Running Head: Rurality and Poverty Effect on COPD Outcomes
Funding: No outside funding sources to report.
Date of Acceptance: July 22, 2022 │Published Online Date: July 29, 2022
Abbreviations: chronic obstructive pulmonary disease, COPD; New Hampshire, NH; length of stay, LOS; confidence interval, CI; Department of Health and Human Services, DHHS; Federal Information Processing Standard, FIPS; emergency department, ED; American Community Survey, ACS
Citation: Warner JS, Bryan JM, Paulin LM. The effect of rurality and poverty on COPD outcomes in New Hampshire: an analysis of statewide hospital discharge data. Chronic Obstr Pulm Dis. 2022; 9(4): 500-509. doi: http://doi.org/10.15326/jcopdf.2022.0299
Introduction
Health disparities are known to exist between rural and non-rural areas, particularly with concern to chronic diseases.1-5 Chronic obstructive pulmonary disease (COPD) is a leading cause of death in the United States,6 and individuals living in rural areas experience worse COPD outcomes.7,8 Rural residence is an independent risk factor for COPD, even among never-smokers,9 with a COPD prevalence in rural areas that is nearly double that of the overall population.9-11 Rural residents with existing COPD face increased exacerbations1,10 and respiratory-related deaths.7,12,13 Although smoking is the leading independent risk factor for COPD,4,12 accounting for smoking does not completely explain the variation between rural and non-rural areas. Additional risk factors, including poverty and wood fuel for heating, are more common in rural areas and have been shown to be associated with increased disease incidence and worse outcomes.14-17 Continued identification of patient and community level factors that are associated with worse COPD outcomes in rural areas is a research priority.1
In addition to the emerging research into disparities in rural health, prior work has suggested variation in health care availability and expenditures by geographic location throughout the United States.18,19 It has been shown that in areas with more health care resources there is a significant increase in health care expenditure whereas there is no significant mortality benefit when compared to non-resourced areas.19 This is especially true for non-surgical cases and chronic medical conditions, including COPD.20 Limited research has been done comparing rural and non-rural areas within the same administrative region such as a state.
As an individual state, New Hampshire (NH) has a large separation between high resource population centers in non-rural areas and the more rural areas served by smaller medical centers. We aim to determine the association of rurality with COPD outcomes, including COPD exacerbation rate, length of stay (LOS), and total charges, accounting for important individual and community-level factors. To do so, we obtained hospital encounter data from the NH Department of Health and Human Services (DHHS) for all NH hospital-based COPD encounters from 2016-2017. These data were linked to publicly available county-level sociodemographic data to quantify differences in COPD exacerbations and expenditures between rural and non-rural counties.
Methods
Data Sources
Hospital discharge data were obtained via request from the Bureau of Public Health Statistics and Informatics of the NH DHHS21 for the years of 2016-2017. The data supplied consisted of all patient encounters pertaining to COPD exacerbations at all hospitals located in the state. This was defined as any individuals who carried a principal visit diagnosis with an International Classification of Diseases, Revision 10 code of J40-44. Individual encounters included the Federal Information Processing Standard (FIPS) code for the residence of the patient and the FIPS code of the hospital where the encounter occurred. The primary analysis included the FIPS code of the county of residence. The study was approved by the Dartmouth-Hitchcock Institutional Review Board.
COPD Exacerbation Rate
To increase certainty of COPD endpoints, given that COPD rarely develops in young adults,22,23 and to match the census level age variable range, we included all encounters over the age of 35. We defined the COPD exacerbation rate as:
COPD Exacerbation Rate by County=[(Number of COPD Encounters)/ (County Population over 35)] X 100
This data was further filtered by encounter status as an inpatient or an emergency department (ED) visit with no admission.
Encounter Level Variables
Each encounter had associated with it the age, gender, and insurance status of the patient (Medicare, Medicaid, commercial, other [worker’s compensation and Tricare], or none [no insurance or self-pay]). Number of beds per hospital was included as a corollary for hospital size. Each encounter included data on total charges and LOS (for inpatient admissions).
