Running Head: COPD and Health Care Professionals’ HZ Vaccine Awareness
Funding Support: This study was funded by GlaxoSmithKline Biologicals SA through the Investigator-Sponsored Studies program. The investigators are responsible for all content. The sponsor reviewed the study design but had no role in the collection, analysis, or interpretation of the data, or manuscript preparation. GlaxoSmithKline Biologicals SA was provided the opportunity to review a preliminary version of this manuscript for factual accuracy. The only change requested was to update the name of the GSK funding program.
Date of Acceptance: September 28, 2022 | Published Online Date: September 30, 2022
Abbreviations: health care professionals, HCPs; herpes zoster, HZ; chronic obstructive pulmonary disease, COPD; Advisory Committee on Immunization Practices, ACIP; family physicians, FPs; nurse practitioners, NPs; physician assistants, PAs; Global initiative for chronic Obstructive Lung Disease, GOLD; Shingles Patient Prevention Study, ShiPPS; American Academy of Family Physicians, AAFP; National Research Network, NRN; American College of Chest Physicians, CHEST; American Academy of Physicians Assistants, AAPA; male, M; chronic bronchitis, CB; short-acting beta2-agonist, SABA; female, F; inhaled corticosteroid, ICS; long-acting beta2-agonist, LABA; long-acting muscarinic antagonist, LAMA; history, hx
Citation: Yawn BP, Loskutova NY, Merrill DD, et al. Health care professionals’ herpes zoster awareness and vaccine recommendations for patients with COPD. Chronic Obstr Pulm Dis. 2022; 9(4): 562-575. doi: http://doi.org/10.15326/jcopdf.2022.0322
Online Supplemental Material: Read Online Supplemental Material (428KB)
Introduction
Adults with chronic obstructive pulmonary disease (COPD) are at increased risk of acquiring vaccine-preventable diseases, including a 31% to 416% age-adjusted increased risk to the 1 in 3 lifetime risk of acquiring shingles or herpes zoster (HZ).1-6 In addition, people with COPD may experience greater HZ severity and more complications.5,7-10 HZ risk and increased burden could be lowered by appropriate HZ vaccination10-16 in those living with COPD. The importance of reducing the HZ burden in those living with COPD has been acknowledged by 2 groups since the development and fielding of this survey study. First, the Advisory Committee on Immunization Practices (ACIP) expanded its preferential recommendation of offering the 2-dose HZ vaccine to individuals aged 50 years and older.11 Beginning in March 2022, the ACIP recommendation was amended to offering the 2-dose HZ vaccine to individuals aged 19 years and older with conditions that increase their HZ risk including COPD.12 In addition, the Global initiative for chronic Obstructive Lung Disease (GOLD) 2022 update recommends giving “Zoster (shingles) vaccination for those with stable COPD.”13
Despite evidence for high HZ vaccine efficacy and cost effectiveness, vaccine uptake, including in people with COPD, lags behind that for other common adult vaccines.17-19 Immunization rates for people with COPD from recent National Health Interview Surveys show a lag for HZ vaccines (40.4%) compared to 64.6% for annual influenza and 85.5% for any pneumococcal vaccine.20,21 Strong HZ vaccine recommendations by health care professionals (HCPs) might shorten that lag.22
Studies have reported several HCP barriers to improving vaccine uptake.23-35 HZ vaccines may have additional barriers such as payments by Medicare Part D, incomplete awareness of HZ risk in patients with COPD, or general awareness of current recommendations for HZ vaccine use. To date, publications related to HCPs’ knowledge and recommendations for the HZ vaccine focus on the general population of patients, not only those with COPD, and on primary care physicians and pharmacists, with little information published regarding pulmonologists, nurse practitioners (NPs), and physician assistants (PAs) despite their significant roles in caring for patients with COPD.27,28,33 We report on the HCPs’ portion of the Shingles Patient Prevention Study (ShiPPS), a companion to the ShiPPS patient survey.36 The goal was to identify gaps and opportunities to increase HZ vaccine knowledge and recommendations focusing on patients with COPD among HCPs caring for people with COPD, using influenza and pneumococcal vaccinations for comparison. We also assessed the ability of a short educational video to increase awareness and modify future HZ vaccine recommendation intent.
Methods
Study Overview
This 2-part cross-sectional survey included an embedded educational video and was identical for all 4 groups of HCPs: family physicians (FPs), pulmonologists, NPs, and PAs. Part 1 aimed to understand knowledge and practice-related HZ vaccine recommendations, and perceived burden of HZ for patients with COPD. Part 2 was offered to the subset of Part 1 respondents who reported they were unaware that COPD increases HZ risk, or that 50 years is the minimum age for routine HZ vaccination, or who did not follow ACIP recommendations regarding HZ vaccines in their responses. Part 2 questions addressed the usefulness of the video and future HZ vaccine recommendation intent.
The study was conducted in the United States between August 31, 2020, and December 31, 2020, and approved by the Western Institutional Review Board (Puyallup, Washington, IRB Tracking Number:20141136) and the American Academy of Family Physicians (AAFP) IRB. Consent was considered implied if a participant chose to complete the survey.
