Running Head: Acute Exacerbations of COPD and Thoughts on Death
Fundıng support: none
Date of Acceptance: April 25, 2023 │ Published Online Date: May 3, 2023
Abbrevıatıons: AECOPD=acute exacerbations of COPD; COPD=chronic obstructive pulmonary disease; COREQ=Consolidated Criteria for Reporting Qualitative Research; GOLD=Global initiative for chronic Obstructive Lung Disease; SABDs=short-acting bronchodilators
Citation: Ceyhan Y. The experiences of individuals with a history of acute exacerbations of COPD and their thoughts on death: empirical qualitative research. Chronic Obstr Pulm Dis. 2023; 10(3): 259-269. doi: http://doi.org/10.15326/jcopdf.2023.0389
Introduction
Chronic obstructive pulmonary disease (COPD) is a serious respiratory system disease characterized by airway obstruction. The thickening of mucus secretion in the airways and difficulty clearing the airways are important causes of the disease’s symptoms. The most common symptoms are dyspnea, cough, sputum, wheezing, and fatigue. However, exacerbations can occur when all of these symptoms suddenly worsen, and the patient requires immediate treatment. Acute exacerbations of chronic obstructive pulmonary disease (AECOPDs) refers to a clinical situation that occurs in COPD and causes severe respiratory distress. An AECOPD is typically caused by viruses, bacteria, environmental pollutants, or unknown factors. Some inflammatory processes begin in the airways during an AECOPD. The severity of dyspnea is greatly increased by hyperinflation and gas trapping, which are characterized by airflow limitation. It also leads to the aggravation of hypoxemia.1
COPD and AECOPDs have a significant place in the category of chronic diseases. Respiratory system diseases are the third leading cause of death from noncommunicable diseases worldwide, with COPD being the most common.1 AECOPD, the most severe complication of COPD, has been reported in more than 70% of patients within 3 years of diagnosis.2,3 It has also been reported that 47% of patients have 2 or more exacerbations per year at various levels of air restriction.4 The factors that cause AECOPDs are not fully understood today, and preventive measures are not effective enough. Therefore, the number of rehospitalizations and negative patient experiences is extremely high. While one-third of patients hospitalized urgently due to exacerbation were rehospitalized 3 months later due to recurrent exacerbation,5,6 this situation accounts for more than half of COPD hospitalization costs.7 The findings emphasize the significance of timely and effective treatment/patient care.
It is necessary to use patient experiences when planning patient treatment and care. The best expert is the one who has the illness. Therefore, early recognition of the patient’s symptoms, particularly in acute situations, allows for faster and more effective management of care. Studies on this subject mostly examined exacerbation experiences. 8-10 However, no study has been found that reveals patients’ experiences, feelings, and thoughts during an AECOPD and investigated the effects of this experience on their perspectives on death. This lack may lead clinical nurses to ignore patient experiences when planning patient care. To provide qualified patient care, it is essential to benefit from patient experiences, especially to know how the symptoms experienced by patients affect their mood and to apply patient-oriented care in this direction. For these reasons, this study aims to examine the experiences of individuals with a history of AECOPDs and the effect of this experience on their perspectives on death.
Methods
Study Design and Participants
The study used a phenomenological design, which is one of the qualitative research methods. The participants were AECOPD patients admitted to a training and research hospital’s pulmonology clinic ward. All patients were diagnosed with exacerbation by a pulmonologist. In addition, all patients had been diagnosed with COPD according to the forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) ratio < 70% criterion for at least one year.1 Participants were chosen using the homogeneous and criterion sampling method, one of the purposive sampling methods, between January and April 2022. The following were the study’s inclusion criteria: (1) being diagnosed with COPD by a pulmonologist for at least 1 year, (2) being in the chest diseases clinic for at least 3 days with the diagnosis of AECOPD, (3) not experiencing intense dyspnea that causes the inability to speak, (4) not having a speech impediment for any reason (such as hearing or speech impairment), (5) speaking the same language as the researcher, and (6) agreeing to participate in the study voluntarily. Exclusion criteria were defined as having a different chronic disease-causing severe shortness of breath (such as heart failure) and being hospitalized for less than 3 days.
