Running Head: 6th World Bronchiectasis and NTM Conference
Funding Support: n/a
Date of Acceptance: October 4, 2023 │ Published Online Date: October 25, 2023
Abbreviations: NTM=nontuberculous mycobacterial lung disease; WBC2023=6th World Bronchiectasis and Nontuberculous Mycobacteria Conference; WBD=World Bronchiectasis Day
Citation: Aksamit TR, Emery EJ, Basavaraj A, Metersky ML, O'Donnell AE, Addrizzo-Harris DJ. The 6th World Bronchiectasis and Nontuberculous Mycobacteria Conference abstract presentations. Chronic Obstr Pulm Dis. 2023; 10(4): 450-516. doi: http://doi.org/10.15326/jcopdf.2023.0464
Introduction
The 6th World Bronchiectasis and Nontuberculous Mycobacteria (NTM) Conference (WBC 2023) was held in New York, New York from July 18, 2023 through July 20, 2023. This conference brought together investigators, clinicians, patients, caregivers, and industry representatives involved in the bronchiectasis and NTM space for a far-reaching, engaging, and cutting-edge update from around the world.
Attendees included more than 650 participants total with 379 in-person participants and the remainder virtually. Participants included 40 faculty members, almost 90 trainees, 24 exhibitors, and more than 160 patients and caregivers from 30 countries and 6 continents reflecting the authentically global nature of this World Bronchiectasis and NTM conference. In addition to new research advancing the science, presentations by international experts addressed a current, state-of-the-art, comprehensive overview of the pathophysiology, natural disease course, epidemiology, and clinical approach to bronchiectasis and NTM lung disease. Investigators presented 60 posters with their latest research results. Exhibitors included industry representatives underscoring robust collaboration and support across many interests in the bronchiectasis and NTM communities.
The World Bronchiectasis and NTM Conference series (Hannover, Germany; Milan, Italy; Washington, D.C.; virtual (2020); Prague, Czech Republic; and New York, New York) celebrates and remains a premier venue for highlighting the international collaboration of a wide range of clinicians, investigators, patients, caregivers, and industry representatives. Other activities raising global awareness in partnership with the World Bronchiectasis and NTM Conference series include World Bronchiectasis Day (WBD) (https://www.bronchiectasisandntminitiative.org/Bronchiectasis/Bronchiectasis-Resources/World-Bronchiectasis-Day). Although a year-long campaign for raising awareness, the WBD initiative involves global activities year-round and is anchored annually on July 1st. The inaugural celebration of World Bronchiectasis Day occurred at the 5th World Bronchiectasis Conference held in Prague, Czech Republic in 2022.
Keynote lectures from global experts began the WBC 2023 with comprehensive and organized lectures on bronchiectasis from James Chalmers, MBChB, PhD, from the University of Dundee as well as a lecture on NTM lung disease from Charles L. Daley, MD, from National Jewish Medical Center in Denver, Colorado. The following 2 full days featured bronchiectasis on the first day in a comprehensive fashion including practical hands-on sessions organized by airway clearance experts. Bronchiectasis sessions focused on etiology, pathophysiology, mechanisms of disease, comorbidities, clinical management, and registry updates by leading experts. Poster presentations with lively discussions guided by content experts in the field of bronchiectasis and NTM were held throughout the conference. Awards were presented to top peer-selected rising stars and investigators sharing outstanding work. Early career researchers had an opportunity to meet with established researchers and clinicians during a networking luncheon that was well received and generated new networking, research strategies, and collaborative opportunities.
The second full day of the WBC 2023 focused on NTM, with sessions on epidemiology, the role of the environment, research activities, treatment, and novel therapies for bronchiectasis and NTM treatment. Robust interactions between presenters and attendees along with moderators enriched the presentations and information provided, creating a memorable experience for all.
The overall upbeat vibe of activities at the conference reflects the exponential growth and explosion of interest in what has been described as the new age of bronchiectasis and NTM lung disease. Great appreciation for tremendous support is extended to many, including but certainly not limited to, patients, caregivers, and industry partners. For those of us fortunate to represent these communities we are all encouraged and passionate regarding progress to date. We are honored to present this collection of abstracts from the WBC 2023 reflecting the high quality and tremendous work of advancing the science and meeting the unmet needs of bronchiectasis and NTM lung disease.
NOTE: The following abstracts have NOT been copyedited, but are presented here in their original format, as presented by the authors at the WBC 2023 (July 18-20, 2023) in New York City. The following abstracts are grouped according to their poster section. Case reports presented at the conference are omitted from the publication.
Figures are labeled/numbered as they appear, sequentially, within the entire article—not each individual abstract. Therefore, the figure number may not match the abstract number.
Rising Star Researcher Awards—Abstract 1
Alpha-1 Antitrypsin and Deoxyribonuclease 1 as Potential Therapies for the Treatment of Bronchiectasis
Paul King, MBBS, FRACP, PhD1
Author Affiliations:
1. Monash Medical Centre/Monash University, Melbourne, Victoria, Australia
Background:
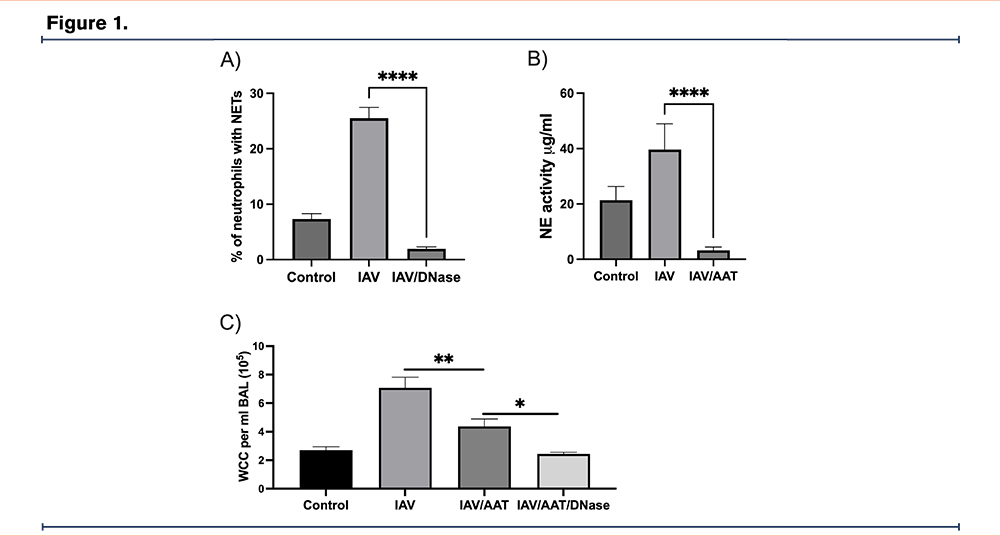
The excessive production of proteases such as neutrophil elastase (NE) drives inflammation and the development of bronchiectasis; the main anti-protease is alpha-1 antitrypsin (AAT). A mechanism of lung protease expression is via neutrophil and macrophage extracellular trap formation (NETs/METs); which are broken down by deoxyribonuclease 1 (DNase 1). The ability of AAT and DNase 1 to reduce inflammation in vitro and in vivo was assessed.
Methods:
AAT eluted from human serum and recombinant DNase 1 (dornase alfa/Pulmozyme) were used. In vitro experiments were performed using blood and bronchoalveolar lavage (BAL) samples from human subjects that were infected with influenza A virus (IAV) or nontypeable Haemophilus influenzae (NTHi) to upregulate NET/MET and NE expression; AAT and DNase 1 were added. In vivo experiments were performed in mice infected with IAV/NTHi and administered inhalational AAT and DNase 1 for 3 days.
Results:
Samples were obtained from 22 adults (mean age of 51 ± 16 years). Infection induced prominent NET (Fig. 1A) and MET expression in vitro, which was reduced by the addition of DNase 1 (p<0.0001). AAT reduced NE expression in vitro (Fig. 1B), (p<0.0001). AAT reduced inflammation in infected mice as assessed by lung weight and BAL white cell count (n=8 mice, p<0.05) (Fig. 1C), this effect was enhanced by the addition of DNase 1.
Conclusions:
Alpha-1 antitrypsin reduces lung inflammation and this effect is enhanced by the addition of DNase 1.
Rising Star Researcher Awards—Abstract 2
Prevalence and Factors Associated with the Isolation of Fungi in the Sputum of Bronchiectasis Patients
Pamela J. McShane, MD1 Amanda E. Brunton, MPH2 Radmilla Choate, MPH, PhD3 David Fraulino, MD4 Christopher Richards, MD5 Kevin Winthrop, MD, MPH2 Kevin Tsui, MD6 Restrepo I. Marcos, MD, MSc, PhD7 Diego J. Maselli Cacer, MD8 Mark L. Metersky, MD4
Author Affiliations:
1. University of Texas Health Science Center at Tyler, Tyler, Texas, United States
2. Oregon Health and Science University, Portland, Oregon, United States
3. University of Kentucky, Lexington, Kentucky, United States
4. University of Connecticut School of Medicine, Farmington, Connecticut, United States
5. Mass General, Boston, Massachusetts, United States
6. University of Chicago, Chicago, Illinois, United States
7. University of Texas Health at San Antonio, San Antonio, Texas, United States
8. UT Health San Antonio, San Antonio, Texas, United States
Background:
The presence of fungi in the sputum of bronchiectasis patients is common but the clinical significance is not fully understood.
Methods:
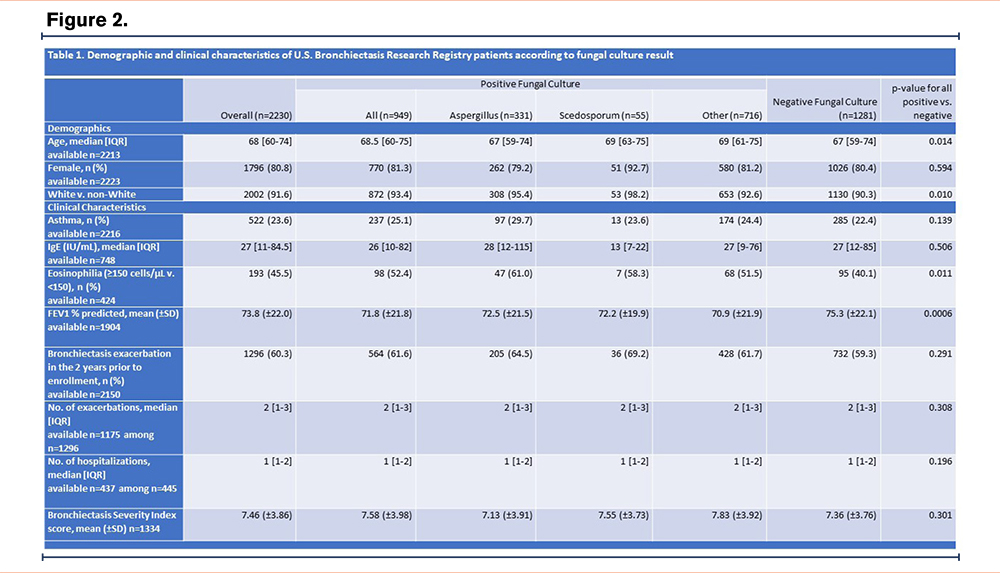
We analyzed data from patients enrolled in the U.S. Bronchiectasis Research Registry as of December 2022 with documented fungal culture results. Fungi included Aspergillus, Scedosporum, and other. Patients with ABPA were excluded. Descriptive statistics were computed for baseline demographics and clinical characteristics for the overall sample, stratified by presence positive or negative fungal culture. Values were compared using the chi-square test for categorical variables and t-tests for continuous variables.
Results:
2,230 patients with bronchiectasis and at least one fungal culture result were included in the study. 42.6% (949/2230) were positive and 57.4% (1281/2230) had no growth on fungal culture. Table 1 shows demographics and clinical characteristics. FEV1 percent predicted was lower in patients with > 1 positive fungal culture than no growth (mean 71.8 +21.8 vs 75.3 +22.1, p=0.0006). Eosinophilia (>150 cells/uL) was more common in patients with positive fungal cultures than in patients with no growth (52.4% [98/193] vs 40.1% [95/193], p=0.011), but prevalence of asthma did not differ according to fungal culture result. Growth of bacteria was more often accompanied by a positive fungal culture than no growth on fungal cultures (62.0% [588/949] vs 46.3% [589/1272], p=<0.0001). Users of corticosteroids (oral or inhaled) were more likely to have a positive fungal culture than a negative result (10.4% [53/509] vs 6.5% [35/539], p=0.022). NTM infection status, exacerbation frequency, and bronchiectasis severity as measured by BSI did not differ between patients with positive or negative fungal culture (p=0.615; p=0.303; p=0.232, respectively).
Conclusions:
In the U.S., the presence of fungus in the sputum of bronchiectasis patients was associated with worse lung function, but does not appear to impact other important clinical outcomes such as exacerbations and severity of disease.
Acknowledgements
The authors would like to acknowledge the COPD Foundation, a 501(c)(3) nonprofit organization, who manages the Bronchiectasis and NTM Research Registry. The Registry is funded by the Richard H. Scarborough Bronchiectasis Research Fund, the Anna-Maria and Stephen Kellen Foundation, a Research Grant from Insmed Incorporated, and the Bronchiectasis and NTM Industry Advisory Committee. Also, this work would not be possible without comprehensive chart reviews and data recording by the dedicated research coordinators and PIs at each participating Registry site.
Rising Star Researcher Awards—Abstract 3
A Single Centre Analysis of Non-Tuberculous Mycobacteria from Johannesburg, South Africa
Lamla Nqwata, MBCHB1 Jotam Pasipanodya2 Marianne Black3 Charles Feldman4
Author Affiliations:
1. Health Department, Johannesburg, Gauteng, South Africa
2. Stanford Health Centre, California, California, United States
3. National Health Laboratory Services, Johannesburg, Gauteng, South Africa
4. Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, Gauteng, South Africa
Background:
In Sub-Sahara African setting, paucity of data regarding the distribution of individual Mycobacterial species and related comorbidities results in underappreciation of nontuberculous mycobacteria (NTM) diseases, allocation of fewer resources with potential adverse outcomes for patients. We hypothesized concomitant infections would be the most significant risk factors that influence patients’ trajectories and outcomes in our South African settings.
Methods:
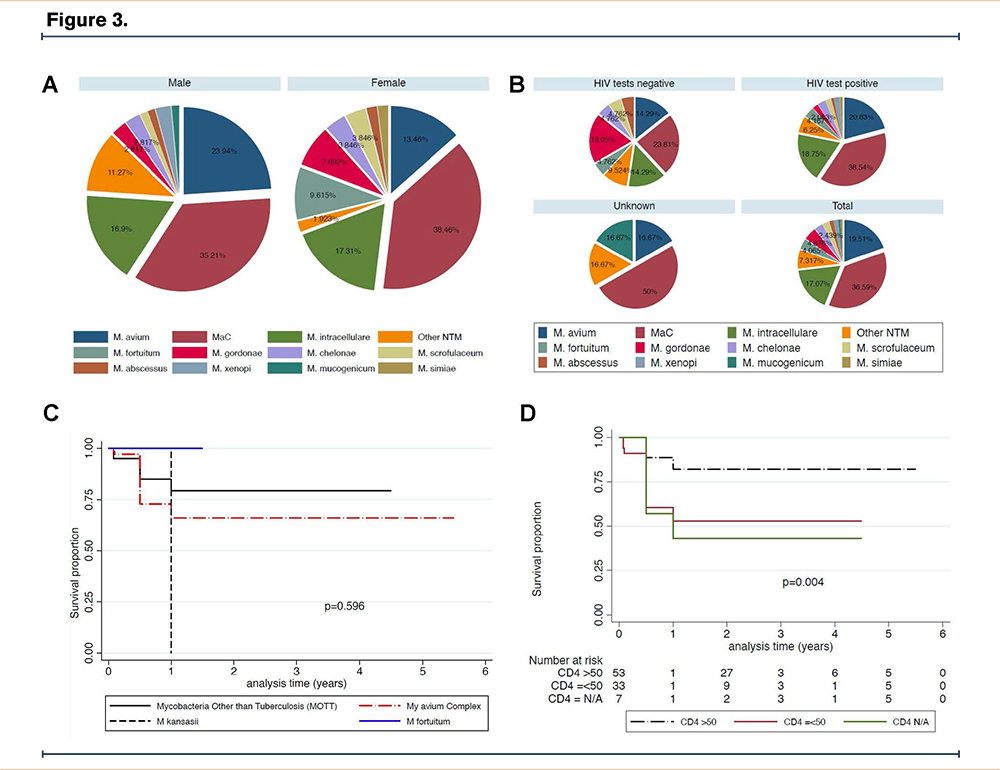
A retrospective review of all clinical isolates that were positive for NTM between 1 January 2010 and 30 June 2017 and the corresponding medical records of the patients at Charlotte Maxeke Johannesburg Academic Hospital (CMJAH), South Africa were extracted, reviewed, and analysed for long-term survival. Cox regression and log rank tests were used to compare survival between patients stratified by NTM species, whether ATS criteria were met, HIV status and CD4 counts.
Results:
Mycobacterium avium complex (Mac) was found in 90 (70%), M. fortuitum 6 (5%) and M. gordonae 5 (4%) out of the 123 patients followed up for median (interquartile range [IQR]) of 1(0.5 – 4.5) years (Figure A&B). HIV 96 (78%) and previous PTB episode 38(30%) were the common comorbid illnesses, while 60 (49%) were observed without antibiotics given. Median age of patients was 39 (IQR 31-51) with male predominance 71(58%), cavitary lesion chest X-ray in 12 (10%) and initial bacterial load of 1.64 (IQR1.25 – 2.39) log10 colony forming units. Overall, 27(22%) were successfully treated and 28 (23%) died (Figure 1). The adjusted hazard rate for low CD4 counts ≤50 cells/mm3 was 2.79 (95% Confidence Intervals [CI], 1.20 - 6.50), while that for those with unknown CD4 counts was 4.01 (95% CI, 1.17 – 13.77) compared to CD4 counts >50 cells/mm3 (Figure D).
Conclusions:
Among patients with pulmonary NTM in our environment, MAC is the most common isolate. HIV infection is significant risk factor for early death regardless of gender.
Rising Star Researcher Awards—Abstract 4
Distinct Features of the Lower Airway Microbiome in NTM Bronchiectasis
Shivani Singh, MD, PhD1 Fares Darawshy1 Kirby Erlandson1 Destiny Collazo1 Kelsey Krolikowski1 Isabella Atandi1 Clea Barnett, MD1 Yonghua Li1 Imran Sulaiman, MD, PhD1 Miao Chang1 Rosemary Schluger, RN1 Ibrahim Kocak1 Rajbir Singh1 Colin McCormick1 Yaa Kyeremateng1 James Tsay, MD1 Ashwin Basavaraj, MD2 David Kamelhar, MD1 Doreen J. Addrizzo-Harris, MD1 Leopoldo Segal, MD1 Benjamin Wu, MD1
Author Affiliations:
1. NYU Langone Health, New York, New York, United States
2. NYU Grossman School of Medicine, New York, New York, United States
Background:
The lower airway microbiome of patients with non-tuberculous mycobacterial lung disease (NTM-LD)/bronchiectasis holds a complex set of microbes, but the influence of the non-pathogen fraction of the microbiome on the disease process is unknown. The significance of the interaction between the microbiome and a dominant or a non-dominant pathogen is also unknown. Here, we investigated whether distinct lower airway microbial communities indicate different patterns of pathogen colonization in bronchiectasis.
