Running Head: Proactive Pulmonary E-Consult Acceptable for Primary Care
Funding support: This work was supported and awarded by VA Health Services Research and Development, IIR 12-130-2 (Au). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Date of acceptance: November 30, 2022 | Published Online Date: December 5, 2022
Abbreviations: AECOPD=acute exacerbation of COPD; CBOCs=community-based outpatient clinics; COPD=chronic obstructive pulmonary disease; DC=discharge; e-consult=electronic consultation; EHR=electronic health record; InCasE=Integrating Care After Exacerbation of COPD; PCP=primary care provider; VHA=Veterans Health Administration
Citation: Spece LJ, Weppner WG, Weiner BJ, et al. Primary care provider experience with proactive e-consults to improve COPD outcomes and access to specialty care. Chronic Obstr Pulm Dis. 2023; 10(1): 46-54. doi: http://doi.org/10.15326/jcopdf.2022.0357
Online Supplemental Material: Read Online Supplemental Material (347KB)
Introduction
Chronic obstructive pulmonary disease (COPD) exacerbations are potentially life-threatening events for patients and present numerous challenges for health care systems.1 Despite efforts to improve care quality, most patients discharged after a COPD exacerbation do not receive care known to improve outcomes.2 The time after hospitalization for COPD is a prime period for intervention to improve patient recovery and decrease risk of recurrence.3 In the U.S. health care system, access to pulmonologists is limited so COPD management typically falls to primary care providers (PCPs).4 Electronic consultations (e-consults) are increasingly adopted to expand access to specialty care.5 Prior work demonstrates that PCPs perceive e-consults as valuable for improving care quality and timeliness, and increase access to specialists.6 However, there is also a negative perception that e-consults increase PCP workload, which could pose limits to adoption by time-constrained providers.7
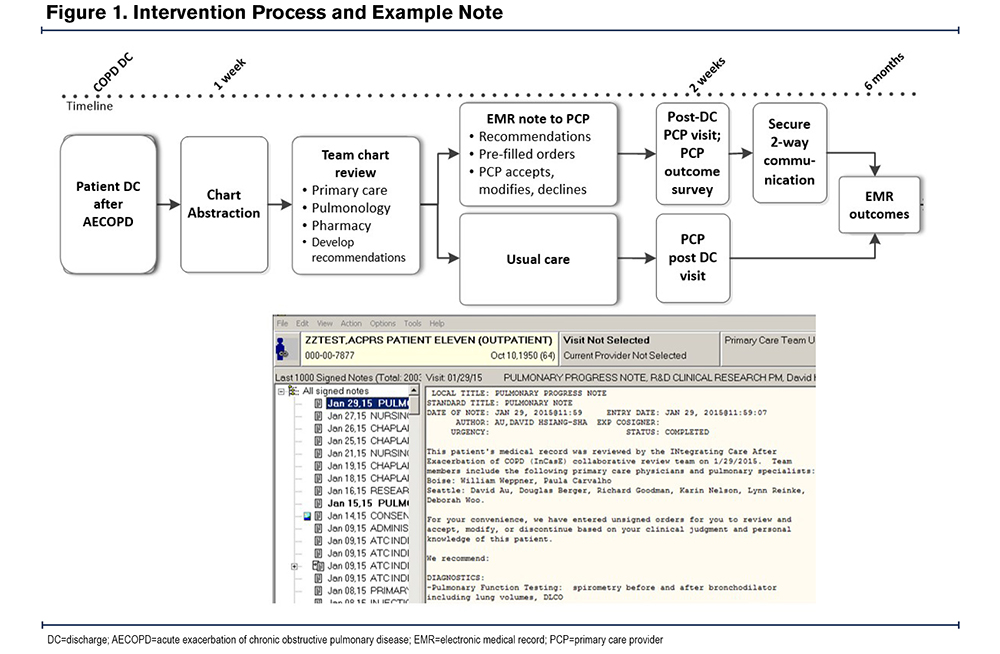
To address these gaps, our group designed a pragmatic, health system intervention with a goal to improve access to pulmonologists, collaboration with primary care, and patient outcomes after hospitalization for COPD.8 The intervention included 5 components: (1) proactive identification of patients recently hospitalized for COPD using a population-based approach, (2) a collaborative multidisciplinary team including a pulmonologist to review the health record and develop tailored treatment recommendations, (3) an e-consult summarizing the salient history, treatment recommendations, and rationale, (4) pre-populated but unsigned orders for PCPs to endorse, modify, or reject, and (5) timed recommendations to coincide with a post-discharge PCP follow-up visit (Figure 1). The intervention yielded positive results; PCPs in the intervention arm adopted most recommendations by the study team (77.3%) and patients reported improved symptom control and quality of life (Clinical COPD Questionnaire scores; -0.47; 95% confidence interval, -0.85 to -0.09).8
This convergent mixed methods study used semi-structured interviews and a survey completed by PCPs who participated in the InCasE clinical trial. Our goal was to further our understanding of the intervention factors associated with PCP adoption to better explain the successful result. Specifically, we sought to understand the feasibility, acceptability, and appropriateness of the intervention from the perspective of the PCP.
