Running Head: Standardized COPD Care and Health Care Utilization
Funding Support: None
Date of Acceptance: June 22, 2023 | Published Online Date: June 27, 2023
Abbreviations: CAD=coronary artery disease; CHF=congestive heart failure; COPD=chronic obstructive pulmonary disease; CT=computed tomography; DEXA=dual energy X-ray absorptiometry; DM=diabetes; ED=emergency department; EHR=electronic health record; ICS=inhaled corticosteroids; JCAHO=Joint Commission on Accreditation of Healthcare Organizations; LABA=long-acting beta2-agonist; LAMA=long-acting muscarinic antagonist; OSA=obstructive sleep apnea; UTMB=University of Texas Medical Branch
Citation: Singh M, Hsu ES, Polychronopoulou E, Sharma G, Duarte AG. Structured evaluation and management of patients with COPD in an accredited program. Chronic Obstr Pulm Dis. 2023; 10(3): 297-307. doi: http://doi.org/10.15326/jcopdf.2022.0366
Note: Part of this work was previously presented in a Thematic Poster Session at the American Thoracic Society International Conference on May 14, 2021, in San Diego, California.
Introduction
Chronic obstructive pulmonary disease (COPD) affects 12.7 million Americans and is a leading cause of death in the United States.1,2 The health-related and economic burdens on patients with COPD are significant and as a group they are more likely to utilize health care services, resulting in higher health care costs compared to age-matched controls.3,4 In the United States, from 2006 to 2011, the number of emergency department (ED) visits for COPD or bronchiectasis increased from 1.48 million to 1.78 million and hospitalizations increased in this period such that in 2011 there were 682,670 hospitalizations.5 More recently, a group of investigators examined the incidence of patients with COPD exacerbations seen in the ED from 2010 to 2018 and they reported yearly increases in the incidence of patients with COPD exacerbations and that the prevalence of smoking among these patients had significantly increased.6 Moreover, patients with COPD suffer from poor symptom control and diminished exercise tolerance and are at risk for moderate and severe exacerbations, thus, there is a need to improve the quality of care.
Patients with COPD have complex needs and usual care may not allow for the delivery of guideline-recommended therapy resulting in inadequate disease control and poor outcomes.7 Specific chronic disease management programs may result in improved patient satisfaction, adherence to therapy, disease management, and cost control, especially for highest-cost patients in the chronically ill population.8-11 In the ambulatory setting, performance measures have been used to improve health care for patients with COPD.2,12,13 Reports have examined the clinical impact of quality care indices in patients with COPD but there is a paucity of data concerning the effect on health care utilization, specifically ED visits and hospitalizations.14-17 Moreover, adoption of evidence-based COPD clinical practice guidelines, incorporation of best care practice into the electronic medical system, and implementation at the point of care may impact individual care resulting in a reduction in health care utilization.7 Accordingly, the Joint Commission has developed a process whereby, health care centers receive accreditation for disease-specific evidence-based care delivery to populations with chronic illnesses including COPD. In April of 2014, the University of Texas Medical Branch (UTMB) received certification from the Joint Commission on Accreditation of Healthcare Organizations for Advanced Disease-Specific Care for COPD. Two clinics located at distinct locations within a single health care system were staffed by pulmonary faculty, fellows, nurses, and advanced practice providers in which a standardized approach was implemented directed at the diagnosis and management of COPD. Performance measures were developed and assessed monthly and reviewed with the ambulatory care staff using quality improvement methodology. The objective of this study was to compare the effect of COPD disease-specific and usual care provided in the ambulatory setting on health care outcomes, specifically all-cause ED visits and hospitalizations. We hypothesized that standardized management of patients with COPD managed in disease-specific specialty clinics using quality improvement methodology would reduce health care utilization compared to usual care in primary care clinics.
