Running Head: Physical Activity, Pollution, and Lung Function in COPD
Funding Support: Supported by National Institute of Environmental Health Sciences grants K23ES026204, R01ES031252, and P30ES000002 and the U.S. Environmental Protection Agency (EPA) grant RD-835872. This work’s contents are solely the responsibility of the grantee and do not necessarily represent the official views of the EPA. Furthermore, the EPA does not endorse the purchase of any commercial products or services mentioned in the publication.
Date of Acceptance: March 15, 2023 | Published Online Date: March 20, 2023
Abbreviations: COPD=chronic obstructive pulmonary disease; EPA=Environmental Protection Agency; FEV1=forced expiratory volume in 1 second; FVC=forced vital capacity; IQR= interquartile range; NO2=nitrogen dioxide; O3=ozone; PAM=personal air quality monitor; PM2.5=fine particulate matter; ppb=parts per billion; SPACE=Study of Pollution And COPD Exacerbation
Citation: Chen K, Aglan M, Purcell A, et al. Physical activity, air pollution exposure, and lung function interactions among adults with COPD. Chronic Obstr Pulm Dis. 2023; 10(2): 170-177. doi: http://doi.org/10.15326/jcopdf.2022.0385
Introduction
Chronic obstructive pulmonary disease (COPD) is an irreversible, progressive lung disease characterized by chronic respiratory symptoms and airflow limitation.1 Prior studies have identified outdoor air pollution as a trigger of COPD exacerbations, with a higher risk of COPD hospitalizations and COPD mortality during periods of higher outdoor air pollution levels.2-4 Recent studies utilizing personal air monitoring have determined that changes in air quality, even at relatively low levels, are associated with worse lung function and symptoms among adults with COPD.5,6
COPD patients often have low levels of physical activity, even early in the disease. Lower levels of physical activity are associated with poor outcomes, including COPD exacerbations, worse health-related quality of life, and mortality in COPD.7,8 Even though COPD patients often have respiratory limitations to exercise, physical activity is encouraged as it has been demonstrated to improve outcomes in COPD, including a lower risk of hospitalization, all-cause mortality, and respiratory mortality.9-12 However, exercise in outdoor settings may lead to greater exposure to air pollution and, therefore, may have potentially harmful effects on respiratory health. Higher minute ventilation during physical activity, whether it occurs indoors or outdoors, may also increase the effective dose of air pollution delivered to the lungs by increasing deposition to the lungs and thereby may augment short-term harmful effects of air pollutants.13 It is unknown if higher routine daily physical activity increases personal daily exposure to ambient air pollutants [such as fine particulate matter (PM2.5), nitrogen dioxide (NO2), and ozone (O3)], and whether physical activity attenuates or exacerbates the known effect of pollutants on lung function in patients with COPD.
In our Study of Pollution and COPD Exacerbation (SPACE), we recruited 30 former smokers with COPD living in an urban environment in the greater Boston area.6 We followed each participant for 4 non-consecutive months in different seasons over a year, during which participants measured their daily step count by Fitbit, daily personal exposure to pollutants (PM2.5, NO2, and O3) by a portable personal air quality monitor (PAM), and daily lung function by office-grade spirometers. We hypothesized that a higher daily step count would be associated with higher exposure to personal pollutants, and that physical activity would exacerbate the previously reported association between personal exposure to NO2 and lung function in this small study population.6
Methods
Study Population
The study population consists of 30 former smokers with COPD who were recruited as part of SPACE at Beth Israel Deaconess Medical Center in Boston, Massachusetts. To be eligible, study participants were required to be former smokers without any active smoking for at least 6 months prior to enrollment, have a ≥ 10 pack-year smoking history, and have a home address within 50 km of the Harvard air pollution supersite in Boston, Massachusetts, and a clinical diagnosis of COPD with at least moderate (Global Initiative for Chronic Obstructive Lung Disease stage 2)14 airflow obstruction, defined as forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) ratio of <0.70 and FEV1 <80% predicted, using National Health and Nutrition Examination Survey III prediction equations. Participants with a history of lung cancer, interstitial lung diseases, or bronchiectasis were ineligible to participate. The study was approved by the authorized institutional review board of the Beth Israel Deaconess Medical Center (Protocol # 2015P000336/03). Written informed consent was obtained from all study participants.
