOPDs during the pandemic could not be compared with previous data. The pandemic impacted the number and severity of AECOPDs and resulted in significant behavioral and social changes.34
Data Collection
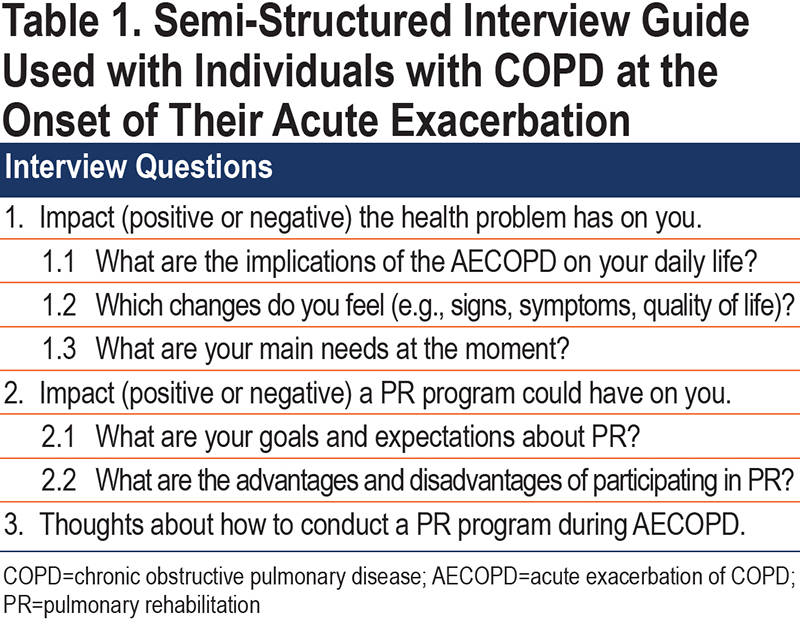
Data collection was conducted at the Respiratory Research and Rehabilitation Laboratory or at participants’ own homes, according to their preference, within 48 hours of the diagnosis of an AECOPD, embedded in the baseline assessment for the RCT. Sociodemographic (age, sex), anthropometric (body mass index [BMI]), and general clinical data (smoking habits, number of self-reported exacerbations in the previous year, use of long-term oxygen therapy [LTOT] and non-invasive ventilation, and lung function – from clinical records) were first collected to characterize the sample. Severity of the AECOPD was classified according to GOLD criteria.1 The COPD Assessment Test (CAT) was used to characterize the impact of the disease, as this is one of the key outcome measures recommended to assess this population1 and the one presenting more robust measurement properties during an AECOPD.35 The total score can range from 0 to 40 and is interpreted as follows: <10 – reduced impact, 10-20 – medium impact, 21-30 – high impact, and >30 – very high impact.36 Then, short, semi-structured, face-to-face interviews were conducted. Semi-structured interviews with open-ended questions were chosen as this approach allows us to understand participants’ experiences and the emergence of new topics that are important to them and have not been previously thought as relevant by the research team.37,38 A semi-structured interview guide (Table 1) informed by the literature, the previous experience of the team, and an experienced qualitative researcher, was used to ensure that the topics under investigation were covered in a consistent manner while allowing for flexibility. The interview guide integrated questions about participants’ experiences during an AECOPD and their thoughts on PR. The interviews were audio recorded (Olympus digital voice recorder WS–750m) and transcribed verbatim, with participants’ names anonymized.
AM, a physiotherapist (PhD student), contacted the participants for the study, led the qualitative interviews, transcribed them, and was involved in the analysis. SA, a gerontologist (PhD), reviewed the transcriptions and was involved in the analysis. CB, a physiotherapist (senior researcher), and ASM, a physiotherapist (senior researcher), reviewed the themes and coding and discussed them with AM and SA.
Data Analysis
Descriptive statistics (i.e., absolute and relative frequencies, mean±standard deviation and median [interquartile range]) were used to describe the sample.