County Level Variables
Encounter level data was linked to county-level population data from the U.S. Census Bureau’s 2016-2017 American Community Survey (ACS) 5-Year Database. Due to variation year to year, these variables were averaged over the 2 years. The 2013 National Center for Health Statistics Urban-Rural Classification of Counties was used to classify the rurality of the counties based on patient residence.24 This schema denotes counties as belonging to 6 categories, from most non-rural to most rural, as listed: (1) large metro central, (2) large metro fringe, (3) medium metro, (4) small metro, (5) micropolitan, and( 6) non-core. New Hampshire does not contain large metro central or small metro counties. In general, large fringe metro and medium metro are considered “non-rural” while micropolitan and non-core counties are considered “rural.” Census level poverty data was obtained, and poverty status was defined as above/below the 75th percentile of mean county-level poverty.
In addition to poverty levels, we used other census level exposures associated by county of residence that may relate to COPD prevalence and exacerbation rates. These exposures include the percentage of the adult population that did not achieve at least a high school diploma or equivalent and the percentage of households using wood fuel as a primary heat source. Smoking prevalence data for the year of 2015 was obtained from the NH WISDOM database of state-wide health metrics.25
Statistical Analysis
Differences in COPD exacerbation rate, LOS, and total charges by non-rural/rural status were determined by analysis of variance and the Kruskal-Wallis test, as appropriate. A multivariable logistic regression model was used to evaluate the association of degree of rurality (reference category large fringe metro) on COPD outcomes, adjusting for age, gender, insurance status, county-level smoking prevalence, and county level poverty. In a sensitivity analysis, given the association between indoor air pollution and COPD risk,2,3 the county-level percentage of households using wood fuels was added as an additional covariate in the models predicting COPD exacerbation rate. Further, in a separate analysis, hospital bed size was added as a covariate to the models predicting LOS and total charges. All analyses were performed using Stata 15.1 (StataCorp LLC, College Station, Texas). Statistical significance was defined as a p-value of less than 0.05.
Results
Population Characteristics
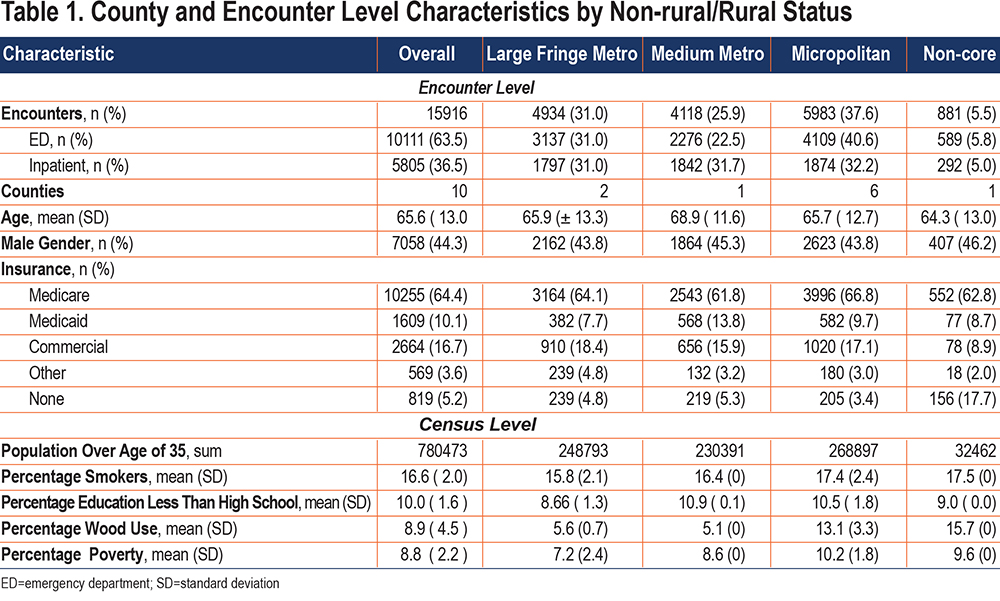
In total, 15,916 hospital encounters were analyzed for the years of 2016 and 2017. The mean age was 65.6 years; 44.3% of all the cases were males. The majority were covered by Medicare (64.4%), followed by commercial insurance (16.7%), Medicaid (10.1%), and individuals having no insurance (5.1%), with the least number of individuals having other forms of insurance (3.6%). Nearly a tenth (9.9%) of the population had less than a high school education (or equivalent). A total of 16.6% of the population smoked tobacco, 8.8% had income below the state 75th percentile, and 8.9% of homes were heated by use of wood. A total of 13,900 (87%) of the encounters involved a patient from the same county as the hospital at which they were treated.