Methods
Study Cohorts
We conducted a retrospective cohort study of ambulatory patients with COPD treated at 2 accredited Joint Commission disease-specific specialty and 15 primary care clinics at the UTMB health care system from April 2014 to March 2018. Patients with COPD were identified through the use of the International Classification of Disease 9th revision codes: 491.x, 492.x, 496; or 10th revision codes: J41.0, J41.1, J44.9, J44.1, J44.0, J41.8, J42, J43.9, and J44.9. Data was extracted from electronic health records (EHRs) and study cohorts consisted of individuals ≥40 years old diagnosed with COPD with ≥ 2 outpatient visits 30 days apart starting April 1, 2014. We excluded patients lacking a diagnosis of COPD, without 2 clinic visits that were > 30 days apart, that received concurrent care in disease-specific specialty clinics and primary care clinics, or who received health care through the Texas Department of Criminal Justice. Demographics, smoking status, comorbidities, supplemental oxygen prescriptions, primary care provider specialty, and insurance status were collected. Comorbidities included obstructive sleep apnea (OSA), congestive heart failure (CHF), coronary artery disease (CAD), diabetes, lung cancer, anxiety, depression, and respiratory failure. This study received approval from the UTMB Institutional Review Board (IRB# 21-0132).
Clinic Structure
Patients with COPD were referred by primary care providers or self-referred to disease-specific clinics and after 2 visits became established patients. Visits to disease-specific clinics consisted of 60 minutes for new visits and 30 minutes for follow-up with more time devoted to patient care. At each clinic visit, patients underwent a structured assessment that involved recording the following performance measures as present or absent in the EHR: diagnostic spirometry, tobacco cessation counseling for current smokers, influenza and pneumococcal immunizations, inhalation technique instruction, alpha-1 antitrypsin deficiency testing, dual-energy X-ray absorptiometry (DEXA) scan for osteoporosis, and chest computed tomography (CT) imaging for lung cancer screening. At the conclusion of the visit, patients were provided with a printed self-management plan that included symptom recognition, medical treatment, and contact information during and after office hours. Clinicians were encouraged to review and record the performance of these variables and provide monthly feedback regarding opportunities for improvement.
The primary care clinic cohort consisted of patients with COPD receiving care at a primary care clinic site in the UTMB health care system staffed by advanced practice providers, interns, residents, and faculty physicians. Visits to primary care clinics consisted of 20 to 30 minutes for new visits and 10 to 15 minutes for follow-up. Clinicians used their discretion in the evaluation and management of these patients. COPD assessment flowsheets and self-management plans were available in the EHR for all clinicians to use. However, data on compliance with performance measures was not reviewed or shared with the individual providers or clinics.
Outcomes
Our primary outcome was all-cause ED visits and/or hospitalizations following a patient’s index date (second outpatient visit). A secondary outcome was the completion of performance measures that were auto-populated from the EHR and completed by the provider.15 Performance of a chest CT for lung cancer screening was recommended to eligible patients based on the U.S. Preventive Services Task Force guidelines.18 Supplemental oxygen prescriptions were available for all patients who qualified based on Centers for Medicare and Medicaid Services’ guidelines and eligible patients were prescribed supplemental oxygen by their provider. DEXA scans were recommended for individuals at high risk for osteoporosis or in need of treatment19 and managed by primary care providers or referred to an endocrinology clinic.
Statistical Analysis
Demographics and clinical characteristics were summarized as frequency and percentage or mean ± standard deviation. Continuous variables were compared using t-tests while categorical variables were assessed using Chi-square tests. The index date for each patient was determined as the time of the second clinic visit. An a priori reduction in ED visits and hospitalizations was anticipated to occur 12 months after the index date. In the propensity score matching process, patients were matched on prior COPD-specific hospitalizations as well as demographics (gender, age, race), prior oxygen prescriptions, and comorbidities as these would more likely influence health care utilization. After propensity matching, we calculated standardized differences in the matched cohort for the variables used in the matching that revealed no statistically significant differences between the groups. Cox regression analysis was performed with additional adjustment for smoking and medication use as these variables could influence the outcomes, ED visits, and hospitalizations. We performed an analysis of time to first health care encounter (ED or hospitalization) with each patient’s second clinic visit as the index date with the maximal follow-up time of 47 months. Cut-off values of 18 and 20 months were used in the ED and hospitalization analysis. This was required due to the violation of proportional hazards in the Cox models and the timepoints were chosen to ensure that the statistical models were appropriate and accurate. For the primary care cohort, the index date was assigned based on the matched disease-specific care patient.At the start of the index date, each patient accrued time recorded as patient months. When there was an obvious violation of the proportional hazard assumption based on Kaplan-Meier curves, we stratified models by adding interaction terms with time. In addition, we considered the competing risk of death during the study follow-up period by modeling cause-specific hazards. All analysis was performed with SAS version 9.4 (SAS Inc., Cary, North Carolina) with reported p-values as 2-sided with p<0.05.