Qualitative data was analyzed using deductive thematic analysis since there were preconceived themes expected to be found (i.e., impact of an AECOPD, needs during an AECOPD, and thoughts about PR) which the research team wished to investigate while still maintaining flexibility to allow for the generation of new themes.39 The 6-step procedure of Braun and Clarke was followed.39 First, 2 researchers (AM and SA) familiarized themselves with the data by reading and rereading the transcriptions before the coding process began; independently organized units of text under each code, creating additional codes if new issues were identified; and organized the codes in themes and subthemes by combining the codes with similar or related ideas. Then, all researchers reviewed the data coded under each theme/subtheme, contributed to the appropriate naming and definition of the themes, and produced the report. The initial themes and subthemes found independently were compared between researchers (AM and SA) and, in case of disagreement, consensus was reached by discussion. All interviews were anonymized by assigning pseudonyms to each participant. The analysis of the transcripts was conducted using the Web Qualitative Data Analysis (WebQDA) software. Representative quotes were included to support the interpretation of the identified themes and subthemes.
Rigor and Trustworthiness
The criteria of credibility, transferability, dependability, and confirmability were used to ensure rigor and trustworthiness.40 Credibility was ensured through: (1) researcher triangulation, i.e., 2 researchers analyzed each interview independently and then compared the analysis and agreed on the final themes/subthemes, (2) continuous discussion of the analysis and interpretation of the data with the entire research team, and (3) presentation of all the representative quotes in the results and supplementary material. Transferability was ensured by describing the characteristics of the researchers, participants, data collection, and analysis in detail. Dependability and confirmability were ensured by triangulating the independent analysis of 2 researchers with different experiences and backgrounds and discussing every step of the process with the entire research team.
Results
Twelve individuals with AECOPDs were approached to participate in this qualitative study and all agreed to participate. One was excluded after enrollment due to diagnosis of asthma-COPD overlap. Therefore, 11 individuals with AECOPD (9 male, 67±10 years, forced expiratory volume in 1 second [FEV1] 41±16%predicted, BMI 27±4kg/m2) were included in the analysis. Baseline characteristics of the study population are present in Table 2.
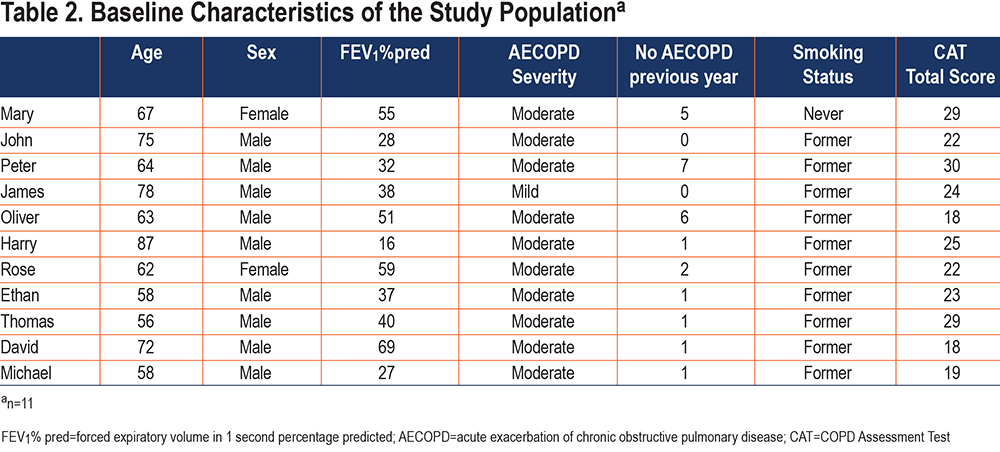
Most participants were married (n=8; 73%), retired (n=9; 82%,), and had completed primary school (n=7; 64%). The CAT scores revealed the disease had a high impact on most participants. Only 2 participants used LTOT and 1 used non-invasive ventilation. About half of the sample (n=6; 55%) had previously participated in PR during the stable phase of their disease. The median interview time was 5 min, 40 sec (shortest: 3min; longest: 9min, 3sec).