There are 10 counties in NH, 2 of which are considered large fringe metro, 1 is a medium metro, 6 are micropolitan, and 1 is non-core. Overall, prevalence of wood use for heating was more common in rural counties (micropolitan 13.1%; non-core 15.7%) compared to large fringe metro (5.6%) and medium metro (5.1%) counties. Smoking prevalence was also higher in micropolitan (17.4%) and non-core (17.5%) counties compared to large fringe metro (15.8%) and medium metro (16.4%) counties. Finally, poverty was greater in micropolitan (10.2%) and non-core (9.6%) counties compared to large fringe metro (7.2%) and medium metro (8.6%) counties. All areas were similar for age, gender, and educational attainment. In general, the proportions of insurance coverage were similar between the 4 categories, with the greatest difference being lack of insurance in non-core locations (17.7%) compared to large fringe metro (4.8%), medium metro (5.3%), and micropolitan (3.4%) counties (Table 1).
Association of Rural/Non-rural Status with COPD Outcomes
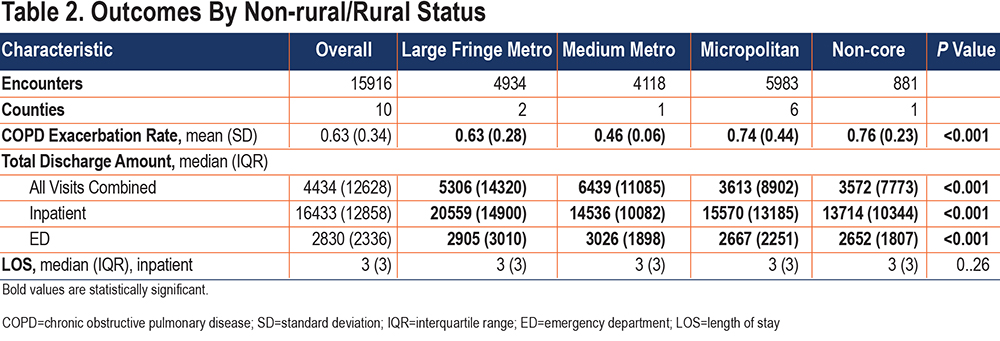
COPD Exacerbation Rate: COPD exacerbation rate was greater in non-core (0.76) and micropolitan (0.74) counties than it was in medium metro (0.46) and large fringe metro (0.63) (p<0.001) counties (Table 2). In unadjusted analysis, more rural counties of residence were associated with higher rates of COPD exacerbations. When accounting for age, gender, insurance type, county smoking prevalence, and county level poverty, with large fringe metro as the referent, non-core (beta=0.18, [confidence interval (CI) 0.16, 0.20]) and micropolitan (beta=0.02, CI [0.01, 0.03]) counties had higher rates of exacerbations, whereas medium metro (beta=-0.07, Cl [-0.09, -0.06]) counties had lower rates of COPD exacerbations (Table 3).