Sample, Setting, and Participant Recruitment
Family Physicians: A total of 229 FPs responded throughcollaboration with the AAFP’s National Research Network (NRN) via email on the Qualtrics platform. Invitees included 2 groups: the 1946 investigators/members of the NRN, an unknown number of which were FPs, and all 1000 FP members of the AAFP’s Marketing Insight Exchange group, a voluntary subset of the overall AAFP membership. Online participation invitations were sent December 4, 2020, with 1 reminder. Survey respondents received a $10 “cup of coffee” gift card.
Pulmonologists: A total of 258 pulmonologists responded through collaboration with the American College of Chest Physicians (CHEST) via email using the Survey Gizmo platform and the 438 members of the COPD Foundation (COPDF) PRAXIS network of HCPs, an unknown number of which were pulmonologists. Invitations from CHEST were sent in 5 batches of 1000 randomly selected pulmonologists from the CHEST membership beginning November 12, 2020. Invitations from the COPDF for PRAXIS were sent from the Foundation’s DATSTAT platform. Reminders for both groups occurred on days 3, 7, and 14. Respondents received a $50 electronic gift card.
Nurse Practitioners: A total of 250 NPs responded through collaboration with the American Association of Nurse Practitioners’ NPInfluence program (N=3131 NPs working in primary care or pulmonology) via email using Qualtrics. Invitations were sent to a random sample of 1524 NPs August 31, 2020, with day 3, 7, and 14 reminders. Respondents received a $20 electronic gift card.
Physician Assistants: A total of 283 PAs responded through collaboration with the American Academy of Physician Assistants (AAPA) via email using the COPDF DatStat Platform. Invitations were sent to a random sample of 376 PAs working in pulmonology, geriatric, and/or primary care settings selected from the overall AAPA membership beginning October 5, 2020, with day 3, 7, and 14 reminders until the response goal of 250 PAs was reached (and exceeded). Ten respondents were randomly chosen to receive a $25 electronic gift card.
The payment amounts to the HCP groups were based on the standards and recommendations of each collaborating HCP group.
Survey and Video
The goals of the HCP survey were 2-fold: (1) to better understand HCPs’ knowledge and current vaccine recommendations related to HZ among patients diagnosed with COPD and compare their reported HZ recommendation timing and strength to recommendations for influenza and pneumococcal vaccines, and (2) in a subset of HCPs, to assess changes in HCPs’ HZ risk awareness and future HZ vaccine recommendation intent after viewing a short educational video. The Part 2 invitee criteria are presented in the study overview.
Questions in Part 1 were developed specifically for this study by a team of experienced survey researchers with expertise in family medicine, pharmacy, and COPD using an iterative process and based on previously reported survey items related to HZ risk and burden and potential barriers to recommendations for all adult vaccines by HCPs for the general patient population.22-33 Those items queried HCPs’ personal demographics and overall beliefs regarding HZ burden. No surveys could be found in the literature that pertained specifically to adult vaccine recommendations in patients with COPD. The authors developed 6 short case-based scenarios to query about minimal age for HZ vaccination, as well as recommendations for those with prior HZ or prior HZ vaccination as well as the strength of HZ, influenza, and pneumococcal vaccinations recommendations among their patients with COPD. The 6 brief cases were designed to assess knowledge and vaccine recommendations in areas that changed with the 2018 Food and Drug Administration approval and ACIP recommendations related to the introduction of the second HZ vaccine. Specifically, HZ vaccine recommendations for patients with COPD in their 50s, patients with prior HZ or prior live attenuated HZ vaccine receipt, and patients with prior immunosuppressive treatment or who use inhaled corticosteroids. Questions were reviewed by the authors and outside consultants in pulmonology, infectious disease, pharmacy, and epidemiology. (Full survey in the online supplement.)
After watching the 5-minute video including HZ pathophysiology, epidemiology, complications, and available vaccine prevention with a short COPD patient testimonial, Part 2 respondents were asked about their perceived value of the video regarding HZ and HZ vaccine knowledge as well as future HZ vaccine recommendation intent. The 5-minute online educational video was developed by one of the authors (BPY) based on prior HZ HCPs’ educational presentations and addressed the general content of the survey including HZ epidemiology, burden, risk factors, and prevention opportunities. The script for the video was reviewed by academic infectious disease and epidemiology experts in HZ with resulting edits prior to being recorded. The video is available to view online.
Statistical Analyses
Results were provided to the study statistician in raw data Excel or SPSS format from each of the collaborating organizations who fielded the surveys. Responses to both parts of the survey (before and after the educational video) were analyzed using descriptive statistics including frequencies and means, and, as applicable, Student’s t-tests (or Welch’s t-tests) for simple comparisons, analysis of variance , or χ2 tests. Participants with missing or incomplete data were excluded from the analyses of those questions with missing data. All analyses were conducted by the study statistician using IBM SPSS, Version 25.0 (IBM Corp., Armonk, New York ).