Methods
This study was completed as part of an evaluation of a clinical trial testing a health system intervention at 2 Veterans Health Administration (VHA) health care systems and 10 community-based outpatient clinics (CBOCs). The intervention was tested in a stepped-wedge design and 139 PCPs experienced the intervention over a 30-month trial period starting in May 2015. The VHA national organizational committee and union offices reviewed and approved provider interview guides and surveys (ClinicalTrials.gov Identifier: NCT02021955). This study was approved by the VA Institutional Review Board (#1587554, Seattle, #1587583, Boise).
Participants and Recruitment
Between September 2016 and January 2018, we conducted semi-structured, phone-based interviews with PCPs who experienced InCasE. Eligible PCPs included physicians, nurse practitioners, physician assistants, and advanced trainees in those fields. We used VA email to contact eligible PCPs to participate in the survey. We used email to contact a purposive sample of PCPs to participate in interviews. Qualitative data collection continued until saturation was reached (i.e., when data failed to generate new findings).9 We invited all PCPs to complete the quantitative survey after their first intervention exposure.
Qualitative Interviews and Analysis
Our team designed semi-structured interview guides to elicit PCPs’ experiences with the intervention (See the online supplement). We included open-ended questions to assess general experience with the intervention and its implementation based on pre-specified themes: (1) acceptability, (2) appropriateness, and (3) feasibility. Acceptability reflects the extent to which a given practice or intervention matches individuals’ needs, expectations, or preferences.10 Appropriateness refers to the perceived fit, relevance, or compatibility of a practice or intervention for a given purpose or a given context.10 For example, a practice or intervention may be perceived as appropriate if it is seen to be efficacious given the context, including patient specific factors, and consistent with social norms regarding conduct in particular situations. Practice alignment with the organizational mission will also factor into perceptions of appropriateness. Feasibility refers to the extent to which a practice or intervention can be successfully implemented and used within a given setting or context.10 For example, a practice will be deemed feasible if it can be performed easily and conveniently given the context and existing resources. We used structured follow-up probes grounded in an interviewee’s verbatim language to elicit greater detail. The interview guide was updated iteratively to explore emerging and unanticipated themes. The interviews were coded using simultaneous deductive and inductive content analysis.11 Inductive content analysis consists of open/unstructured coding and allows for the identification of emergent, previously unidentified, or unexpected content, while deductive content analysis is structured and consists of identifying meaningful units that fit within a-priori categories. Additional details regarding the conduct of interviews can be found in the online supplement. We used qualitative software (ATLAS.ti 7; Scientific Software Development, Berlin, Germany) for data management and coding.
Quantitative Survey
Surveys were administered by email and mail to 139 PCPs between August 2015 and December 2017. PCPs received a survey invitation 1 week after initial exposure to the intervention. The survey had 9 items and 1 example is “The InCasE intervention has increased my workload,” with a rated response from “Strongly Disagree” to “Strongly Agree” on the 5-point Likert scale. The survey is available in the online supplement. Providers who answered “Agree” or “Strongly Agree” were aggregated for descriptive analysis.