The patients who met the inclusion criteria were interviewed until data saturation was reached or until a new topic was created. When different patients began to repeat similar concepts and expressions independently of each other, it was determined that data saturation had occurred, and the sample was terminated. A total of 27 patients (20 males, 7 females) were hospitalized during the study period. Among these patients, there were 19 who met the inclusion criteria. However, 4 patients did not want to participate in the study. As a result, the study was completed with 15 patients with a history of AECOPD.
Data Collection Tools
Data collection tools included a personal information form and a semi-structured interview form, created in line with the studies in the literature. 8-10 Pilot interviews with 2 patients were conducted to ensure that the study’s key questions and intended topics were adequately addressed. These interviews were not included in the study.
Personal Information Form: Questions about the participants’ age, gender, marital status, religious beliefs, and disease-related symptoms were included in this form.
Semi-Structured Interview Form: This form included open-ended questions to reveal the experiences of patients hospitalized for AECOPDs and their feelings about death. The questions on this form were as follows:
- How did you know you were having an AECOPD? Compared to your previous symptoms, how was the manifestation of AECOPD, its severity?
- Do you remember the moment of exacerbation? What did you experience at the time?
- How did you feel after the exacerbation, how would you describe its impact on your body and mind?
- How did this event (AECOPD) make you feel about death or life? Could you please explain?
- Did you associate this event with death? How did that feel for you? 8-10
Implementation of the Study
The study was conducted in the pulmonology clinic between July and September 2022. Before beginning the study, the purpose and content of the study were explained to the patients, and it was stated that participation in the study was voluntary. Meanwhile, it was ensured that the patients were alone in their rooms and that a quiet and calm environment was created. Patients were interviewed one-on-one and in-depth for the research project in the privacy of their rooms. The researcher conducted all of the interviews, which were recorded on a voice recorder with the patient’s permission. The questions were repeated, or the patient was asked to elaborate if they did not understand the question, or the researcher did not understand the patient’s response. At the end of the interviews, the patients and the interviewer reached a mutual agreement on the general aspects of the interview, and the interview was terminated if there was nothing to add. Each interview lasted approximately 45-60 minutes.
Evaluation of the Data
The data were evaluated using descriptive content analysis. To conduct a more systematic evaluation, Colaizzi’s phenomenological interpretation technique was used. 11 First, the audio recordings were transcribed by the researcher on the evening of the same day of the interview. After highlighting the meaningful sentences and expressions in the transcription, the patients’ messages were assessed. All records were analyzed in this way and patient statements were coded. The codes were then thematically classified. As a result, the codes yielded 4 themes and 11 sub-themes. The study was presented in accordance with the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist for qualitative research.12
Validity and Reliability of the Study
A semi-structured interview form was used during the interviews to increase the study’s validity, and the researcher refrained from using directive statements. To improve the study’s reliability, the data from the interviews were examined independently by 2 different researchers who were not involved in the study but had qualitative research experience, and the suitability between the codes and the themes was assessed. Patient statements were directly included in the findings to ensure external validity.
Ethical Considerations
Ethical permission (Decision No: 2022-10/102; Decision Date: 24.05.2022) was obtained from the Clinical Research Ethics Committee of Kirsehir Ahi Evran University to conduct the research. Ethical rules and principles of the Declaration of Helsinki were followed at every stage of the study. Before starting the interviews, the patients were informed that the interviews would be recorded, and their consent was obtained. They were also informed about their right to withdraw from the study at any time. The names of the participants were kept confidential throughout the study, and they were named Participant 1, 2, 3, and so on.