Methods:
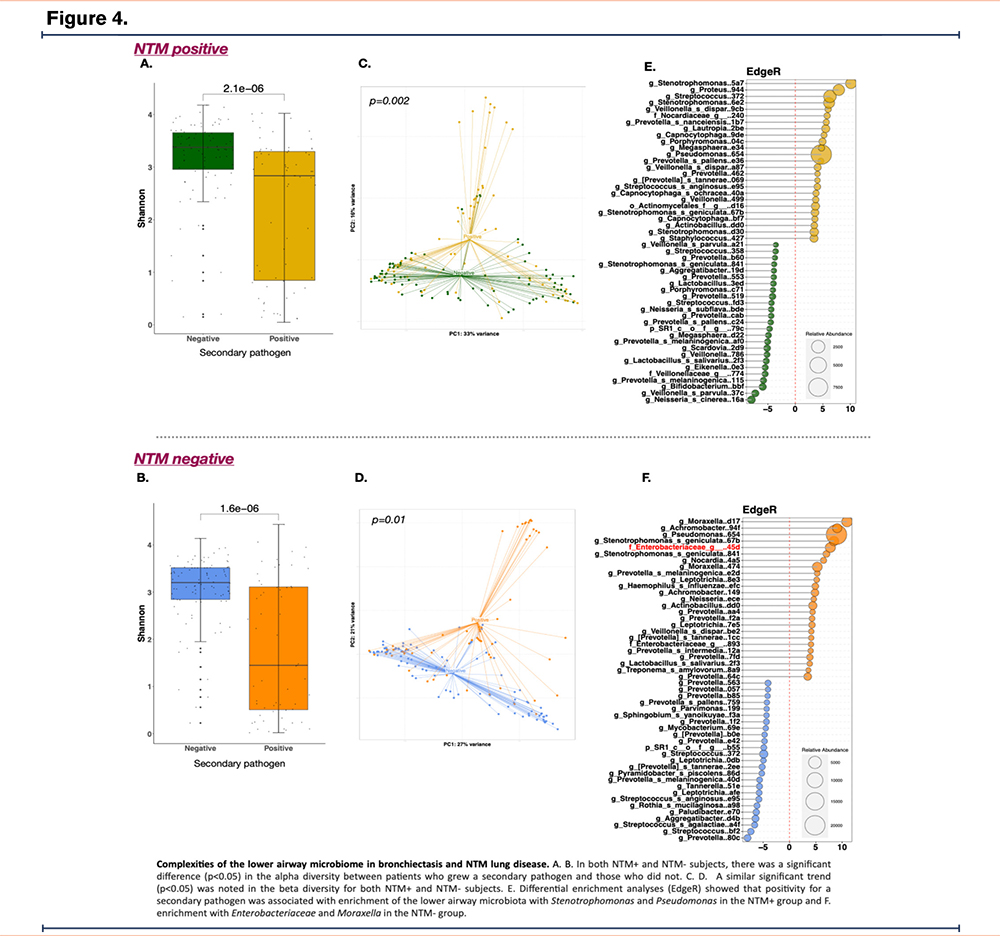
Patients with bronchiectasis underwent clinically indicated bronchoscopies. Samples (upper/ lower airways and backgrounds) underwent 16S rRNA gene sequencing and were analyzed with QIIME2, PhyloSeq and EdgeR.
Results:
In a cohort of 200 patients, a large proportion (n=94, 47%) met the diagnostic criteria for NTM-LD. In the NTM–group, Pseudomonas was frequently recovered in culture (15.7%). Within this group, there was a sub-cohort of patients showing high dominance, or low alpha diversity, and a distinct microbial composition that presented with frequent exacerbations. In the NTM+ group, a high proportion (44%) exhibited a secondary pathogen in culture. In both NTM+ and NTM- subjects, patients who grew a secondary pathogen in cultures had lower alpha diversity than those who did not (p<0.05, Fig. A. B). Compositionally, based on alpha diversity analyses, isolation of a secondary pathogen was also associated with distinct taxonomic differences (Fig. C.D). In particular, differential enrichment analyses (EdgeR) showed that within the NTM+ group, positivity for a secondary pathogen was associated with enrichment with Stenotrophomonas and Pseudomonas (Fig. E), whereas in the NTM- group, there was enrichment with Enterobacteriaceae and Moraxella (Fig. F). DESeq2 showed that in the NTM- group, positive respiratory culture was associated with enrichment with Moraxella.
Conclusions:
This study illustrates that heterogeneity and structure of the lung microbiome in bronchiectasis is in part dependent on the main pathogen isolated and the presence of a secondary pathogen.
Bronchiectasis and Genetics—Abstract 5
Validation of a Commercial Human ELISA Kit to Measure Alpha-1 Antitrypsin (AAT) in Sputum
Ianire Gallego Amaro1 Letizia Traversi, MD1 Almudena Felipe, MD1 Antonio Álvarez, MD, PhD1 David Clofent, MD1 Mario Culebras, MD, PhD1 ML De Souza Galvão, MD1 Karina Loor, MD1 Eva Polverino, MD, PhD1
Author Affiliations:
1. Department of Respiratory Medicine, Vall d’Hebron University Hospital, Barcelona, Spain
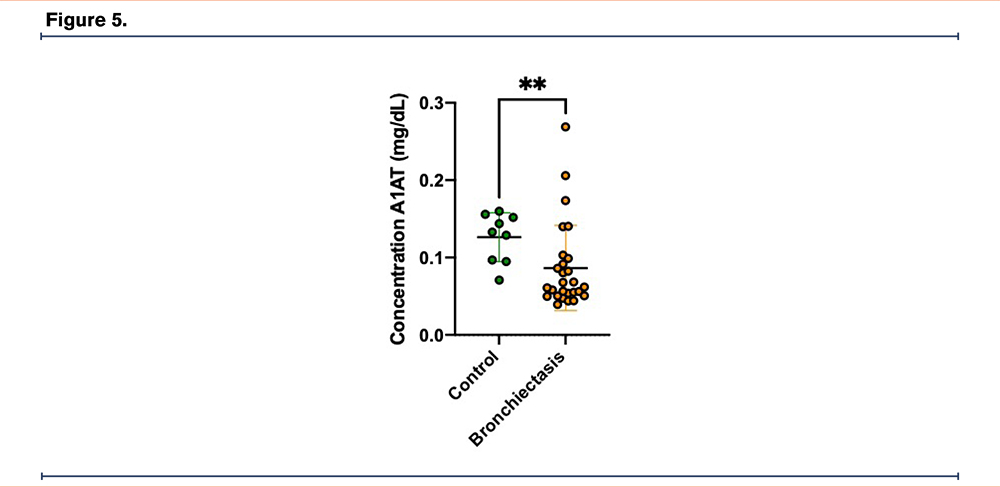
Background:
Bronchiectasis (BE) is a chronic disease characterized by persistent lung inflammation. AAT participates as one of the main lung proteins with anti-proteinase capacity, mainly targeting neutrophil elastase. Quantification of AAT in blood samples is widely used in both clinical practice and research, but little attention has been paid to clinical methods for evaluating AAT concentrations in sputum (AATs). The aim of this study was to validate an ELISA to measure AATs in samples collected from BE patients compared with healthy subjects.
Methods:
Spontaneous sputum samples were collected from 34 clinically stable BE patients, while induced sputum was obtained from a control group of 9 age-matched (±10yrs), healthy, non-smoking volunteers. Sputum samples were processed and the supernatant were frozen at -80°C. Quantification of AATs was measured by a sensitive sandwich ELISA (Hycult Biotech). All samples were diluted 5x with supplied dilution buffer according to the manufacturer’s recommendations. Statistical analysis of the data was carried out with GraphPad 9.0.1.
Results:
Standard curve was generated for concentrations between 0,00016 and 0,01 mg/dL. The sample dilution was appropriate, and samples showed concentrations within this range. The results obtained from the preliminary analysis of AATs concentration showed a significant difference between BE patients and controls (0.086 mg/dL vs 0.126 mg/dL; p = 0.005).
Conclusions:
These preliminary data of AAT quantification with ELISA technique in sputum can represent a base for future studies. Moreover, the lower AATs in BE, compared to controls, suggests that AAT could represent a useful biomarker and provide compelling information about pathophysiology of BE.
Bronchiectasis and Genetics—Abstract 6
Lung Function Differences in Primary Ciliary Dyskinesia: Radial Spoke (RSPH) vs DNAH5 Mutations
Kunal Jakharia, MD1 Maimoona Zariwala, PhD1 Kelli M. Sullivan, MPH1 Nicole Capps, DNP1 Lin Feng-Chang, PhD1 Lang Li, BA1 Margaret Leigh, MD1 Kenneth N. Olivier, MD, MPH1 Michael Knowles, MD1
Author Affiliations:
1. University of North Carolina, Chapel Hill, North Carolina, United States
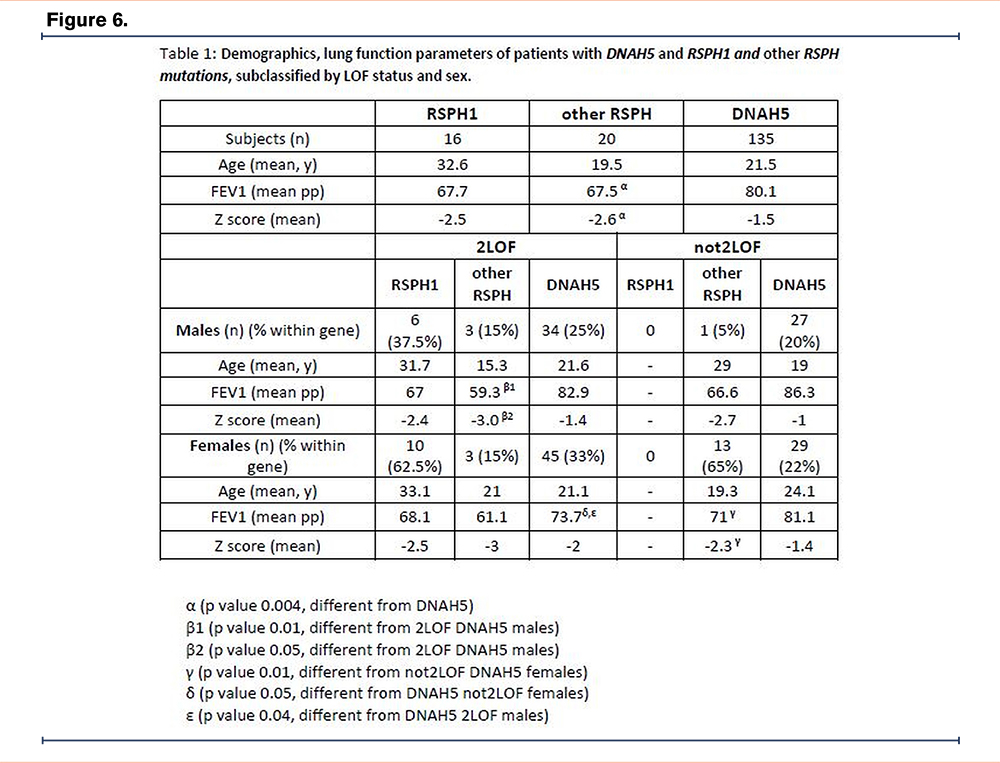
Background:
In Primary Ciliary Dyskinesia (PCD), a genetically heterogenous disorder, 2 loss of function (LOF) mutations could conceptually cause greater loss of ciliary and pulmonary function compared to those who do NOT have 2 LOF mutations. Mutations in RSPH1 have been reported to be associated with milder lung disease than other gene mutations (Knowles, M et al, AJRCCM 2014). We compared lung function in subjects with RSPH1 and non-RSPH1 (“other-RSPH”) radial spoke mutations to mutations in DNAH5 (most common PCD gene).
Methods:
Cross-sectional analysis was performed on demographic, spirometric, and genetic data from prospective studies by the Genetic Disorders of Mucociliary Clearance Consortium (GDMCC). Participants with pathogenic/likely pathogenic variants in RSPH1, other-RSPH and DNAH5 were subdivided by variant functionality: 2 LOF (both variants - LOF) and not2LOF (one or two variants - not LOF) subgroups and sex. FEV1 percent predicted (FEV1pp) and Z-scores (GLI reference) were compared between the groups and subgroups using statistical regression analysis, adjusting for age, sex and LOF.
Results (Table):
18 other-RSPH subjects had RSPH4A and one each had RSPH9 and RSPH3 mutations. There was no difference in FEV1 and Z-score between RSPH1 and DNAH5 group; other-RSPH group had significantly worse FEV1 and Z-score compared to DNAH5. 2LOF males and not2LOF females of other-RSPH group had lower FEV1 and Z-score compared to their DNAH5 counterparts. Within DNAH5, 2LOF females had worse FEV1 compared to not2LOF females and 2LOF males.
Conclusions:
Our data suggest that RSPH1 variants are not associated with milder lung disease than DNAH5. Subjects with non-RSPH1 mutation, mostly RSPH4A, had worse lung disease compared to those with DNAH5 mutation. We postulate, this may be due to factors that need further exploration including healthcare disparities among RSHP4A subjects. Along with the specific gene involved, sex and LOF status of the mutation also impacts lung function.
Bronchiectasis I—Abstract 7
The Clinical and Socioeconomic Burden of Bronchiectasis: Preliminary Results of A Systematic Literature Review
James D. Chalmers, MD, PhD1 Marcus Mall2 Pamela J. McShane, MD3 Kim G. Nielsen4 Michal Shteinberg, MD, PhD5 Sean D. Sullivan6 Sanjay H. Chotirmall, MD, PhD7
Author Affiliations:
1. Division of Molecular and Clinical Medicine, Ninewells Hospital, University of Dundee, Dundee, Scotland, United Kingdom
2. Charité – Universitätsmedizin Berlin, Berlin, Brandenburg, Germany
3. University of Texas Health Science Center at Tyler, Tyler, Texas, United States
4. Copenhagen University Hospital, Rigshospitalet, Copenhagen, Byen København, Denmark
5. Lady Davis Carmel Medical Center, Haifa, Israel
6. University of Washington, Seattle, Washington, United States
7. Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore
Background:
The overall burden of bronchiectasis (BE) continues to lack clarification even after the introduction of clinical care recommendations. A better understanding of the overall burden could support development of new therapies. We present preliminary findings of a systematic literature review (SLR) of the overall clinical and socioeconomic burden of BE across aetiologies and its associated diseases.
Methods:
Following PRISMA guidelines, Embase, MEDLINE and Cochrane Library were searched for publications relating to BE disease burden (December 2017–2022). Journal articles and congress abstracts reporting on observational studies, randomised controlled trials and registry studies were included, as well as editorials, narrative reviews and existing SLRs for the purpose of identifying primary studies. A reviewer screened all titles and abstracts to identify publications for full-text review, which were then screened for potential inclusion. A second reviewer verified both screening steps.
Results:
In total, 1624 publications were identified, of which 636 full texts were screened and 95 were included in this preliminary analysis. Of these, the majority (n=77) reported on non-cystic fibrosis BE, although few (n=18) reported on individual aetiologies and associated diseases. Commonly reported symptoms and complications included reduced lung function, exacerbations, cough, sputum, dyspnoea, haemoptysis and respiratory infections, with disease severity reported across several indices and mortality reported in several studies. BE impacted health-related quality of life across several patient-reported outcome measures and domains, with patients experiencing fatigue, anxiety and depression. Healthcare resource utilisation (HCRU; hospitalisations/readmissions/length of stay/annual hospital days) was considerable. Patients, health insurance companies and healthcare systems accrued substantial medical costs related to hospitalisations, treatments, and emergency department and outpatient visits. Indirect costs included sick pay and lost income.
Conclusions:
These preliminary results suggest that BE causes significant overall clinical and socioeconomic burden. Disease-modifying therapies that reduce symptoms, improve quality of life and reduce HCRU and costs are needed.
Bronchiectasis I—Abstract 8
Efficacy and Safety of Dipeptidyl Peptidase-1 (DPP-1) Inhibition in Long-Term Macrolide Users with Bronchiectasis: A Post-Hoc Analysis of the WILLOW Trial
Charles S. Haworth, MD1 Pamela J. McShane, MD2 Carlos Fernandez, MD, MPH, MBA3 Sebastian Fucile, PhD3 Melanie Lauterio, PhD3 Andrea Maes, PhD3 Ariel Teper, MD3 James D. Chalmers, MD, PhD4
Author Affiliations:
1. Royal Papworth Hospital and University of Cambridge, Cambridge, United Kingdom
2. University of Texas Health Science Center at Tyler, Tyler, Texas, United States
3. Insmed Incorporated, Bridgewater, New Jersey, United States
4. Division of Molecular and Clinical Medicine, Ninewells Hospital, University of Dundee, Dundee, Scotland, United Kingdom
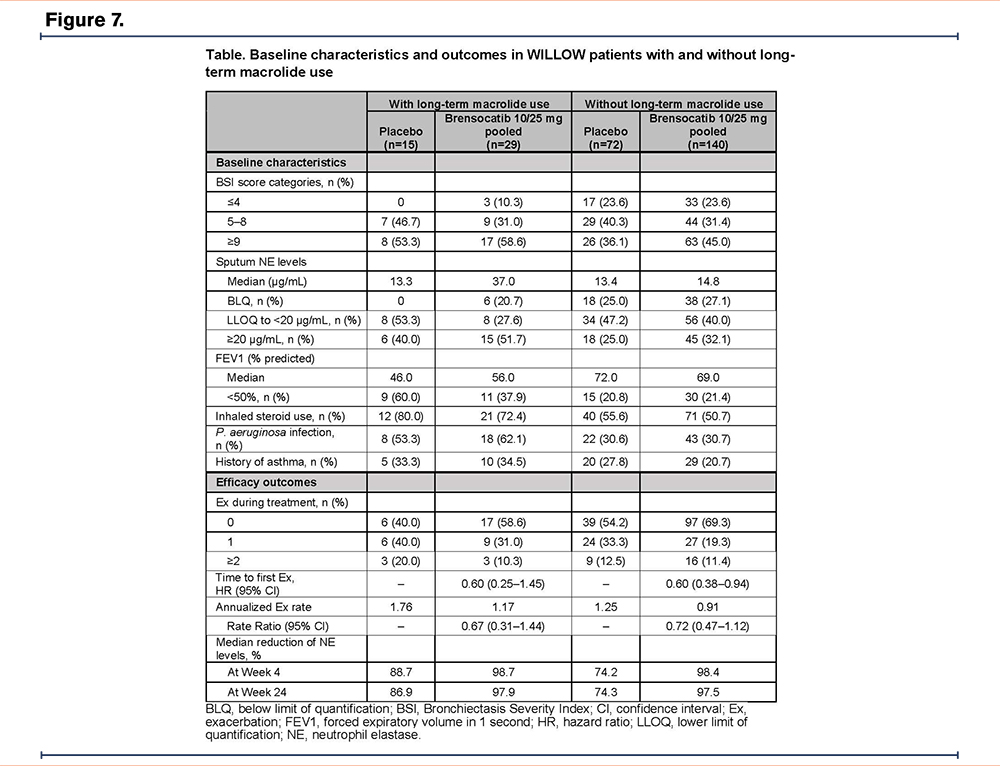
Background:
Neutrophil serine proteases, such as neutrophil elastase (NE), are activated by DPP-1 in the bone marrow. Brensocatib, a reversible DPP-1 inhibitor, prolonged time to first exacerbation vs placebo in non–cystic fibrosis bronchiectasis (NCFBE) patients in the phase 2 WILLOW trial (NCT03218917). Long-term macrolides are widely used and have been shown to reduce neutrophilic inflammation. The present post-hoc analysis compares patient characteristics and outcomes in WILLOW subgroups based on long-term macrolide use.
Methods:
Adult bronchiectasis patients received once-daily brensocatib (10 or 25 mg) or placebo. Patients on stable long-term macrolide therapy could be included in the trial. Endpoints included time to first exacerbation, annualized rate of pulmonary exacerbations, sputum NE changes, and treatment-emergent adverse events (TEAEs). Pooled results from brensocatib arms are presented.
Results:
Patients on long-term macrolide treatment (n=44) were more likely to have P. aeruginosa cultured from sputum, a higher background exacerbation rate, lower baseline FEV1, higher baseline levels of sputum NE, higher Bronchiectasis Severity Index (BSI) scores, a medical history of asthma, and inhaled steroid use than patients without long-term macrolide treatment (n=212) (Table). Brensocatib prolonged time to first exacerbation (hazard ratio 0.60 [95% CI: 0.25–1.45] in the macrolide subgroup; 0.60 [0.38–0.94] for the subgroup without macrolides) and reduced exacerbation rates in patients with and without long-term macrolide treatment (Table). Brensocatib led to greater median reductions of sputum NE levels vs placebo at Week 24 (Table). Similar TEAE rates were observed across all subgroups. The most common TEAEs across the pooled brensocatib arms were increased sputum, cough, and dyspnea.
