Running Head: Home-Based Pulmonary Rehab with Health Coaching for COPD
Funding Support: National Institutes of Health Grants# R01 HL140486, K24HL138150. Clinical Trial Registration: NCT03480386. The sponsor had no role in the study's design, the collection and analysis of the data, or the preparation of the manuscript.
Date of Acceptance: April 17, 2023 │ Published Online Date: May 3, 2023
Abbreviations: COM-B=Capability, Opportunity, Motivation–Behavior model; COPD=chronic obstructive pulmonary disease; COVID-19=coronavirus disease 2019; ED=emergency department; FEV %pred=forced expiratory volume in 1 second percentage predicted; MI=motivational interviewing; mMRC=modified Medical Research Council; PR=pulmonary rehabilitation; QoL=quality of life
Citation: Midthun WR, Benzo MV, Ridgeway JL, Benzo RP. Understanding the patient experience of home-based pulmonary rehabilitation with health coaching for COPD: a qualitative interview study. Chronic Obstr Pulm Dis. 2023; 10(3): 224-233. doi: http://doi.org/10.15326/jcopdf.2022.0384
Online Supplemental Material: Read Online Supplemental Material (212KB)
Introduction
Chronic obstructive pulmonary disease (COPD) is a prevalent lung condition in the United States resulting in 15.4 million physician visits, 1.5 million emergency department (ED) visits, and 726,000 hospitalizations each year. 1 Pulmonary rehabilitation (PR) has proven to be an effective means of improving the quality of life (QoL) and management of symptoms for patients living with COPD.2,3 However, adherence to these programs remains low.4 Traditional PR programs involve leaving one’s home and traveling to a wellness facility: attending center-based PR programs can be especially challenging.
Home-based programs have been proposed as an alternative for individuals that cannot participate in traditional programs,4-6 and have proved to be feasible, effective, and possibly non-inferior to center-based PR.7-9 However, the remote nature of these home-based programs may limit social interactions that are related to the modeling aspect of behavioral change.
This group initially reported the feasibility and effect size of a home-based PR program that significantly improved the QoL and the self-management abilities of people with moderate to severe COPD.10 A larger confirmatory study testing an updated home-based rehabilitation program, which included telephonic health coaching and remote monitoring of the activity-based program, showed significant improvement in patients' breathlessness, disease-specific QoL, measured daily physical activity, sleep, self-management, and depression-related symptoms.7
A deeper understanding of how patients experience health behavior change interventions—especially complex, multi-component programs—is needed to untangle how diverse patients interact with programs and the factors related to behavior change. While previous qualitative research has provided insights into patient satisfaction with home-based programs,11 this study not only provides insights on the patient experience but also uses a theory-based approach to understanding ways in which this specific home PR program —found to be effective in the largest home PR trial in the United States —was experienced by individual patients.12,13
Methods
Setting and Intervention
The parent trial was conducted with adult patients with a diagnosis of COPD who received care at an academic medical center and a community health system in the upper Midwest.7 The home-based PR program included 3 key components and was conducted over 12 weeks:
- Three daily mindfulness-based exercise practices guided by a recording on a computer tablet: two slow 6-minute walking (or balance) practices, and an upper extremity flexibility practice that could be completed either seated or standing;
- Remote monitoring using an activity monitor, an oximeter, and a computer tablet for comunication, exercise practices to follow, and reports on steps, and patient-reported outcomes and accountability of daily exercises; and
- Weekly telephonic health coaching with a health coach trained in motivational interviewing (MI) and mindfulness. The health coaching sessions specifically included mindfulness by cultivating the coach's ability to be present in the moment of coaching and to listen intently.
Interview Recruitment
Trial participants were eligible to participate in an individual interview about their experience if they completed the 12-week PR intervention and completed post-intervention measurements (filling out questionnaires and wearing an activity monitor) within the prior 12 months. Eligible participants were sent a letter and asked to contact study staff to express their interest in participating. Participants were provided $40 remuneration after the interview.