Results
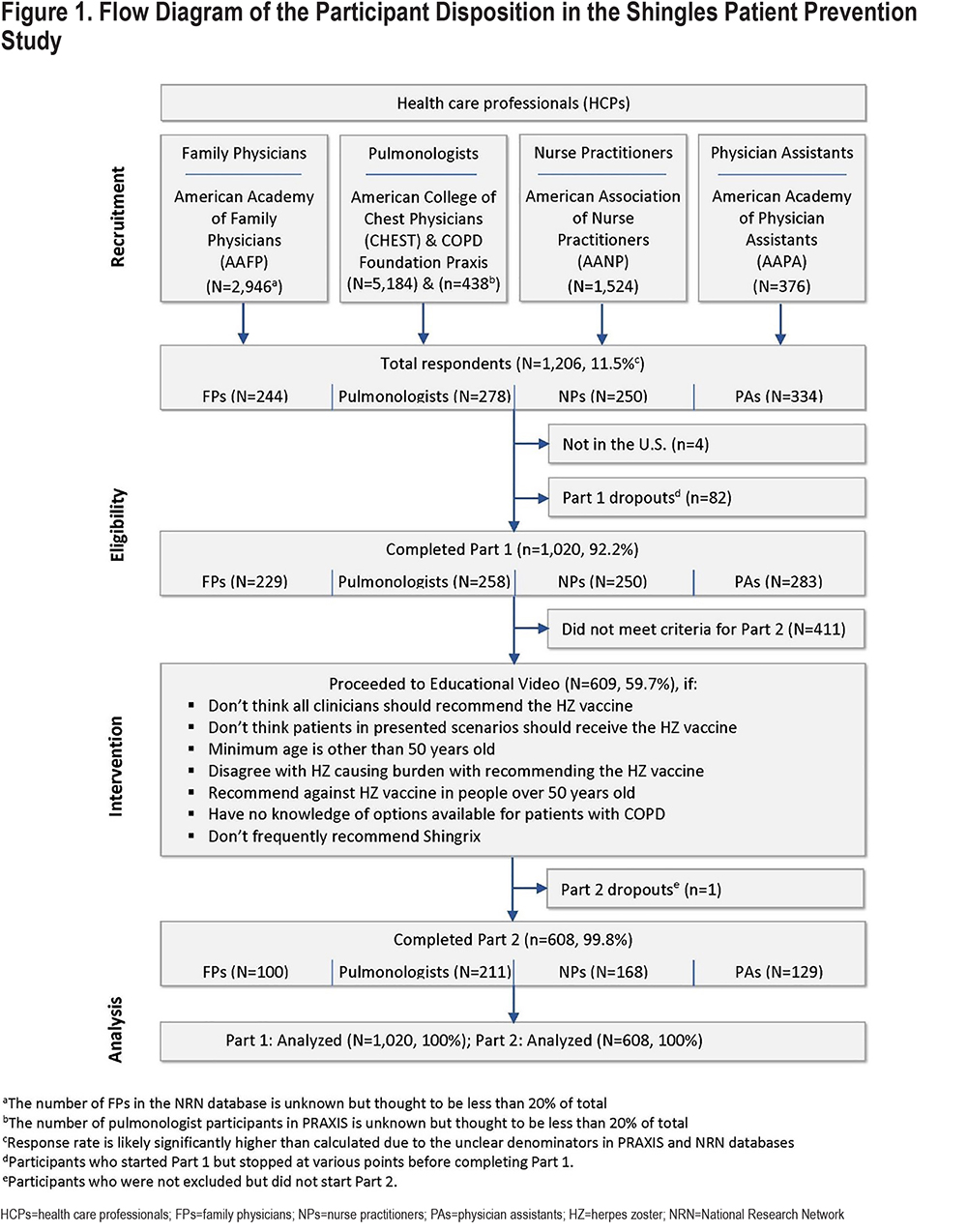
Overall, 1020 HCPs (229 FPs, 258 pulmonologists, 250 NPs, and 283 PAs) completed Part 1 and were included in the analyses (Figure 1). NPs and PAs were more likely than the physician respondents to be women (P<0.001) and to have fewer years of work experience (p<.001). More than 75% of each HCP group spent >75% of their time in clinical practice (Table 1).