Results
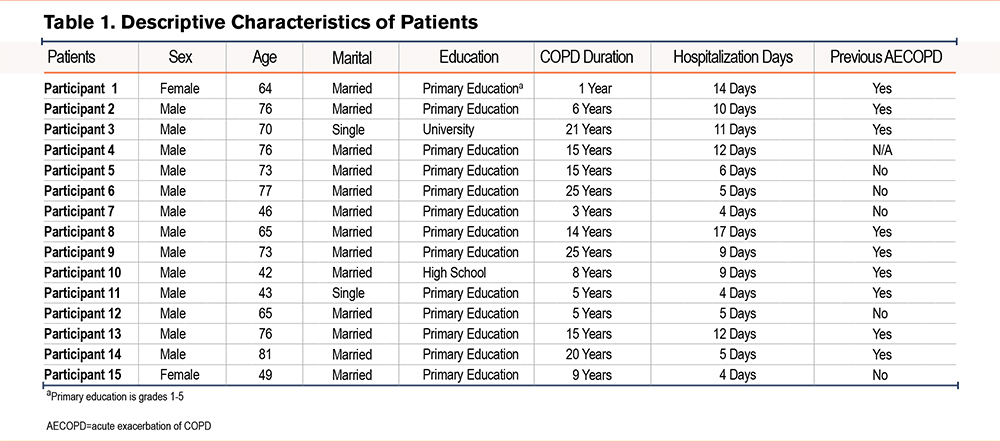
Table 1 shows the descriptive characteristics of the 15 COPD patients who participated in the study. The mean age of the participants was found to be 65.06±13.48 years, 86% of them were male and married. The mean COPD diagnosis duration was 12.47±7.89 years. All of the patients first visited the hospital’s emergency unit and were transferred from there to the chest diseases service. The mean of hospitalization days was determined as 8.47±4.13 as of the day the patients were recruited to the study (Table 1). In addition, it was observed that all patients experienced COPD symptoms such as dyspnea, cough, sputum, fatigue, sweating, and insomnia.
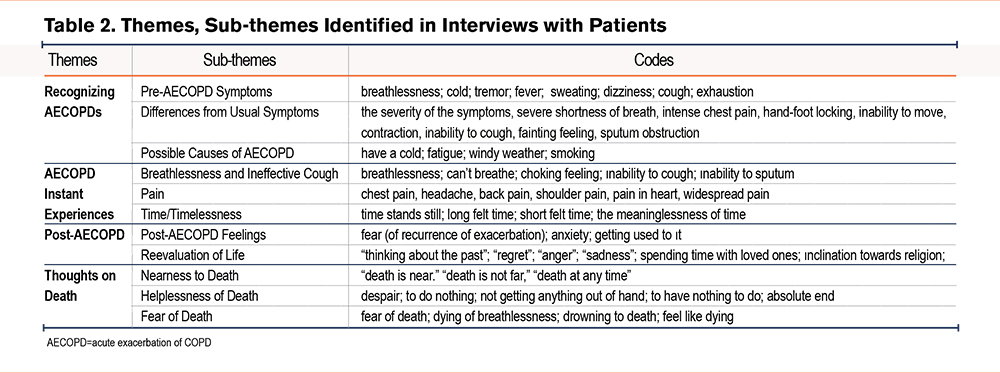
When the statements of the participants were coded, 4 main themes were identified: Recognizing AECOPD, AECOPD Instant Experiences, Post-AECOPD, and Thoughts on Death. Table 2 shows the sub-themes and codes that make up each theme.
Theme 1: Recognizing an Acute Exacerbation of COPD
In this theme, the patients described how their typical COPD symptoms got worse, how they felt at the time and any potential underlying factors that may have contributed to the development of an AECOPD. This theme’s sub-themes are pre-AECOPD symptoms, differences from usual symptoms, and possible causes of AECOPD.
Sub-theme 1—Pre-Acute Exacerbation of COPD Symptoms: General COPD symptoms were observed in this sub-theme derived from patient statements. Some patients described their symptoms as:
Participant 9: You’re having trouble breathing, your movements are becoming increasingly difficult, and you’re sweating. If you still can’t breathe, things will get worse. a couple of minutes, 3 minutes, 5 minutes... You will relax if you take medicine, breathe, and get over it (42 age, male).
Participant 13: It began with a cough. I was in a lot of pain because my cough didn’t stop. It gets worse when I’m out of breath; you can’t even speak when your windpipe is closed. The reason for this is an inability to throw phlegm (76 age, male).