Data Collection
Participants entered the study between February 24, 2017, and January 17, 2019. At study entry, demographic information, height, weight, past medical history, medication history, and baseline measures of lung function were obtained, and participants were instructed on the use of the Fitbit, portable spirometer, and PAM to be used for subsequent data collection in the home. Participants were directly observed successfully completing lung function testing using the portable EasyOne™ spirometer at the entry visit and then used the same device at home. They were then observed for up to 4 non-consecutive 30-day periods in different seasons over 12 months. Participants measured their lung function daily in the morning before taking any medications, using the portable EasyOne™ Plus Diagnostic Spirometer, a device that meets American Thoracic Society guidelines15 and has built-in quality assurance and incentive software. EasyOne™ incorporates an automatic quality control function, where at least 3 acceptable reproducible maneuvers must be performed before a participant is able to complete a session. At the end of the follow-up, the 30 participants had contributed a total of 3314 observation days.
Exposure Assessment
We measured personal 24-hour step counts using the portable Fitbit® Charge 2 worn by participants each day for all hours, except during bathing (during which the participants were instructed to charge the device). We excluded observation days with a recorded total step count of zero. We measured personal pollutant exposures using PAMs (Atmospheric Sensors Ltd., model 520). Details about the PAM technology, reproducibility of pollutant measurements, and agreement with stationary monitors in diverse settings have been reported previously.16 All personal 24-hour exposure measures for PM2.5, NO2, and O3 collected during our study were calibrated against reference monitors prior to data analysis, as previously described.6
Statistical Analyses
Associations with Same-Day Pollutant Exposure and Daily Step Count:
To assess the association of daily step count with daily personal exposure to each pollutant, we constructed unadjusted multilevel linear mixed-effects models with random intercepts for person and person-observation month and an autoregressive correlation structure. We also constructed multivariable models with adjustments for age, sex, body mass index, season, humidity, and temperature.
Interaction Between Step Count and Previous-Day Pollutant Exposure on Daily Lung Function:
We have previously reported that personal exposure to NO2 is associated with lower lung function in this study population.6 To determine whether the relationship between prior-day personal exposure to pollutants (PM2.5, NO2, and O3) and daily lung function (FEV1 and FVC) differs by prior-day total step count, we included a cross-product term in our adjusted models and evaluated the p-value for the statistical test for interaction with step count. We classified step count per tertile: low (<1998 steps), medium (1988 – 4169 steps), and high (> 4169 steps). If we found evidence of effect modification (pinteraction<0.05), we performed stratified analyses to determine associations of pollution and lung function within each tertile of step count. All models were adjusted for age, sex, race, height, weight, pack years of cigarette use, education, income, season, temperature, and humidity.
Results
Study Participants
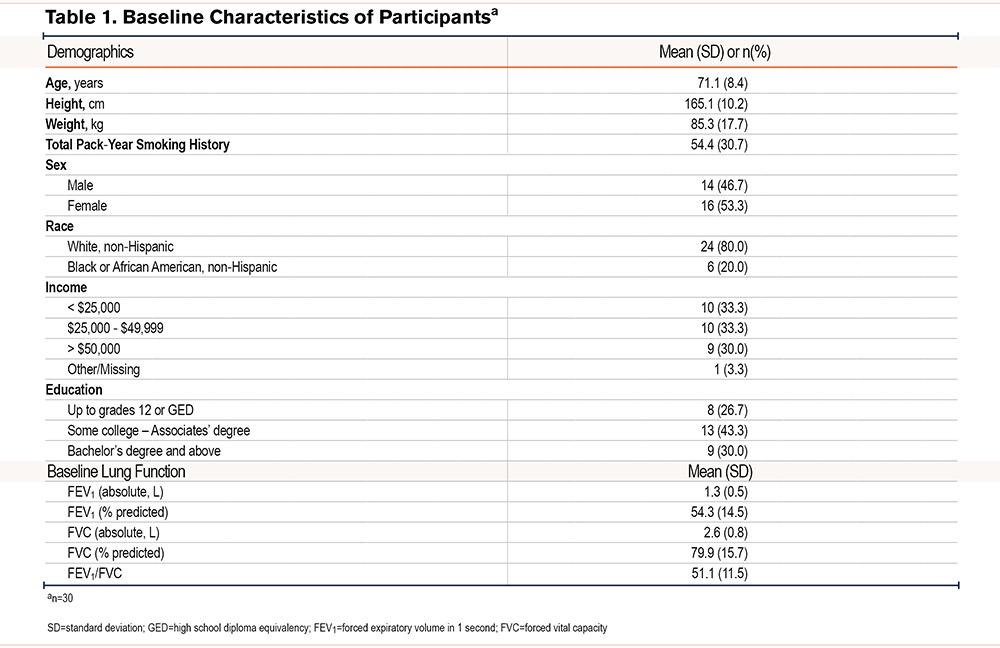
Baseline participant characteristics are reported in Table 1. Participants were on average 71.1±8.4 years of age and were 80% non-Hispanic White and 20% non-Hispanic Black or African American, with a slight majority of females. Baseline lung function was impaired, with a mean FEV1 of 54% predicted, FVC of 80% predicted, and FEV1/FVC ratio of 51%.