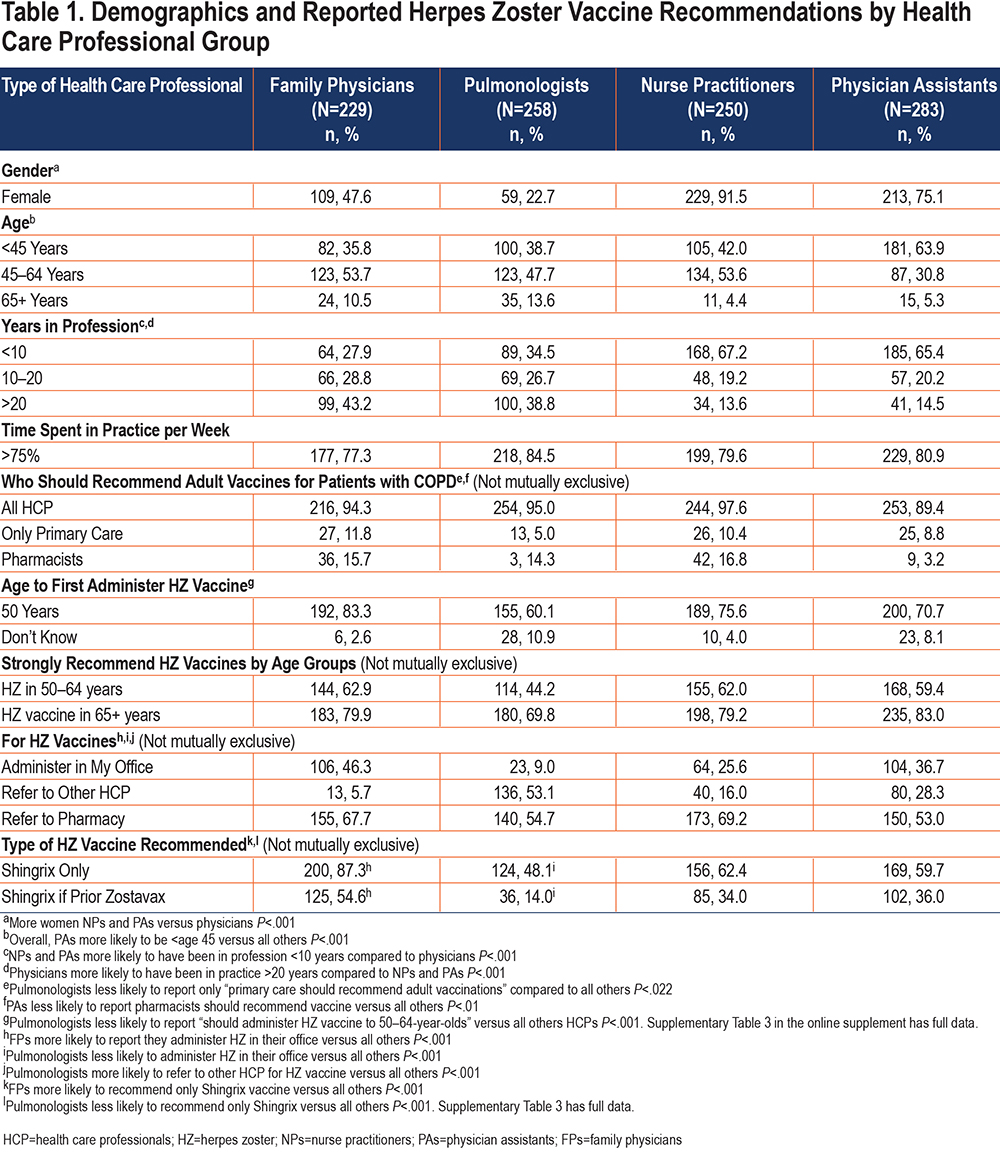
While most respondents (967, 94.8%) reported that all HCPs should recommend vaccines for their patients with COPD (with no difference by group), reports of specific vaccine recommendations varied by HCP group. Over 95% of all HCPs reported they strongly recommend influenza vaccination for all ages. Strong recommendations for pneumococcal and HZ vaccines differed by patient age and HCP group (Supplementary Table 1 in the online supplement). Strong HZ vaccine recommendations for patients 50 to 64 years of age were significantly lower for pulmonologists (44.2%) compared to all other HCPs (FPs 62.9%, NPs 62.0%, and PAs 59.4%, P<.001) (Table 1). Pulmonologists also reported lower rates of any pneumococcal vaccinations in the 50 to 64 years age group. A total of 10.9% of pulmonologists reported they “don’t know” the age for beginning HZ vaccinations (Supplementary Table 2 in the online supplement).
Pulmonologists, compared to the other HCPs, were the least likely to strongly agree that HZ, post herpetic neuralgia, and HZ eye complications caused sufficient burden in patients with COPD to strongly recommend the HZ vaccine (pulmonologists 41.1%, FPs 63.3 %, NPs 59.2%, and PAs 55.1%, P<.001). They were also most likely to report being “not sure” regarding HZ vaccine recommendations for ages 50 to 59 and 80+ years (Supplementary Table 1 in the online supplement). Longer practice experience (10+ versus <10 years) in all HCP groups was associated with higher rates of strongly agreeing that HZ burden would warrant vaccination (P<0.005) with the results not different for HCPs <50 years of age versus 50+ years of age.