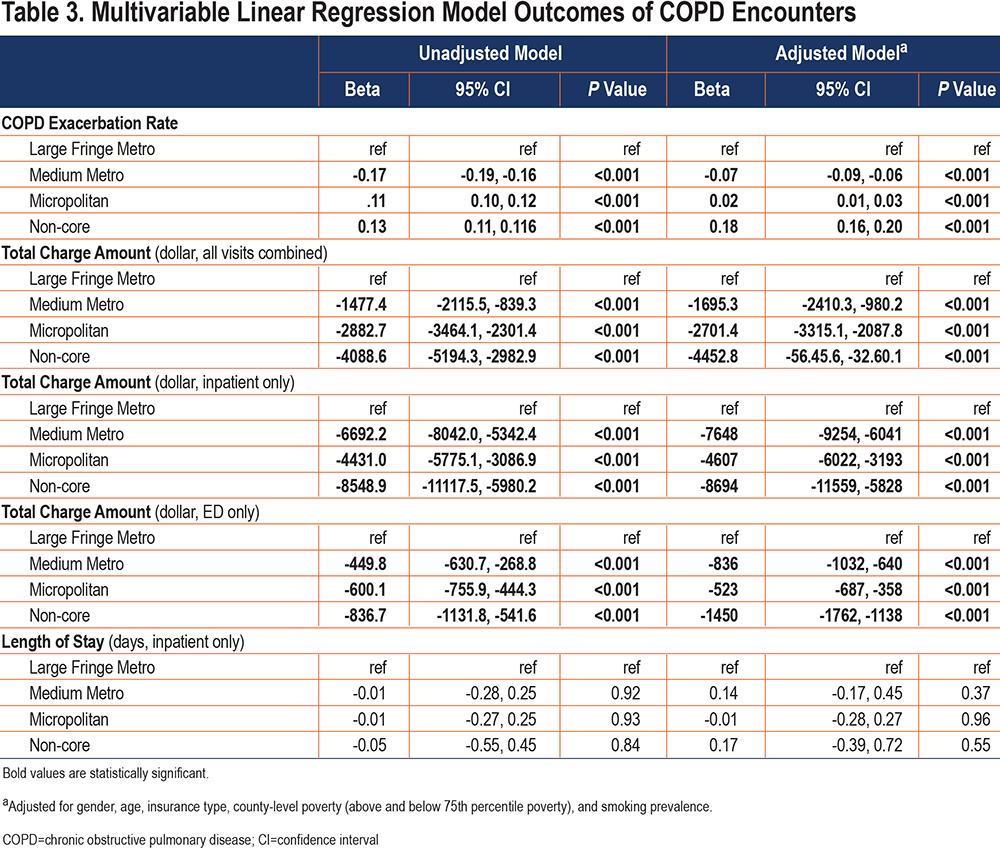
In a sensitivity analysis including county-level wood fuel use in the model, the relationship between medium metro counties and COPD exacerbation rate did not meaningfully change (beta=-0.08, CI [-0.09, -0.06]). The relationship between micropolitan counties and COPD exacerbation rate somewhat differed (beta=-0.03, CI [-0.05, 0.01]), and was slightly attenuated in the most rural counties (non-core beta=0.11, CI [0.08, 0.14]).
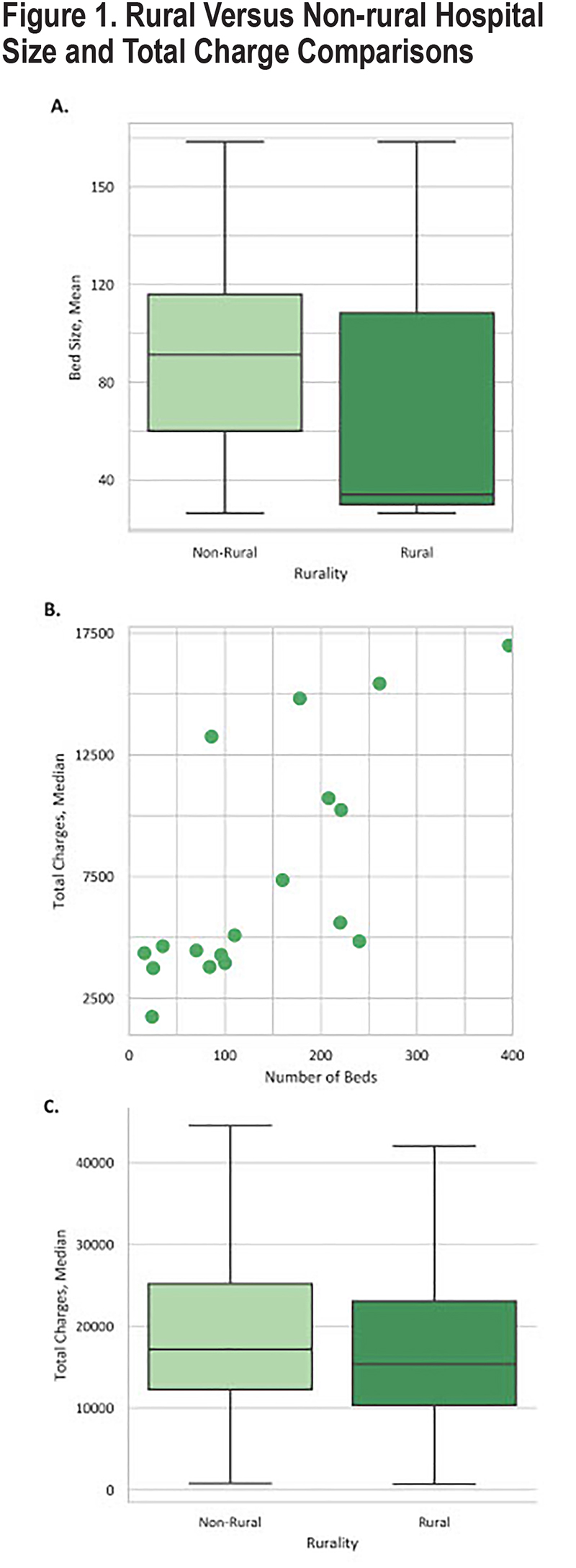
Length of Stay and Total Charges: Median LOS was 3 days for all counties and not statistically different (p=0.26) (Table 2). The average rural (micropolitan and non-core) hospital size was 99.7 beds whereas non-rural (large fringe metro and medium metro) hospitals averaged 167.7 beds (Figure 1A). An increase in expenditure per encounter was seen in relation to increasing bed size of the hospital (Figure 1B). When comparing total amount charged per patient at discharge from an inpatient encounter, the median amounts for rural and non-rural counties were $15,363 and $17,154, respectively (p<0.001) (Figure 1C).
LOS did not differ significantly by county rural status in the unadjusted or the adjusted model. Total amount charged for the encounter using the unadjusted model with large fringe metro as a reference showed that less metropolitan areas had lower total charges for all visits—inpatient and ED visits. When adjusted for age, insurance type, gender, county level smoking prevalence, and county poverty level, this relationship remained, such that total charges for all visits combined (medium metro beta=-1695 [-2410, -980], micropolitan beta=-2701 [-3315, -2088], non-core beta=-4453 [-5646, -3260]), ED visits (medium metro beta=-836 [-1032, -640], micropolitan beta=-523 [-687, -358], non-core beta=-1450 [-1762, -1138]) and inpatient visits (medium metro beta=-7648 [-9254, -6041], micropolitan beta=-4607 [-6022, -3193], non-core beta=-8694 [-11,559, -5828]) were all lower in more rural counties of residence compared to large fringe metro counties (p< 0.001 for all) (Table 3).