Exposure Distributions and Associations
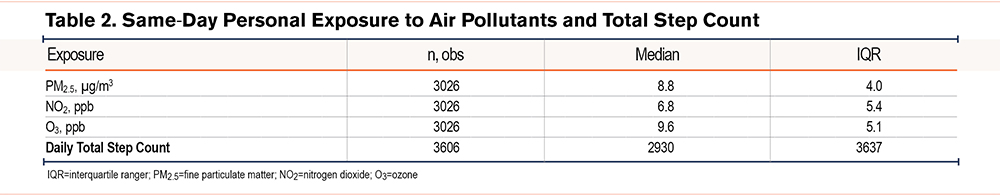
Table 2 displays the distribution of personal exposure to pollutants and daily total step count. Median previous-day 24-hour personal exposure to PM2.5 (8.8 μg/m3) was within the EPA 24-hour PM2.5 standard17 of 35 μg/m3 and the annual standard of 12 μg/m3. Median previous-day personal exposure to both NO2 and O3 were also relatively low (6.8 parts per billion [ppb] and 9.6 ppb, respectively). The median daily total step count was 2930 steps, which is a low level of physical activity (4000 steps or less) and falls below the recommended Centers for Disease Control and Prevention physical activity guideline of 10,000 daily steps.18
Associations with Same-Day Pollutant Exposure and Daily Step Count:
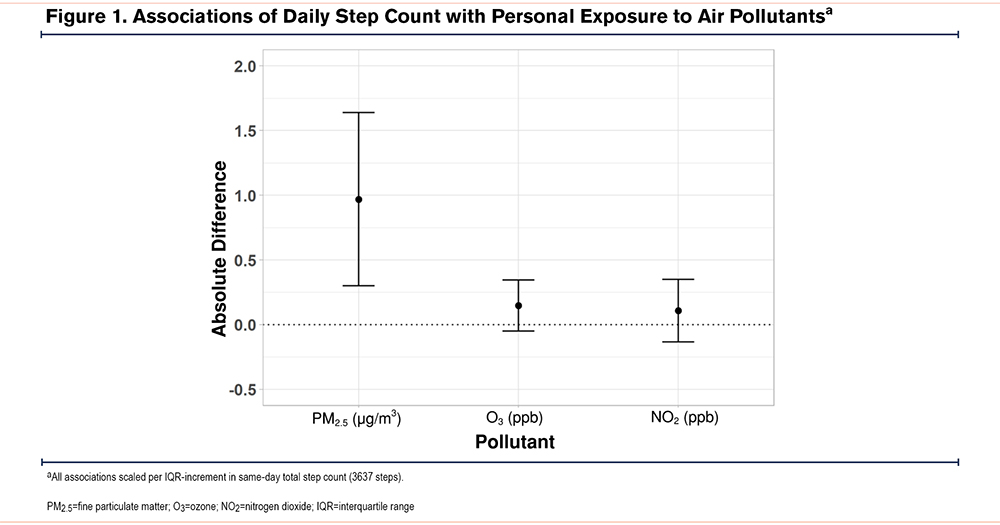
Adjusted associations between daily step count and personal exposure to each pollutant are presented in Figure 1. In adjusted models, higher daily physical activity was associated with higher same-day personal exposure to PM2.5, and O3, but not NO2. Each interquartile range (IQR) increment in daily step count was associated with a 0.97 µg/m3 (95% CI: 0.30, 1.64) higher exposure to PM2.5 and a 0.15 ppb (95% CI: -0.05, 0.35) higher personal exposure to O3. A similar pattern was seen in unadjusted models. For example, per IQR higher daily step count, daily PM2.5 was 0.98 µg/m3 higher (95% CI: 0.31, 1.65).