Sub-theme 2—Difference from Usual Symptoms: The patients reported much more severe symptoms than they were used to with COPD. They stated that as the severity of their shortness of breath increased, their daily living activities were limited, and they were almost unable to move.
Participant 8: You have a hard cough, sputum comes out, and you will pass out if it does not come out. You’re becoming quite frail. You’re in excruciating pain all over your body. You understand what’s going on at the time, and if I’m physically capable, I’ll call an ambulance (65 age, male).
Participant 10: It’s like you can’t breathe. It’s not the same as shortness of breath. There’s also a cough, but it’s so bad you can’t cough (42 age, male).
Participant 11: I recognize it (AECOPD), you understand when it comes. For example, when you cough, you choke and sweat a lot. I feel as if I’m being paralyzed; I can’t walk, I can’t sit... I’ve been through it a lot before, so I realize that it will happen (43 age, male).
Sub-theme 3—Possible Causes of Acute Exacerbations of COPD: Most of the patients blamed themselves and stated that they paved the way for the emergence of an AECOPD. Some patient statements were as follows:
Participant 1: This is different, you get cold. Then you’re out of breath. First, I had a cold, then I got a fever and started vomiting, then the ambulance… (64 age, female).
Participant 6: If the weather is windy that day, it chokes me. I’m short of breath, I can’t breathe... (77 age, male).
Participant 13: What I regret is that… my reason is that I smoke. I started smoking when I was 16 and smoked for 50 years, and the doctor said don’t smoke, but I did... (76 age, male).
Participant 14: Caused by smoking. And that’s what happens when we get a cold on top of it (81 age, male).
Theme 2: Acute Exacerbation of COPD Instant Experiences
When asked if they remembered the AECOPD moment, 3 patients (Participants 2, 4, 7) said they felt they were about to have an exacerbation but couldn’t remember anything else and then fainted. Other patients were asked to recall as much as they could about their experiences at the time. The sub-themes identified from the patient statements were breathlessness and ineffective coughing, pain, and time/timelessness.
Sub-Theme 1—Breathlessness and Ineffective Cough: Most patients emphasized that the exacerbation, unlike the usual state of the disease, caused severe breathlessness and intensified cough, but they were not able to cough effectively enough.
Participant 9: I remember the moment of exacerbation. How could I not remember? Of course, I do. It starts like an asthma attack, shortness of breath hits hard, and you want to get rid of it as soon as possible. I do everything to save myself, to relax. If I’m lying down, I try to sit down or turn on my side, I’m constantly trying to catch my breath. I recognize when it will come, I try to take precautions. I try to get my air machine with me (73 age, male).
Participant 10: I was extremely tired, so I had shortness of breath. It was like I was out of breath; I couldn’t breathe. I tried to cough, but I couldn’t... At that moment, my hands and feet went numb, I couldn’t get up from my seat, drink water, or come to my senses. They washed my face. Although it felt a little better, my shortness of breath continued, and I could not swallow (42 age, male).
Participant 14: I was so smothered, so smothered that I gasped… It was like someone was suffocating me and choking my throat like this, squeezing this place like this (showing their throat with their hands) (81 age, male).
Sub-theme 2—Pain: The majority of patients reported severe pain as a result of the exacerbation. They described that they felt the pain, especially in the chest and back, and that it took their breath away. Some patient statements describing this situation were as follows:
Participant 1: I had a lot of pain. My chest was such a pain… the pain was all over me. Then it felt like needles were pricking me all over me (64 age, female).
Participant 5: Painful, too much… Painful as if you have a fever all over you (73 age, female).
Participant 7: I felt the exacerbation. My chest hurt, and my shoulders hurt, especially my left shoulder (46 age, male).
Participant 8: Exacerbation comes with pain. The pain started in my head. At that time, there was dense sputum, the pain increased as I tried to remove it. It started in my head and spread to my chest and back. When the pain comes from the heart, then you think that your world is just breath... (65 age, male).