Four main themes were identified: impact of the AECOPD, dealing with an AECOPD, main needs during an AECOPD, and (un)certainty about PR. All themes and related subthemes are described in the following section and supported by quotations. Additional interview quotations can be found in the online supplement.
Impact of Acute Exacerbations of COPD
All participants reported a negative impact of the AECOPD, which was described with 6 subthemes: symptoms, physiological changes, limitations in activities of daily living, social constraints, psychological and emotional challenges, and family disturbances (Figure 1).
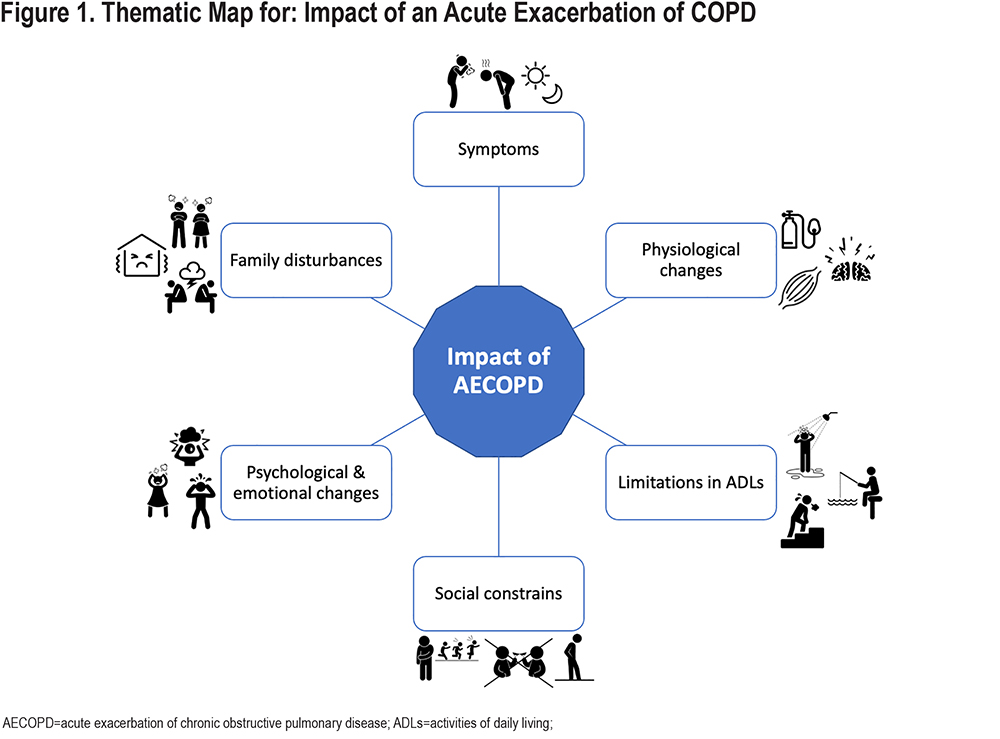
They all experienced the presence of several symptoms, namely shortness of breath, tiredness, lack of energy, cough, sputum, wheezing, pain, and sleep disturbances, which often severely limited their daily life. Participants felt that some symptoms, such as shortness of breath and tiredness or cough and sputum, were related to each other and fluctuated through the day, being worse in the morning and at night, or when they had to exert an effort.
“I feel really tired in the morning, I barely get up. As soon as I put my feet on the ground, I start dressing and I’m already tired. …. My chest feels very tight. It seems that I have to make a huge effort to be able to breathe.” (Peter, 64)
Individuals with AECOPDs experienced some physiological changes, such as the loss of mental abilities and the lack of oxygen to help their brain and muscles to work.
“As I get older, I feel that the respiratory crises are getting worst, heavier, stronger. I feel increasingly less knowledgeable. I’m losing my abilities, both mental and physical.” (Mary, 67)
Limitations in activities of daily living were also highly reported. Participants felt that the AECOPD limited their ability to perform their usual activities, both basic (e.g., walking, climbing stairs, dressing, personal hygiene) “It is very hard to breathe, I can’t climb the stairs.” (Mary, 67); instrumental (e.g., doing household activities, buying groceries, talking, getting transportation) “… I can’t even leave the house to catch the bus” (Mary, 67); and advanced (e.g., working, fishing, singing, going out with friends).