Interaction Between Step Count and Previous-Day Pollutant Exposure on Daily Lung Function:
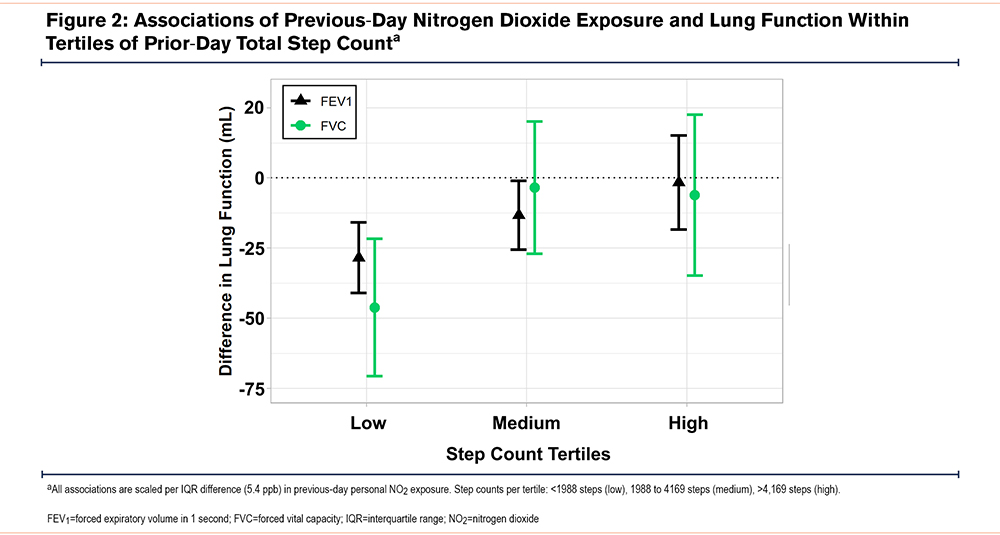
A total of 2689 participant days with exposure and lung function data were included for the analysis of effect modification by physical activity. Step count modified the relationship between prior-day NO2 and FEV1 (pinteraction=0.004) and FVC (pinteraction=0.045). We did not find evidence of effect modification by physical activity for the associations of PM2.5 or O3 with lung function.
We then examined associations of previous-day NO2 exposure and lung function within tertiles of prior-day total step count. The negative associations between NO2 and lung function were greatest in magnitude on participant days with the lowest level of physical activity and absent on participant days with the highest activity levels (Figure 2). For example, in the lowest tertile of physical activity (prior-day step count <1988 steps), each IQR increment in NO2 was associated with a 28.5 mL (95% CI: -41.0, -15.9) lower FEV1. On days when the prior-day step count was between 1988 and 4168 steps, we observed a 13.3 mL (95% CI: -25.5, -1.0) lower FEV1. In the highest tertile of physical activity (prior-day step count ≥4169 steps), there was no association between NO2 exposure and FEV1 (-1.6 mL, 95% CI: -18.4, 15.2).
Discussion
In this urban setting, routine physical activity resulted in a modest increase in pollution exposure compared to sedentary behavior for some pollutants. Higher daily step count was associated with a small increase in personal exposure to PM2.5, a small, borderline significant increase in exposure to O3, and no difference in exposure to NO2 among COPD patients living in the Boston area. We also found that physical activity, when examined continuously, attenuated the association between NO2 and lung function. When examining tertiles of physical activity, personal NO2 exposure was negatively associated with FEV1 and FVC on more sedentary days (in the lower tertiles of physical activity), but not on more active days (in the highest tertile of physical activity). These findings suggest that, within the relatively low pollution levels of the Boston area where our study population resided, higher daily physical activity appears to mitigate, not exacerbate, the harmful effects of NO2 on lung function in COPD. However, we did not find evidence of physical activity modifying associations of PM2.5 or O3 with lung function.
A limited number of studies have examined interactions between short-term exposure to pollution and physical activity on cardiopulmonary health, and few have focused on COPD.19,20 One case crossover study in London involving former smokers with COPD found a lung function benefit from walking for 2 hours in the relatively less polluted Hyde Park in London, but that walking along the more polluted Oxford street attenuated the lung function benefit of exercise.21 Estimated and/or measured exposure to NO2, PM2.5, black carbon, and fine particles was higher during the walk along the urban street compared to the park. Although not a primary aim of our study, we did not find that daily physical activity (as quantified by step count) improved lung function the next morning, and we did not measure lung function immediately after exercise. However, as reported in the London experiment, we did find an interaction between physical activity and pollution exposure on lung function, with a higher step count attenuating the harms of NO2 exposure on FEV1 and FVC. Notably, the London study also found, as in our Boston population, that higher exposure to NO2 was associated with lower lung function. In contrast, the London study did not directly test if the amount of physical activity mitigated or exacerbated the effect of a given level of pollution. Many patients, especially those limited by severe COPD, may not have a lot of choice about where they are physically active in their daily lives. Overall, the findings of our study in Boston are reassuring, as we found that while routine physical activity modestly increased exposure to select pollutants, it did not increase the harms of daily pollution exposure and in fact, reduced the apparent effects of NO2 on lung function.