Conclusions:
Consistent with overall WILLOW results, brensocatib prolonged time to first exacerbation and reduced exacerbation rates and sputum NE levels vs placebo regardless of long-term macrolide use, and was generally well tolerated with consistent safety signals. A confirmatory phase 3 trial (ASPEN; NCT04594369) is ongoing.
Bronchiectasis I—Abstract 9
The Efficacy and Safety of Colistimethate Sodium Delivered via the I-neb in Patients with Bronchiectasis and Pseudomonas Aeruginosa Infection: The PROMIS-I and PROMIS-II Randomised Controlled Trials
Charles S. Haworth, MD1 Michal Shteinberg, MD, PhD2 Kevin Winthrop, MD, MPH3 Alan Barker, MD3 Francesco Blasi, MD4 Aikaterini Dimakou, MD, PhD5 Lucy Morgan, BMed, PhD6 Anne E. O'Donnell, MD7 Felix C. Ringshausen8 Oriol Sibila9 Rachel Thomson, MBBS, PhD10 James D. Chalmers, MD, PhD11
Author Affiliations:
1. Royal Papworth Hospital and University of Cambridge, Cambridge, United Kingdom
2. Lady Davis Carmel Medical Center, Haifa, Israel
3. Oregon Health and Science University, Portland, Oregon, United States
4. Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico, Milan, Italy
5. Sotiria Thoracic Diseases Hospital of Athens, Attica, Athens, Greece
6. Concord Hospital, Sydney, New South Wales, Australia
7. Georgetown University Hospital, Washington, District of Columbia, United States
8. Medizinische Hochschule Hannover and Affiliation German Center for Lung Research (DZL), Hannover, Hannover, Germany
9. Hospital de la Santa Creu i Sant Pau, Barcelona, Spain
10. Gallipoli Medical Research Foundation, Greenslopes Private Hospital, Greenslopes, Queensland, Australia
11. Division of Molecular and Clinical Medicine, Ninewells Hospital, University of Dundee, Dundee, Scotland, United Kingdom
Background:
Bronchiectasis is a chronic debilitating condition with no approved treatments in which chronic Pseudomonas aeruginosa infection is associated with increased morbidity and mortality. The PROMIS-I and -II trials investigated the efficacy and safety of 12 months of inhaled colistimethate sodium delivered via the I-neb (CMS I-neb).
Methods:
Two randomised, double-blind, placebo-controlled trials of twice daily CMS I-neb (delivered dose 0.3ml of 1 MIU in 1ml 0.45% saline) vs placebo (0.3ml 0.45% saline) were conducted in patients with P. aeruginosa and a history of at least 2 exacerbations requiring oral antibiotic treatment or 1 requiring IV antibiotics in the previous year. The primary endpoint was the mean annualised exacerbation rate (AER).
Results:
In PROMIS-I, the AER was 0.58 in CMS I-neb vs 0.95 in placebo treated patients (rate ratio (RR) 0.61 95% CI 0.46-0.82, p=0.00101). Use of CMS I-neb was also associated with significant improvements in time to first exacerbation, severe exacerbations and quality of life (SGRQ). In PROMIS-II, there was no difference in the AER between CMS I-neb and placebo patients (0.89 vs 0.89, RR 1.0 95% CI 0.75-1.35, NS). As PROMIS-II was conducted predominantly during the COVID-19 pandemic (in contrast to PROMIS-I), the impact of the pandemic was investigated in post hoc analyses. Pre-pandemic (before 11th March 2020), the AER in PROMIS-II was 0.92 in CMS I-neb vs 1.26 in placebo patients, RR 0.73 95% CI 0.49-1.08; whereas during the pandemic period, the AER was 0.87 in CMS I-neb vs 0.62 in placebo patients, RR 1.40 95% CI 0.93-2.13. Similar reductions in P. aeruginosa density were seen in both trials (p<0.00001). Rates of AEs and SAEs were similar between treatment arms in both trials.
Conclusions:
The data from PROMIS-I and the pre-pandemic period of PROMIS-II demonstrate the efficacy of CMS I-neb in patients with bronchiectasis and P. aeruginosa.
Bronchiectasis I—Abstract 10
Airway Pathogen Trends: A Look at the US Bronchiectasis Research Registry
Meghan Marmor, MD1 Amanda E. Brunton, MPH2 Radmila Choate, PhD, MPH3 Nicole Lapinel, MD4 Restrepo I. Marcos, MD, MSc, PhD5 Christopher Richards, MD6 Stephen Ruoss, MD7 George M. Solomon, MD8 Kevin Winthrop, MD, MPH9 Mark L. Metersky, MD10
Author Affiliations:
1. Stanford University, Palo Alto, California, United States
2. COPD Foundation, Miami, Florida, United States
3. University of Kentucky, Lexington, Kentucky, United States
4. Louisiana State University, New Orleans, Louisiana, United States
5. University of Texas Health at San Antonio, San Antonio, Texas, United States
6. Mass General, Boston, Massachusetts, United States
7. Stanford University School of Medicine, Palo Alto, California, United States
8. University of Alabama at Birmingham, Birmingham, Alabama, United States
9. Oregon Health and Science University, Portland, Oregon, United States
10. University of Connecticut School of Medicine, Farmington, Connecticut, United States
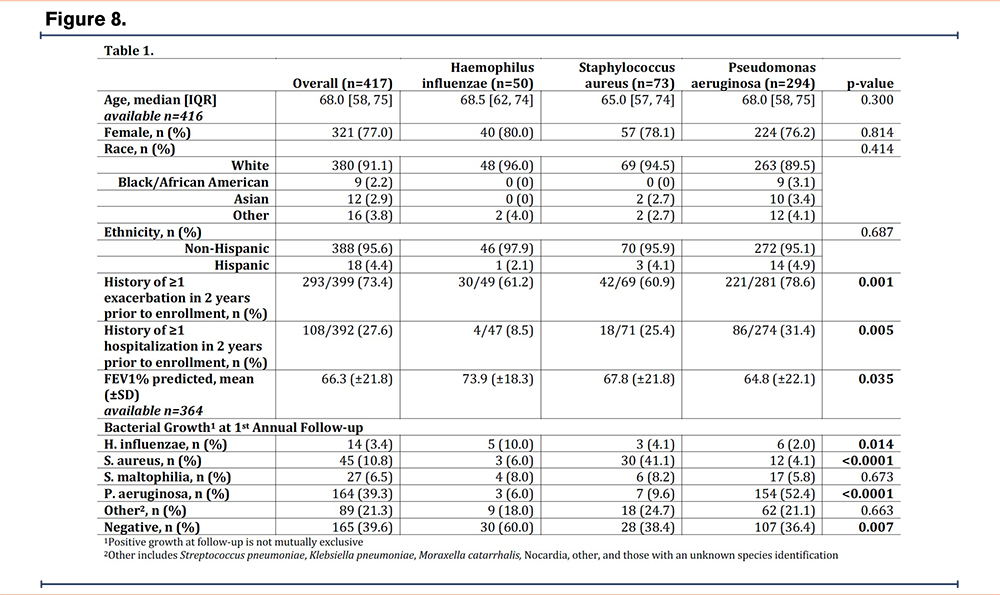
Background:
Bronchiectasis is characterized by alterations of the airway microbiome. We investigated changes in airway pathogen recovery in sputum cultures over time among adult patients with bronchiectasis.
Methods:
Using data from the US Bronchiectasis and NTM Research Registry (BRR), we identified individuals with bronchiectasis (excluding cystic fibrosis) with at least 1 sputum culture for Haemophilus influenzae, Pseudomonas aeruginosa or Staphylococcus aureus at baseline, and at least 1 year of follow-up culture data. Patients on treatment for NTM or who isolated other bacterial pathogens were excluded.
Results:
Of the 5346 patients in the BRR, 417 patients met the study inclusion criteria. At baseline, 294 patients (70.5%) were colonized with Pseudomonas, 50 (12%) with Haemophilus, and 73 (17.5%) with Staphylococcus. There were no significant between-group demographic differences. Pseudomonas group had the lowest FEV1 at baseline and the greatest burden of exacerbations and hospitalizations in the two years prior to enrollment compared to other groups (Table 1).
At 1 year, 154 (52%) of Pseudomonas patients had culture persistence; 107 (36%) had negative sputum cultures, and the remaining isolated other airway pathogens. In the Haemophilus group, 5 (10%) had culture persistence; 30 (60%) had negative sputum cultures and 5 (10%) isolated Pseudomonas. In the Staphylococcus group, 30 (41%) had culture persistence, 28 (38%) had negative sputum cultures and 9 (12%) isolated Pseudomonas.
Conclusions:
Airway pathogen presence in bronchiectasis changes over time. At 1-year, most patients initially infected with Haemophilus were no longer infected with this organism, and very few Haemophilus or Staphylococcus patients went on to isolate Pseudomonas. While half of patients infected with Pseudomonas had culture persistence, one third had negative cultures by 1 year. Additional investigation is needed to understand factors involved in these microbiome changes, including possible contributions from antibiotic exposure and underlying lung function.
Acknowledgements
The authors would like to acknowledge the COPD Foundation, a 501(c)(3) nonprofit organization, who manages the Bronchiectasis and NTM Research Registry. The Registry is funded by the Richard H. Scarborough Bronchiectasis Research Fund, the Anna-Maria and Stephen Kellen Foundation, a Research Grant from Insmed Incorporated, and the Bronchiectasis and NTM Industry Advisory Committee. Also, this work would not be possible without comprehensive chart reviews and data recording by the dedicated research coordinators and PIs at each participating Registry site.
Bronchiectasis I—Abstract 11
Bronchiectasis with Chronic Rhinosinusitis is Associated with Non-Allergic Eosinophilic Airway Inflammation and is Distinct from Asthma
Michal Shteinberg, MD, PhD1 James D. Chalmers, MD, PhD2 Jayanth K. Narayana, PhD3 Alison J. Dicker, PhD4 Sanjay H. Chotirmall, MD, PhD3 Michal A. Rahat, PhD5 Elina Simanovitch, MSc5 Lucy Bidgood2 Shai Cohen, MD, PhD6 Nili Stein, MSc7 Nizar Abo-Hilu, MD6 James Abbott2 Sharon Avital, MSc8 Einat Fireman-Klein, MD8 Hollian J.I. Richardson, PhD2 Emad Muhammad, PhD9 Jenny Jrbashyan, MD10 Sonia Schneer, MD8 Najwan Nasrallah, MD11 Iya Eisenberg, MD11 Yochai Adir12
Author Affiliations:
1. Lady Davis Carmel Medical Center, Haifa, Israel
2. Division of Molecular and Clinical Medicine, Ninewells Hospital, University of Dundee, Dundee, Scotland, United Kingdom
3. Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore, Singapore
4. Division of Molecular and Clinical Medicine, University of Dundee, Dundee, Scotland, United Kingdom
5. Immunotherapy Laboratory, Carmel Medical Center and the Technion - Israel Institute of Technology, Haifa, Israel
6. Allergy and Immunology Unit, Carmel Medical Center and Lin Medical Center, Haifa, Israel
7. Community Medicine and Epidemiology Department, Carmel Medical Center, Haifa, Israel
8. Pulmonology Institute, Carmel Medical Center, Haifa, Israel
9. Hematology Laboratory, Carmel Medical Center, Haifa, Israel
10. ENT Department, Carmel Medical Center, Haifa, Israel
11. Radiology Department, Carmel Medical Center, Haifa, Israel
12. Pulmonology Institute, Carmel Medical Center and the Technion - Israel Institute of Technology, Haifa, Israel
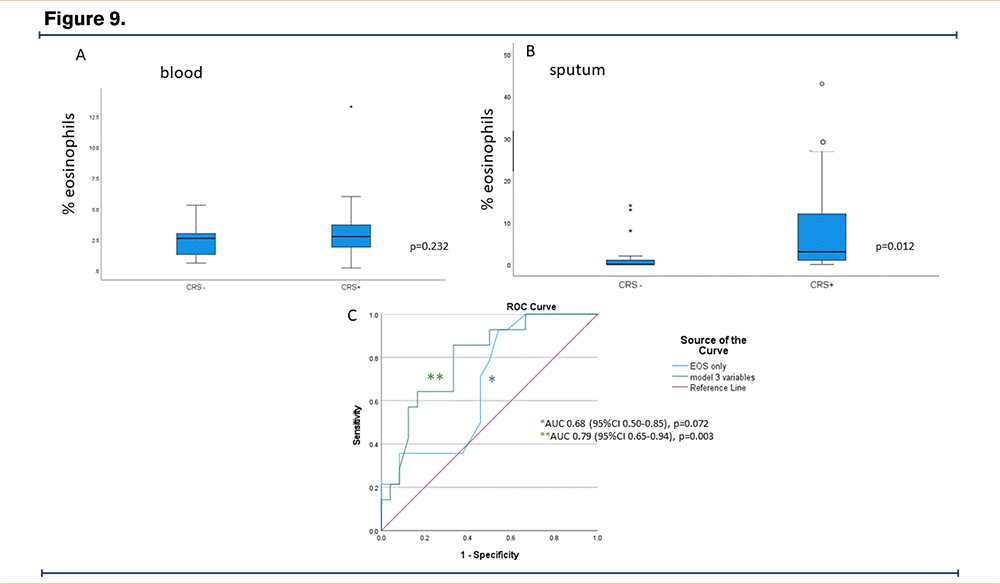
Background:
Bronchiectasis is an airway inflammatory disease frequently associated with chronic rhinosinusitis (CRS)- a disease characterized by eosinophilic inflammation. An eosinophilic endotype of bronchiectasis has recently been described, but detailed testing to differentiate eosinophilic bronchiectasis from asthma has not been performed.
We aimed to explore clinical, microbiological, and inflammatory phenotypes among patients with bronchiectasis with CRS in comparison with bronchiectasis alone.
Methods:
People with idiopathic or post-infectious bronchiectasis were assessed for concomitant CRS. We excluded people with asthma, PCD, and smokers. During stble state, we assessed sputum and blood cell counts, nasal NO and fractional excreted NO (FeNO), methacholine reactivity, skin allergy testing, total IgE, reactive immunoallergen testing (RAST), inflammatory cytokines in sputum and serum, and microbiome in sputum and nasal brushing.
Results:
22 people with CRS (BE+CRS) and 17 without CRS (BE-CRS) were included. Sex, age, Reiff score, and bronchiectasis severity were similar between groups. Median (IQR) sputum eosinophil percentages were 0 (0-1.5)% in BE-CRS, and 3(1-12)% in BE+CRS (p=0.012). Blood eosinophil counts were predictive of sputum eosinophil counts (AUC 0.68, 95% CI 0.50-0.85), and inclusion of a CRS diagnosis and SNOT-22 questionnaire score improved prediction (AUC 0.79 (95%CI 0.65-0.94). Methacholine tests were negative in 85.7% BE-CRS and 85.2% BE+CRS (p>0.99). Specific IgE and skin testing were similar between the groups, and FENO levels were <20 ppB in both groups, without a difference. Microbiome analysis demonstrated distinct microbiota in nasopharyngeal and airway samples in both BE+CRS and BE-CRS without significant differences between groups, however, interactome analysis revealed altered interactomes in individuals with high sputum eosinophils and CRS.
Conclusion:
Bronchiectasis with CRS is associated with an eosinophilic, non-allergic airway inflammation that is distinct from asthma.
Bronchiectasis II—Abstract 12
Bacterial Coinfection is Related to the Severity and Clinical Course as Bronchiectasis in Patients with Mycobacterium Avium Complex Pulmonary Disease
Masashi Ito1 Koji Furuuchi1 Keiji Fujiwara1 Fumiya Watanabe2 Tatsuya Kodama1 Fumiko Uesugi1 Yoshiaki Tanaka1 Takashi Yoshiyama1 Atsuyuki Kurashima1 Ken Ohta1 Kozo Morimoto, MD, PhD1
Author Affiliations:
1. Respiratory Disease Center, Fukujuji Hospital, Japan Anti-Tuberculosis Association (JATA), Kiyose, Tokyo, Japan
2. Department of Pharmacometrics and Pharmacokinetics, Meiji Pharmaceutical University, Kiyose, Tokyo, Japan
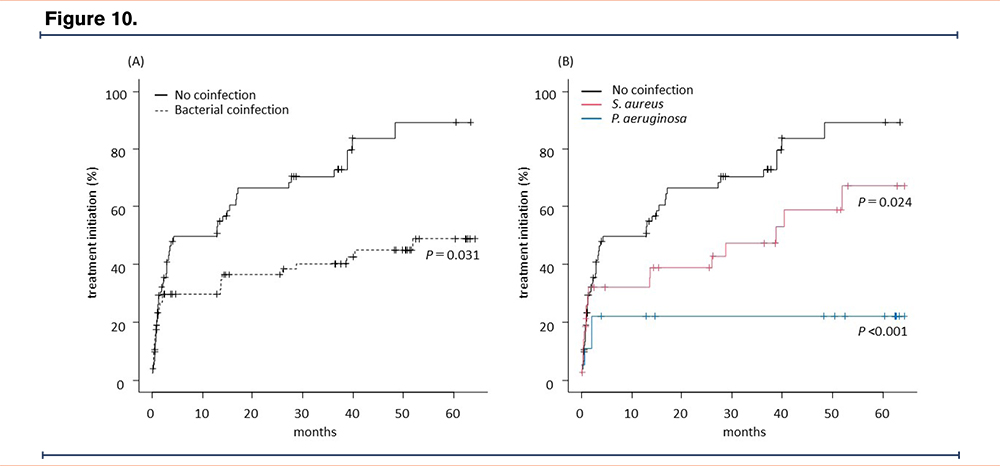
Background:
Bacterial coinfections are observed in 19 – 66% of patients with Mycobacterium avium complex pulmonary disease (MAC-PD) during the entire duration of the disease. The impact of bacterial coinfection (BC) at diagnosis on the clinical course of MAC-PD has not been reported.
Methods:
Among 558 patients diagnosed with MAC-PD between January 2016 and December 2020, 218 patients who underwent sputum culture tests twice or more within one year before and after diagnosis were included. We compared the patient characteristics and disease courses between the patients who had the same bacterial species detected twice or more (BC group) and those who never had bacteria cultured (no coinfection group).
Results:
We included 70 patients in the BC group and 74 in the no co-infection (NC) group. The sputum acid-fast bacilli smear-positive rate in the BC group was lower than in the NC group (35.7% vs. 56.8%, P =0.013). During the median follow-up period of 42 months (interquartile range [IQR]: 16.5 – 55 months), patients in the BC group were more likely to accomplish spontaneous sputum conversion of MAC (18.6% vs. 6.8%, P =0.044). The treatment initiation rate for MAC-PD in the BC group was lower than that in the NC group (41.4% vs. 67.6%, P =0.003). In contrast, the time to the first bronchiectasis exacerbation in the BC group was shorter than in the NC group, and the frequency of bronchiectasis exacerbations was higher in the BC group. In the radiological findings, BC correlate with a high Reiff score (p=0.045) and are not associated with cavitary lesions (p=0.852).
Conclusions:
Patients with BC at diagnosis have less disease severity in MAC-PD and are more likely to develop bronchiectasis exacerbation. It is important to treat the patients with BC as bronchiectasis, not only as MAC-PD.