Results
Patient Demographics and Cohort Characteristics
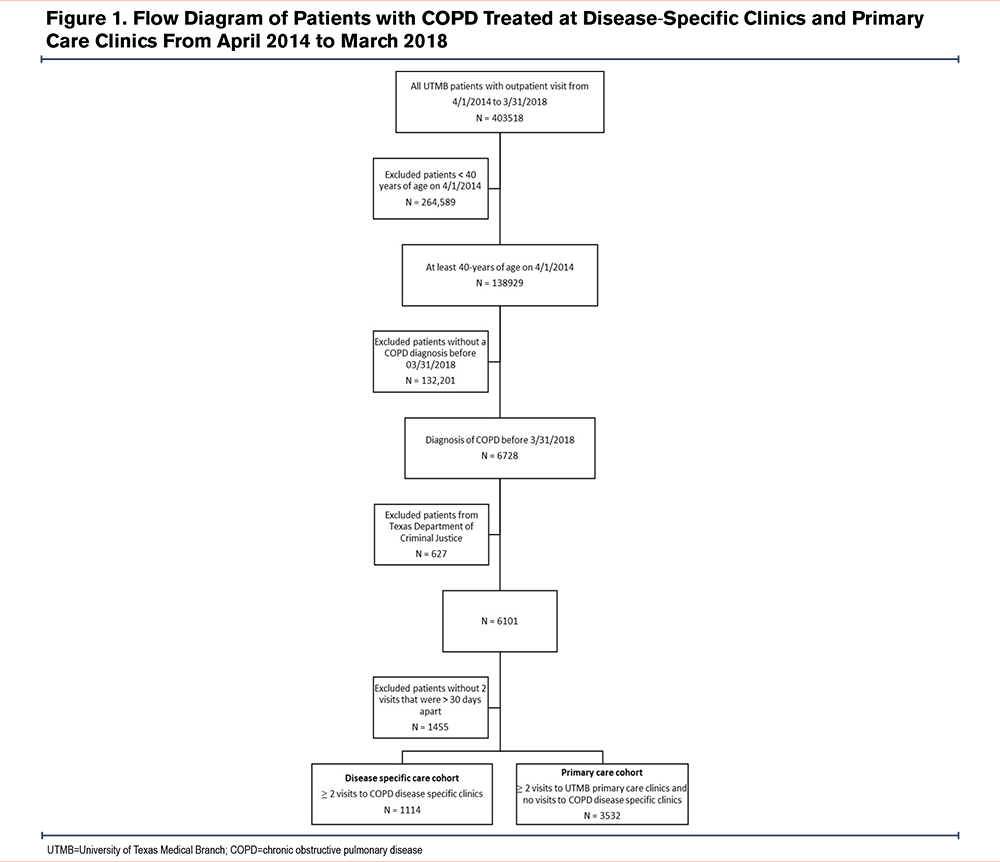
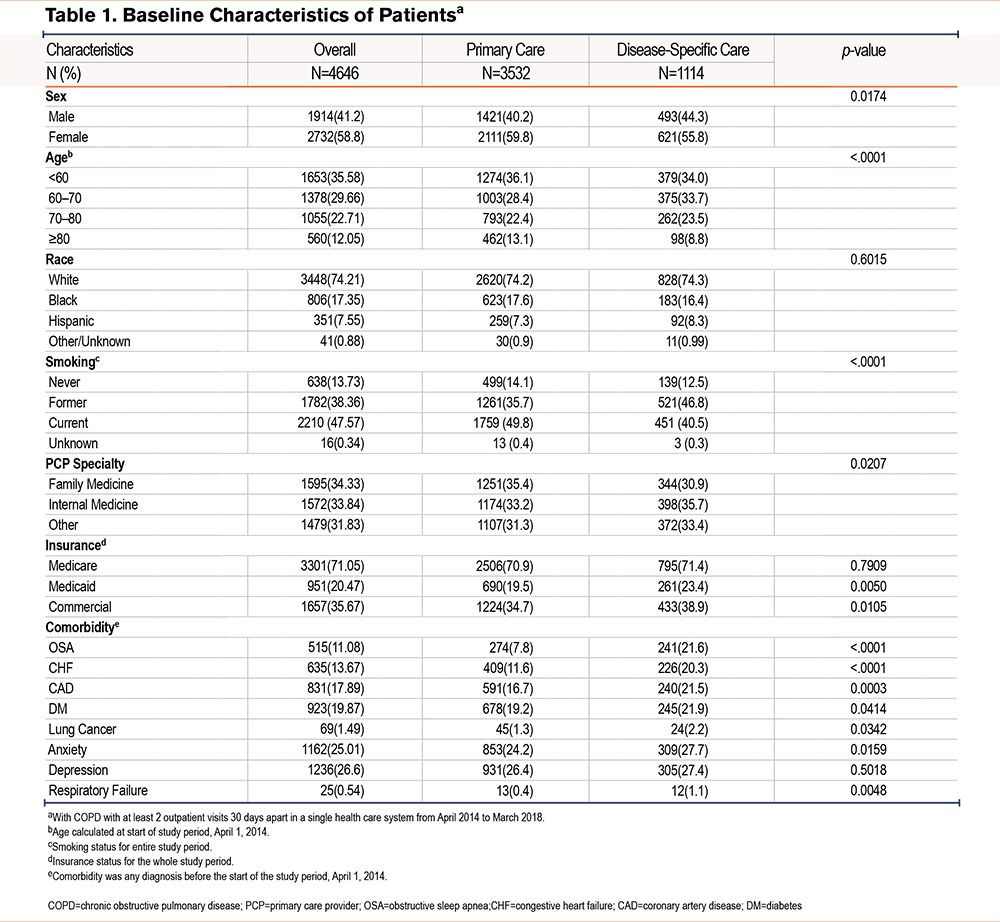
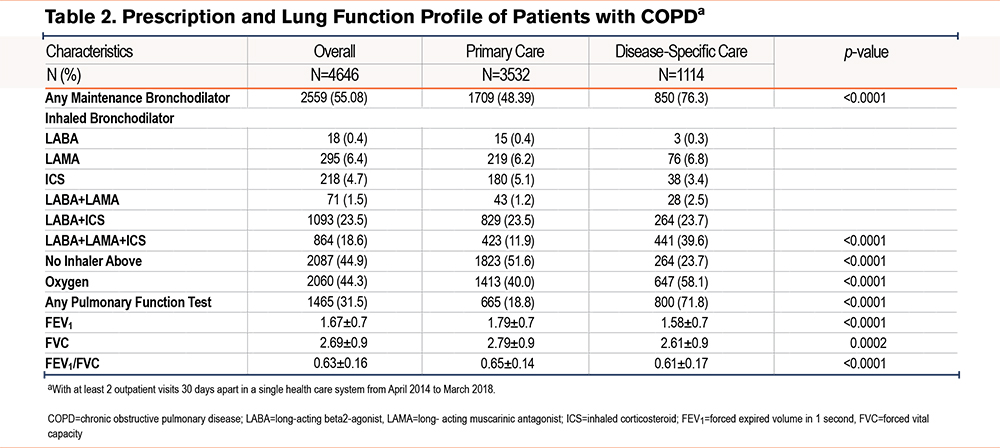
From April 1, 2014, to March 30, 2018, a total of 6101 patients with COPD had an outpatient encounter with a health care provider. The study cohort consisted of 4646 patients with COPD with at least 2 office visits, 30 days apart, and 1114 who solely received care at disease-specific care clinics and 3532 who received treatment only at primary care clinics (Figure 1). The mean follow-up time of the cohort after the index date was 12.2±12.6 months. Characteristics of the entire cohort demonstrated a mean age of 65.4 ± 11.4 years that was predominantly female (58.8%), non-Hispanic White (74.2%) with current (47.6%), or former smokers (38.4%) (Table 1). Patients treated in disease-specific clinics consisted of more patients 60 to 70 years old (33.7% and 28.4%, respectively; p≤0.0001) and fewer females (55.8% and 59.8%, respectively; p=0.02) compared