Data Collection
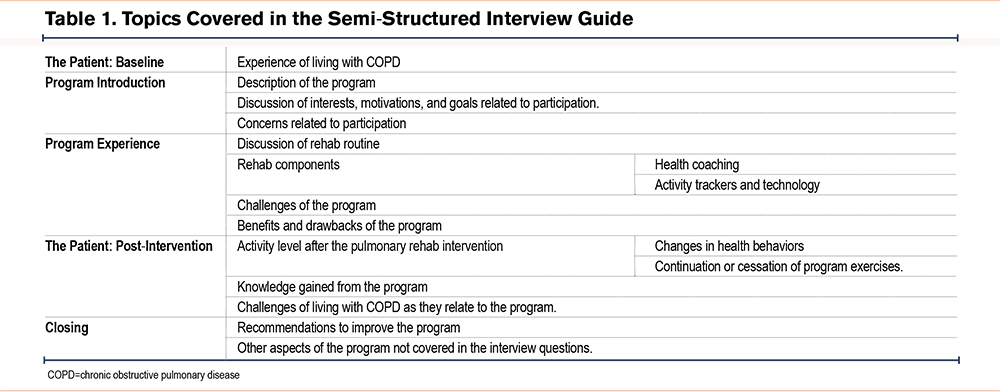
Interviews were conducted via telephone by members of the study team unaffiliated with the parent program delivery (JLR and WM) using a semi-structured interview guide developed to elicit information about motivations for participation, program experience (including the various components of the program), expected benefits or concerns, and recommendations for improvements (see Table 1 for topics and Supplementary file A in the online supplement for the full interview guide). The study team met weekly during data collection to discuss impressions and inform any necessary changes to the interview guide or sampling approach. Weekly reflections were also used to decide whether adequate interviews had been conducted to answer the research question (i.e., a high degree of data redundancy with each new interview), such that recruitment and data collection could stop. This study was approved by the Mayo Clinic Institutional Review Board (17-009449).
Data Analysis
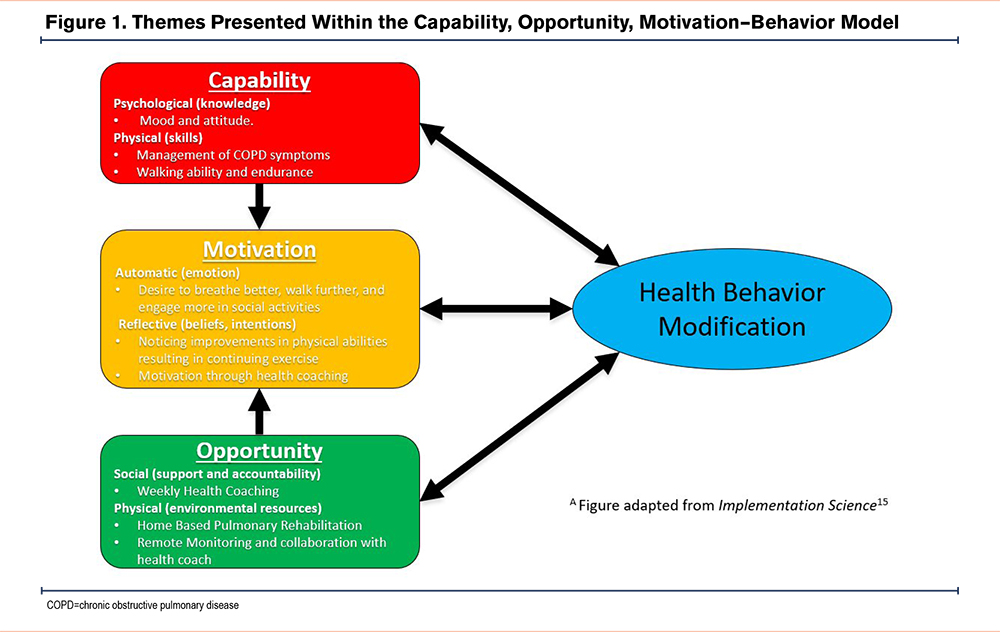
Interviews were transcribed, de-identified, and reviewed for accuracy. Data analysis followed an inductive thematic approach to coding followed by categorization and interpretation using the Capability, Opportunity, Motivation–Behavior (COM-B) model, which was developed to provide a framework for connecting program functions to aspects of individual behavior change.14 The COM-B model proposes that behavior, in this case, completion of home-based PR, is the result of an interaction between a person’s capability (knowledge or skills), opportunity (societal influences or environmental resources), and motivation (emotion or beliefs and intentions).15 This model was selected for its potential to understand how patients with varying social and health contexts experienced a home-based intervention with both technical and social components. In doing so, it identified ways the program can be used or improved to affect change. The COM-B model posits that behavior change is a result of an interaction between 3 components: psychological (knowledge) or physical (skills) capabilities; social (social support) or physical (environmental resources) opportunities; and automatic (emotion) or reflective (beliefs, intentions) motivation. A team of 4 investigators reviewed 4 transcripts to