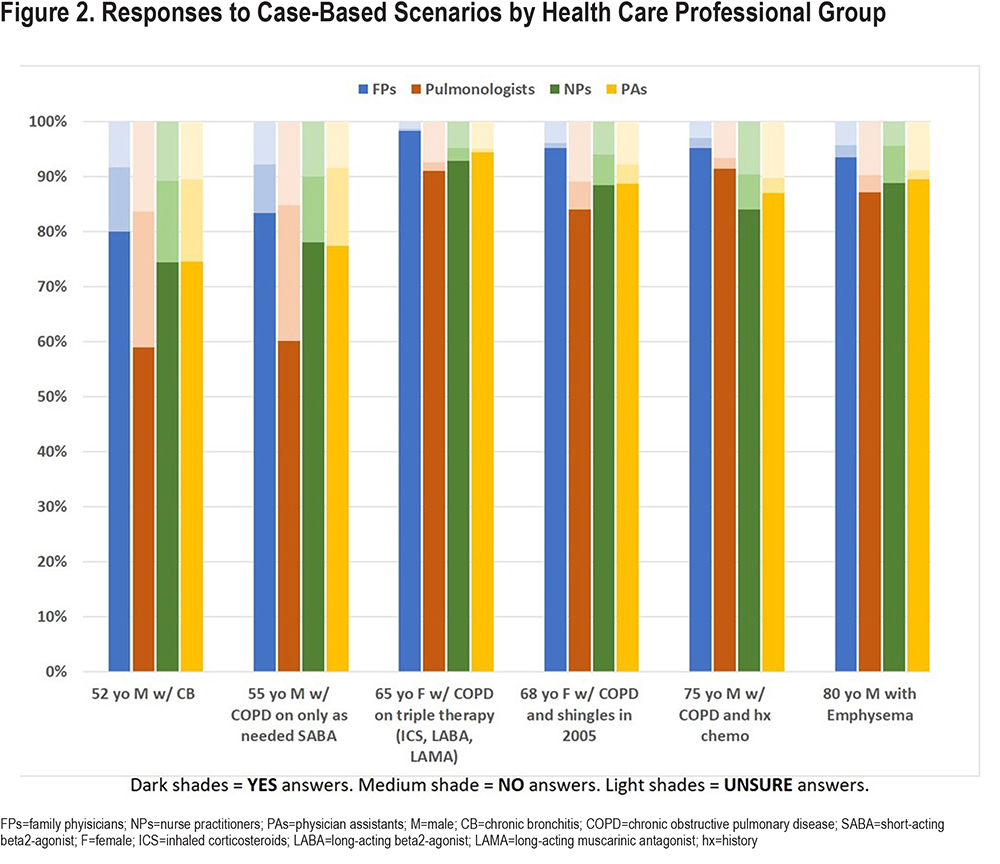
Responses to the 6 brief cases highlight differences by HCP groups with the greatest differences related to ACIP HZ recommendations (Figure 2). Significantly fewer pulmonologists, (P<.001) compared to all other groups, responded that HZ vaccines should be recommended/given to patients in the 2 cases of patients in their 50s and significantly more reported they were “unsure of recommendations” (P<.01). Other significant deviations from current ACIP recommendations occurred in the 75-year-old person with COPD and a history of chemotherapy (NPs and PAs lower versus FPs, P<.001) and the 68-year-old woman with a prior history of shingles (pulmonologists lower versus FPs, P<.001) with PAs’ and NPs’ rates between those of FPs and pulmonologists (Figure 2). There were fewer differences for influenza and pneumococcal vaccine recommendations across all cases and all HCP groups (Supplementary Table 2 in the online supplement).
HCPs varied in types of HZ vaccines they recommend/administer to patients with COPD with the ACIP-preferred 2-dose recombinant vaccine (Shingrix in the United States) selected by 87.3% of FPs, 62.4% of NPs, 59.7% of PAs, and 48.1% of pulmonologists (P<.001). Contrary to current ACIP recommendations for preference for the 2-dose HZ vaccine, about 30% of pulmonologists, NPs, and PAs reported continuing to recommend either of the 1- or 2-dose HZ vaccine versus 12.2% of FPs (P<.001). FPs (54.6%) were also significantly more likely to recommend/administer the 2-dose recombinant vaccine in patients who previously received the 1-dose live attenuated vaccine compared to all others (pulmonologists=14.0%, NPs=34.0%, PAs=36.0%, P<.001). Among all HPC groups, pulmonologists reported the highest rate of not recommending HZ vaccine at 20.9% versus PAs 12.0%, NPs 5.2%, and FPs 2.6% (P<.001) (Table 1) (Supplementary Table 3 in the online supplement).
Overall, the HCPs were more likely to refer patients to a pharmacist rather than administering HZ vaccines in their offices with pulmonologists the least likely to administer HZ vaccines (FPs 46.3%, pulmonologists 9.0%, NPs 25.6%, and PAs 36.7%, P<.001) (Table 1). Conversely, most HCPs reported stocking and administering influenza and pneumococcal vaccines in their offices (Supplementary Table 4 in the online supplement).