Sub-theme 3—Time/Timelessness: Patients were asked to describe the concept of time they felt at the time of exacerbation. While some patients reported that the exacerbation was short-lived, others stated that it took quite a long time. In addition, some patients stated they were unaware of the time.
Participant 1: When it (the AECOPD) starts, even a second seems to take an hour or 2 hours. It’s like time stands still when you feel a tightness in your chest and start to tremble… (64 age, female).
Participant 2: At that moment, hours may have passed or not… I’ve experienced it (an AECOPD) twice, and both were like this, it was as if time did not exist (76 age, male).
Participant 7: Everything happened in an instant (46 age, male).
Participant 8: It took maybe 10-20 minutes. You don’t know how much time it takes when you’re living it (65 age, male).
Participant 14: It takes a long time. An hour, sometimes 2 hours… After 2 hours, when you sit down and lie on your back, you can relax a little (81 age, male).
Theme 3: Post-Acute Exacerbation of COPD
The patients were asked about the emotions they felt intensely after the exacerbation when they started to feel better. The sub-themes were formed according to the patient statements: post-AECOPD feelings and reevaluation of life.
Sub-theme 1—Post-Acute Exacerbation of COPD Feelings: The common emotion of all patients who survived an exacerbation was fear. On the other hand, some patients stated that they got used to it, saw it as a part of the disease, and even felt relieved after the exacerbation.
Participant 1: When I regained myself and relaxed a bit, it was as if a fire was still burning inside me. Frankly, this scared me (64 age, female).
Participant 2: I felt relieved when I calmed down a bit. I didn’t know what to do after that (76 age, male).
Participant 5: I don’t know what I exactly felt. I had pain. The doctors and nurses asked if my pain was gone. I realized when they asked that my pain had eased a little (73 age, male).
Participant 6: When I came to myself, I thanked God. I was relieved that I got over it for that time (77 age, male).
Participant 8: I said to myself that I was dealing with the same thing again (exacerbation). It is incredibly difficult to go through it again, and unsettling to wait for it to happen without knowing when it will (65 age, male).
Participant 10: This time, what I went through was very serious. I’ve had it before, but never like this. The previous time, once I recovered, I was able to carry out my daily tasks. This time, it was very frightening. I panicked so much. My wife called an ambulance, which took nearly 30 minutes to arrive. Far from being relieved, I recall being afraid that I would have to go through it (the AECOPD) again (42 age, male).
Sub-theme 2—Re-evaluation of Life: Some patients stated that AECOPDs had caused them to reconsider their regrets, anger, or sacrifices in their lives.
Participant 1: After this incident, there was a desire in me to do more good to people. I went to the Kaaba last year. I was hospitalized there 3 times, but not this bad. That’s why I want to pray constantly and thank God. I regret it so much when I can’t. I also regret that I haven’t done this much before (64 age, female).
Participant 2: I used to smoke and spent a lot of time in coffee houses (smoky environment). At that time, indoor smoking was allowed, so I got sick because of it (in anger). I had already quit smoking, but after the exacerbation, I did not let anyone smoke at my home or even near me. I started to pay more attention to my health and to have more frequent doctor check-ups (76 age, male).
Participant 7: How could I feel, of course, I was sad. I thought of my friends, I thought of what we did. I wish I had done even better things. I would like to have done more good and helped people more (46 age, male).
Participant 8: I thought a lot about my family, I didn’t think about anyone else. I wish I had spent more time with them. I’ll spend more time with them after this, but I had a brother and he’s gone (died)… There’s nothing I can do to spend time with him anymore (65 age, male).
Participant 10: Actually, I was not a good person who did a lot of good deeds. I have too many shortcomings. But, from now on, I will try to do my best. Even if I have a little or a trillion, I will use them all for good. The important thing is not material, but the willingness to do good (42 age, male).
Participant 13: It turns out that I bought my disease with my money. I paid for this sickness. It took my money and left me with this illness. I’m lying down here, it’s all because of smoking. Look, I’m out of breath now. If I had known, I would never have done it, and I will warn those who do not pay attention to it as much as I can from now on (76 age, male).