identify topics and created a coding framework and codebook with definitions and examples. The coding framework was independently applied to transcripts, coding was resolved through discussion, and transcripts were entered into qualitative analysis software (NVivo Release 1.0, QSR International) to assist with organization and analysis. Two investigators reviewed coding summaries and wrote analytic memos. Interpretation of findings was organized around the COM-B model.15
Results
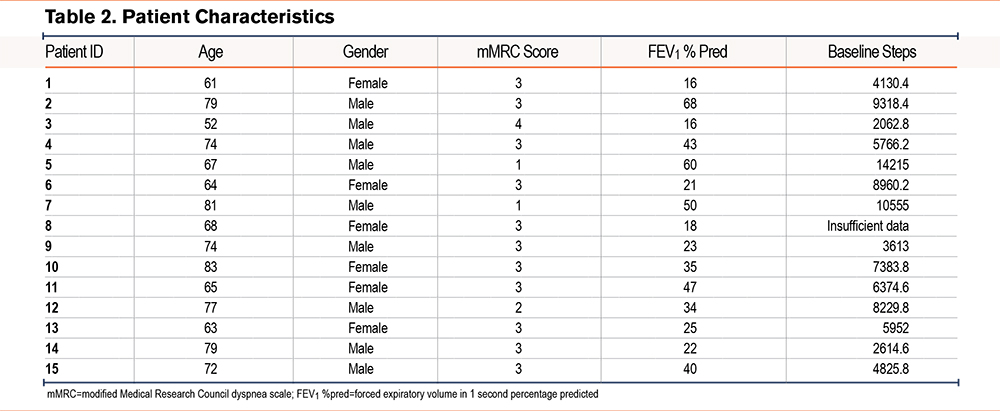
Thirty-two eligible trial participants were approached to participate, and between October 19, 2021, and January 13, 2022, 15 individuals consented and completed interviews. The mean duration was 46 minutes (range 24 to 84 minutes). Patient characteristics are shown in Table 2. Participants differed in COPD severity and daily activity, with daily steps ranging from 1062 to 14,215. At the time of their participation in the program, none of the patients were active smokers. Participants also varied in their places of residence (some lived in private homes while others lived in assisted living facilities) and working status (most patients were retired).
Qualitative findings are summarized below and in Figure 1 by constructs in the COM-B model. Table 3 provides additional exemplar quotations from participants by constructs in the model. Results are focused on the 3 aspects (capability [C], opportunity [O], and motivation [M]) that impact behavior change, in this case, engagement with the PR intervention. Recommendations for program improvement are also summarized below.
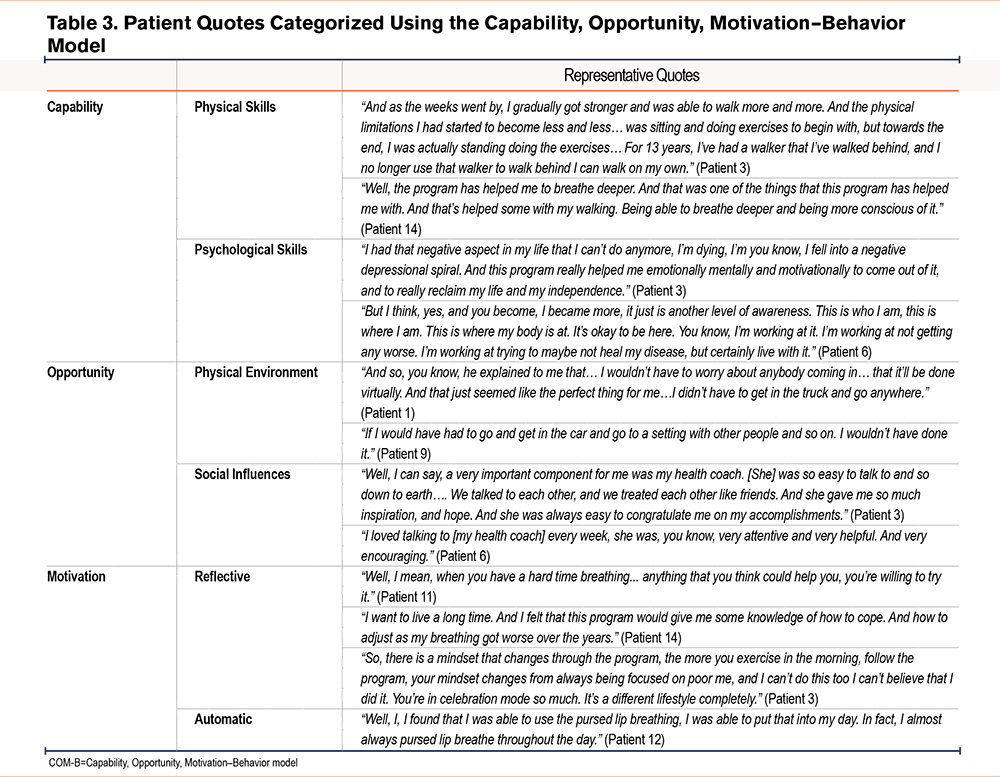
Capability
The analysis identified physical and psychological capabilities relevant to starting and continuing the program. Several reported having tried other rehabilitation programs in the past with mixed results. There were differences in how capable participants said they felt about doing the activities described to them, including the breathing exercises and walking exercises. Some reported feeling confident and described the program as "doable." As described by one patient who was using a wheelchair at the time of enrollment:
"When he told me I could do a 6-minute walk, and it was like a snail, I thought, I can do that…. I was so excited to just find a way to start moving again." (Patient 6).