to primary care clinics. Regarding smoking status, more current smokers were noted in the primary care group, while a greater number of former smokers were observed in the disease-specific care group. Patients treated in the disease-specific clinic were more likely to have spirometry testing that revealed significantly greater airflow obstruction compared to the primary care group (Table 2). Furthermore, patients managed in the disease-specific clinics were more often prescribed inhaled combination therapy (corticosteroids, long-acting antimuscarinics, and long-acting beta-agonists) compared to the patients treated in the primary care clinics. After matching for age, sex, race, previous year hospitalizations, supplemental oxygen prescription, and comorbidities, a comparison of the groups demonstrated the disease-specific care group to have more patients aged 60–70 years (33.7% versus 27.5%), former smokers (43.8% versus 30.3%), patients with obstructive sleep apnea (21.6% versus 8.3%), or congestive heart failure (20.3% versus 14.6%) compared to the primary care group.
Performance Measures and Outcomes
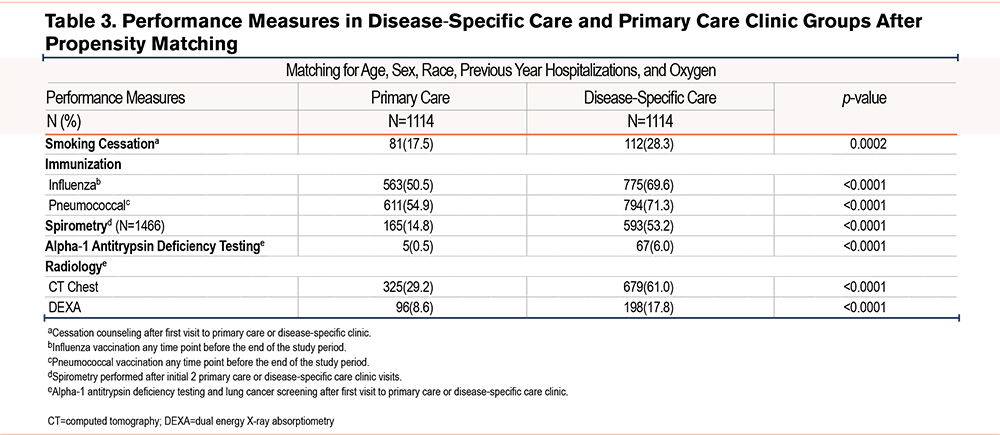
After propensity matching, comparison of performance measures between the 2 groups demonstrated that patients provided care in disease-specific clinics were more likely to receive tobacco cessation counseling (among current smokers) (28.3% and 17.5%; p=0.0002), influenza vaccination (69.6% and 50.5%; p≤0.0001), and pneumococcal vaccination (71.3% and 54.9%; p≤0.0001), spirometry testing (53.2% and 14.8%; p≤0.0001) and testing for alpha-1 antitrypsin deficiency (6.0% and 0.5%; p≤0.0001), respectively (Table 3). Lung cancer screening with chest CT imaging was performed more frequently in the disease-specific group compared to the primary care group(61.0% and 29.2%, respectively; p≤0.0001). Assessment for osteoporosis with DEXA scans was performed more often in the disease-specific care group compared to the primary care group; 17.8% and 8.6%, respectively; (p≤0.0001) (Table 3).