AECOPDs also resulted in social constraints. Participants felt that they were not able to keep up with their peers, felt isolated, were ashamed of having symptoms in front of others, and indicated that their self-sufficiency was affected.
“I don’t want to expectorate in front of others, it is not pleasant. Not for me, even less for the others.” (Ethan, 58)
The AECOPDs impacted participants’ psychological and emotional well-being. Individuals with AECOPD mentioned feeling down, scared, anxious, nervous, and frustrated and had little desire to do things or even leave the house.
“Sometimes I get angry because I want to do something, and I can’t… I feel frustrated.” (David, 72)
Lastly, David revealed that AECOPDs impacted not only people with AECOPDs but also their families.
“The sputum makes me feel desperate and then I bother my family, I know it.” (David, 72)
Dealing with Acute Exacerbations of COPD
Dealing with an AECOPD was described within 2 subthemes: (not) depending on others and planning and compensation strategies (Figure 2).
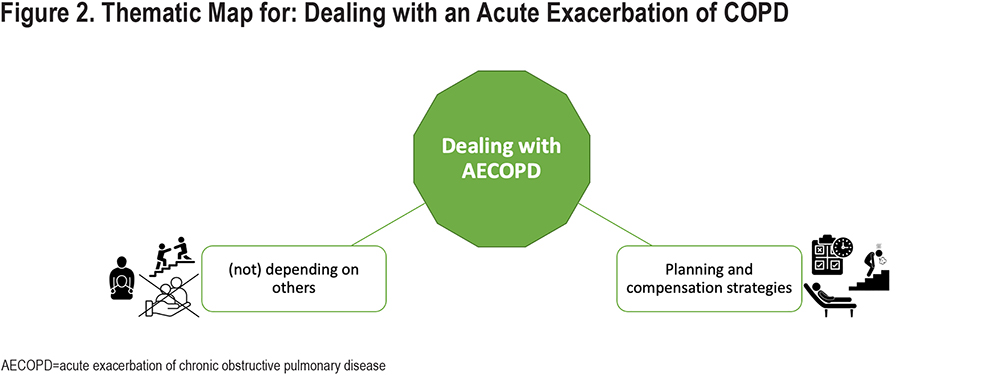
A dichotomy emerged regarding dependency on others, with participants reporting the need to rely on family for support with showering or climbing stairs, and others not wanting to be dependent. As James said:
“I shower alone. Sometimes my wife is at home, others she is not, because she has her own things to do, and often I only shower when she is back. Usually I shower alone, but I always calculate more or less how I am feeling so I don’t have any problems.” (James, 78)
Participants mentioned that during an AECOPD they do fewer daily activities, perform everything more slowly, and feel the need for taking breaks. They also plan their routines depending on how they are feeling and try to compensate for their symptoms by using breathing strategies and laying down barely moving. One participant reported using LTOT but not feeling dyspnea relief.
“I reduce my daily activities. I also have to do them slower, but I reduce them. And I recover, and then I do another one. … Sometimes I think to myself, yoga breathing, with your belly, and it helps.” (Rose, 62)
Main Needs During an Acute Exacerbation of COPD
Four main needs during an AECOPD emerged: to breathe better, to feel less tired, to get rid of sputum and to be able to walk (Figure 3).