Mixed Methods Analysis
We used convergent mixed methods to identify qualitative data that enhanced our understanding of survey findings. Data were analyzed using the Merging Data Approach (QUAL-QUAN).12 Following data collection and concurrent data analysis of the quantitative provider survey, deductive analysis of acceptability, appropriateness, and feasibility with inductive content analysis. A merging data approach was used to integrate the survey data that complements the qualitative narrative by providing quantitative findings from a broader, more representative sample.
Results
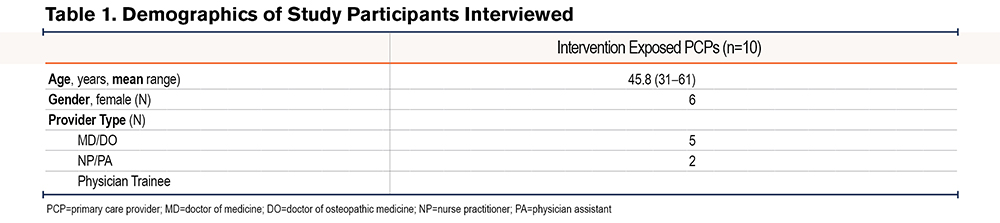
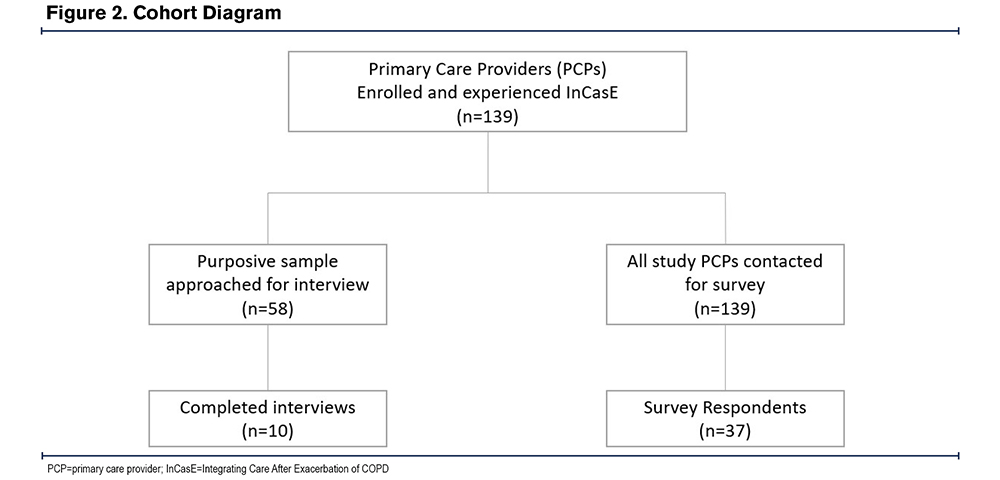
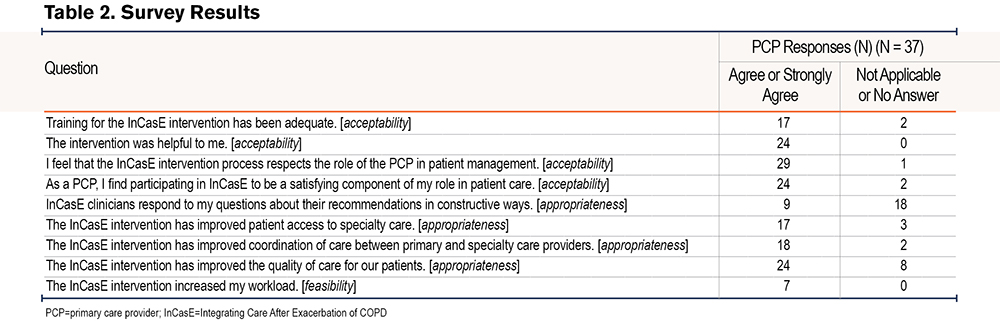
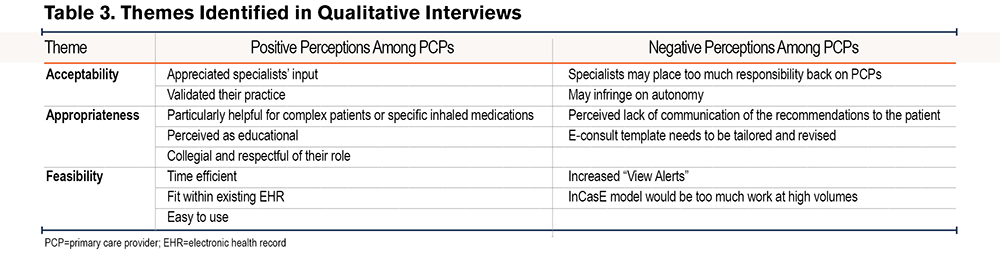
We contacted 58 intervention-exposed PCPs, of whom 10 completed interviews (17%, 10/58). Demographics of interview participants are presented in Table 1. Thirty-seven PCPs completed the survey (27%, 37/139 PCPs) (Figure 2). The response rates are consistent with prior studies.13,14 The survey results are presented in Table 2. Using deductive coding with our a priori constructs, PCPs found the intervention to be acceptable, appropriate, and feasible but also identified negative observations of the intervention (Table 3).
Acceptability
In the survey, most PCPs found the InCasE intervention to be acceptable. Most agreed that the intervention was helpful (65%, n=24), satisfying (65%, n=24), and respectful of the PCP role (78%, n=29). These positive perspectives were elaborated upon in interviews:
“I felt like the study team was there to help me and help the Veteran, working collaboratively.”
“It’s great to have somebody else look at what’s going on independently and to have feedback and recommendations.”
“They validated some of the practices that I was already doing.”
Providers may find a practice to be unacceptable if it is perceived to undercut their clinical autonomy. One survey participant did not find the intervention to be helpful (3%, n=1) or respectful (3%, n=1). In qualitative interviews, one participant perceived a threat to their clinical autonomy from the intervention:
“At what point does the primary care provider just become someone that just takes recommendations and doesn’t have to think for him or herself?”
Appropriateness
Most survey respondents agreed that the InCasE intervention was appropriate as a means of improving care quality (65%, n=24). About half agreed that InCasE improved care coordination (49%, n=18) and patient access to specialty medicine (50%, n=18). In interviews, PCPs elaborated that they perceived InCasE to be evidence-based, educational, and efficacious:
“I think this type of thing is very helpful for providers. Not just for COPD, but across the board to assist PCPs because we’re so buried under the number of patients we must follow. If someone’s a special case, or if they have a real complicated problem, that can be a challenge to follow and to give it full attention. And if there’s back up on that, that’s fantastic.”
“Certainly, with [recommending] a specific inhaler. There was good data for that inhaler, I didn’t have that information. I think that’s all good.”
“It’s sort of like an educational intervention that’s centered around the patient, which makes it more meaningful, and it helps the patient.”
Interviewees also noted that InCasE respected social norms in the consultant-PCP relationship:
“It wasn’t offered as ‘you moron, you’ve missed this obvious thing to do’. It was more collegial, helping hand. It was friendly.”
“It wasn’t like with some situations with certain specialties, talking down to a provider. So, it was positive reinforcement of recommendations.”
“It wasn’t written as a directive, just a suggestion of various things. So, it’s just a matter of me taking the steps or not.”
One interviewee also noted that InCasE improved access to pulmonologists after COPD exacerbation:
“If somebody is admitted for a COPD exacerbation, they don’t always see a pulmonary doc, so that’s why InCasE was kind of nice, because the pulmonary team is who is looking at it.”
One interviewee also noted that the intervention could be appropriate for other chronic diseases:
“I’m just wondering and hoping that they might do something similar with major chronic disease conditions, whether opioids, diabetes, CHF admissions, acute MI.”