Bronchiectasis II—Abstract 13
Preliminary Baseline Data from the Phase 2 Airleaf™ Trial of the Novel Cathepsin C Inhibitor BI 1291583 in Adult Patients with Non-Cystic Fibrosis Bronchiectasis
Pamela J. McShane, MD1 Sanjay H. Chotirmall, MD, PhD2 Anne E. O'Donnell, MD3 Naoki Hasegawa4 Michal Shteinberg, MD, PhD5 Henrik Watz6 Edith Frahm7 Li Ling8 Wiebke Sauter9 James D. Chalmers, MD, PhD10
Author Affiliations:
1. University of Texas Health Science Center at Tyler, Tyler, Texas, United States
2. Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore, Singapore
3. Georgetown University Hospital, Washington, District of Columbia, United States
4. Department of Infectious Diseases, Keio University, Tokyo, Japan
5. Lady Davis Carmel Medical Center, Haifa, Israel
6. Pulmonary Research Institute, LungenClinic, Airway Research Center North (ARCN) (DZL), Grosshansdorf, Germany
7. Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim, Germany
8. Boehringer Ingelheim (China) Investment Corporation Limited, Shanghai, China
9. Boehringer Ingelheim International GmbH, Biberach, Germany
10. Division of Molecular and Clinical Medicine, Ninewells Hospital, University of Dundee, Dundee, Scotland, United Kingdom
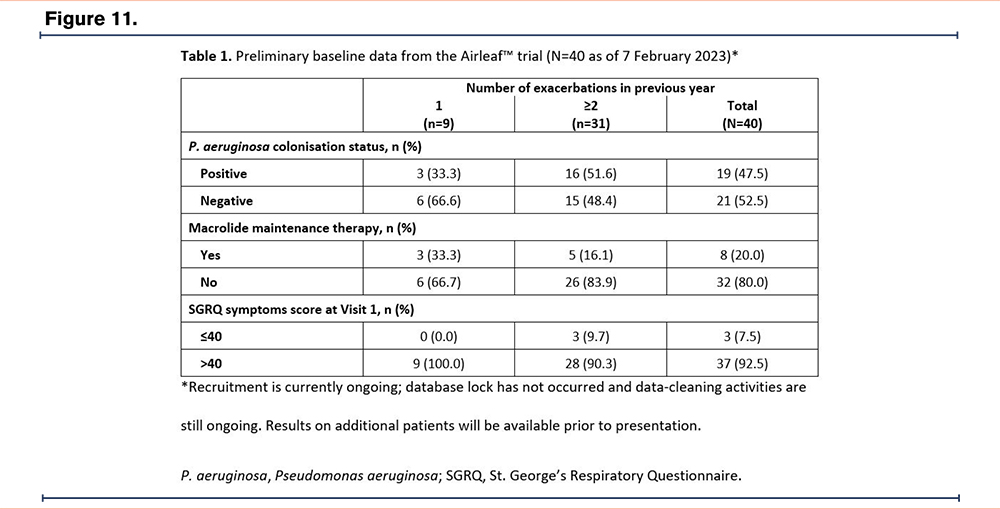
Background:
Bronchiectasis is a heterogenous lung disease characterised by chronic neutrophilic inflammation and an imbalance between neutrophil serine proteases (NSPs) and their antiproteases. As NSPs are activated by cathepsin C (CatC), inhibition of CatC is expected to reduce inflammation in the lungs of patients with bronchiectasis. BI 1291583 is a novel CatC inhibitor being investigated in the Phase 2 Airleaf™ trial in patients with bronchiectasis.
Methods:
Airleaf™ is a randomised, double-blind, placebo-controlled trial in which approximately 240 patients with bronchiectasis of multiple aetiologies will be randomised to one of three once-daily doses of BI 1291583 or placebo. The trial comprises a treatment period of 24–48 weeks and a follow-up period of 4 weeks. The primary endpoint is time to first pulmonary exacerbation, and the key secondary endpoint is the rate of pulmonary exacerbations (number of events per patient-time), both up to Week 48. Patients are required to have CT-confirmed bronchiectasis and a history of pulmonary exacerbations requiring antibiotic treatment (≥2 exacerbations in the past year or one exacerbation and severe symptoms indicated by a St. George’s Respiratory Questionnaire [SGRQ] symptoms score >40).
Results:
As of 7 February 2023, 40 patients with the following aetiologies have been recruited: idiopathic (n=14), asthma (n=12), COPD (n=7), post-infectious (n=4) and primary ciliary dyskinesia (n=4). Patients experienced 1 (n=9), 2 (n=17) or 3 (n=12) or ≥4 (n=2) exacerbations in the year prior to trial entry. Baseline clinical data can be seen in Table 1. A total of 33.3% and 51.6% of patients who experienced 1 or ≥2 exacerbations in the previous year, respectively, were positive for Pseudomonas aeruginosa, whereas 33.3% and 16.1% were receiving macrolide therapy. Most patients (92.5%) had an SGRQ symptoms score >40.
Conclusions:
Recruitment into Airleaf™ is ongoing and the trial is expected to conclude in Q1 2024.
Bronchiectasis II—Abstract 14
Evidence for Respiratory Pathogens in Culture Independent Data from Non-CF Bronchiectasis
Shivani Singh, MD, PhD1 Fares Darawshy1 Kirby Erlandson1 Kelsey Krolikowski1 Destiny Collazo1 Isabella Atandi1 Yonghua Li1 Miao Chang1 Ashwin Basavaraj, MD2 David Kamelhar, MD1 Doreen J. Addrizzo-Harris, MD1 Benjamin Wu, MD1 Leopoldo Segal, MD1
Author Affiliations:
1. NYU Langone Health, New York, New York, United States
2. NYU Grossman School of Medicine, New York, New York, United States
Background:
The lower airway microbiome is complex and culture independent techniques offer a new approach to identification of potential pathogens. Here, we investigated whether culture independent approaches can help understand the lower airway microbial environment in non-CF bronchiectasis.
Methods:
Patients with bronchiectasis underwent clinically indicated bronchoscopies. Samples (upper/ lower airways and background controls) underwent 16S rRNA gene sequencing (MiSeq) and were analyzed with QIIME2, PhyloSeq and EdgeR.
Results:
In a cohort of 200 patients, 94 (47%) had non-tuberculous mycobacterial (NTM) isolation while the others did not. In the NTM– group, Pseudomonas was the most frequently recovered respiratory pathogen via culture techniques (15.7%). Within the NTM+ group, 66.7% of the lower airway samples showed identification of a secondary respiratory pathogen in the 16S rRNA sequencing data whereas only 44% of the subjects grew a secondary pathogen by standard culture techniques. Within the NTM- group, 50% of the lower airway samples showed identification of a secondary respiratory pathogen in the 16S rRNA sequencing data. Importantly, within the subjects with bronchiectasis deemed to have negative cultures (both for NTM and for typical respiratory pathogens), a large proportion had microbial DNA identified as potential respiratory pathogens. In the NTM+ group without other respiratory pathogens by culture, a high exacerbation rate (≥2) was associated with a low alpha diversity. In these patients, the culture independent 16S rRNA sequencing approach identified potential respiratory pathogens in 57% of the subjects. Importantly, in the NTM- group, high rates of exacerbations were associated with enrichment with Pseudomonas and Moraxella.
Conclusions:
These data suggest that culture independent approaches may uncover the presence of potential respiratory pathogens that might not be suspected based on standard culture techniques.
Eosinophilic Bronchiectasis—Abstract 15
Case Series: The Use of Biologics in Eosinophilic Bronchiectasis
Carina Iskandir, MD1 Tejas Shah, MD1 Gail Schattner, MD1 Ashwin Basavaraj, MD1
Author Affiliations:
1. NYU Grossman School of Medicine, New York, New York, United States
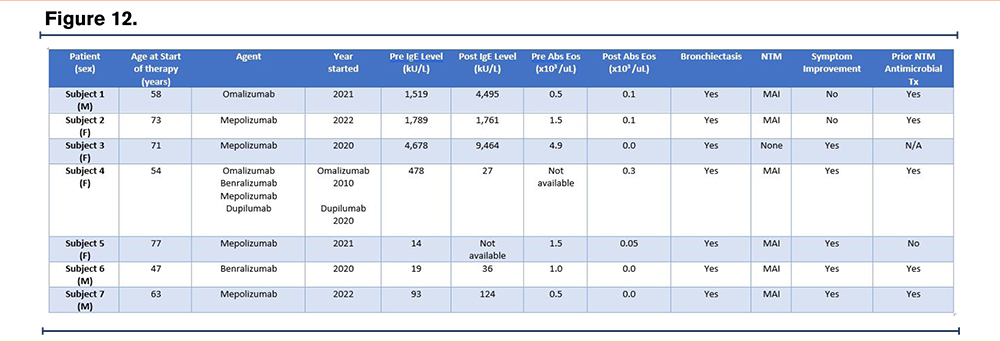
Background:
The inflammatory pathways which lead to airway inflammation, mucus production and bronchospasm in asthma are involved in the pathogenesis of non-cystic fibrosis bronchiectasis. The increasing use of biologics and their favorable side effect profile have led clinicians to expand their use to other airway diseases potentially mediated by the TH2 pathway. This case series outlines the use of biologics in the increasingly recognized entity of eosinophilic bronchiectasis.
Methods:
This series includes seven adult subjects from a single center with non-cystic fibrosis bronchiectasis with symptoms of productive cough, wheezing and dyspnea composed of 4 females and 3 males with a median age of 63 years. All subjects had markers of TH2 pathway activation. Eighty-six percent of subjects had a minimum absolute eosinophil count of 500 eosinophils/microL at baseline and the remainder had an elevated IgE level. Biologics were initiated in five of the six subjects who had concomitant MAI pulmonary infections as they did not respond sufficiently to guideline-based MAI treatment. All subjects with available data had a decline in peripheral absolute eosinophil count with seventy-one percent experiencing improvement in respiratory symptoms. In this small sample no negative side effects were observed.
Results:
Until recently bronchiectasis was thought to be a disease of irreversible airway damage mediated by neutrophilic inflammation. However, a subset of these patients has elevated sputum eosinophils, peripheral eosinophilia and even abnormal exhaled nitric oxide testing. This has been linked to increased exacerbation risk and severity. In this heterogenous disease in which the interplay of immune dysregulation and infection leads to progressive lung destruction, biologic therapy is a novel approach of addressing the inflammatory pathway upstream. We demonstrate the successful use of this class of medications in such patients.
Conclusions:
Biologics in eosinophilic bronchiectasis may be a viable and safe treatment option which warrants further investigation
Eosinophilic Bronchiectasis—Abstract 16
The Effects of Endoscopic Sinus Surgery on Upper and Lower Airway Health in Patients with Non Cystic Fibrosis Bronchiectasis
Joseph Z. Lebowitz, MD1 Seth Lieberman, MD1 Gail Schattner, MD1 Ashwin Basavaraj, MD1 Yan Zhang, PhD1
Author Affiliations:
1. NYU Grossman School of Medicine, New York, New York, United States
Background:
Chronic rhinosinusitis (CRS) and bronchiectasis are often comorbid conditions. The unified airway theory suggests that upper and lower airway physiology are intimately linked and pathology affecting one negatively affects the other. This study aims to determine the effects of endoscopic sinus surgery (ESS) on upper and lower airway health in patients age >18 with non-cystic fibrosis (CF) bronchiectasis.
Methods:
This is a retrospective case series of adult patients at NYU Langone with a diagnosis of non-CF bronchiectasis who have undergone endoscopic sinus surgery (ESS). Medical records of the 9 enrolled patients were reviewed in the 6-24 month period before and after ESS; all data is retrospective and between October 1, 2015 and December 19, 2022. The primary outcome is the number of lower airway exacerbations requiring medical management or hospitalization (in the 24 months pre- and post- ESS). Secondary outcomes include pre and post-operative: sputum cultures / BAL, sinus cultures, pulmonary function tests (PFTs; FEV1, FVC, FEV1/FVC), CT scan changes in mucoid impaction or bronchiolitis and quality of life as measured by St. George's Respiratory Questionnaire.
Results:
Statistical analysis is ongoing, however, preliminary data shows, on average, a decrease in bronchiectasis exacerbations requiring antibiotics and / or steroids and those requiring hospitalizations in the observed post-operative period.
Conclusions:
Prior studies have examined the effects of ESS in patients with bronchiectasis, however this literature is lacking in two important ways. First, it does not distinguish between patients based on the etiology of their bronchiectasis; our study focuses on patients with non-CF bronchiectasis. Second, the existing literature looks at objective outcomes pre and post-ESS such as culture data and PFTs, however this study demonstrates how this translates to clinical improvement for the patient; namely decreases in both bronchiectasis exacerbation requiring outpatient medical management and hospitalization.
Eosinophilic Bronchiectasis—Abstract 17
Monoclonal Antibodies for Treatment of ABPA
Dimple Shah, MD1 Harry Steinberg, MD2 Ilana Borukhov, PA-C1 Jonathan Ilowite, MD2 Mina Makaryus, MD2 Effie Singas, MD2
Author Affiliations:
1. Northwell Health, Manhasset, New York, United States
2. Northwell, New Hyde Park, New York, United States
Background:
Allergic bronchopulmonary aspergillosis (ABPA) is a disorder defined by clinical, immunologic and radiologic criteria. Diagnosis requires the presence of a predisposing condition such as asthma or cystic fibrosis, a positive aspergillus skin test or elevated IgE against A. fumigatus (Af) and a total IgE > 1000 Iu/mL. Supportive criteria include IgG against Af, radiographic features consistent with ABPA and a blood eosinophil count of > 500 cell/L.
Treatment includes corticosteroids, oral/nebulized antifungal medications, and more recently, monoclonal antibodies (MAB).
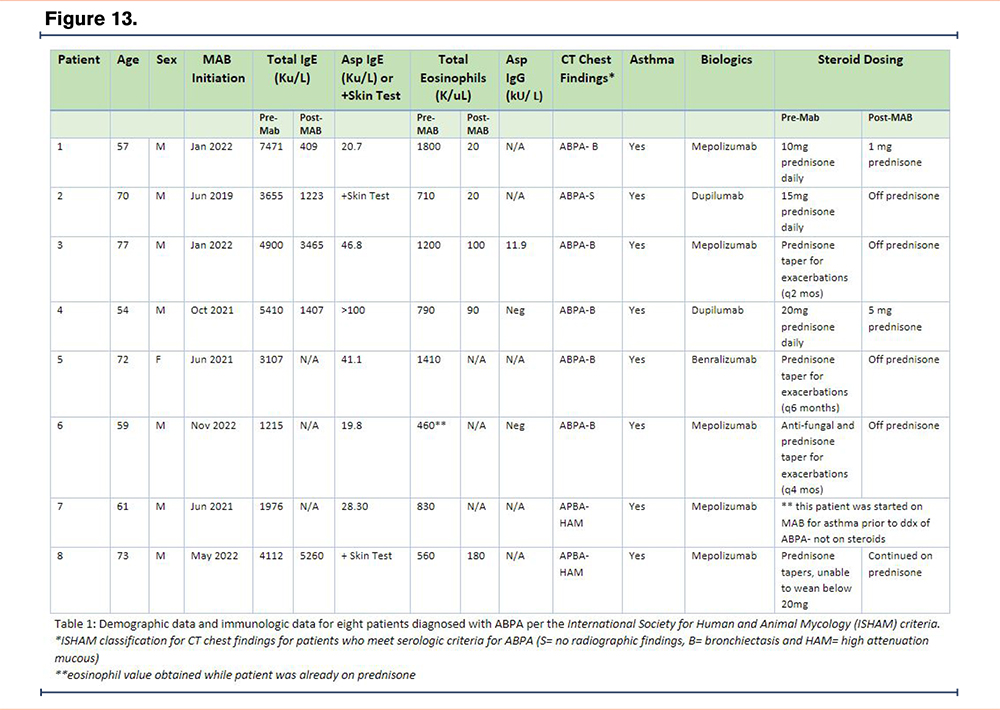
Methods:
We report 8 patients with ABPA (per ISHAM definition) who are being treated with MABs (see table 1). All patients had been diagnosed with asthma prior to their diagnosis of ABPA and have been treated with either mepolizumab (5 patients) or benralizumab (1 patient) (IgG antibody against interleukin (IL) -5), or dupilumab (2 patients) (IgG antibody against Il-4 and Il-13) for >4 months. Seven out of the eight patients had required daily or frequent (>3 exacerbations / year) use of systemic steroids. Six out of seven patients demonstrated reduction or cessation in steroid use after MAB initiation. One patient was started on MAB for severe persistent asthma prior to ABPA diagnosis.
Results:
Immune-mediated pathogenesis of ABPA remains incompletely understood. Af elicits a polyclonal antibody response as evidenced by elevated Af-IgE and IgG as well as a TH2 mediated response which generates Il -4, 5 and 13. The immune response increases both peripheral and bronchial eosinophils and IgE leading to chronic inflammation and airway damage. Corticosteroids and antifungals have been the mainstay of treatment, however recent data suggests that MABs against IgE, Il- 4, Il-5 and Il-13 can be effective as steroid sparing alternatives.
Conclusions:
ABPA should be suspected in patients with persistent asthma despite standard management, and steroid dependent patients should be considered for MAB therapy.
Epidemiology I—Abstract 18
Survival Outcomes in US Medicare Patients with Bronchiectasis by Rate of Baseline Exacerbations
Joseph Feliciano, PharmD, MS1 Benjamin Lewing, PhD2 Maitreyee Mohanty, PhD3 Melanie Lauterio, PhD3 Sebastian Fucile, PhD3 Joseph Tkacz, PhD2 Alan Barker, MD4
Author Affiliations:
1. Insmed Incorporated, Philadelphia, Pennsylvania, United States
2. Inovalon, Bowie, Maryland, United States
3. Insmed Incorporated, Bridgewater, New Jersey, United States
4. Oregon Health and Science University, Portland, Oregon, United States
Background:
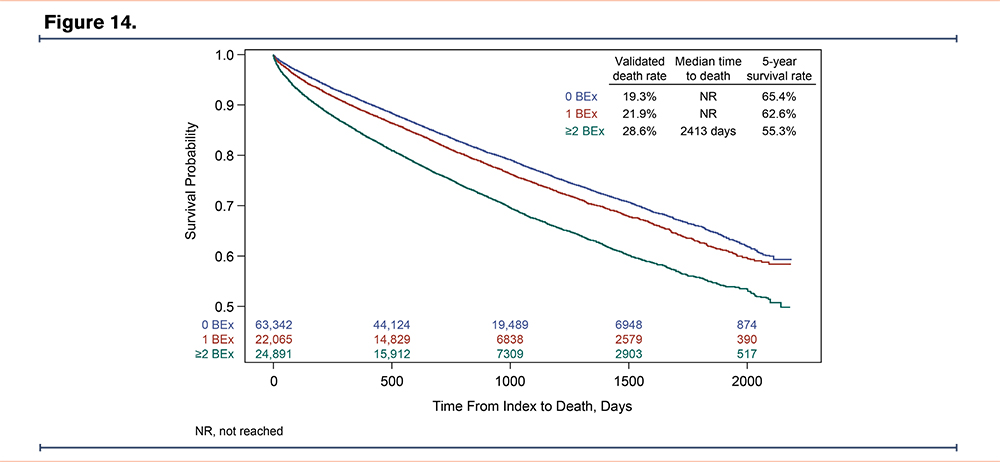
Bronchiectasis (BE) is associated with chronic respiratory inflammation and recurrent BE exacerbations (BEx). Greater frequency of BEx (≥2/year) is associated with declining lung function and increased mortality. This study aimed to assess differences in clinical characteristics and overall survival between patients with BE by rate of baseline BEx.
Methods:
This was a retrospective study of patients with a diagnosis of BE (≥1 inpatient or ≥2 outpatient claims with an ICD-9/ICD-10 diagnosis code for BE, or 1 outpatient claim with a BE diagnosis and chest CT scan) in the 100% Medicare fee-for-service database (Jan 2014-Dec 2020). All patients had continuous enrollment ≥12 months pre-index (baseline) and ≥12 months post-index (follow-up). The index date was set to a random BE claim preceded by ≥1 year of BE disease history. Patients were segmented by number of BEx during baseline (0, 1, or ≥2). The follow-up rate of BEx (per-year) and mortality were assessed for each baseline BEx group. Time to death from index was estimated by Kaplan-Meier analyses.
Results:
In total, 92,529 patients with BE were identified; demographics were similar across groups: 0 BEx (n=54,258 [58.6%]; mean [SD] age, 76.7 [8.7] years; 70.9% female); 1 BEx (n=18,427 [19.9%]; 76.5 [8.8]; 74.0%); ≥2 BEx (n=19,844 [21.4%]; 76.1 [9.3]; 74.5%). BEx during follow-up were common, with 21.6% of all patients presenting ≥2 BEx (mean [SD] rate of BEx, 0.98 [2.07]), and increased with the number of baseline BEx: 0 BEx (11.4% with ≥2 BEx; mean [SD] rate of BEx, 0.51 [0.92]); 1 BEx (24.2%; 1.00 [0.77]); ≥2 BEx (46.8%; 2.23 [1.85]). Time to death was shorter in patients with a greater rate of baseline BEx (Figure).