Emergency Department Visits and Hospitalizations
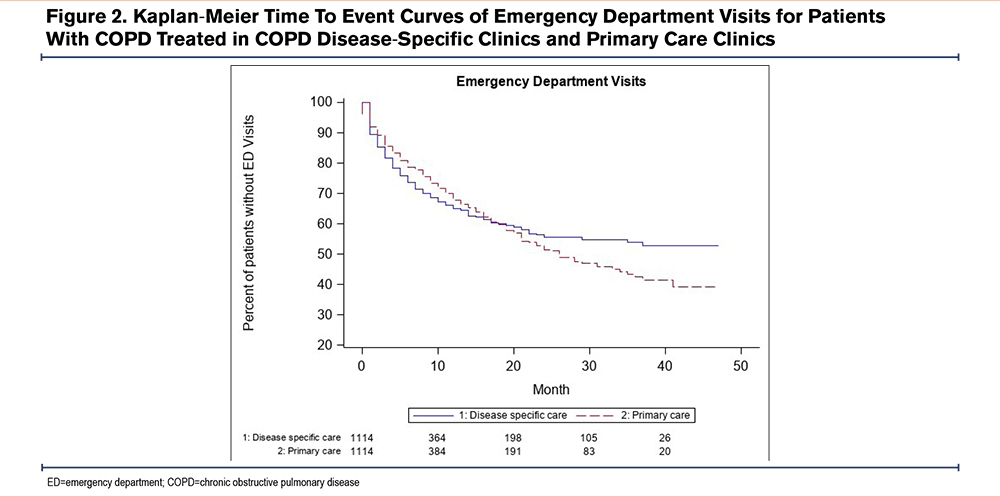
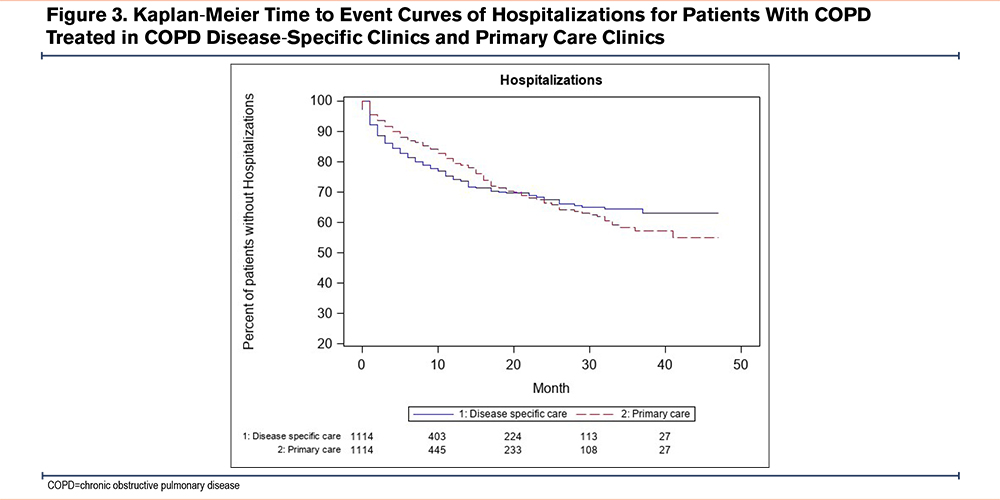
A comparison of the time to first ED visit between the disease-specific care and primary care groups revealed that starting at 18 months after the index date, the disease-specific care group had fewer ED visits compared to the primary care group (HR 0.31, 95% CI 0.18–0.54) (Figure 2). A comparison of time to first hospitalization revealed that starting at 20 months after the index date, the disease-specific care group had significantly fewer hospitalizations compared to the primary care group (HR 0.41, 95% CI 0.21–0.79) (p=0.001) (Figure 3).