Providers may judge an intervention as inappropriate if perceived to be contrary to organizational norms, and/or ineffective in meeting varied patients’ needs. Some PCPs agreed that the InCasE intervention team was responsive to their questions (24%, n=9) but nearly half responded that this was not applicable to their experience (49%, n=18). In interviews, some PCPs noted friction in the communication of the e-consult recommendations to the patient:
“Who’s going to teach them about the new medicine and, am I supposed to call them? Some of the logistics were not clear to me.”
“I haven’t talked to the patient specifically about any of those treatments.”
Other negative themes emerged in relation to communication of specialists’ recommendations with InCasE. Specifically, some PCPs did not like the template used to document in the electronic health record:
“Just the impression that this is a standard template kind of prompts the reaction of, ‘ugh, is this something worth reading?’”
PCPs made suggestions about how to improve the template:
“I think it could be made more friendly. If it were more apparent that this is a specialty review, a very brief statement that this is a specialty review of this patient, and these are my recommendations.”
“Perhaps a personalized paragraph of maybe a few sentences followed by bullet point recommendations at the top in a very prominent way, and then the template could be down below, so that we could have the option to ignore the template.”
Feasibility
In the survey, some respondents felt that InCasE increased their workload (19%, n=7). This was repeated among interviewees, noting specifically that the intervention was efficient in terms of time:
“They don’t take long to review. And they are fairly easy to implement.”
“I remember consults being put in for me, so I didn’t have to take that step.”
“I kind of look through it to see if there’s anything I disagree with, which, so far there has not been, and just sign the orders essentially.”
“Efficient and useful.”
The intervention was also noted to fit well into existing workflows:
“It flows very well with the way our system works with the computer within the VA system. So that part’s not hard.”
An intervention could be viewed as infeasible if perceived to be too costly or time consuming (resource limitations) or too complex. Three survey participants strongly agreed that the intervention increased their workload (8%, n=3). Some interviewees noted negative perceptions regarding workload:
“You worry with interventions like these that they may increase the amount of work that you have to do.”
“We all get a lot of View Alerts (electronic health records [EHR] notifications), so it’s… more View Alerts.”
“I certainly wouldn’t want to be inundated with InCasE information. I wouldn’t like
that.”
“That someone is going to come in, meddle around, stir things up and that you’re going to have to do a lot more.”
PCPs also expressed a desire to know more about the enrollment process and patient selection:
“I think if you make us more aware of when it’s happening, I think it would be much
more useable.”
“How did you go about enrolling these people? If these criteria were given and then if patients came through, maybe we could’ve enrolled some.”
“It would have been nice to say, ‘hey these guys are in this study, just letting you know that, pay attention, things will be coming.”
Discussion
InCasE changes the delivery model for specialty medicine, shifting the focus of specialists toward the health of populations, rather than on individual cases. In this new delivery model, specialists work collaboratively with PCPs across geographically separate institutions while expanding access to specialists’ expertise. Specialist review is triggered automatically using structured criteria rather than by PCP initiation. Our qualitative work sheds light on several potential barriers and facilitators to a proactive, e-consult care delivery model. Overall, PCPs found InCasE to be acceptable and feasible, but they had concerns considering the appropriateness of InCasE to their workflow. The challenges noted by PCPs highlight the difficulties faced by health systems that are responsible for patients across a broad geography to deliver complex, personalized care to an aging population with multimorbidity and finite resources. These findings support wider expansion of the program and will help refine the intervention for future implementation. Our findings also suggest that InCasE could provide a transferable care delivery model for other chronic diseases to improve patient outcomes, support primary care, and provide access to specialty care.