In the sensitivity analysis including hospital bed size as a covariate, the relationship between rural status and LOS remained non-significant. For all visits combined, large fringe metro counties once again had the greatest charges, although the magnitude of the effect size within each category differed (medium metro beta=-4055 CI [-4779, -331]; micropolitan beta=-1969, CI [-2573, -1365]; non-core beta=-1511 CI [-2702, -320]). For inpatient encounters only, the relationship between rurality and charges remained similar (medium metro beta=-10,784 CI [-12,416, -9153]; micropolitan beta=-4988 CI [-6378, -3598]; non-core beta=-5757 CI [-8597, -2916]). Similarly, the relationship between rurality and ED charges did not meaningfully change (medium metro beta=-907 CI [-1109, -705]; micropolitan beta=-484 CI [-651, -318]; non-core beta=-1348 CI [-1668, -1028]).
When the dataset was limited to patients who were treated at a hospital that was within the same county as the individual’s residence, there was no meaningful change in the relationship between rurality and COPD exacerbation rate, total charges, or LOS (data not shown).
Discussion
The results from our study show that there is a clear association with increased rates of COPD exacerbations in counties that are more rural. These relationships persisted even when accounting for county-level poverty and smoking, supporting evidence that rural status itself is a potent predictor of worse COPD outcomes. Moreover, we also found that encounters in rural counties tended to have lower charges associated with them, raising the question of distribution of resources and allocation of care among rural and non-rural counties.