Theme 4: Thoughts on Death
It was revealed that AECOPDs, which necessitate inpatient care and cause severe respiratory distress, give rise to thoughts of death in many patients. While some patients described it as full of fear, some patients thought that death was an expected situation and the expected end had come. The sub-themes were formed according to the patients’ statements: nearness to death, helplessness of death, and fear of death.
Sub-theme 1—Nearness to Death: Many patients stated that they thought they were on the verge of death because of the severe symptoms they experienced during an AECOPD. Some patients, in particular, stated that they believed death was inevitable if an AECOPD recurred.
Participant 7: After getting sick, I started to think about death from time to time. Of course, when people get sick, they wonder if they are going to die. Especially this situation (an AECOPD) made me feel that death was very close (46 age, male).
Participant 8: We live for the moment. This disease will take my life eventually. Whether it’s today or tomorrow, it’s not too far away anymore (65 age, male).
Participant 9: I am always ready to die. I am not afraid of death. Just as we were born, we will eventually die. That’s it. Therefore, we should adapt ourselves, we should prepare for death, and if we have such a disease, we should know that death is always near (73 age, male).
Sub-theme 2—Helplessness of Death: Most of the patients stated that they could do nothing to prevent or delay death even though they saw death as a situation that they would experience eventually.
Participant 2: I thought about my life, my whole life flashed before my eyes, as they say. No one thinks about death, but I thought about it. Then I got scared, who wouldn’t… Feeling death was something else. When I regained a bit of relief after the exacerbation, I said oh, thank God I didn’t die, I was very happy about that (76 age, male).
Participant 8: Either take my life or save me from this disease (he prayed to Allah). I can’t do anything but… I wanted to die and get rid of it. God gives us life and then takes it away; I can’t do anything against death. My brother also had this disease, and now I do. There was nothing we could do for him, we couldn’t do anything, he died, it’s my turn... (65 age, male).
Participant 11: I lived alone, there was no one. Well, I said, there’s nothing you can do if you die like this. There is always death anyway, so you have to die, is there a cure for death? No, there is not (43 age, male).
Sub-theme 3—Fear of Death: Some patients emphasized that death would come eventually, so that fear was meaningless. However, many patients seriously fear death because of COPD and AECOPDs. In particular, the increase in the severity of the symptoms causes patients to feel it more intensely. Some striking patient statements were as follows:
Participant 1: I was scared. I was terrified. I felt like, I mean, I thought I was dead… My whole body was shivering. There was no line between death and life, it was as if death arrived when I had an exacerbation (64 age, female).
Participant 3: Sometimes death comes with struggle, you know, people die struggling. That’s how our lack of oxygen makes us struggle. I’m so afraid to die struggling, but our disease, COPD, causes it. I always pray to God to give me a comfortable death (70 age, male).
Participant 10: You can’t breathe during an exacerbation, it’s like you’re suffocating, I’m so afraid that I’m going to suffocate and die. Anyone who says they are not afraid is lying. There is a very thin line between death and life, I am one of those who feel it the most. Our chances of dying are very high, you’re gone when you’re short of breath… that’s what I’m so afraid of (42 age, male).
Discussion
This study investigated the experiences of COPD patients who were hospitalized for AECOPDs in the chest diseases service and the effect of these experiences on their idea of death by using a phenomenological method. The majority of the patients who participated in the study were male. Considering the impact of COPD on gender, it has been reported to impact predominantly the male population. In the most comprehensive gender-specific systematic review and meta-analysis study, it was revealed that the prevalence of COPD in men was higher than in women and this difference was more pronounced especially in patients over 70 years of age.13 Similarly in Turkey, in the number of patients affected by COPD as officially announced by the Ministry of Health, 14,195 of the total 21,828 patients in 2021 are male and 7633 are female.14 This reveals that men suffer from COPD about twice as much as women. As age increases, the number of affected male patients increases as well. Our study group was similar to the literature in that most of the patients with COPD who were both hospitalized and who could be included in the study were male and over 65 years of age.