A few studies have examined if long-term exercise habits modify the harmful effects of long-term exposure to pollution on cardiopulmonary health, based on the concern that exercise enhances the uptake of pollutants into the lung. These studies, largely conducted in Western Europe at relatively low pollution levels, have generally found that the benefits of exercise outweigh the harms of higher pollution exposure attributable to exercise.20,22 The Danish Diet, Cancer, and Health cohort of more than 50,000 adults with 16 years of follow-up examined whether baseline participation in sports and cycling moderated associations between pollution exposure and incident asthma and COPD.13 The authors found that while long-term NO2 exposure was associated with incident asthma and COPD hospitalization, physical activity reduced the risk of these outcomes, and there was no evidence of an interaction between physical activity and pollution exposure on COPD (or asthma) incidence. The authors concluded that the long-term benefits of exercise for respiratory health were not reversed by the harms of pollution exposure during exercise. Although this large population-level study in Denmark and our study favor physical activity despite the risks of pollution exposure, there are some key differences in methodology between the studies. The Danish Diet, Cancer and Health cohort study investigated long-term exposure over many years in the general population compared to our short-term study of daily exposure among COPD patients, as well as investigating the outcome of incident COPD hospitalizations rather than lung function. Taken together, our collective findings provide evidence in favor of greater physical activity for COPD patients, and for exercising in less polluted areas when possible.
Our study has several limitations. While we collected a large number of repeated measures (3314 observation days in total), our study only included 30 unique individuals in the Boston area. Therefore, our findings should be interpreted with caution given our small sample size and will require replication in larger cohorts with COPD. Our findings are limited in their generalizability to other patients with COPD, including those with milder diseases, those with and without asthma/COPD overlap, those with more vigorous exercise habits, or those living or exercising in more polluted urban environments or rural settings. Our study population consists only of former smokers and may not be generalizable to current smokers with COPD. While we were able to assess for personal exposures to air pollutants with the use of PAM and Fitbit devices, we did not measure device adherence (e.g., whether a participant left the home without the PAM or did not wear the Fitbit for part of the day), which may result in some misclassification of the personal pollutant exposure and step count estimates. However, such misclassification would likely result in a bias towards the null.
Our study also has several strengths. Our unique longitudinal study design with daily exposure and health measures allowed us to evaluate how day-to-day variability in step count and personal exposure to air pollutants is associated with daily lung function in an older population with COPD. We accounted for within-person correlation of measurements and adjusted for a robust list of potential individual-level and seasonal confounders. We used lightweight portable exposure monitors, calibrated to gold standard stationary monitors, to measure exposure at the individual level for a prolonged period (a total of 4 months) across different seasons. Our study demonstrates that measuring physical activity and personal pollution exposure using portable monitors is feasible for extended durations in a high-risk older population with COPD in order to address research questions about how typical exposures and activity levels affect respiratory health in the outpatient setting at an individual patient level. A recent American Thoracic Society workshop called for this type of research on the trade-offs of exercise and avoiding outdoor air pollution, especially for chronic medical conditions such as COPD that have known long-term health benefits of physical activity.23
In this study of former smokers with COPD living in an urban environment, routine physical activity resulted in only a modest difference in pollution exposure compared to sedentary behavior. Further, physical activity attenuated the negative association between personal exposure to NO2 and lung function in COPD. Our study did not find evidence to suggest that COPD patients should forego physical activity in order to avoid pollution exposure at typical daily exposure levels within current EPA standards.
Acknowledgements
Author contributions: MBR, KC, MA, AJS, LN, PK, and BAC planned the quantitative analyses for the study, which were carried out by KC and AJS. KC interpreted the findings, and KC, MA, and AP wrote the first manuscript draft. MBR supervised all aspects of the study, including data collection, analysis, interpretation, and manuscript preparation. All authors contributed to the critical revision of the manuscript and approved the final submitted version.
The authors thank the SPACE study participants for volunteering their time and effort; the research staff who assisted in this study, especially Wendy Sun, whose hard work and patience were integral to the success of this study.
Declaration of Interest
The authors have no potential conflicts of interest to declare.