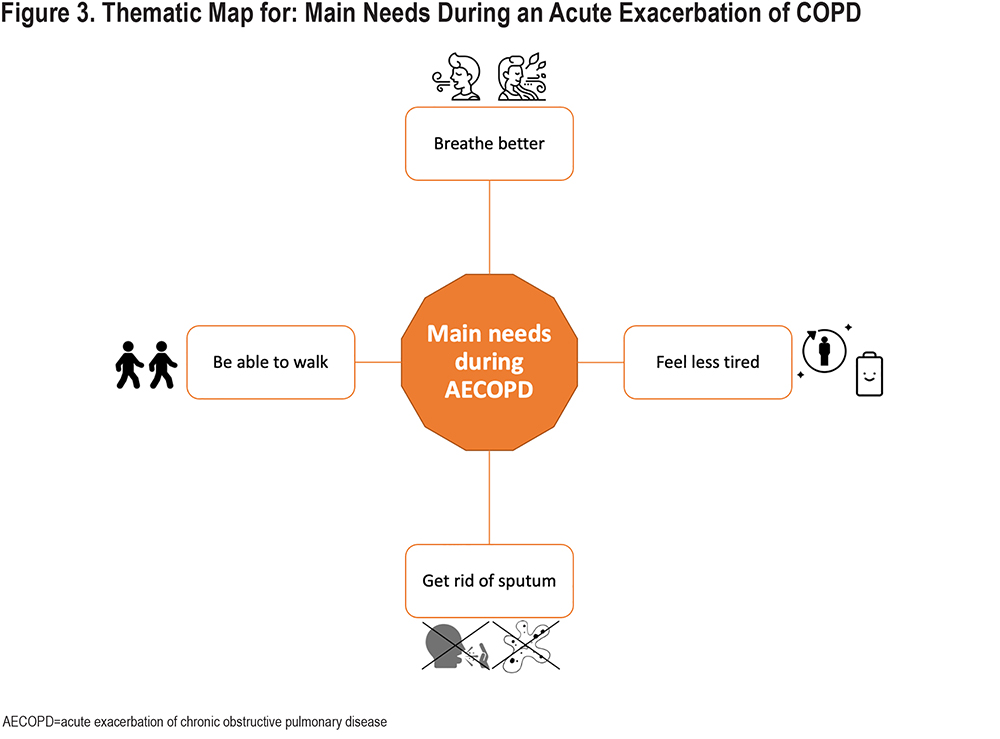
The main needs of participants were focused on improving symptoms.
“I just wanted to get my chest better. The breathing. It is important, very important to me.” (Oliver, 63)
“I need to feel less tired. My problem is really the general tiredness.” (Peter, 64)
“My main need is the sputum, to get rid of this sputum. It is something that bothers me. If I don’t have sputum, then I also don’t have the need to cough.” (David, 72)
Nevertheless, Michael also drew attention to:
“Hmm... I would like to be able to walk like I used to walk.” (Michael, 58)
(Un)certainty about Pulmonary Rehabilitation
Individuals with AECOPDs with previous PR contact shared their (un)certainty about PR through 5 subthemes: lack of knowledge, get better, exercises, design and timing, and trust in health professionals (Figure 4). Individuals naive to PR had more difficulties addressing this theme and the 3 subthemes that emerged for this group were: lack of knowledge, exercises, and design and timing.
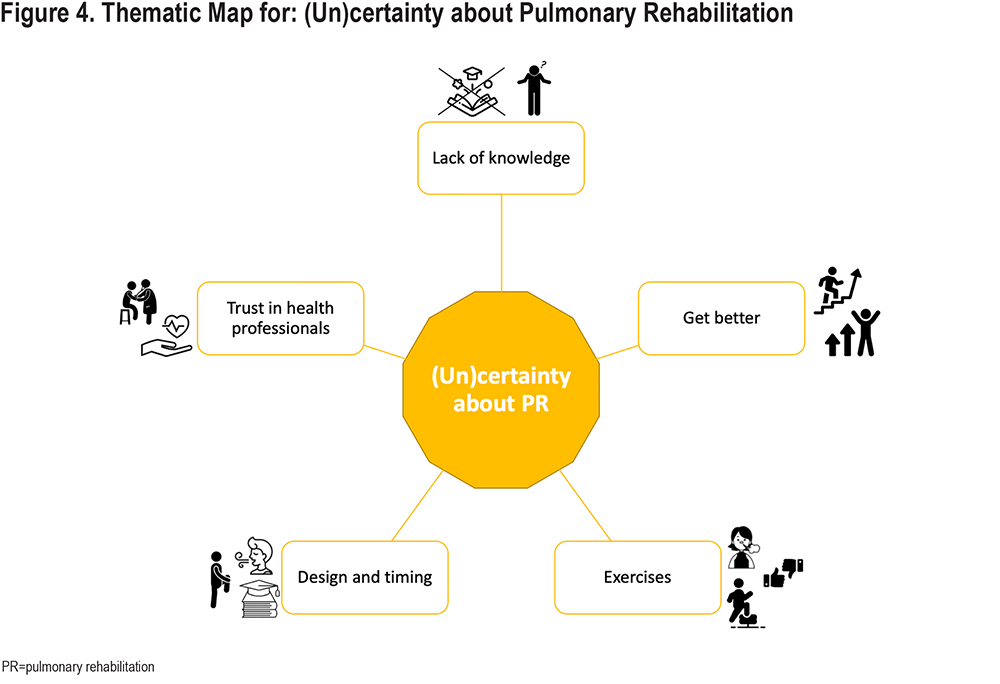
Lack of knowledge about PR was perceived by both participants with previous PR contact and those individuals naive to PR, who also felt the need of experiencing PR before sharing their thoughts:
“Oh, that I don’t know, only at the end I will be able to tell you.” (Harry, 87)
Independently of their level of knowledge, individuals with AECOPDs who had previous contact with PR believed it would be beneficial to them.