Conclusions:
In this BE patient cohort, BEx were relatively common with history of BEx associated with future BEx, and a higher BEx rate associated with increased all-cause mortality.
Epidemiology I—Abstract 19
Treatment Patterns Among Patients with Bronchiectasis by Baseline Exacerbations
Joseph Feliciano, PharmD, MS1 Maitreyee Mohanty, PhD2 Joseph Tkacz, PhD3 Benjamin Lewing, PhD3 Melanie Lauterio, PhD2 Alan Barker, MD4
Author Affiliations:
1. Insmed Incorporated, Philadelphia, Pennsylvania, United States
2. Insmed Incorporated, Bridgewater, New Jersey, United States
3. Inovalon, Bowie, Maryland, United States
4. Oregon Health and Science University, Portland, Oregon, United States
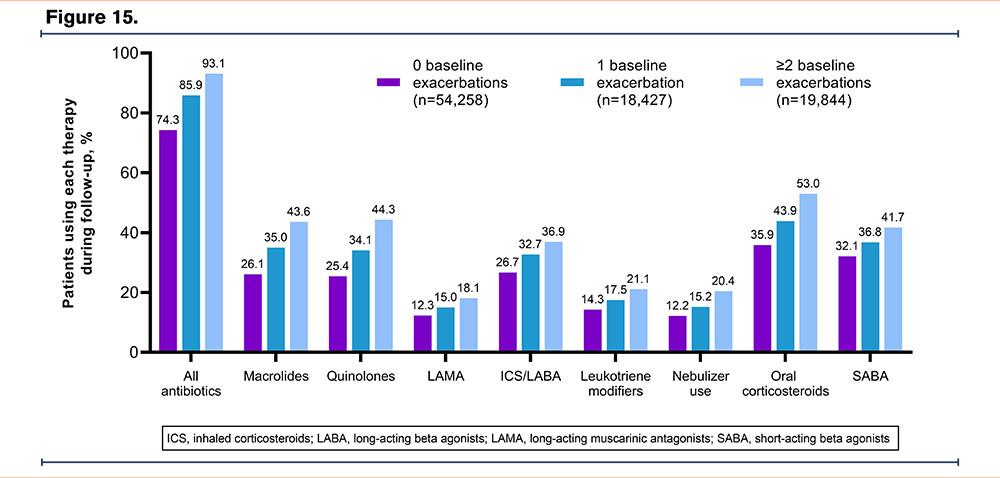
Background:
Patients with bronchiectasis (BE) often experience BE exacerbations (BEx) but data on how these are treated in the real-world are limited. The objective of this study was to assess treatment patterns in patients with BE by baseline BEx.
Methods:
A retrospective study of patients with a diagnosis of BE (≥1 inpatient or ≥2 outpatient claims with an ICD-9/ICD-10 diagnosis code for BE, or 1 outpatient claim with a BE diagnosis and chest CT scan) in the 100% Medicare Fee-for-Service database (Jan 2014-Dec 2020). Index date was a random BE claim preceded by ≥1 year of BE disease history. Patients had continuous enrollment ≥12 months pre-index (baseline) and ≥12 months post-index (follow-up). Treatment patterns during follow-up were assessed in patients stratified by baseline BEx (0, 1, or ≥2).
Results:
In 92,529 patients with BE (mean [SD] age, 76.7 [8.8] years; 72.3% female; 55.1% with asthma; 45.9% COPD), use of antibiotics and other therapies was significantly greater in patients with a higher baseline BEx (Figure). Mean (SD) duration of antibiotic therapy was 103.0 (126.3), 152.6 (127.1), and 208.4 (118.1) days, and proportion with antibiotic use ≥12 weeks was 42.0%, 59.2%, and 76.1%, in the 0, 1, and ≥2 BEx groups, respectively (p<0.001).
Conclusions:
The greater range, and duration, of treatments received by patients with BEx is indicative of more severe disease, which adds to the burden on patients and highlights the need for more effective treatments.
Epidemiology I—Abstract 20
Non-Tuberculous Mycobacteria – Trends in the State of Israel
Sivan Perl, MD1 Sharon Enghelberg, MD1 Noam Natif, MD1 Murad Shehab, MD1 Efrat Rorman, PhD2 Hasia Keidar Shwartz, PhD2 Benjamin Fox, MD1
Author Affiliations:
1. Shamir Medical Center, Beer Yaakov, Israel
2. The National Center for Mycobacteria, Israel, Tel Aviv, Israel
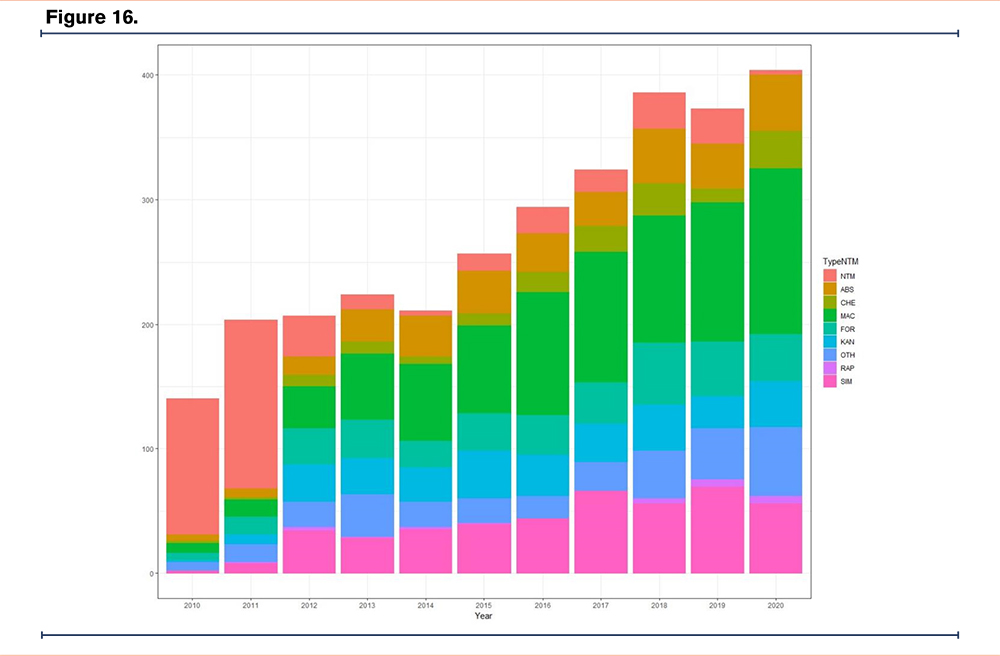
Background:
Nontuberculous Mycobacteria (NTM) are ubiquitous environmental bacteria that can induce pulmonary and non-pulmonary diseases in susceptible persons. In recent years there has been an increase in the incidence of NTM infections. We examined the national temporal and geospatial trends in NTM isolation in Israel.
Methods:
Data on NTM isolatios, between the years 2010-2020, were extracted from the National Center for Mycobacteria database. Data was cross matched with the demographic characteristics of the Israeli population taken from the 2017 Israeli Central Bureau of Statistics (ICBS). The identified mycobacteria were classified into 9 groups: M. Simiae, M. Abscessus, M. Fortuitum, M. Kansasii, M. Chelonae, Other pathogenic NTM species, Other rapidly growing mycobacteria, M. Avium, Unclassified NTM.
Results:
The study included 3024 samples from 4061 subjects. The mean age of the subjects was 60.4 (±19) years, and most subjects were male (54.9%). The majority of the subjects were living in localities with a Jewish majority (66.1%). Most isolates came from cities in the upper half of the socio-economic ranking. Over the last decade there has been an upward trend in NTM bacterial isolates (140 isolates in 2010 to 402 in 2020). The increase in incidence was driven mostly by M. avium (26.2%), and M. simiae (14.5%). M. Avium was isolated mostly in the Central region of Israel, whereas M. Simiae was isolated in the Central region but also predominant in the North regions. Most isolates were from the Central District of Israel (26.7%).
Conclusions:
There has been an increase in NTM bacterial isolation in Israel in the last decade. At the global level, underdiagnosis and underreporting make it difficult to obtain an accurate picture of the epidemiology of NTM bacteria. M. Avium and M. Simiae are the most commonly isolated strains in Israel. Regional differences in the types of isolates were seen.
Epidemiology I—Abstract 21
Establishment of Optimized Care for BE Patients from 2021 in a German Center
Sivagurunathan Sutharsan1 Matthias Welsner2 Svenja Straßburg2 Gerhard Weinreich1 Christian Taube Sarah Dietz-Terjung1
Author Affiliations:
1. University Medicine Essen, Essen, North Rhine-Westphalia, Germany
2. University Medicine Essen - Ruhrlandklinik, Essen, North Rhine-Westphalia, Germany
Background:
Bronchiectasis is a chronic inflammatory structural respiratory disease that is often underestimated in its prevalence due to its clinical similarity to other respiratory diseases. Bronchiectasis can be caused by various pulmonary and extrapulmonary diseases and is characterized by a variable number and severity of exacerbations, often with an infectious profile.
To improve the care of these patients, regardless of the underlying disease, the University Medicine Essen, Ruhrland Clinic is evaluating the care situation since 2018 and also examining subsequent care situations for these patients. Here, we present the results of 2021.
Methods:
All patients presenting with bronchiectasis or associated diseases as inpatients or outpatients at the University Medicine Essen, Ruhrland Clinic in 2021 were recorded in our database. Statistical analysis was performed using version 27 of the SPSS statistics package (SPSS Inc., Chicago, USA). Data are presented as mean ± standard deviation (SD).
Results:
The care situation for patients with bronchiectasis is being evaluated at the University Medicine Essen, Ruhrland Clinic, and the results of 2021 show that 354 patients with bronchiectasis and associated diseases were treated, resulting in 717 cases. The findings also suggest that there is a significant positive correlation between the occurrence of an exacerbation and the severity of bronchiectasis.
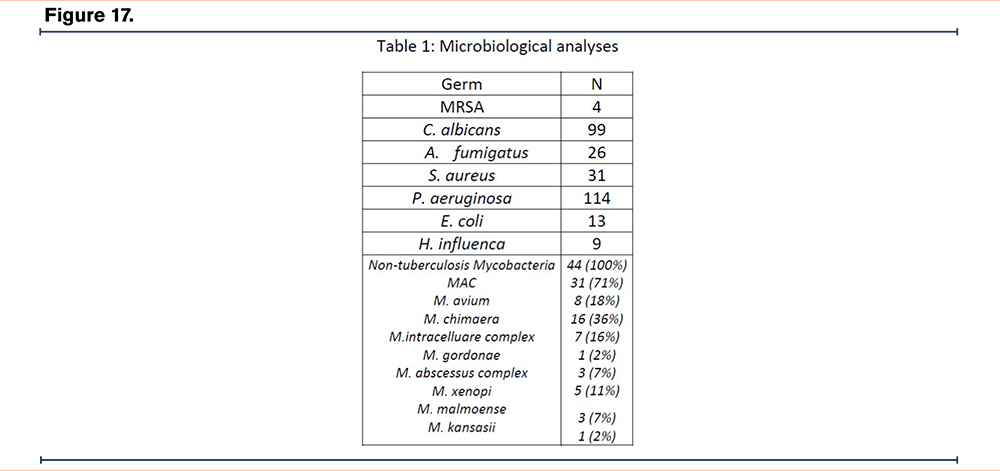
In addition, various microbial colonization were found in the microbiological analyses (Table1).
Conclusions:
The presented data represent the most comprehensive data set in the field of bronchiectasis and hold the potential to bring new insights into this complex disease. Given the potential underestimation of the prevalence of bronchiectasis, more research and attention should be given to this disease to improve the care of patients with bronchiectasis. NTM infections are an important consideration in patients with BE. Early detection and treatment can help prevent disease progression and improve clinical outcomes in these patients.
Epidemiology II—Abstract 22
Bronchiectasis and NTM Research Registry: 5-year Mortality by BSI and FACED Severity Categories
Timothy R. Aksamit, MD1 Mark L. Metersky, MD2 Nicolas Locantore, PhD3 Ruth Tal-Singer, PhD3 Bruce E. Miller, PhD3
Author Affiliations:
1. Mayo Clinic, Rochester, Minnesota, United States
2. University of Connecticut School of Medicine, Farmington, Connecticut, United States
3. COPD Foundation, Washington, District of Columbia, United States
Background:
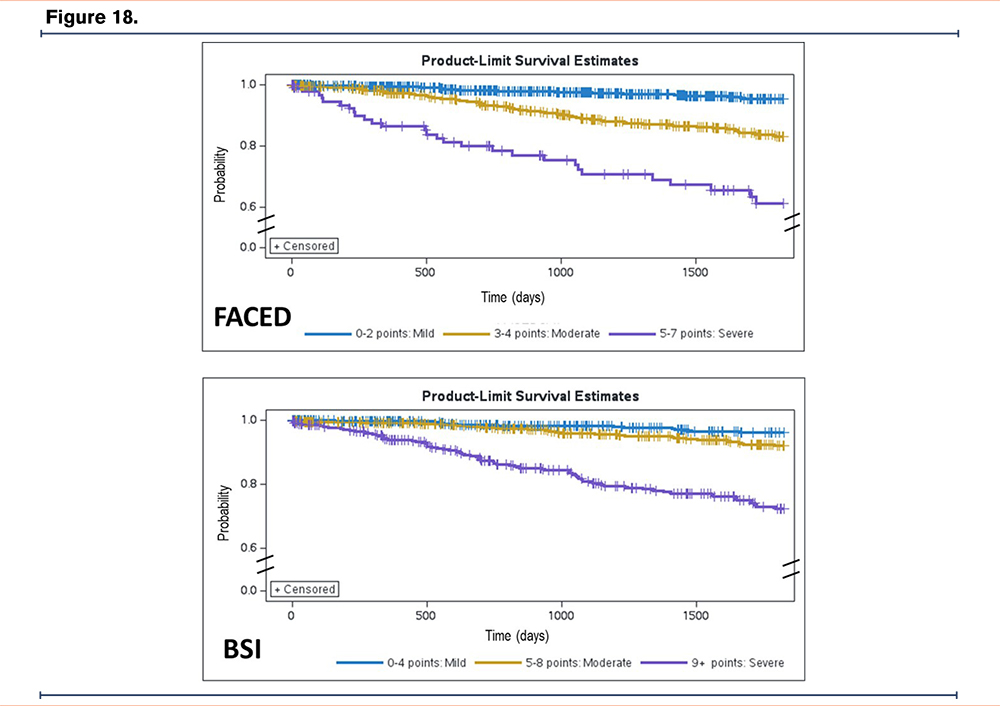
Bronchiectasis is a chronic lung disease characterized by recurrent infections, inflammation, and frequent exacerbations. Factors associated with longitudinal outcomes including mortality remain uncertain. We sought to establish the 5-year survival of people enrolled in the Bronchiectasis and NTM Research Registry (BRR) based on their Bronchiectasis Severity Index (BSI) and FACED scores.
Methods:
The BRR is a database of people with bronchiectasis and/or nontuberculous mycobacteria (NTM) lung disease recruited from US sites between 2008-2017. All components of the BSI and FACED were available for 1647 and 2061 people with bronchiectasis, respectively. Participants were categorized as Mild/Moderate/Severe for each scale according to their scoring components. Survival to 5 years after BRR entry was measured for each index/category using a log-rank test and Kaplan-Meier curves.
Results:
Baseline scoring into Mild/Moderate/Severe categories yielded n=579/642/426 for BSI and n=1264/677/120 for FACED, respectively. Probability of death over 5 years was 4%/8%/28% for BSI and 5%/17%/39% for FACED among Mild/Moderate/Severe scores. Kaplan-Meier curves are shown in Figure 1.
Conclusions:
For this US-based population with bronchiectasis, both FACED and BSI categories differentiate mortality risk. Similar to smaller cohorts, FACED seems to be a stronger predictor of mortality than BSI due to FACED isolating a smaller, more severe subset of participants at higher risk, while the BSI yielded a more even distribution of severity.
Acknowledgements
The authors would like to acknowledge the COPD Foundation, a 501(c)(3) nonprofit organization, who manages the Bronchiectasis and NTM Research Registry. The Registry is funded by the Richard H. Scarborough Bronchiectasis Research Fund, the Anna-Maria and Stephen Kellen Foundation, a Research Grant from Insmed Incorporated, and the Bronchiectasis and NTM Industry Advisory Committee. Also, this work would not be possible without comprehensive chart reviews and data recording by the dedicated research coordinators and PIs at each participating Registry site.
Epidemiology II—Abstract 23
Health Related Quality of Life in Bronchiectasis Patients Undergoing Home-Based Pulmonary Rehabilitation with Health Coaching
Caitlin Batzlaff, MD1 Roberto Benzo, MD, MSc1 Timothy R. Aksamit, MD1
Author Affiliations:
1. Mayo Clinic, Rochester, Minnesota, United States
Background:
Bronchiectasis is a chronic airway disease that impacts heath related quality of life (HRQL). Common HRQL themes identified by patients include symptom burden/variation and feeling in control of their disease. Pulmonary rehabilitation (PR) improves HRQL and exercise capacity, but the uptake is poor.
We aim to evaluate the feasibility, acceptability, and effect size of home-based PR with health coaching (HC) in patients with bronchiectasis and high symptom burden.
Methods:
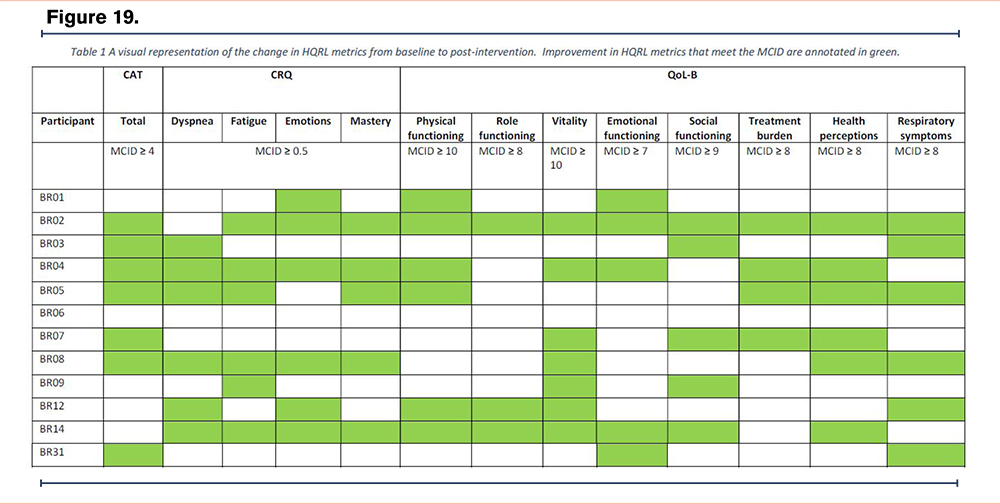
Prospective, cohort study testing 12 weeks of home PR and weekly HC.
Inclusion Criteria:
1. Clinical & radiologic diagnosis of non-cystic fibrosis bronchiectasis
2. Clinically meaningful symptomatic burden (COPD Assessment Test score ≥10)
3. Age ≥ 18 years
Outcomes:
COPD Assessment Test (CAT), Chronic Respiratory Questionnaire (CRQ), Quality of Life – Bronchiectasis (QoL-B) measured at baseline and 12 weeks.
Results:
This pilot study includes 12 participants. Mean age 67.8 y/o (SD 10.2), 58.3% female, all participants were white. Mean FEV1 was 73.5% predicted (SD 26.5%).
Program adherence is a percentage of days participated divided by total days. Adherence to the flexibility exercise, balance exercise, mindful breathing practice, and check-in questions were 55.1%, 51.7%, 60.4%, and 63.6% respectively. Compliance with health coaching calls was 99.3% (143/144 calls).
Of the 12 participants that completed the program, the intervention was well received and the ratio of patients achieving the minimal clinically important differences (MCID) in at least one domain of the outcomes was high: 7/12 (58%) for CAT, 9/12 (75%) for CRQ, and 11/12 (92%) for QoL-B. Table 1 reflects each participant, meeting the MCID for each domain of the outcome (annotated in green) or not.