Other patients had concerns about starting the program and being able to do the exercises because of their breathing issues. Those patients reported mostly sedentary lives due to shortness of breath, limited energy, and fears of exacerbations at enrollment. For patients concerned about the challenges of participating, some noted the possibility for improvement in their QoL as a reason to join despite reservations. In both cases, participants described study staff providing information about the exercises and the reasons they were developed specifically to support people with COPD. That knowledge helped engage participants whether they found the program doable or challenging.
Patients also described improved moods and attitudes. For example, before beginning the program, one patient explained:
"I fell into a negative depressional spiral. And this program really helped me emotionally, mentally, and motivationally to come out of it, and to really reclaim my life and my independence" (Patient 3).
Many patients also reported approaching exercise and a healthy lifestyle with a positive mindset following the program. That combination of improved physical and psychological capacity impacted motivation to continue, especially among patients for whom the goal for participating was to feel and breathe better.
Both physical and psychological capabilities were reported as being supported by the health coach. Participants reported the impact of health coaching on their confidence to do the exercises and adapt exercises to meet their needs. The following patient (Patient 3), who reported being severely depressed and experiencing panic attacks due to fear of COPD exacerbations when she entered the program, described in the interview how the personal health coaching approach made her feel empowered:
"And so, I'd have to say she [my health coach] was a very large influence. And she was very powerful in helping me to help myself. She empowered me. She's a great person."
Opportunity
There were both physical and social aspects of opportunity described by participants in this study. Most notably, patients reported being excited about doing a PR program from the comfort of their homes. One patient described their home as a "comfort zone" because of their physical limitations and the threat of a COVID infection. She would only leave her home to attend doctors' appointments and pick up medications from a pharmacy. This patient stated:
"And so, you know, he explained to me that… I wouldn't have to worry about anybody coming in… it'll be done virtually. And that just seemed like the perfect thing for me… I didn't have to get in the truck and go anywhere" (Patient 1).
Another patient recalled being unable to attend PR in person because of their work schedule. Given that the program was remote and asynchronous, patients could vary the time of day and the number of times exercises were completed. Patients collaborated with their health coach to discover a personalized approach to the program that worked best for them. Additionally, many patients commented that they were pleased to discover the opportunity to do the program on their own time and at their own pace (i.e., able to take breaks when/if needed). For example, one interviewee lived in a large, assisted living facility and used the long hallways for the walking practice. Another patient reported:
"I have a very large railing around … the Living Center. So, I could hit the pause button on the tablet and take a break" (Patient 3).
Other patients lived in private residences that varied in how suitable they were for walking practice due to space limitations.
The interviews provided insight into how participants relied on their health coach. When asked about their health coach, one patient stated:
"It's hard to make yourself get out and do exercises when you're alone. If you've got somebody doing them with you, [it's] a lot easier" (Patient 1).
Many patients appreciated the check-in with their health coach. They found their health coach very respectful, enjoyed their conversations, and valued their bond and partnership. For example, one patient stated:
"I loved talking to [my health coach] every week. She was, you know, very attentive and very helpful. And very encouraging" (Patient 6).
Several patients mentioned that they felt emotionally empowered to invest time in their self-care and daily physical activity, which gave them hope and a sense of gratitude. Specifically, there were reports that the program gave them hope for themselves and their condition.