Prior research has exhibited the relationship between rurality and COPD,1,7,9-12 a relationship that often persists despite careful adjustment of individual and community level factors that are associated with increased COPD risk and morbidity. The effects of factors typically attributed with rural living, including sociodemographic differences such as poverty, did not fully explain the observed differences.5 Although our study did not account for mortality, prior research in the Veterans Affairs database has shown that while rurality does not affect in-hospital mortality,26 it may be an independent risk factor in 30-day mortality post-discharge,27 suggesting that factors in the post-discharge rural environment may impact long-term outcomes. Our data reinforces this, as we found that rural counties had greater COPD exacerbation rates, even when accounting for county-level poverty and smoking. Additionally, while wood fuel use explained some of the relationship between geographic location and COPD exacerbation rates, it did not completely explain the higher burden in the most rural counties, highlighting the role of rurality as an independent predictor of COPD exacerbation rates.
Similar to prior studies showing that non-rural areas tend to have higher charges for treatment of chronic conditions when compared to rural areas,19,20,28 our study also showed that decreased rurality was associated with a higher cost per COPD encounter. This difference did not seem to reflect itself in the breakdown by insurance, as both rural and non-rural counties had similar levels of Medicare, Medicaid, and commercial insurances in this dataset. Interestingly, this difference in charges was seen despite no difference in the median LOS. Further, inclusion of hospital bed size as a covariate in the sensitivity analysis did not completely explain the observed differences in charges by rurality. While larger hospitals generally have greater resources and tools than smaller, critical access hospitals,29 recent research has suggested that bed size alone is not a comprehensive measure of overall hospital resources.30 Other characteristics that were not captured in our analyses, including imaging modalities, advanced procedures, consultants, etc., may explain some of these differences.
Our work supports other studies that have shown that COPD exacerbations can cost from $340 in the outpatient setting up to a mean of $27,597 per inpatient visit.31,32 This wide spread between inpatient and outpatient cost is similar to our data. Our results are similar to prior disease-specific work looking at geographic variations in total charges. In an analysis of costs related to spine treatment, Cher et al33 found that increased spending was driven by inpatient costs versus outpatient, consistent with what our data shows. Other work has shown that the higher the capacity of a regional health system, there are more tests, imaging, and specialists seen, increasing the health care spending per patient.19,34 When accounting for solely ED encounters, there was still a significant difference in charges, however, the differences were not as pronounced. This implies that supply-sensitive care may apply primarily to inpatient settings as there is less opportunity to use these resources in outpatient and ED settings.
Our study had several limitations. One limitation was that each encounter could only be ascribed to a county instead of a more granular level such as zip code or census tract. By assigning a single value to each county, we are unable to capture variability of demographics and outcomes between locations within counties. Another limitation is that the hospital data did not reliably indicate if the patient was a smoker or not; smoking prevalence had to be obtained at a county level from the NH DHHS database. Similarly, variables such as wood use, poverty, and education were census level variables based on the county, not the individual encounter. Furthermore, the total charges do not capture the true reimbursement that the hospital received or the actual cost the patient paid. Another limitation was that the diagnosis of COPD in these encounters was not confirmed with spirometry. Physician diagnosis of COPD has been shown to be unreliable, particularly in the outpatient setting.35 Finally, while each encounter was identified by a unique ID, individual patients were not, so it is possible 1 patient may have represented more than 1 encounter.
Strengths of this study include use of the NH DHHS database that included over 15,000 encounters. Since each encounter involved the FIPS code of the patient, this, in conjunction with the ACS, allowed us to evaluate individual and population level characteristics. Additionally, encounter level data at the hospital of treatment allowed for evaluation of different characteristics based on hospital size and location. Although this study focused on a single state, many states in the United States have a similar spread of rural and non-rural counties, and thus, these findings may be applicable to other states besides New Hampshire.
Our study showed that COPD exacerbation rates were higher in rural counties of the state of New Hampshire, independent of smoking prevalence or overall poverty of the county. It also showed that a higher health care financial burden may be placed on the individuals served by a larger hospital system, regardless of LOS. Further research can explore what exact risk factors beyond poverty, smoking, and increased wood fuel use are unique to rural areas and predispose to a higher COPD exacerbation rate. Additional insight into whether higher total charges in non-rural areas are justified by improved quality of life and disease management pertaining to COPD would be of value.
Acknowledgements
Author contributions: JSW formulated the dataset and collated Census data. Both JSW and JMB conducted literature review. Both JSW and LMP analyzed and interpreted the data. JSW wrote the first draft. JSW, JMB and LMP edited, revised and finalized final draft of the manuscript.
Declaration of Interest
The authors have nothing to declare.