Recognizing an AECOPD was determined as the first theme of this study. It turned out that the patients were able to distinguish the AECOPD symptoms from the usual symptoms. The causes of an AECOPD in general and what happened prior to the exacerbation were identified. Accordingly, it was found that symptoms such as shortness of breath, cough, sputum, and sweating intensified before an AECOPD. A COPD exacerbation is a severe crisis that comes with extremely intense symptoms. The Global initiative for chronic Obstructive Lung Disease (GOLD)1 guidelines classify an exacerbation as mild if treated with short-acting bronchodilators (SABDs) only, moderate if treated with SABDs plus antibiotics or oral corticosteroids, and severe if requiring hospitalization or emergency department treatment. 1 According to different guidelines, having 2 major (dyspnea, sputum) or 1 major and 1 minor (wheezing, cough, chills) symptom for 2 days or longer is diagnosed as mild/moderate exacerbation.15,16 The symptoms are quite severe during an exacerbation. It is critical for patients to correctly identify the exacerbation and seek treatment as soon as possible. In their COPDPredictTM study in 2021, Patel et al discussed the significance of the knowledge gained from the experience of those who have the disease, with an emphasis on “experts by experience.”17 Nine patients with a history of exacerbations reported that their prior experiences helped them better define subsequent exacerbations. Pepin et al (2022) emphasized the importance of detecting COPD exacerbations early in their study and the importance of patient follow-up in this regard.18 One of the patients in Chin’s study stated that they could predict an exacerbation with the phrase “I knew something was coming.”19 In line with the literature, the majority of patients in our study stated that they were aware of the exacerbation symptoms beforehand.
Knowing the factors that cause exacerbations is as important as recognizing the exacerbation. Protecting oneself from these factors can prevent a possible exacerbation. Wu et al (2021) reported in their study that factors such as pollution, temperature, or circulating viruses can cause exacerbations. This coincides with the fact that the patients in our study also stated that they experienced exacerbations due to bad weather conditions, chills, and fatigue.20 Most of the patients in Chin’s study (2021) expressed prodromal symptoms before exacerbation as cold symptoms and fatigue. In particular, one patient stated that “I had absolutely no energy. I was so worn out. I didn’t want to go out, visit my friends, or even eat my meals.”19 These findings support the findings of this study. It has shown that the patients were aware of the conditions that caused the exacerbation and were able to distinguish the exacerbation from the usual symptoms.
“AECOPD Instant Experiences,” the second theme of the study, was associated with the sub-themes of breathlessness, cough, pain, and timelessness. In particular, increased mucus and ineffective cough cause dyspnea to be exacerbated. In the GOLD 2022 report, it was emphasized that the increase in cough and sputum purulence should be monitored for exacerbations.1 In their study in 2022, Hughes et al stated that patients with productive cough are likely to have more than one exacerbation in a year.21 In a systematic review published by Tsiligianni and Kocks in 2020, it was reported that cough, sputum, and dyspnea symptoms of patients worsened especially in the morning hours, and intensified at the time of exacerbation.22 Parallel to these results, it was observed in this study that all of the patients were coughing, they were unable to produce sputum as a result of ineffective coughing, and this led to exacerbation, so the findings of this study were also consistent with the literature.
Pain is an expected symptom during a COPD exacerbation. The feeling of tightness in the chest increases with dyspnea. In this study, the patients complained of headaches and pain caused by chest tightness. Jorgensen et al (2021), in their qualitative study, included a patient’s statement describing chest pain (“It is as if there is an iron ring across my chest”) and obtained similar results to this study.9 Both female patients in our study complained of intense pain at the time of exacerbation. Although men also reported experiencing pain, the fact that women have a lower pain threshold and higher pain sensitivity than men results in them being more susceptible to this condition. Studies have reported that women are more affected by pain at many points.23
The third theme of the study, “Post-AECOPD,” was obtained from the findings in which patients described how they felt after an AECOPD and their reevaluation of life. The patients were most afraid of the recurrence of exacerbation. Giacomini et al (2012) stated in their study that the patients attributed the fear of recurrence to environmental conditions or infections, not the progression of the disease.24 Rosa et al (2018), on the other hand, reported in their study that the patients did not feel safe at home after an exacerbation, they felt safe only while receiving health care in the hospital, and therefore, they were uneasy about a possible re-exacerbation.10 Hughes et al (2022), on the other hand, associated the patients’ fear of exacerbation with the increased frequency of coughing.21 The fact that the patients in this study also suffered from cough and experienced exacerbations more than once affected their thoughts after an exacerbation. In addition, the fatalistic approach of the patients in this study impacted their evaluation of the disease and its symptoms.