Motivation
A common motivation described by participants was a desire to improve physical health and daily physical activity. When reflecting on living with COPD, one patient stated:
"Well, I mean, when you have a hard time breathing…anything that you think could help you, you're willing to try it" (Patient 11).
Additional comments regarding patient motivations included wanting to breathe better, do things without losing their breath, and engage more in social activities, such as spending time with family and friends. Additionally, many patients expressed goals and expectations to improve endurance, strength, and walking distance. Even when expectations for outcomes were low, some patients thought that adding lower-intensity exercise to their day would not hurt and could help. Those who started and kept up the routine for a few weeks found the program was easier than anticipated, and they could create a daily routine to complete their practice.
Similarly, at the beginning of the exercise program, some patients found it hard to complete the exercises; they experienced sore muscles and had to take breaks. However, after sticking with it, they noticed improvements in their walking endurance and breathing. For example, one patient who identified as incredibly limited, was too breathless to leave the house, and experienced panic attacks over fears of feeling shortness of breath before the program explained that:
"As the weeks went by, I gradually got stronger and was able to walk more and more. And the physical limitations I had started to become less and less… was sitting and doing exercises, to begin with, but towards the end, I was actually standing doing the exercises… for 13 years, I've had a walker that I've walked behind, and I no longer use that walker to walk. I can walk on my own." (Patient 3).
Another patient who had to retire from his job due to failing an employment-related health physical found himself leading an inactive lifestyle. However, after beginning the program, he stated:
"It was really a good experience because it kept me in a routine every day" (Patient 4).
Patients also reflected on improvements during the program, which served as motivation to continue. One patient reported returning to everyday activities, such as making the bed, cleaning, and cooking, that they could not do before the program. She commented that these improvements:
"…allowed me to find success in very small places. And that made me feel good about myself. And when I felt better about myself, I think I had better hope for things to come," which led to the comment "I was pretty motivated to keep that going" (Patient 6).
Patients referred to an overall sense of improvement in their exercise capacity, mainly walking more and breathing better while performing daily activities. Patients clearly stated that the program motivated them to stay active in their daily routines. Many patients mentioned that benefits appeared with long-term practice. One patient who, at baseline, was only able to take 20 steps before needing to pause and catch their breath reported:
"The longer I was doing it, the better I was feeling. You know, it isn't a quick fix… it takes weeks before you start noticing a difference," (Patient 2).
However, after sticking with the program, this patient reported being able to do yard work and take what he described as "long walks" outdoors.
Patients reported that they found their health coach to be a good motivator and helped encourage them to continue with the program. The coach monitored their progress and helped them progress toward their step goal. Many patients also reported that their health coach held them accountable during the 12-week program. When reflecting on their program experience, one patient mentioned:
"the accountability of having the check-in record and then checking in with the rehab coach weekly like that, I think that makes a huge difference… I know it would benefit me, and I feel like it would benefit others as well" (Patient 13).
Recommendations for Program Improvement
Although most patients reported satisfaction with the exercises, especially their capacity to complete them despite physical challenges, a few patients found the program too easy or monotonous and suggested adding variations to the exercises. For example, one patient who began the program with an average of 6374 steps per day explained that she:
"found the exercising to be very boring. It's just not anything that would challenge you, wasn't enough variety to it. So, I just kind of lost interest in that," (Patient 11).
Other patients mentioned that having more exercise options with some moderate-intensity exercise would have been beneficial for them. Also, although the majority found the interactions with their health coach beneficial, a small minority found this partnership less valuable, described it as just another thing to do in the program, and recommended health coaching as an optional component.
Some patients also reported wanting an improved transition after the program, e.g., the possibility of monthly check-ins with the coach for accountability and keeping the tablet to continue with their exercise routine. Although YouTube links to the videos and DVDs are an option, one patient recommended a physical copy of the exercises or even the ability to purchase the tablet or an app with the program on it. Several patients stated that they wanted to keep the tablet after the 12-week intervention and were willing to pay for it, as they felt they needed it to continue doing the exercises, suggesting a feedback loop with perceived capabilities around sustained behavior change. One patient explained that he "struggled" to continue practicing the program exercises after returning the tablet. He explained:
"yeah, I would have bought it… If I had the tablet, if I had the visual in front of me. And tablet in front of me. I would go back to doing those exercises" (Patient 5).
This patient suggests that the continuation of the program exercises could have been aided by post-program interaction with the computer tablet.