Conclusions:
Home-based PR with HC is feasible, acceptable, and possibly effective for patients with bronchiectasis and high symptom burden. Technology was not a barrier to delivering PR. Health coaching had very high uptake indicating high engagement.
Epidemiology II—Abstract 24
Pseudomonas Treatment Practice Patterns and Outcomes in Non-Cystic Fibrosis Bronchiectasis: Analysis from the US Bronchiectasis and NTM Research Registry
Sarah Chalmers, MD1 Jamie Felzer1 Amanda E. Brunton, MPH2 Margaret Johnson3 Kevin Winthrop, MD, MPH4 Radmila Choate, PhD, MPH5 Shoshana Zha6 Nicole Lapinel, MD7 Diego J. Maselli Cacer, MD8 Christopher Richards, MD9 Kunal Jakharia, MD10 Timothy R. Aksamit, MD1
Author Affiliations:
1. Mayo Clinic, Rochester, Minnesota, United States
2. COPD Foundation, Miami, Florida, United States
3. Mayo Clinic-Jacksonville, Jacksonville, Florida, United States
4. Oregon Health and Science University, Portland, Oregon, United States
5. University of Kentucky, Lexington, Kentucky, United States
6. University of California-San Francisco, San Francisco, California, United States
7. Northwell Health, Hempstead, New York, United States
8. UT Health San Antonio, San Antonio, Texas, United States
9. Mass General, Boston, Massachusetts, United States
10. UNC Health, Chapel Hill, North Carolina, United States
Background:
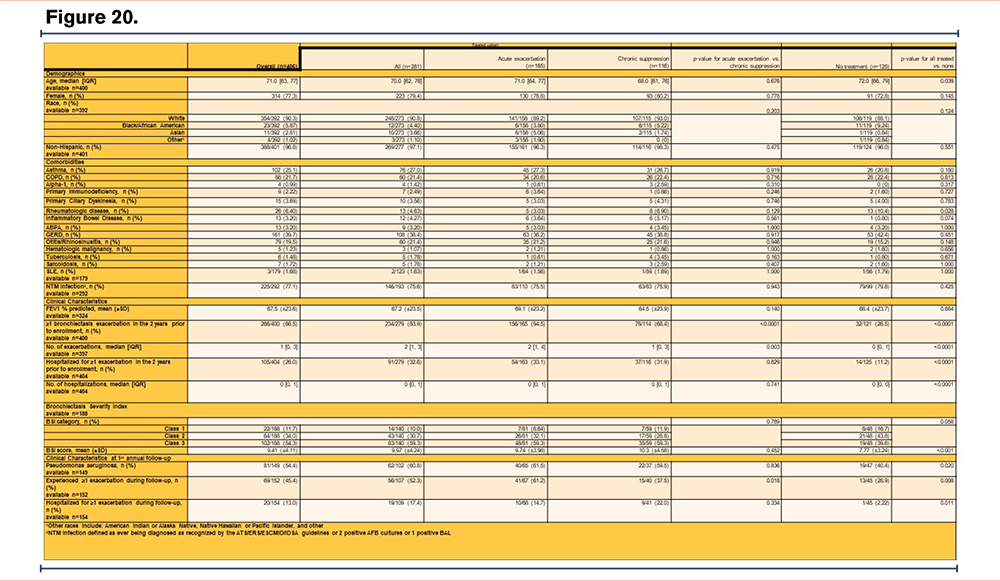
In patients with bronchiectasis, chronic Pseudomonas aeruginosa (PSA) colonization is associated with worse outcomes. Eradication of PSA after colonization is unlikely, therefore current guidelines recommend treatment upon first isolation. Prior studies have suggested that prescribing practices reflect understanding of the negative impact of chronic PSA colonization, but wide variation in treatment patterns exist.
Methods:
This was a retrospective analysis of the treatment patterns and associated outcomes in patients with bronchiectasis and PSA isolation (chronicity unknown) from the United States (US) Bronchiectasis and Non-Tuberculous Mycobacterial (NTM) Research Registry. Patients were included if they had at least one positive PSA culture and known antibiotic treatment status at baseline (defined within two-years prior to registry enrollment).
Results:
406 patients met inclusion criteria, of which 281(69%) received antibiotics. At baseline, of those treated, 165(59%) received antibiotics for acute exacerbations [151/165(91.5%) systemic only, 14(8.5%) systemic and inhaled], 74(26%) received antibiotics for acute exacerbation and chronic suppression, and 42(15%) received antibiotics for chronic suppression (systemic and/or inhaled). Older patients were significantly less likely to receive antibiotics. Those with a greater median number of exacerbations (p<0.0001), hospitalizations for exacerbations (p<0.0001), and higher mean bronchiectasis severity index (p<0.001) were more likely to receive treatment.
One year after enrollment, those who received prior antibiotic treatment were more likely to have a positive PSA culture (p=0.020), an exacerbation (p=0.008), and be hospitalized for an exacerbation (p=0.011). There was increased likelihood of hospitalization in those acutely treated verses those receiving chronic suppressive therapy. (p=0.018).
Conclusions:
Bronchiectasis patients with at least one positive PSA culture plus a history of prior exacerbations or severe exacerbations were more likely to be treated with antibiotics and have subsequent exacerbations. Our findings suggest that while prior exacerbations may lead to increased antibiotic use, impact of treatment on risk of future exacerbations requires further investigation.
Acknowledgements
The authors would like to acknowledge the COPD Foundation, a 501(c)(3) nonprofit organization, who manages the Bronchiectasis and NTM Research Registry. The Registry is funded by the Richard H. Scarborough Bronchiectasis Research Fund, the Anna-Maria and Stephen Kellen Foundation, a Research Grant from Insmed Incorporated, and the Bronchiectasis and NTM Industry Advisory Committee. Also, this work would not be possible without comprehensive chart reviews and data recording by the dedicated research coordinators and PIs at each participating Registry site.
Epidemiology II—Abstract 25
Failure of Mycobacterium Avium to Adhere to Interior Surfaces of Positive Expiratory Pressure (OPEP) and Nebulizer Devices
Judy Schloss, MBA, RRT-NPS, AE-C1 Jason Suggett, PhD, BPharm, MBA2 Dominic Coppolo, MBA, RRT, FAARC3 Joseph O. Falikinham, PhD4
Author Affiliations:
1. Monaghan Medical, Lester Prairie, Minnesota, United States
2. Trudell Medical, London, Ontario, Canada
3. Monaghan Medical, Plattsburgh, New York, United States
4. Virginia Tech Department of Microbiology, Blacksburg, Virginia, United States
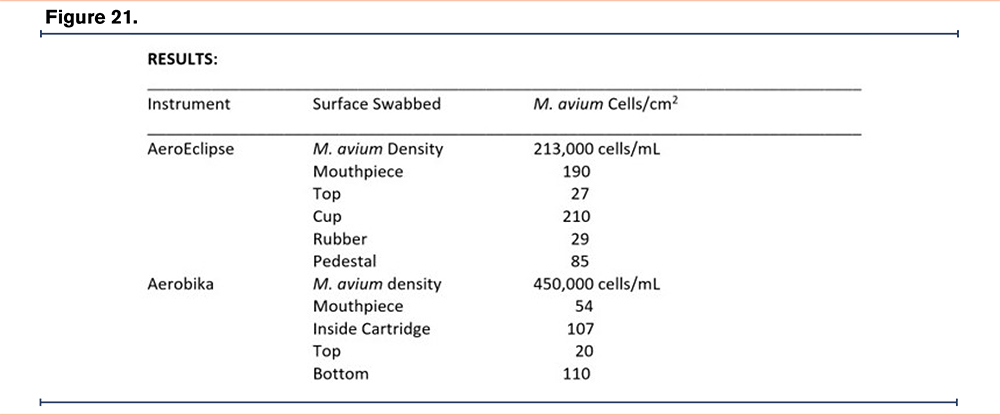
Background:
Risk of respiratory infection is a common concern for bronchiectasis patients often leading to caution involving use of medical devices for inhalation. As M. avium is a major cause of lung infection in bronchiectasis patients and is common in household drinking water that could be used to rinse respiratory devices. Accordingly, the object of this study was to measure the adherence of M. avium cells to interior walls of two commonly used respiratory devices.
Methods:
One OPEP device (Aerobika*, Monaghan Medical) and one breath actuated nebulizer (AeroEclipse* XL BAN* nebulizer, Monaghan Medical) were evaluated. Each device was disassembled and separately submerged in a one-liter high density suspension of M. avium 18 hours and then air dried. A 4-cm2 area of the mouth piece, top, cup, and pedestal were swabbed, the swab placed in 2 mL of sterile distilled water and vortexed to release and suspend M. avium cells. Cells were counted as colony-forming units on Middlebrook 7H10 agar media after 10 days incubation at 37° C.
Results: (see table)
Conclusions:
The test was designed to provide a worst-case scenario, with a very high-density suspension of M. avium cells and a long 24-hr period to allow for adherence. Compared to copper, stainless steel, galvanized steel, and PVC surfaces (average > 2,000 cells/cm2 in 24 hr.), the number of adherent M. avium cells on the surfaces of the AeroEclipse* or Aerobika* is minimal. Thus, even under a worst-case scenario the measurements indicate that materials comprising the surfaces of the Aerobika* OPEP and AeroEclipse* XL BAN* nebulizer devices fail to collect adherent M. avium cells.
Epidemiology II—Abstract 26
Patient Experiences Living with Bronchiectasis – Results from a US Focused Online Survey
Judy Schloss, MBA, RRT-NPS, AE-C1 Jason Suggett, PhD, BPharm, MBA2 Dominic Coppolo, MBA, RRT, FAARC3 Linda Esposito, MPH4
Author Affiliations:
1. Monaghan Medical, Lester Prairie, Minnesota, United States
2. Trudell Medical, London, Ontario, Canada
3. Monaghan Medical, Plattsburgh, New York, United States
4. Be Clear Today, New York, New York, United States
Introduction:
Patient engagement in therapy and self-management is generally high in those with bronchiectasis, although diagnosis is challenging, and the burden of treatment can be high. This study looked to understand themes around time to diagnosis, treatment burden and maintenance of therapeutic devices.
Methods:
An online survey was shared via social media platforms to bronchiectasis patients by a patient advocate. Questions related to a) time to diagnosis b) time spent performing pulmonary therapy and device combinations c) lung infections, and d) ways to clean/disinfect and the time spent doing that.
Results:
Of the 122 detailed responses received, some headline results are reported here. Almost 50% of patients had been diagnosed within the last 5 years with 30% of all patients having symptoms for >5 years prior to diagnosis. A little over 70% of respondents spent more than 30mins per day on nebulizer/airway clearance therapy (34% more than 1hour) with different device combinations used to save time (nebulizer/OPEP/Vest) being prevalent amongst the majority of patients. Bacterial infections (various types) were reported by majority of patients. 97% of patients cleaned or disinfected their devices, with almost 50% of patients spending more than 1 hour a week performing such cleaning / disinfecting. Boiling on stove was the most commonly used method of disinfecting, however many different methods of cleaning were reported.
Conclusions:
The results from the survey confirmed that a large proportion of patients experience significant time from onset of symptoms to formal diagnosis. Despite patients utilizing combination therapy in various forms, the burden of therapy along with cleaning / disinfecting their devices remains high. Based on these results, in addition to continuing to raise the awareness of bronchiectasis within the HCP community, there remains an onus on therapy manufacturers to develop time efficient and easy to clean/disinfect devices for these patients.
Epidemiology III—Abstract 27
Health Literacy Analysis of Online Patient-Directed Educational Materials about Mycobacterium Avium Complex
Olabimpe O. Asupoto, BS1 Shamsuddin Anwar, MD1 Alysse Wurcel, MD, MS1
Author Affiliations:
1. Tufts Medical Center, Boston, Massachusetts, United States
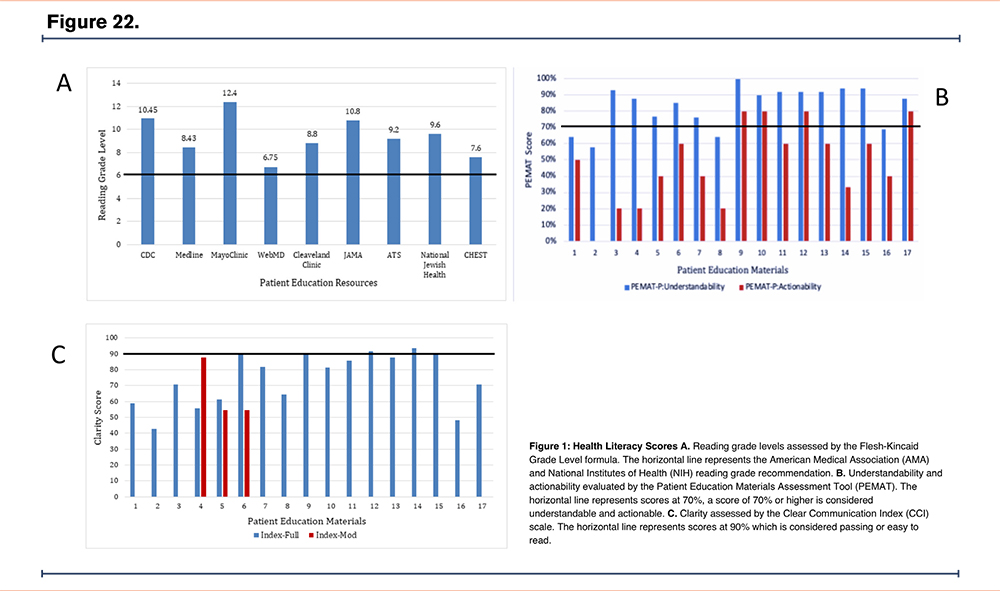
Background:
Mycobacterium avium complex (MAC) is a complex lung infection requiring multi-disciplinary approach and management. Due to limited clinician-patient interactions, clinicians may refer patients to online resources to learn about the diagnosis, prognosis, and treatment of MAC. The American Medical Association and the National Institutes of Health recommends patient education materials be written at a sixth-grade reading level; however, several evaluations found these materials are inaccessible due to high literacy levels. To date, there has never been a health literacy assessment of MAC patient education materials. The study aims to assess online patient education materials about MAC with validated health literacy tools.
Methods:
The patient education materials were evaluated for readability, actionability, understandability and clarity. Readability was measured through the Flesch-Kincaid Grade Level Scale. Actionability and understandability was evaluated using the Patient Education Materials Assessment Tool (PEMAT). The Centers for Disease Control (CDC) Clear Communication Index (CCI) was used to assess the clarity.
Results:
Ten patient education resources were evaluated: CDC, Cleveland Clinic, Mayo Clinic, JAMA, American Thoracic Society (ATS), National Jewish Health, UpToDate, CHEST, WebMD, and Medline. WebMD was the only resource that contained materials written at a sixth-grade reading level. Most of the materials received a passing score for understandability but failed to achieve it for actionability. Cleveland Clinic, JAMA, and ATS all received a passing clarity score, indicating they are easy to read. No patient education materials were available on UpToDate, a well-known resource utilized by physicians.
Conclusions:
Most patient education materials scored poorly for actionability and clarity while scoring highly for readability and understandability. This study should serve as a guide for clinicians interested in offering online education materials to their patients. Increasing access to readable MAC educational materials should be a priority for those working at the intersection of public health, clinical care, and communications.
Epidemiology III—Abstract 28
Evaluation of Candidate Computable Phenotypes for the Identification of Bronchiectasis in the Electronic Medical Record Using Patient Centered Outcome Research Network (PCORnet) Data Architecture
Rebecca Bascom, MD, MPH1 Jordan Pearson, BS1 Anne E.F. Dimmock, MS1 Wenke Hwang, PhD1 Emily M. Henkle, PhD, MPH2
Author Affiliations:
1. Penn State College of Medicine, Hershey, Pennsylvania, United States
2. Oregon Health and Science University, Portland, Oregon, United States
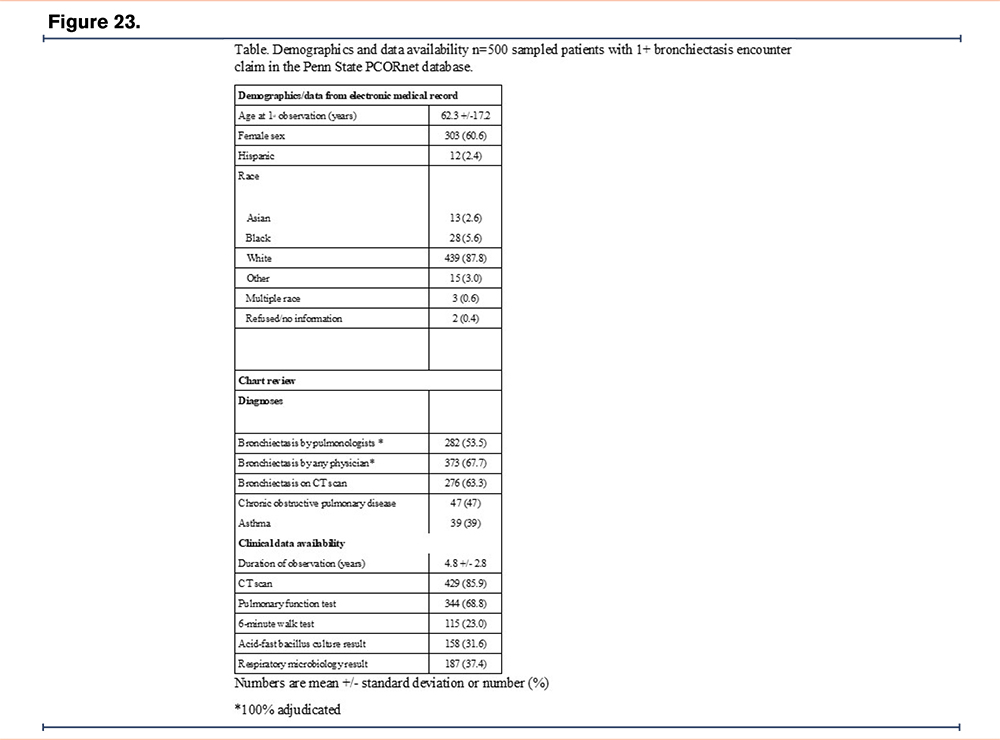
Background:
The electronic medical record (EMR) offers a rich data source for bronchiectasis studies. The PCORnet Common Data Model is a consistent data architecture utilized by 8 networks and 64 participating United States institutions. This study’s objective is to validate and compare four bronchiectasis computable phenotypes against a gold standard of pulmonologist-diagnosed bronchiectasis.
Methods:
The data source is a single institution, tertiary care center: Penn State PCORnet dataset from 01/01/2011 to 06/09/2019. We identified an adult EMR cohort with an inpatient or ambulatory/emergency department [ED] encounter with a bronchiectasis ICD-10 diagnosis code (J47.0, J47.1, J47.9), excluding cystic fibrosis diagnosis. We tested the following computable phenotypes: A) 1+ ambulatory/ED encounters or 1+ hospitalization with a principal or secondary diagnosis of bronchiectasis; B) 2+ ambulatory/ED encounters 30+ days apart or 1+ hospitalization with a principal or secondary diagnosis of bronchiectasis; C) definition B or 1 ambulatory/ED encounter with a computed tomography (CT) scan of the thorax (CPT-4 71250, 71260, 71270) within 60 days; D) either B or C. We constructed a validation sample of 4 overlapping samples, oversampling for racial/ethnic minorities and mycobacterial disease. Duplicate independent REDCap-based retrospective chart reviews validated the computable phenotype samples against a gold standard of a 100% adjudicated pulmonologist-diagnosed bronchiectasis. We first described the validation sample, then calculated the positive predictive value (PPV, 95%CI) for each of the four candidate computable phenotypes.
Results:
From an EMR cohort of 1514 persons we selected a validation sample of 500 (see Table). The PPVs were as follows: Computable Phenotype A 0.51 (0.43-0.59), Computable Phenotype B 0.62 (0.52-0.72), Computable Phenotype C 0.48 (0.37-0.58), and Computable Phenotype D 0.6 (0.52-0.68).
Conclusions:
This validation study provides search strategies to identify patients with bronchiectasis and will facilitate future multi-institutional studies of bronchiectasis using the PCORnet data architecture to improve bronchiectasis diagnosis, treatment, and outcomes.