“Thoughts on Death,” the fourth theme of the study, was obtained from the sub-themes of nearness to death, helplessness of death, and fear of death. Although some of the patients associated the disease with fatalism, it was observed that the fear of death was still intense. Revealing patients’ thoughts about death is the most important part of physical and psychosocial care. Rosa et al (2018) emphasized that nurses play a key role in physical and psychological support.10 Nurses have the opportunity to communicate and provide appropriate care to reveal the fears and concerns of patients. The fear of death is expected to be felt at a high level in COPD exacerbation.25,26 In a study investigating the fear of death in COPD patients, it was reported that of the patients had a fear of death.27 In another study, it was shown that 64% of patients were afraid of death at the time of exacerbation.19 Most of the patients emphasized “on the last day” and a patient said, “I honestly thought it was going to be my last day. Nobody wants it to be their last day.” On the other hand, a patient in Chang’s study in 2016 expressed his fear of death with these words: “couldn’t breathe . . . It was just like my neck was squeezed . . . I was afraid that my heart might stop beating . . . I needed oxygen right away.”8 When gender-specific perceptions of death are examined, it is observed that the women in our study again have a high fear of death. The metaphor of comparing exacerbation to the moment of death is striking. This was associated with women's persistent severe and prolonged pain both at the time of exacerbation and after. All these results indicate that it is expected that patients with COPD fear death, especially at the time of exacerbation.
It was observed that patients’ thoughts about death may be related to previous exacerbation experiences. In the overall theme of death-related thoughts and especially in the sub-theme of fear of death, all of the patients who established a closer relationship between exacerbation and fear of death were those who had previously experienced an AECOPD. This situation leads to a higher level of fear and panic in patients who experience re-exacerbation compared to patients who experience it for the first time. It is crucial to consider patient experiences in clinical care and to provide holistic care by considering the physiological and psychological effects of exacerbations.
Conclusion
Patients hospitalized in the chest diseases service due to an AECOPD were found to be able to recognize the AECOPD and distinguish it from other symptoms. Shortness of breath was the most common symptom reported by patients. In almost every patient’s statement, they mentioned shortness of breath and the difficulties it causes. The ineffective cough and inability to produce sputum were then identified as other significant factors in exacerbation. Patients expressed mostly negative emotions about their experiences during and after the AECOPD. The most significant effect of these negative emotions was determined to be the strengthening of the thought of death. Many of the patients who had an AECOPD said that this experience was similar to death and that they expected to die this way one day. However, many patients sadly emphasized that this situation caused a fearful wait. Therefore, it is extremely crucial for nurses and physicians, who have an important role in patient treatment and care, to closely evaluate patients diagnosed with COPD, to intervene to prevent possible causes of an AECOPD and to provide emergency support during the AECOPD. At this time, the emotional state of the patient between life and death and the effect of this feeling on the desire to be treated should be taken into consideration.
Acknowledgements
Author contributions: YC was responsible for the conception and design of the study, acquisition of the data, data analysis and interpretation, and writing the article and revising it prior to submission. The author takes responsibility for the integrity of the data and the accuracy of the data analysis.
I would like to thank the physicians and nurses of the pulmonology clinic, as well as the patients who provided support in the conduct of the study. In addition, I would like to express my gratitude to Associate Professpr Gökçe Demir, PhD, and Associate Professor Sevil Güler, PhD, for their contributions in the analysis part of the study.
Declaration of Interest
The author has no conflicts of interest to declare.