Discussion
This qualitative study provides insights into how patients who completed a home-based PR program experienced it, including reasons for participation and ways that features of the program and behavioral aspects of participation intersected. While all patients completed the program, they varied in several key characteristics potentially related to behavior change, including their physical and emotional readiness at enrollment. Previous research has found patients to express concern about "starting out" and their ability to begin PR after living a rather sedentary lifestyle.11,16 We found that knowledge about what to expect in the program, the realization of physical or emotional benefits during participation, and continued motivational support during the program were key to patients’ initial and ongoing involvement in the program.
The health coaching component was key in how participants experienced behavior change. One likely factor for the positive impact of the health coach on the patient experience of PR stems from the use of motivational interviewing,11,17 which promotes autonomy. Specifically, the health coach does not tell the patient what to do but instead uses their values to illicit behavior change in the patients.18,19 Health coaching involves 3 aspects of motivational interviewing: an evocation of the patient's reasons to change or do a particular behavior, the sincere cognition of the patient's capabilities (autonomy), and the ability of the coach to be "in people's shoes" (compassion). In addition, this health coaching program adopted mindfulness by cultivating the coach's ability to be present in the moment of coaching despite distractions and to listen intently. Health coaching has been reported to motivate patients to continue with PR through social support.11,17 In this study, we found that coaching motivated behavior change through empowerment and accountability and that coaches also provided support to adapt exercises to fit participant needs. This further supports the importance of social engagement and partnership with the patients in PR 17,18,20 and aligns with our previous findings that health coach engagement can positively impact self-management abilities. 17 Previous studies have found that interactions with peers help patients stay active and compliant with behavior change programs.8,11
The health coaching component of this PR program may provide a sufficient substitute for the lack of interaction with other patients in home-based programs and downplay the absence of a modeling effect from peers.21
Our findings were also consistent with other research that reported patient appreciation for the home-based nature of the program.22 The patient experience in this report endorses the positive results of the parent study in QoL, physical activity, and self-management and suggests the importance of adding health coaching in the context of PR behavior change. It also proposes the potential benefit of training PR providers in MI and the science of behavior change. Remote patient monitoring and remote therapy CPT codes could be options for health coaching and lifestyle monitoring reimbursement. However, bringing health coaching to daily practice will require providers' and administrators' collaborative effort to bill for it. There may have been additional benefits to this program because it took place during the coronavirus disease 2019 (COVID-19) pandemic, which brought risks to in-person program attendance and disrupted some social opportunities for patients with COPD. Still, patients expressed that the home-based program may require support from a PR provider or health coach to consider how exercises can be done in different home settings and can be maintained (forming a habit).
There are some limitations to this work. This study did not include patients who withdrew from the study or did not complete the intervention. Although their experiences are critical to understanding barriers to participation, those patients were not eligible for inclusion under the parameters of the parent study.7 The qualitative nature of this inquiry and its sample size also limits generalizability; however, the relatively homogenous study population, focused research question, and use of theory as a systematic guide to analysis and interpretation are consistent with samples of this size.23-25 The use of a theoretical framework also bolsters the transferability of these findings to other similar settings and interventions. Like the parent trial, this study enrolled a demographically homogenous population. Specifically, these participants were all patients of a midwestern hospital with a primarily White, non-Hispanic, English-speaking patient population. Future research is needed to understand aspects of behavior change, including social norms, socioeconomic status, cultural beliefs, and structural or environmental factors of opportunity that may differ. This investigative team is working on modifying the program to engage minority populations, including the COPD minority groups that experience dramatic issues related to social determinants of health.
Conclusion
This study used a theory-based approach to unpack the experience of patients with COPD who completed a home-based PR program,15 including their perspectives on factors that may impact program completion and subsequent behavior change. Patients found the program feasible and described improved mood, attitudes, and physical function. Health coaching provides support, motivation, and accountability. Home-based programs like this should consider the unique factors that bolster motivation and self-efficacy to complete the program and structural ways to support initial uptake and sustained use. Our findings may be significant in informing the growing field of home-based programs for COPD—especially the combination of technical and social aspects—which is critically needed to increase the uptake and adherence of PR, further unveiled by the COVID-19 pandemic.
Acknowledgments
Author contributions: RB is the guarantor of the manuscript's content, including the data and analysis. All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. In addition, all authors were responsible for interpreting the results and writing the manuscript. JR and WM contributed to the data collection and interpretation of results.
The authors appreciate the support and work of the members of the Mindful Breathing Laboratory that made this study possible.
Declaration of Interest
The authors claim no conflict of interest and have no financial disclosure.