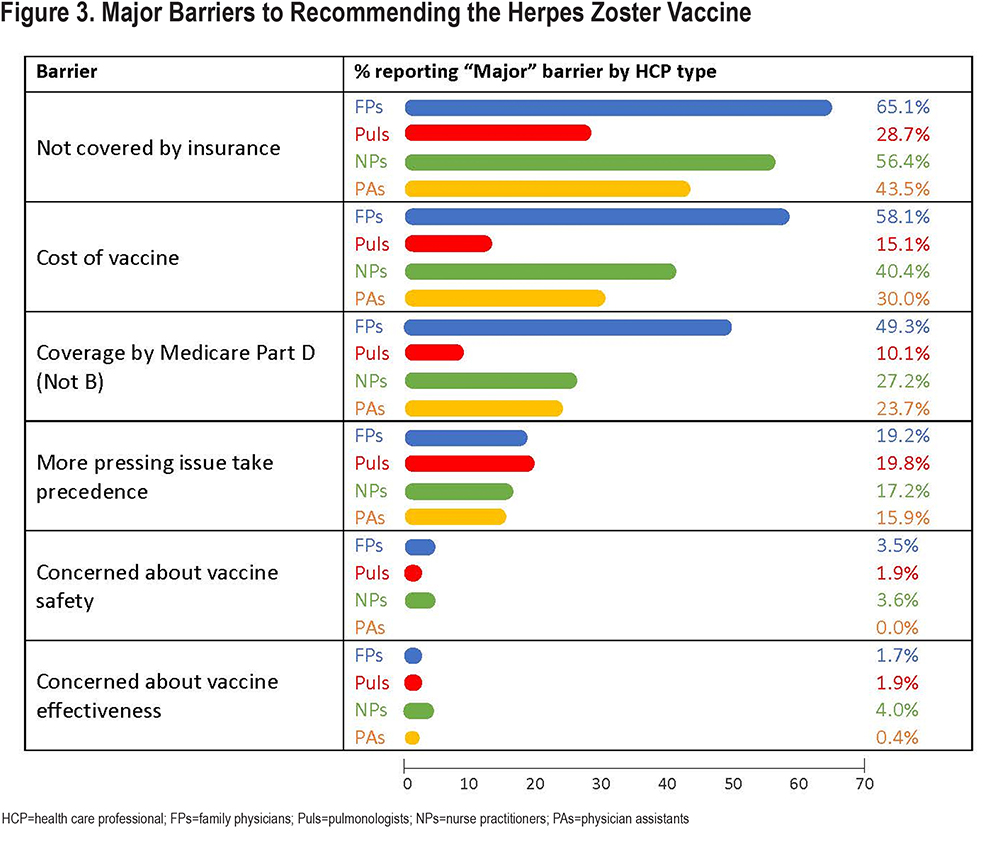
All HCPs reported barriers to HZ vaccinations with pulmonologists the least likely to report concerns about lack of insurance coverage, costs, and issues with Part D Medicare coverage (Figure 3 highlights the most common major barriers). Very few HCPs reported that vaccine safety, efficacy, or availability were barriers and only 20% reported “more pressing medical issues” as a major barrier. Supplementary Table 5 in the online supplement displays all reported major and minor barriers. Overall, 93.4% of these HCPs reported that the coronavirus disease 2019 (COVID-19) pandemic has not changed their adult vaccine recommendations/administration, with <5% reporting delaying non-COVID-19 vaccines.
After the Video
Altogether, 608 of the 1020 HCPs were invited to and completed Part 2. Based primarily on significant numbers of non-ACIP HZ concordant responses to cases and lack of strong HZ vaccine recommendations, the Part 2 cohort included pulmonologists (81.1%), NPs (67.2%), PAs (45.6%), and FPs (43.7%) (P=.001). Over 86% of Part 2 respondents reported the video presented new information in several areas including the increased risk of HZ in patients with COPD—47.5% (all new) and 38.7% (somewhat new) with lower rates for all or somewhat new information reported among FPs versus all others (P<.001). In addition, the responses indicated the video presented high levels of all new or somewhat new information on the 2 types of HZ vaccines for most HCPs (pulmonologists 79.2%, NPs 64.3%, and PAs 65.1%, versus FPs 27.0%; P<.001) and current HZ ACIP-recommendations (pulmonologists 86.3%, NPs 77.4%, and PAs 78.3 versus FPs 46.0%; P<.001). The pulmonologists who reported in Part 1 that they currently made no HZ vaccine recommendations were the most likely to report the information on the 2 types of HZ vaccines was all or somewhat new compared to the other HCPs who did not make HZ vaccine recommendations (P<.03) (Table 2) (Supplementary Table 6 in the online supplement).