Epidemiology III—Abstract 29
Bronchiectasis and COPD: Is it Special Disease Phenotype?
Kateryna Gashynova1 Ksenia Suska1 Valeriia Dmytrychenko1
Author Affiliations:
1. DDMU, Dnipro, Ukraine
Background:
Bronchiectasis (Bx) is a chronic airways disease with high rate of comorbidity and heterogeneity.
The aim: to detect if there are features in patients (pts) with Bx and COPD.
Methods:
The prospective observational single-center study enrolled stable pts with Bx in Dnipro, Ukraine. COPD was diagnosed based on GOLD recommendations. Bx exacerbations frequency during the previous year was calculated by self-reports and medical documentation. Smoking status, comorbidity by BACI scale, BMI, were evaluated.
Results:
99 pts (33 (33,3%) men, age 55 (39-63) years, were included. 19 pts had COPD (19.2%). Pts were divided in groups: G1 - with COPD, G2 - without COPD. There were no significant differences between the groups in age. In G1 there were more men (p=0,0001). The number of exacerbations in G1 was 4 (2;5) per year, G2 - 2(1;4), p=0.19. The number of frequent exacerbators in G1 was 11(57.9%), G2 -37(46.3%), p=0.37. The number of smokers in G1 - 16(80%), G2 - 20(25%), p=0,000002. The pack/years in G1 - 27,5 (17,5;40), G2 - 8,3 (1,5-25), p=0.003. The comorbidities in G1 - 4 (3;5), G2 - 2(1;3), p=0.00002. The number of high risk pts (by BACI) in G1 - 14(73.7%), G2 - 7(8.8%), p=0.000001. BMI ≥ 25,0, in G1 - in 13 (68.4%), G2 - in 34(42.5 %) pts, p=0.04. mMMRC score was 2 (1;3) in G1; 1 (1;2) in G2.
Conclusions:
19.2% pts with Bx have COPD in Dnipro (Ukraine). In this groupe prevalent men, active smokers with higher pack/years. They have no more frequent exacerbations and a higher proportion of frequent exacerbators, but h more comorbidities and a higher risk by BACI. Pts wis Bx and COPD have more severe dyspnea by mMRC. We recommend to focusing on COPD detection in pts with Bx as on a potential treatable trait.
Epidemiology III—Abstract 30
Profile of Nontuberculous Mycobacteria Infections in the Finger Lakes Region of New York, 2018-2020
Sonal S. Munsiff, MD1 Michael Croix, MD1 Ghinwa Dumyati, MD1 Alexandra Adams, MD1 Dwight Hardy, PhD1 Paul Levy, MD1 Emil Lesho, DO2
Author Affiliations:
1. University of Rochester, Rochester, New York, United States
2. Rochester Regional Health System, Rochester, New York, United States
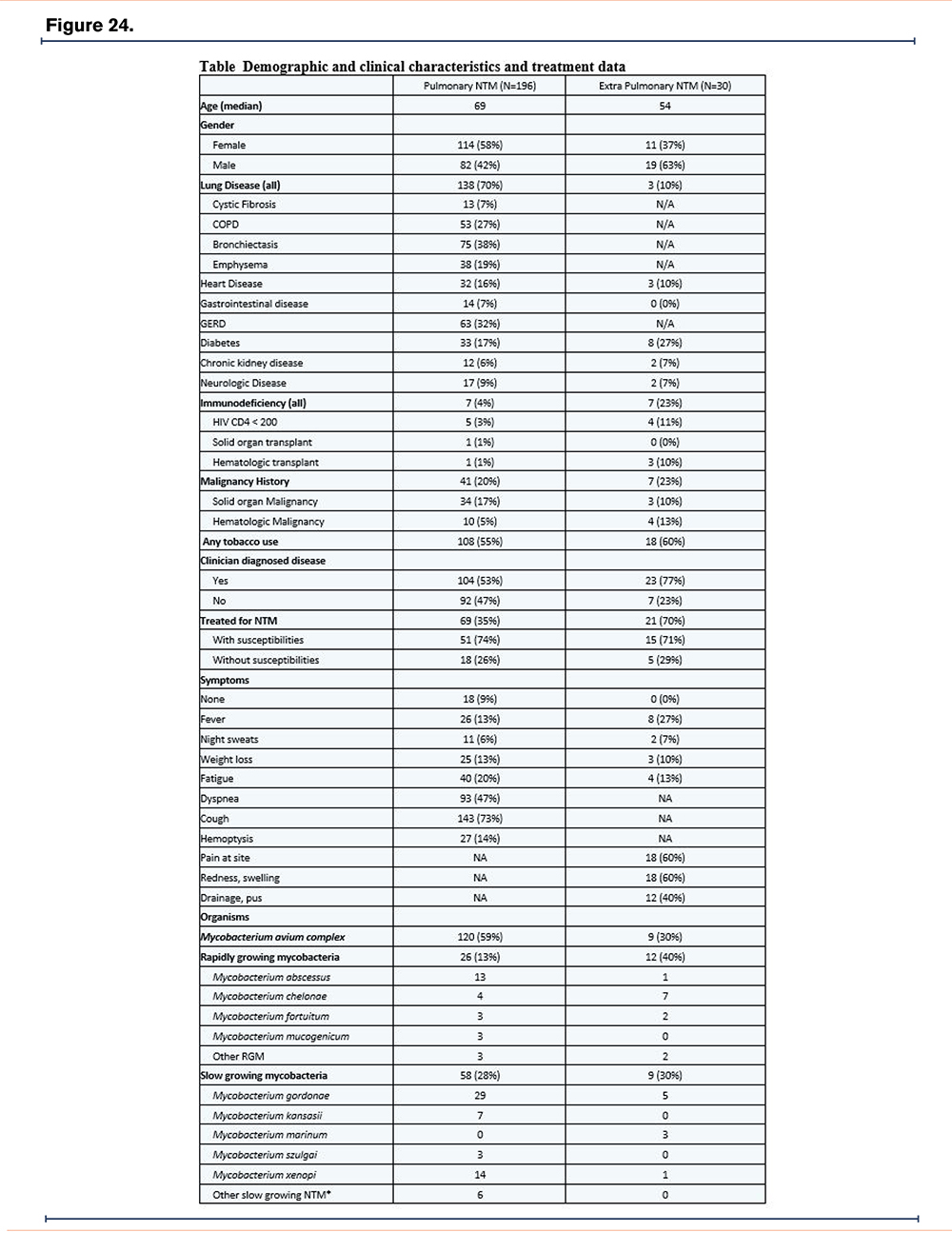
Background:
The prevalence of Nontuberculous Mycobacteria (NTM) disease is increasing. Evaluation and treatment is labor intensive, but not all patients need treatment. Our clinic is seeing increasing referrals for NTM disease. We reviewed the clinical characteristics of NTM patients in our region to assess the burden of disease, and plan for developing a referral center.
Methods:
We retrospectively identified patients with at least one culture growing NTM in the University of Rochester Medical Center and Rochester Regional Health laboratories from April 1, 2018 thru March 31, 2020. These healthcare systems serve as the mycobacterial laboratories for the Finger Lakes region. We reviewed records to obtain demographic, comorbidity, culture, and treatment information and compared data between patients with pulmonary and extra-pulmonary isolates.
Results:
235 NTM isolates from 226 persons were identified; 205 from pulmonary and 30 from extra-pulmonary sites. Mycobacterium avium complex was the most commonly isolated NTM from all sites (Table). The rate of positive culture was 16.4/100,000 for pulmonary sites and 2.5/100,000 population for extra-pulmonary sites.
Persons with pulmonary NTM (pNTM) were more likely to be older, female, and have underlying lung disease (p<0.01). Persons with extra-pulmonary NTM (eNTM) isolates were more likely to have clinician diagnosed disease (8.7/100,000 vs 1.92/100,000 population, p=0.036). Only 66% with clinician diagnosed pNTM disease were treated (35% of total pNTM) compared with 91% with clinician diagnosed eNTM disease (70% of total eNTM) (Table). Disease site specific symptoms were more common than constitutional symptoms (Table).
Conclusions:
Many pulmonary isolates were not considered reflective of clinical disease and only 35% were treated highlighting the difficulty of determining NTM disease vs. colonization. Most of the patients in our cohort had extensive evaluation, and many more are being monitored for disease progression. Resources need to be allocated to provide treatment and monitoring for all patients with NTM.
Epidemiology III—Abstract 31
Interpreting Susceptibility Results for Clinical Use of Novel Drugs for Rapidly Growing Mycobacteria
Sonal S. Munsiff, MD1 Michael Croix, MD1 Dwight Hardy, PhD1
Author Affiliations:
1. University of Rochester, Rochester, New York, United States
Background:
Susceptibility breakpoints are not available for several antibiotics that may be useful for treatment of nontuberculous mycobacteria (NTM) infections. We present minimum inhibitory concentrations (MIC) of rapidly growing mycobacteria (RGM) from our institution and suggest interpretation for use of bedaquiline, clofazimine, delafloxacin, omadacycline, and tedizolid based on literature review.
Methods:
RGM were identified by partial sequencing of the 16S rRNA gene and hsp65 gene, and Mass Spectrometry of protein profiles. MICs (μg/ml) were determined in CA-MHB by microdilution methodology as recommended by CLSI M24, 3rd ed.; breakpoints where available were as recommended by CLSI M62.
Results:
From January 2020-July 2022, we identified 30 RGM isolates from 28 patients. Eighteen isolates were M. abscessus, seven M. fortuitum, four M. chelonae, and one M. smegmatis. MIC50 (range) for 17 M. abscessus isolates was 0.12 (0.06-0.5) for bedaquiline, 0.5 (0.25-1) for clofazimine, 128 (2-128) for delafloxacin, 1 (0.12-4) for omadacycline, and 2 (0.12-128) for tedizolid.
Literature review and drug pharmacokinetics suggest the following MICs(ug/mL) for RGM treatment: bedaquiline ≤0.25, clofazimine ≤0.5, Omadacycline ≤2, tedizolid ≤2. Fluoroquinolone MICs were too high for most M. abscessus isolates, though may be options for other RGMs.
Conclusions:
Treatment of RGM is challenging in the setting of resistance to commonly used antibiotics. Newer and repurposed antibiotics show in vitro activity against RGM, but lack established MIC breakpoints. We present MIC data from RGM isolates at our institution. Current pharmacologic, microbiologic, and clinical data for use of these agents is limited and often uses single agents for short periods of time making extrapolation to treatment with multiple agents for many months challenging. We propose MICs for clinical use until additional in vitro studies, including time-kill analyses with Monte Carlo simulations, and clinical studies correlating outcomes with MIC are available.
M. Abscessus–Treatment—Abstract 32
Pharmacokinetics and Tolerability of Clofazimine Applied as Oral Inhalation Suspension (MNKD-101) in Healthy Adults
Thomas Hofmann1 Stefan Ufer2 Marshall Grant1 Jason Lickliter3 Christopher Rose1 Kirsten Kaiser4 Sebastian Canisius5
Author Affiliations:
1. MannKind Corporation, Westlake Village, California, United States
2. Swabian Tech LLC, Raleigh, North Carolina, United States
3. Nucleus Network, Melbourne, Victoria, Australia
4. Ratatoa Consulting GmbH, Oberwil, Basel-Country, Switzerland
5. ACliRA Consulting ApS, Tønder, Jutland, Denmark
Background:
MNKD-101 is an orally inhaled formulation of Clofazimine (CFZ) as treatment for pulmonary nontuberculous mycobacteria (NTM) infections to avoid adverse drug reactions associated with oral CFZ and achieve higher drug concentrations in the lung compared to systemic administration.
Methods:
In a Phase 1, first-in-human, randomized, double-blind, placebo-controlled study of MNKD-101 in healthy adult participants single and daily repeated doses for 7 days of MNKD-101 up to 90mg CFZ were inhaled with a PARI e-Flow® nebulizer system to investigate tolerability and pharmacokinetics (PK). Prior to each dose increase, interim safety and PK assessments were conducted, considering both pulmonary and systemic effects, and to ensure systemic drug levels being below preclinical NOAEL.
Results:
Inhaled MNKD-101 was well tolerated with no SAEs occurring and most AEs being mild. No abnormal, clinically significant ECG results were reported. Abnormal, not clinically significant ECG results were only QRS interval and PR interval. There was no evidence of skin discoloration.
The investigated doses in single and repeated administration showed proportional increases in MNKD-101 plasma levels with increasing dose. Peak plasma concentrations of CFZ with single administration were reached within 4-8 hrs, whereas with repeated administration this was reached within 2-12 hrs. Dose increases within single administration of CFZ were associated with a 2.3-fold increase in AUC0-24 with a dose increase of 2-fold, and a 1.6-fold increase in AUC0-24 with a dose increase of 1.5-fold. As expected, CFZ showed a long plasma half-life of 290 hrs after repeated administration. Accumulation following repeated MNKD-101 dosing was considered meaningful. Ctrough levels did not appear to plateau between Day 1 and Day 6 reflecting the longer t½.
Conclusions:
Safety and PK data support further development as a treatment for NTM infections, and a Phase 2/3 efficacy study will utilize the long half-life to alleviate patient burden with favorable dosing regimen.
M. Abscessus–Treatment—Abstract 33
Antibacterial Activity of Pravibismane Against Mycobacteroides Abscessus
Jeff W. Millard, PhD1 Amy Leestemaker-Palmer, BS2 Luiz Bermudez, MD3 Brett Baker, MSc, DC1
Author Affiliations:
1. Microbion Corporation, Bozeman, Montana, United States
2. Oregon State University, Corvallis, Oregon, United States
3. University of Oregon, Corvallis, Oregon, United States
Background:
The unmet medical need related to Mycobacteroides abscessus lung infection is driven by multidrug resistance and lengthy treatment regimes. Pravibismane is the first in a new class of therapeutics that demonstrates broad-spectrum anti-infective and anti-biofilm activity. We evaluated the ability of pravibismane to inhibit M. abscessus infection both in vitro and in a chronic mouse model.
Methods:
To determine the minimum inhibitory concentration (MIC), M. abscessus 19977 and two CF patient isolate strains were suspended in Middlebrook 7H9 broth to desired concentrations, spun down, washed, and final inoculum was established in Hanks Balanced Salt Solution. THP-1 macrophages utilized for in vitro infection assays were infected with M. abscessus (multiplicity of infection of 5) or uninfected. Cells were treated with amikacin to remove extracellular bacteria, followed by pravibismane or amikacin treatment for 72h. Supernatants were plated for colony forming unit enumeration.
Pravibismane’s activity against M. abscessus was further tested in a SCID/Beige mouse model. Mice were infected with 108 M. abscessus 19977, and chronic lung infection was allowed to develop for 3 weeks. Mice were spilt into: baseline, vehicle, amikacin (100 mg/kg/day), pravibismane suspension “low” (200 µg/kg/day), and pravibismane suspension “high” (1000 µg/kg/day). Inhalation dosing was conducted using a PARI LC STAR® nebulizer. Animals were euthanized after 28 days and blood, lungs, and spleen were collected for determination of pravibismane’s activity against M. abscessus.
Results:
Pravibismane exhibited 16-32x lower MICs compared to amikacin in three M. abscessus strains tested. Similarly, pravibismane exhibited lower bacterial counts compared to vehicle treated THP-1 cells. In the chronic M. abscessus mouse model, 1000 µg/kg/day pravibismane exhibited a statistically significant (p = 0.016) reduction in bacteria in lung homogenates compared to vehicle control.
Conclusions:
These results support evaluation of inhaled pravibismane as a potential safe and efficacious therapeutic agent to treat M. abscessus pulmonary infections.
M. Abscessus–Treatment—Abstract 34
A Longitudinal Retrospective Review of Mycobacterium Abscessus Complex Antibiograms Over a Decade Reveals No Increasing Antibiotic Resistance Trends
Dorothy Hui Lin Ng, MBBS, PhD, MRCP(UK)1 Shireen Yan Ling Tan, MBBChir, PhD1 May Yee Choy, BSc (Hons)1 Charlene Cheong, BSc1 Jamie Bee Xian Tan, MBBS, FRCPath1
Author Affiliations:
1. Singapore General Hospital, Singapore
Background:
Mycobacterium abscessus complex (MABC) is the commonest rapid-growing mycobacteria identified in Singapore. It is resistant to many antibiotics and is associated with significant morbidity and healthcare costs. Local treatment regimens usually include an induction phase with a macrolide (e.g. clarithromycin) and an aminoglycoside (e.g. amikacin) along with a β-lactam (imipenem, cefoxitin), followed by a continuation phase of a combination of oral antibiotics with or without nebulized amikacin. There is a growing public health concern that MABC may be developing increasing levels of resistance to these agents. However, there has not been any data published to date. This retrospective study aims to describe the longitudinal antibiogram of MABC in our center over the past decade to elucidate any emerging resistance trends.
Methods:
All MABC isolates identified by the Singapore General Hospital Central TB Laboratory between 1st January 2012 to 31st December 2022, where antibiotic susceptibility data were available, were included. Isolates were cultivated from pulmonary and extrapulmonary sources. Only unique and nonduplicate isolates from the first culture of each patient were analyzed. Statistical analyses were performed using GraphPad Prism software. Data were anonymized and IRB exemption was granted.
Results:
707 MABC isolates were identified. After the removal of duplicates, 477 isolates were included in the analysis. Of these, 289 (60.59%) were pulmonary specimens and 188 (39.41%) were extrapulmonary specimens. Between 2012 to 2022, average yearly resistance rates to amikacin, cefoxitin, imipenem, clarithromycin, and linezolid were 0.15%, 5.34%, 19.25%, 23.41%, and 25.57%, respectively. There were no increasing resistance rates to these antibiotics. The average resistance rates to co-trimoxazole, ciprofloxacin, moxifloxacin, and doxycycline were >95% throughout.
Conclusions:
Our study confirms the high multi-drug resistance rates of MABC; however, there has been no significant increase in resistance to routinely tested antibiotics over the past decade. Further studies could include additional antibiotic susceptibility data.
Novel Diagnostics—Abstract 35
Neutrophil Elastase Regulates CFTR Function in Chronic Neutrophilic Lung Disease
Courtney M. Fernandez Petty, PhD1 Reny Joseph, MS1 Xin Xu1 Karen Bernard1 Mohamed A. Hanafy, MD1 Amit Gaggar, MD, PhD1 George M. Solomon, MD1
Author Affiliations:
1. University of Alabama at Birmingham, Birmingham, Alabama, United States
Background:
Many chronic airway disorders, including chronic obstructive pulmonary disease (COPD), bronchiectasis, and cystic fibrosis (CF), are characterized by chronic neutrophilic inflammation and altered mucociliary transport. Neutrophil elastase (NE) is a serine protease found in abundant quantities in these chronic pulmonary diseases. However, the mechanism underlying how NE contributes to airway remodeling is poorly understood. Here, we investigated the role of NE in CFTR function in airway epithelia through protease activated receptor-2 (PAR-2) activation and stimulated intracellular cAMP depletion.
Methods:
Utilizing CF bronchial epithelial cells stably expressing complementary wild-type (WT) human CFTR, we were able to evaluate ENaC activity and CFTR function (Fsk-dependent Isc) in Ussing Chambers after exposure to NE. We also assessed the role of PAR-2. Using Micro-optical coherence topography (µOCT), a real time imaging modality that visualizes the microanatomy and functional aspects of the airway in response to NE-mediated inhibition of CFTR function and potential rescue with CFTR modulation.
Results:
NE-treated WT monolayers demonstrated a 32% reduction in mean forskolin-stimulated Isc compared to vehicle (P<0.01). NE inhibition was reversed by co-addition of a synthetic NE specific inhibitor (83% of vehicle). PAR-2 activating peptide recapitulated the NE inhibition of CFTR current and decreased cAMP levels. Using µOCT, we observed a 16% decrease in airway surface liquid (ASL) in NE-treated cultures (P<0.05), which was not rescued by CFTR potentiation.
Conclusions:
NE via PAR-2 mediates an important signaling pathway resulting in an acquired loss of CFTR function, highlighting new therapeutic targets for chronic pulmonary disorders and strongly suggesting a role for CFTR dysfunction in the inherent remodeling of chronic pulmonary disorders aside from CF. Furthermore, our findings suggest that PAR-2 may serve as a potential therapeutic target to abrogate downstream effects induced by chronic airway inflammation.