“I think it will be positive. Yes, I think I will get a bit better.” (Thomas, 56)
Conflicting ideas regarding exercises emerged, with 1 participant who was naive to PR feeling that both exercise training and breathing exercises could make her worse, while the others (with or without previous PR contact) mentioned exercises as something positive or even fundamental for their recovery.
“I think that, in the situation that I am in, due to the muscle mass or to what my body already asks for, the weakness, the oxygen, walking can help. I feel the walk training helps.” (Ethan, 58)
Several ideas regarding the design and timing of PR were reported. Individuals with AECOPDs with previous PR contact mentioned the importance of breathing techniques, individualization, and education, namely about how to breathe. Opinions regarding exercise training were divided between less intense exercises with a shorter duration, or something similar to a stability program. One participant felt that it would be better to wait a few days to relieve symptoms before starting PR.
“Less intense exercises, without weights, or as long as it is not too heavy and it is not for too long, I don't know. Less exercise time and lighter weights.” (Peter, 64)
On the other hand, individuals naive to PR highlighted the relevance of exercises and education on how to breathe and manage symptoms.
“It would be important to learn how to manage symptoms.” (Oliver, 63)
Lastly, high levels of trust for health professionals were reported but only by those who had already experienced PR.
“But you do everything ... I know that you do everything to make me get better.” (John, 75)
Discussion
This study identified individuals’ experiences during mild to moderate AECOPDs, namely the exacerbation’s impact and strategies to deal with it, main needs, and thoughts on PR during this period. To the authors’ best knowledge, this is the first study exploring the perceptions of individuals with mild to moderate AECOPDs, conducted at the onset of an exacerbation.
AECOPDs have a negative impact on people’s lives. Symptoms are the main concern at the onset of an AECOPD, but the variety of symptoms (e.g., cough, wheezing, lack of energy) reported by our participants was broader than previously described,14,20,41-43 emphasizing the heterogeneity of exacerbations’ clinical presentation and the need for a comprehensive symptoms’ assessment. Limitations performing activities of daily living affect different dimensions than those reported by people with severe AECOPDs,42 with impacts also occurring on the advanced activities (e.g., work). Surprisingly, people with AECOPDs noticed physiological changes, namely that they lacked oxygen in their brain with a negative impact on their mental abilities, which has not been reported in previous qualitative literature.