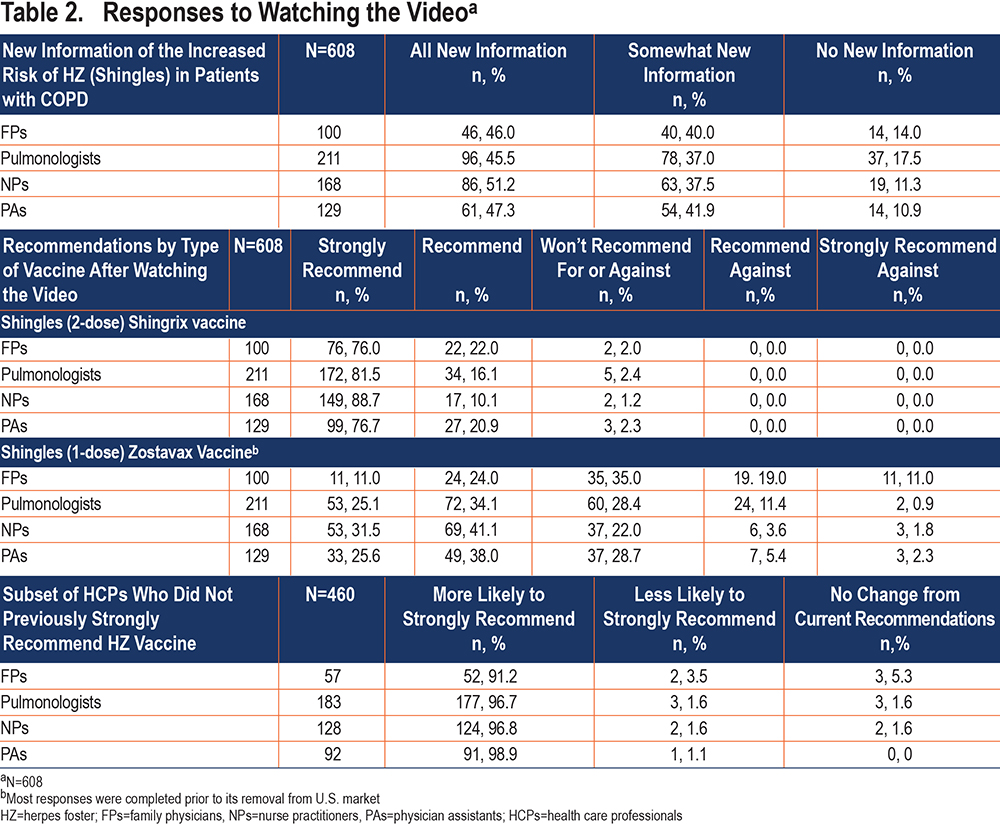
More than half of NPs (69.6%), pulmonologists (64.9%), and PAs (52.7%) versus FPs (35.0%) found the video very helpful for supporting future HZ vaccine patient discussions (P<.001). Overall, 75% or more of NPs, PAs, and pulmonologists reported the video was also helpful for considering future decisions about adding HZ vaccine office administration compared to 56% of FPs (P<.003) (Supplementary Table 7 in the online supplement). Among those chosen for part 2 due to lack of strong HZ vaccine recommendations (in any age group), >91% stated they were more likely to recommend HZ vaccines and the 2-dose HZ vaccine after viewing the video (Table 2) (Supplementary Table 8 in the online supplement).
Discussion
These surveyed HCPs supported vaccine recommendations as the responsibility of all HCPs and reported high rates of recommendations for influenza and pneumococcal vaccines, however, reported rates for HZ vaccine recommendations were significantly lower. In addition, the HZ recommendations reported were often not concordant with the 2018 ACIP HZ recommendations which were the most recent at the time of fielding the survey.11 Opportunities to enhance knowledge and increase awareness and vaccine recommendations appeared to be highest for HZ vaccine in adults 50 to 59 years of age, those with prior HZ or prior one-dose HZ vaccine receipt, and concerns about possible immunosuppression (prior cancer therapy and use of inhaled corticosteroids ) with the greatest opportunities among pulmonologists. Post video responses suggest that short, focused education can enhance knowledge and vaccine recommendation intent. Improvements were specifically noted for reported future HZ vaccine recommendation intent and perceived newness of video information on the risk of HZ in those with COPD and current ACIP HZ vaccine recommendations.
Studies of HCPs’ vaccine attitudes and practices are numerous,23-28 and have reported that pulmonologists and other subspecialists believed vaccine recommendations/administration were the responsibility of primary care.37 While the overwhelming majority (94.8%) of all respondents’ response that vaccine recommendations are the responsibility of all HCPs is encouraging, the responses to the COPD case-based HZ recommendations were not consistent with this and appear to reflect a lack of awareness of the then current 2018 ACIP HZ recommendations11 for both appropriate ages (especially 50 to 59 years) and preferred type of vaccine. The gaps between pulmonologists and primary care HZ recommendations reported here were confirmed in results from the patient portion of this study where only 26.6% of patient respondents who received care from a pulmonologist remembered receiving any HZ vaccine recommendations compared to 68.8% of those who attended primary care offices.36,38 This discrepancy appears to confirm the opportunities to enhance pulmonologists’ vaccine awareness and recommendations. The recent changes in the ACIP recommendations to also offer the 2-dose HZ vaccine to individuals 19 to 50 years of age with COPD and other chronic illnesses,12 as well as the addition of the HZ vaccine to the GOLD care recommendations for those with stable COPD,13 may enhance opportunities to educate and involve both primary care and lung specialists in strongly recommending or giving HZ vaccines to people with COPD.