Discussion
The establishment of an accredited advanced chronic disease COPD program resulted in the implementation of quality measures aimed at improving care of patients with COPD. Our findings reveal that patients with COPD treated in disease-specific clinics were more likely to undergo spirometry, vaccine administration, tobacco cessation counseling, and lung cancer screening than patients with COPD in primary care clinics. Furthermore, the group that received care at disease-specific clinics had lower rates of all-cause ED visits and significantly fewer hospitalizations compared to patients receiving care in primary care clinics.
Management of patients with COPD in the ambulatory setting is challenging given the variability in clinical features and response to medical therapy. Consensus group guidelines recommend the use of spirometry as a reference standard for diagnosis, preventive measures (smoking cessation, vaccination, lung cancer screening), and treatment directed by patient symptoms and exacerbation frequency.1 Notably, reports have demonstrated influenza vaccination is associated with fewer hospitalizations and deaths20,21 while patients receiving pneumococcal vaccination were less likely to experience an exacerbation.22 Likewise, smoking cessation was reported to reduce exacerbations and frequency of ED visits.23 Yet, guideline-recommended care for the treatment of COPD is not readily implemented and health care providers do not commonly provide patients with evidence-based care.24-27 In addition, a recent observational study conducted at the University of Washington demonstrated that COPD quality of care was suboptimal over a 1-year period and pulmonary medicine referral was associated with a greater receipt of optimal outpatient care quality.17 Our findings highlight the variance in the implementation of evidence-based guidelines and standard practice in the ambulatory setting. Moreover, it is difficult to assess whether the amount of time at each clinic visit or a knowledge gap in the primary care setting is responsible for differences in performance of evidence-based guidelines.
Various governmental agencies have recognized the challenges in the delivery of high-value care to patients with COPD and proposed measures to improve care.28 Performance measures directed at the care of patients in the ambulatory setting have been reported that include diagnostic spirometry, pneumococcal and influenza vaccinations, smoking cessation, oxygen saturation assessment, pulmonary rehabilitation referral, and bronchodilator reconciliation.26 Implementation of COPD-specific performance measures that lead to improvements in patient outcomes has been examined by various groups.14,29,30 From 2008 to 2011, a Danish population-based cohort study examined the quality of care for ambulatory patients with COPD and reported improvements in the delivery of processes of care but did not have sufficient data for analysis on outcomes or prognosis.31 Another group designed a study to promote physician adherence to COPD guidelines and thereby, reduce the rate of exacerbations for patients treated in primary care clinics located in Oregon. The authors reported that neither case management, health care provider education, nor a web application regarding disease management was associated with a reduction in exacerbation rates.14 Recently, a multidisciplinary team reviewed health records of discharged patients from the Veteran’s Administration and developed recommendations focused on diagnostic, pharmacologic, and nonpharmacologic care that was provided electronically to patients' primary care physicians. Over a 30-month period, the investigators found the health system-level intervention resulted in a significant improvement in COPD-specific quality of life but did not reduce readmissions or mortality.30 Similarly, in the current study, the effects of receiving care for COPD in the disease-specific care clinics led to increased delivery of optimal care for patients with COPD. Additionally, we found that the impact of performance measures on outcomes lagged by 18–20 months, therefore, studies designed with a shorter interval may not observe the outcomes associated with improvements in process of care measures.