AECOPDs further impacted individuals on a social, psychological, emotional, and family level. Our study reinforces findings from existing literature,14,20 and adds that people with mild to moderate AECOPDs also feel ashamed of having symptoms in front of others, have little desire to do things, are not able to keep up with their peers, and have their self-sufficiency affected. This psychological burden leads to low functional performance and health-related quality of life, 44,45 and is often neglected.14,46
To deal with AECOPDs, people usually reduce their daily activities and/or perform them slower or after some breaks, planning and adjusting based on how they feel. Yet, some people just spend most of their day laying down or sitting on the couch barely moving.14,20,41 Since physical activity is the best predictor of mortality in this population,47 breaking this dyspnea-inactivity vicious circle48 must be a goal of treatment strategies. Moreover, during AECOPDs people demand additional support to perform their tasks,14 but there is a dichotomy between the individuals who rely on their network for help and the individuals who do not want to be dependent, highlighting the need to provide formal support to these people and their families.49,50
In line with previous literature,20,42 the main needs reported during AECOPDs were to breathe better, to feel less tired, to get rid of sputum, and to be able to walk. Health professionals must therefore tailor interventions for this population to comply with these needs, namely by conducting PR programs that include not only exercise, education, and psychosocial support, but also breathing techniques.26
Both individuals with AECOPDs naive to PR and with previous PR contact (stable disease) reported a lack of knowledge on how PR should be delivered during an AECOPD. This highlights the need to raise awareness for PR and educate the population about what it is and its benefits,27 and suggests that education on PR might enhance participation. Similarly, to previous findings, in different severities of AECOPDs and treatment settings, 27,28 most participants considered it important to have an individualized program, including exercise training, breathing techniques, and education. There was some uncertainty regarding the timing and intensity of the program.
In summary, we found that mild to moderate AECOPDs have a negative impact on several aspects of people’s lives and share some similarities with reports from those individuals hospitalized with a severe AECOPD, emphasizing the importance of also providing proper interventions to manage mild to moderate AECOPDs.51 The multitude of impacts and needs reported during the AECOPD require a comprehensive assessment, which would allow for the identification of the treatable traits to be addressed during a personalized PR program.52,53 Previous literature has shown that PR is a safe intervention for the management of AECOPDs that targets several of these treatable traits, namely, physical activity, exercise capacity, muscle weakness, dyspnea, and emotional burden.23,26,54,55 To address the complexity of individuals with AECOPDs, an interdisciplinary team composed of physicians, physiotherapists, respiratory therapists, nurses, psychologists, behavioral specialists, occupational therapists, social workers, and a care coordinator seems to be necessary.28,56-58
Methodological Considerations
This study has several strengths and limitations that need to be acknowledged. The performance of the interviews at the onset of the exacerbation prevented a potential memory bias related to the recall of the experience. Additionally, the most well-established guideline for reporting qualitative research (COREQ) was followed. Our main limitation was the short duration of the interviews, which might have affected the depth of the gathered information and was probably related to the acute phase59 individuals were experiencing, and the tiredness they felt.60 The sample included was small, but consistent with qualitative studies41,61,62 and a maximum variation sampling (e.g., gender, severity of the AECOPD, occupation, marital status) was used to ensure the representativeness of the population. Finally, as the interviews were conducted in Portuguese, the translation process might have influenced the findings, particularly regarding the use of colloquial expressions or proverbs. However, we believe the main themes and conclusions are not affected by the translation process.
Conclusion
Mild to moderate AECOPDs have a negative impact on individuals’ lives, even though no hospital admission is required. Symptoms were reported as the main concern, thus interventions focusing on symptomatic relief are needed. Further physical, functional, psychological, emotional, social, and family level impacts were noted, highlighting the importance of comprehensive assessments and interdisciplinary PR programs. Individuals with AECOPDs considered PR beneficial but lacked knowledge about the intervention, highlighting the need to raise awareness for PR within this population. This study contributes with a foundation for the development of tailored and meaningful person-centered interventions during AECOPDs.
Acknowledgments
Author contributions: All authors contributed to the conceptualization and/or design of the study. AM performed data collection. AM and SA performed the formal data analysis and all authors contributed to data interpretation. AM wrote the first draft of the manuscript, and all authors provided critical review of the manuscript and approved the final revision.
The authors would like to acknowledge the support from the clinicians at Unidade Local de Saúde de Matosinhos and Centro Hospitalar do Baixo Vouga in recruiting participants to this study. We are also grateful to all the individuals with COPD who agreed to participate in this study.
Declaration of Interest
The authors have no conflicts of interest to declare.