HCP-perceived barriers to adult vaccinations, especially influenza and pneumococcal vaccines, have been widely reported and may limit vaccine recommendations, especially older reports of vaccine safety and effectiveness.23-31,33-35,38,39 Here the rates of concern about HZ vaccine safety and effectiveness were very low (<4% of any group) and some of the lowest among recently published results.27,31,40 The most common major barriers reported in our study were related to costs: cost of vaccine, lack of insurance coverage, and coverage falling under Medicare Part D which can require patients to pay for clinic-based vaccinations and await Medicare reimbursement.41 Pulmonologists were significantly less likely than any other group to consider cost-concerns as major barriers, which may reflect differences in dealing with these issues, lower rates of HZ vaccine administration, or pulmonologists having better systems to address them. This should be further explored. Less than 20% of all respondents reported “more pressing medical issues” as a major barrier which may reflect increasing perceptions of the value of vaccine prevention.42-44
None of the HCP respondents reported any major changes in immunization practices during the pandemic, which is different from what has been reported in studies of pandemic-era health care.45,46 The apparent differences may be due to the way the question was interpreted—if patients attended in-person visits, vaccines were offered, yet we know that in-person and routine visits declined during the pandemic. It is important to follow adult vaccination rates to see if they return to pre-pandemic levels and in the case of HZ, continue to rise to equal rates of other adult vaccines.
The invitation to Part 2 was based on initial responses not concordant with ACIP HZ recommendations or that suggested a lack of awareness of the HZ burden in COPD. Pulmonologists were most likely to qualify, suggesting they had the greatest opportunities for additional education. The high rates of reported new and useful information related to ACIP-recommended types and indications for HZ vaccines and initiating patient discussion about HZ vaccines were encouraging suggesting a significant potential impact of brief video education.32 The reports of high rates of future strong HZ vaccine recommendations requires confirmation using actual practice data. While there is some evidence to suggest that patient testimonials or anecdotal reports have a measurable positive impact on learning,47 future studies should assess the value of both the didactic and patient testimonial components of education.
This study has strengths and limitations that may affect the generalizability of the results. Strengths include the addition of NPs and PAs to the HCPs. We found no other HZ vaccine publications that included NPs or PAs. In the United States, both NPs and PAs are important vaccinators, often in independent practice or in practice without real-time oversight or collaboration with physicians and need to be included when assessing HCPs’ adult vaccine beliefs, attitudes, and practices. Among our respondents, NPs' and PAs’ responses were not always the same as either FPs’ or pulmonologists’ responses, highlighting the importance of their inclusion to fully understand adult vaccine practices and identify educational opportunities.48 Limitations include the variable HCP response rate that was low for both physician groups. The low pulmonologist response rate may have been in part due to the timing of the study during the pandemic when many pulmonologists/critical care physicians were busy managing COVID-19 care. Physician response rates were similar to those reported from other recent HCP surveys.49 While the overall socio-demographic and practice characteristics of the HCP samples appear to be similar to all HCPs in the 4 areas, respondents who agreed to answer the survey may have higher interest in adult immunizations or COPD than non-respondents. The results reflect HCPs’ self-reported awareness and actions related to adult vaccines but the concordance between self-reported clinical behavior and actual clinical behavior is controversial. We do not know to what extent the self-reported practices correlate with objective measures of current clinicians’ performance or their reported future intentions.50 However, evidence has been published demonstrating that changes in knowledge or attitudes have resulted in changes in behavior.51 This survey was conducted during the COVID-19 pandemic and responses and respondents may have been influenced by the widespread disruption of clinical care, especially outpatient and preventive clinical care.45 Running the full 5-minutes of the video was required to move on to the post video questions in Part 2, but we cannot confirm that respondents actually viewed the video as it played.
Conclusions
HZ educational opportunities exist for all primary care and specialist HCPs, with the greatest opportunities among pulmonologists. Identified opportunities exist for HZ ACIP-preferred age, vaccine type, and patient selection recommendations further supported by recent GOLD recommendations. The educational video was reported to provide new and useful information regarding an increased risk of HZ in those with COPD, current HZ vaccine recommendations, and initiating HZ vaccine discussions with patients. Among HCPs not strongly recommending HZ vaccinations prior to watching the video, most reported they now intend to strongly recommend HZ vaccines. These results suggest that brief education may improve HCPs’ future vaccination recommendations.
Acknowledgements
BPY takes responsibility for (is the guarantor of) the content of the manuscript, including the data and analysis. BPY and EC had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. BPY, EC, DM, SM, NL, DW, JC, and JKC contributed substantially to the study design, data analysis and interpretation, and the writing and review of the manuscript.
Declaration of Interest
BPY reports COPD or HZ consulting or advisory board fees from GlaxoSmithKline, Boehringer Ingelheim, TEVA, and Pulmonx. NYL, DDM, SM, EC, JC, JKC, and DW report no potential conflicts of interest.