Emergency Department Visits and Hospitalizations
The impact of COPD on health care utilization is significant and individuals with COPD account for a greater burden on health care systems compared to the general population.32 From 2001 to 2012, a report described temporal trends in health care use among adults with COPD that revealed age-adjusted rates of hospitalizations and ED visits for COPD did not change significantly in the United States, while the rates decreased significantly for common cardiovascular disorders, pneumonia, and lung cancer.5 A recent population-based study from Ontario Canada found that adults with physician-diagnosed COPD treated between 2006 and 2016 had increasing ED visits over the study period.33 In another large population-based study from North Carolina from 2008 to 2009 that involved 33,799 patients, the authors reported that the percentage of patients with COPD-related return ED visits within a 365-day period of their index ED visit was 28%, highlighting thatED visits are a risk factor for future ED visits. In the same study, more than half of patients required hospitalization, and the presence of comorbidities like congestive heart failure, substance-related disorders, or respiratory failure requiring supplemental oxygen was associated with a higher likelihood of hospitalization than those without these comorbidities.2 Hence, for patients with COPD, measures to prevent ED visits, especially among patients with comorbidities, are important.
In the current study, there was no difference in health care utilization between disease-specific care and primary care groups months after the index date, however, 18 months after the index date (patient’s second visit to disease-specific care), the disease-specific care group had fewer ED visits. Likewise, 20 months after the index date the disease-specific care group had fewer hospitalizations. A delay in improved patient outcomes has been reported in clinical trials examining the effect of long-acting bronchodilator therapy in which moderate-severe exacerbations and COPD-related death was delayed by 17–24 months.34,35 Moreover, the outcomes associated with chronic disease management programs can occur over months. This was demonstrated in a chronic disease management program implemented for patients with heart disease or diabetes and the effect size reduction in hospital admissions increased over time.36 However, implementation of a chronic disease assessment can be difficult, since the demand on primary care providers to screen, manage, and counsel patients with numerous chronic medical conditions may pose a challenge to primary care physicians and lead to suboptimal care of patients with COPD. Overall, our study supports the longitudinal effect of a chronic disease management program and demonstrates the increasing effect over time related to provider-patient interactions, a structured approach to a COPD action plan, and patient access to nurse- directed management of acute exacerbations.
Limitations
There are several limitations including that this single-center study compared performance measures and patient outcomes between accredited COPD specialty and primary care clinics that are subject to bias. We acknowledge that this study, like other observational studies, is prone to unmeasured confounding factors. Although this might have led to some of the weaker associations, we believe that the integration of performance measures and implementation of an action plan with access to a medical provider resulted in earlier treatment of acute exacerbations and avoidance of hospitalizations. Further investigation with multiple sites may provide additional support to this approach. Another limitation concerns our limited capacity to accurately assess prior exacerbations in the primary care group as well as the low performance of diagnostic spirometry in the primary care setting. Similarly, due to the nature of the structured evaluation and management at the advanced disease program, it was not possible to determine the benefits of individual components. Another weakness concerns the length of the study, and it is possible that increasing the study duration could further delineate the differences in ED visits and hospitalizations between the groups. An additional limitation concerns our assessment of all-cause ED visits or hospitalizations rather than COPD-related events. Another limitation concerns death as a competing risk factor in the time-to-event analysis. Although we were only able to determine patient deaths within our health care system, we conducted a competing risk analysis for any death captured in the electronic health care record that did not change the findings for the outcome of ED visits or hospitalization.
Conclusion
In summary, patients with COPD who were provided care in specialty-specific clinics received greater attention to processes of care that encompassed diagnostic, preventive, and screening measures. The multifaceted approach that involved guideline-directed process of care implementation, patient engagement, an outlined action plan of care, and accessibility to providers resulted in the observed outcomes. In this observational study, implementation of a disease management program in the ambulatory setting for patients with COPD, within a single health care system, was associated with a reduction in all-cause ED visits and hospitalizations. Additional investigations are needed regarding causality between implementation of a structured disease management program and health care utilization.
Acknowledgement
Author contributions: AGD and GS contributed to the conception, design, analysis, writing, and editing. MS contributed to the analysis, writing, and editing. EH contributed to data acquisition, design, analysis, and writing of the manuscript. EP contributed to data acquisition, analysis, writing, and editing of the manuscript. All authors provide final approval of the submitted manuscript. MS and AGD take responsibility for and are guarantors for all the content in the manuscript including the data and analysis.
Declaration of Interest
The authors have no conflicts of interest to declare.