One of the key components likely to have contributed to the favorable experience was the proactive identification of patients for consultation after hospitalization for COPD. The InCasE e-consult overcame wait times, geographic proximity, and other known barriers of access to consultation with specialty medicine.15 While unsolicited, this e-consult mechanism lessened the burden on primary care to arrange specialty referrals and coordinate care following discharge. A second key component of InCasE was the pre-populated orders entered by the study team, also saving valuable clinic time while respecting PCP autonomy. Results from the clinical trial indicated that pre-written orders for medications, diagnostics, and other therapies were accepted by PCPs at high rates.8 A third component was the tone of the e-consult note. The e-consults offered praise for guideline-concordant care, and acknowledged limitations in care delivery (e.g., patient previously declined tobacco cessation efforts, significant psychosocial barriers). Taken together, these 3 components could explain much of PCP’s positive perception of InCasE when describing it as respectful, time efficient, and fitting well into the existing clinic workflow. In the traditional referral system, PCPs perform these tasks without assistance and describe a more adversarial relationship with specialty medicine.16,17 In contrast, PCPs described the interaction with the InCasE team to be collegial.
At the same time, some PCPs voiced frustration with InCasE related to a perceived lack of communication. The InCasE intervention disrupts usual patterns of communication in the triangle between specialist-PCP-patient, because InCasE specialists communicate solely with the PCP and do not speak directly with the patient. In typical face-to-face consults, the consultant would instead speak directly to patients and copy the PCP on a written note. Furthermore, the InCasE e-consult mechanism is unsolicited, whereas, typical e-consults are requested by the PCP. Some providers also expressed concern that their workload could increase, and autonomy could decrease if there were multiple interventions modeled after InCasE. This study did not include the patient perspective, so it is not clear if these negative perceptions reached the patients. As health systems consider similar interventions, they will need to find a balance between efficiency of automatic, population-based referrals and PCP workload and autonomy.
As part of the VA’s goal to operate as a learning health system, we have used these study findings to refine the intervention. We launched another intervention modeled after InCasE to improve the quality of prescriptions for stable COPD. Our group changed the PCP recruitment materials to provide more clarity regarding patient selection based on the results of this study. We also revised the consult note template to increase the personalization and tailoring to each patient. For the future, we plan to engage with key stakeholders to understand how to communicate the consult findings to Veterans/patients in a way that is acceptable and feasible for all parties. This could take the form of scripted suggestions for communication with patients, or a mechanism for PCPs to request a follow-up call quickly and easily between the patient and specialist.
Our study provides perspectives around the adoption of InCasE but has a few noteworthy limitations. First, our study is limited to a small number of PCPs at 2 sites of whom a minority opted to participate. There could be response bias and we do not know if non-responders had similar experiences to those who participated. Although our interviews included a small number of providers, we were able to achieve saturation of themes and there was repetition of those themes among participants. Our experience of early saturation speaks to the consistency of experience. Also, PCPs practicing in the VA health care system may differ from providers in other systems.18 VA providers may have differing values on health care priorities, perceptions on EHR-based interventions, the relationship between primary and specialty care, and autonomy in decisions. There are practical and financial considerations in referrals for payers and networks who rely on fee-for-service reimbursement and do not share a common electronic health record, though this is less of a limitation as the private sector increasingly adopts more value-based payment models. For these limitations, this study has important strengths, including that it was conducted as part of a prospective clinical trial of an intervention that demonstrated a high rate of adoption by PCPs and improved quality of life outcomes among patients. We obtained both qualitative and quantitative data, giving us a fuller picture of how PCPs responded to the intervention.
Specialty medicine can improve access to high quality care using a population health approach in collaboration with primary care. InCasE provides an opportunity to redesign consultation with specialty medicine in a way that is acceptable, appropriate, and feasible to primary care. Further work will need to test how InCasE could be adapted to other clinical scenarios.
Acknowledgements
Author Contributions: Drs. Spece and Weppner had full access to all data used in this study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Au, Sayre, and Weppner. Acquisition, analysis, and interpretation of data: Epler, McDowell, Sayre, Spece, and Weppner. Drafting of the manuscript: Sayre, Spece, and Weppner. Critical revision of the manuscript for important intellectual content: all authors. Obtained funding: Au.
Declaration of Interest
LCF serves as Associate Editor at the Annals of the American Thoracic Society and receives consultant fees from the U.S. National Committee for Quality Assurance. DHA serves as Deputy Editor at the Annals of the American Thoracic Society and served on an advisory board for Boehringer Ingelheim, Inc., on gaps in quality of care. No other disclosures are reported.