Novel Diagnostics—Abstract 36
Validation of the Use of Cromolyn Sodium as a Marker of Aspiration in Bronchiectasis and Other Respiratory Diseases
Timothy P. Riddles, BSc, MBBS, MPHTM1 Rachel Thomson, MBBS, PhD1 Katherine Semple, MBBS, MPhil1 Igor Gonda, PhD2 Charles V. Herst, PhD3 Homer A. Boushey, MD4
Author Affiliations:
1. Gallipoli Medical Research Foundation, Greenslopes Private Hospital, Brisbane, Queensland, Australia
2. Respidex LLC, Dennis, Massachusetts, United States
3. Oakland, California, United States
4. University of California, San Francisco, California, United States
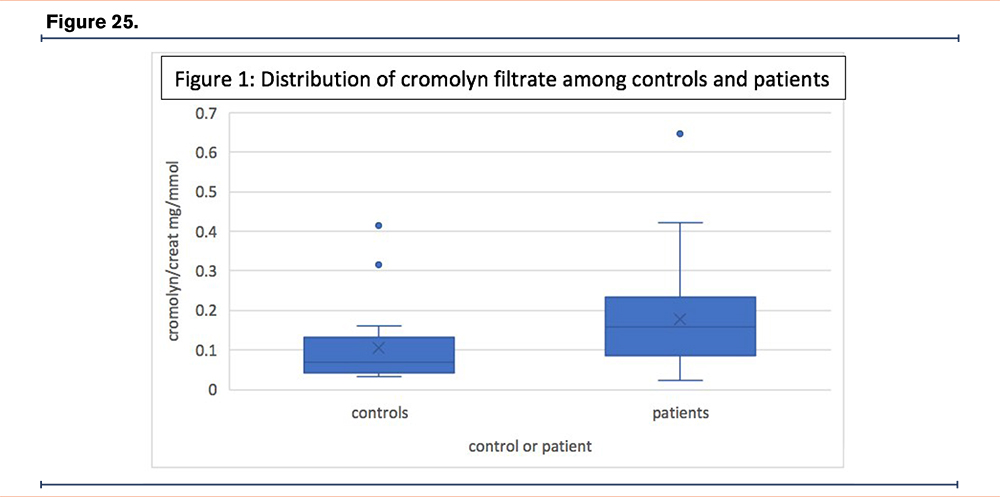
Background:
Gastro-oesophageal reflux and micro-aspiration may contribute to the pathogenesis of many respiratory conditions. Methods to confirm micro-aspiration are lacking due to insensitivity, expense, or invasiveness. When ingested, 0.5% cromolyn sodium is systemically absorbed. However, when instilled into the lungs, 30-50% is absorbed, of which >50% is renally excreted unmetabolized. The aim of this study was to detect cromolyn sodium in the urine of patients with respiratory conditions, to confirm aspiration following oral ingestion.
Methods:
Healthy controls, and patients with respiratory conditions requiring bronchoscopy were included. All participants ingested 200mg of cromolyn sodium after their evening meal, and collected voided urine overnight. Patients additionally consumed 50ml blue food colouring with the cromolyn sodium, and presented for morning bronchoscopy the following day. A subset of patients with suspected or previous nontuberculous mycobacterial (NTM) infection, had bronchoalveolar lavage (BAL) fluid stored for additional analysis.
Results:
Forty-six patients and 21 controls were enrolled. Blue-staining was visualised endobronchially in 80% (35/44) patients. Ninety percent of NTM patients (27/30; p=0.069) and 75% of bronchiectasis patients (15/20; p=0.538) had blue-stain visualised. A significant difference in urinary cromolyn/creatinine (mg/mmol) was detected between patients and controls (p=0.004); particularly in those with a history of GORD (p=0.021), Hull score >13 (p=0.01) and acid suppression use (p=0.029). No significant association between urinary cromolyn/creatinine was observed with NTM (p=0.094), or bronchiectasis (p=0.536) participants. Within the patient cohort, there was no significant association between urinary cromolyn and other markers of aspiration.
Conclusions:
Prevalence of aspiration was high among our patient cohort, determined by an elevated urinary cromolyn, which identified patients with aspiration not previously confirmed with traditional diagnostics. Future validation studies on larger cohorts will evaluate different cromolyn dosages and a urinary concentration that determines a positive result.
Novel Diagnostics—Abstract 37
Alpha-1 Antitrypsin (AAT) in Sputum: Is it a Useful Biomarker in Bronchiectasis (BE)?
Letizia Traversi, MD1 Ianire Gallego Amaro1 Javier Perez-Miranda, MD2 Almudena Felipe, MD1 Antonio Álvarez, MD, PhD1 David Clofent, MD1 Mario Culebras, MD, PhD1 ML De Souza Galvão, MD1 Karina Loor, MD1 Eva Polverino, MD, PhD1
Author Affiliations:
1. Department of Respiratory Medicine, Vall d'Hebron University Hospital, Barcelona, Spain
2. Department of Anesthesiology, Reanimation, Perioperative and Pain Medicine, Hospital Mutua Terrassa, Barcelona, Spain
Background:
Protease-antiprotease impaired balance is crucial in the pathophysiology of BE, contributing to airways (AW) inflammation. AAT represents one of the main protease inhibitors, contrasting the effect of proteases such as Neutrophil Elastase, but little is known about its concentration in AW or its role in BE as a biomarker.
We hypothesize that AAT levels in sputum (AATs) could correlate with BE severity, and represent a marker of airways disease activity.
Methods:
We collected spontaneous sputum and blood from stable BE patients, along with most relevant clinical data. AAT levels were measured in sputum supernatant by ELISA, and in blood with nephelometry.
AATs was also measured in 9 healthy non-smokers controls.
Results:
We recruited 34 patients, mostly women(74%), mean age 63±11.9 years old, mean FEV1 86±20.5%.
Significantly lower values of AATs were observed in BE compared with healthy controls (0.086mg/dl versus 0.126mg/dl, p=0.005).
Level of AATs had inverse correlation with radiological extension (number of involved lobes, r=-0.45, p=0.016; Reiff score, r=-0.58; p=0.001). No correlation was found with severity (BSI and FACED), FEV1, dyspnoea, age or BMI.
We calculated the ratio between AATs and AAT in blood (SBAAT) in 24 patients: correlation with Reiff index was confirmed (p=0.016). Lower SBAAT was associated with chronic Pseudomonas infection (p= 0.039) and sputum purulence (p=0.040).
Conclusions:
Our results suggest a possible correlation between AATs and disease extension. SBAAT and its correlation with sputum characteristics (purulence and chronic infection) seems to indicate higher consumption of AAT in airways that could correspond to an increased disease activity and protease imbalance.
Novel Diagnostics—Abstract 38
Pseudomonas Aeruginosa Eradication (PAE) in Bronchiectasis (BE) with Oral Ciprofloxacin Regimen - Retrospective Study
Letizia Traversi, MD1 Maria Teresa Martín-Gómez2 Daniel Romero2 Almudena Felipe, MD1 Clara Pons1 Antonio Álvarez, MD, PhD1 Ianire Gallego Amaro1 Eva Polverino, MD, PhD1
Author Affiliations:
1. Department of Respiratory Medicine, Vall d'Hebron University Hospital, Barcelona, Spain
2. Department of Microbiology, Vall D'Hebron University Hospital, Universitat Autònoma de Barcelona, Barcelona, Spain
Background:
Eradication of PA is currently recommended in BE guidelines although none of the proposed PAE schemes has demonstrated clear superiority.
Our study aims at evaluating the efficacy of PAE therapy with oral ciprofloxacin (OC) in a cohort of adult BE patients.
Methods:
We retrospectively evaluated BE patients attending respiratory outpatient clinic of University Hospital Vall d’Hebron, Barcelona (ES), between 2009 and 2022. We selected patients with a first infection by PA diagnosed between January 2009 and February 2019, and at least 3 years of follow up after first positive culture. We assessed the eradication rate (described as ≥3 negative sputum cultures in the year after treatment), reinfection rate (new positive sputum culture after eradication) and correlation with demographic and clinical data.
Results:
We identified 85 patients, mean age 65 years old, 63% females (54/85).
Eradication was achieved overall in 51 patients (60%), being obtained in 30 of the 41 cases (71%) treated with 21days OC and in 21 other patients with other regiments (IV+ inhaled antibiotics or other combinations)
In 28/51 (55%) of all patients achieving PAE, reinfection was observed with variable latency, from 13 to 109 months (average, 38 months).
Neither erradication rates nor reinfection did correlate with previous exposure to quinolones in the previous year or chronic treatment with azithromycin.
Conclusions:
The eradication regimen based on OC is successful in most BE patients. However, concern is raised by the elevated rate of PA reinfection even after years from the first episode. Further research is needed to identify risk factors for unsuccessful eradication. In addition, genotype studies of PA strains over time could distinguish between new infections and relapses caused from the same strain over time.
Nontuberculous Mycobacterial I and II—Abstract 39
The Clinical Implications of Trehalose Dimycolate in Patients with Mycobacterium Avium Complex Pulmonary Disease
Nakwon Kwak1 Jihoo Lee, MD1 Jake Whang, PhD2 Joong-Yub Kim, MD1 Jae-Joon Yim1
Author Affiliations:
1. Seoul National University Hospital, Seoul, South Korea
2. Korea Institute of Tuberculosis, Osong, Chung-Nam, South Korea
Background:
Trehalose 6,6’-dimycolate (TDM) is the glycolipid molecule found in the cell wall of mycobacteria. However, the clinical implications of TDM of Mycobacterium avium complex (MAC) are not known. In this study, we investigated the presence of TDM in clinical isolates from patients with MAC-pulmonary disease (PD) and analyzed the impact of TDM on disease severity, clinical course and treatment outcomes in patients with MAC-PD.
Methods:
Patients, who were diagnosed as MAC-PD between 1 January 2019 and 31 December 2021 at Seoul National University Hospital, were included in the study. After incubation for 4 weeks, the morphology of colony was classified into smooth opaque, smooth transparent, rough and glued form. The lipids of clinical isolates collected at the time of diagnosis were extracted and used for mass spectrometry. Mass peaks between 500 m/z and 3500 m/z were obtained and the peaks patterns of total lipids were analyzed.
Results:
During the study period, a total of 343 patients and their clinical isolates were included in the analysis. TDMs were identified in clinical isolates from 176 patients. Cavities were more common in patients without TDM (19.8%) than patients with TDM (10.2%) (P=0.015). The rough morphotypes were more prevalent in patients without TDM (10.2%) than patients with TDM (2.3%) (P=014). The time to antibiotic treatment was shorter in patients without TDM (4 months, interquartile range [IQR] 2-10) than patients with TDM (7 months, IQR 3-16). The proportion of culture conversion was significantly lower in patients without TDM (42.0%) than patients with TDM (69.8%) (P=0.012).
Conclusions:
The absence of TDMs predicted the advanced disease in terms of cavity formation and earlier adoption of anti-mycobacterial treatment. Moreover, patients without TDMs failed in achieving culture conversion more frequently
Nontuberculous Mycobacterial I and II —Abstract 40
Relevant Parameters in Clinical Decision Making for (Antibiotic) Treatment in NTM Patients
Susan Lassche, MSc1 Wouter Hoefsloot1 Jakko van Ingen, MD, PhD1
Author Affiliations:
1. Radboud University Medical Center, Nijmegen, Gelderland, Netherlands
Background:
Antibiotic treatment for NTM-PD is long, poorly effective and toxic, which complicates the decision on treatment initiation. We investigate the differences in clinical symptoms in a cohort of NTM-PD patients who received either antibiotic treatment or conservative treatment to gain a better understanding of the clinical decision making process to start antibiotic treatment.
Methods:
We performed a retrospective cohort study in 34 NTM-PD patients. All subjects completed the Nijmegen Clinical Screening Questionnaire (NCSI) and functional tests (6MWT, maximal voluntary strength of M. Quadriceps and handgrip strength).
Results:
MAC species were the most common causative agents (28/34; 18 M. avium, 7 M. chimaera and 3 M. intracellulare); 44% (15/34) of the patients started antibiotic treatment. In both groups, the majority of the patients had a nodular-bronchiectatic form (conservative: 12/19, antibiotic 9/15). The antibiotic treatment and conservative treatment groups had similar pulmonary function and physical capacity (6MWT, quadriceps muscle strength and handgirip sttrength). Patients who started antibiotics reported significantly lower health-related QoL scores and higer depression scores. About a third of these patients (36%, 4/11) had a score which would classify them as depressed. Furthermore, the group who started antibiotic treatment had a significantly lower BMI and FFMi. About half of these patients (53%, 8/15) would be classified as cachectic (BMI < 21.0 kg/m2 and FFMi < 15.00 kg/m2).
Conclusions:
NTM-PD patients who start antibiotic treatment have a worse HR-QoL, higher depression scores, a lower BMI and lower FFM index. One third of these patients could be classified as depressed and half of these patients could be classified as cachectic. Recognition of these features can assist in the decision-making process for pulmonologists to start treatment, but early recognition and intervention may be even better. Quality of life and functional tests should be part of NTM-PD management.
Nontuberculous Mycobacterial I and II —Abstract 41
Effect of Conservative or Antibiotic Treatment in NTM-PD Patients on Physical Capacity, Pulmonary Function and Cough Complaints During 3 Month Follow-Up
Susan Lassche, MSc1 Wouter Hoefsloot1 Jakko van Ingen, MD, PhD1
Author Affiliations:
1. Radboud University Medical Center, Nijmegen, Gelderland, Netherlands
Background:
Management of Nontuberculous Mycobacterial pulmonary disease (NTM-PD) requires much more than antibiotics. This study aim to investigate the effects of a multidisciplinary approach (a chest physician, dietician, nurse and respiratory physiotherapist) on NTM-PD during a 3 month follow-up.
Methods:
This study is set up as a prospective cohort study starting from August 1st 2022. Patients performed baseline measurements including demographics, questionnaires (Nijmegen Clinical Screening Questionnaire) and functional tests. These measurements are repeated at 3 months. Patients received conservative treatment (among other saline inhalation, nutritional advice and couching techniques) or antibiotic treatment (according to the ARS/ETS guideline).
Results:
Up till now, 28 patients are included. Of these patients, 20 patients received conservative treatment and 8 patients received antibiotic treatment. At baseline, the antibiotic group had a significantly worse pulmonary function, lower BMI, lower 6MWD and quadriceps muscle strength, but less cough complaints, better Quality of Life and lower anxiety score. After 3 month follow-up, a statistically significant and clinically meaningful difference in the LCQ score was found in the conservative treatment group; this group had significantly less cough complaints after 3 months. No such results were seen (yet) in the antibiotic group.
Conclusions:
In NTM-PD, significant clinical improvements can be expected on a conservative treatment approach when applying appropriate patient selection. These preliminary results of this ongoing study show promising short-term results in the conservative group. The durability of these results remains uncertain. The inclusion process is still open and should give more data in the future. The effects in the antibiotic group remain to be seen, especially for the decisive parameters to start antibiotic treatment.
Nontuberculous Mycobacterial I and II —Abstract 42
Nontuberculous Mycobacteria Testing and Culture Positivity in Florida Using Labcorp Data
Julia Marshall, BS1 Rachel A. Mercaldo, PhD1 Ettie M. Lipner, PhD, MPH1 Max Salfinger, MD2 Rebecca Prevots, PhD, MPH1
Author Affiliations:
1. NIAID, NIH, Bethesda, Maryland, United States
2. College of Public Health & Morsani College of Medicine, University of South Florida, Tampa, Florida, United States
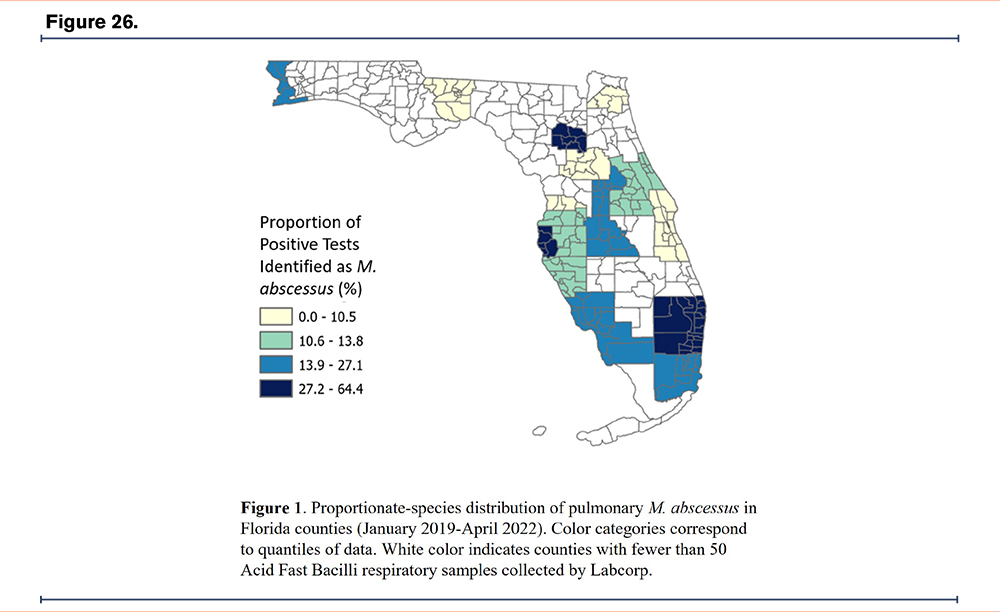
Background:
The prevalence of NTM pulmonary infection and disease is increasing in the United States (U.S.) and represents an increasing public health burden. Florida is a ‘hotspot’ for NTM in the U.S. and has a high burden of Mycobacterium abscessus, a difficult to treat infecting species. More current and precise data are needed from Florida to direct interventions. The development of PCR probes for rapid NTM detection has driven NTM testing by commercial laboratories. Real-time microbiology results are available from Laboratory Corporation of America (Labcorp) through the Centers for Disease Control and Prevention. We analyzed these data to estimate NTM culture positivity prevalence by county and describe the proportionate species distribution.
Methods:
We analyzed data from respiratory samples sent for Acid Fast Bacilli (AFB) cultures from January 2019 to mid-April 2022. We defined NTM positive results as those that identified an NTM species. We excluded tests that identified Mycobacterium tuberculosis complex species or Mycobacterium gordonae. We excluded counties with 50 or fewer tests from our county-level analysis.
Results:
9,110 samples were sent from the state of Florida to Labcorp for AFB testing from January 2019 through mid-April 2022. The counties with the highest total NTM positivity were: Alachua (72.7%) and Pinellas (67.5%). The proportionate distribution of species varied by county: the proportion of samples which were M. abscessus was highest in Pinellas County (64.4%) and 5 counties reported no positive tests for M. abscessus. The proportion of positive tests that were identified as Mycobacterium avium complex was highest in Hernando County (88.2%) and lowest in Broward County (13.0%).
Conclusions:
Southeast Florida had the highest culture positivity for M. abscessus. Although samples sent to Labcorp may not be representative of those from all persons with suspected NTM, these findings nevertheless provide a view of high-risk in Florida.
Nontuberculous Mycobacterial I and II —Abstract 43
Patient-Reported Perspectives on Nontuberculous Mycobacterial Lung Disease Care – Results from a European Patient Survey
Roald van der Laan, PhD1 Christian Hoenig2 Roger Legtenberg2 Andreas Reimann2 Marko Obradovic3
Author Affiliations:
1. Insmed, Utrecht, Netherlands
2. admedicum, Cologne, North Rhine-Westphalia, Germany
3. Insmed, Frankfurt, Hessen, Germany
Background:
Nontuberculous mycobacterial lung disease (NTM-LD) is a rare but growing health concern, particularly affecting vulnerable patients with chronic lung conditions. Learning from patients about their disease experience can inform decision-making and improve NTM-LD-care. The survey aimed to understand patients’ needs, identify gaps in patient care, and gain insights into how the disease impacts patients’ daily life.
Methods:
Patients with self-declared active NTM-LD (recruited via communities, online ads/social media and flyers) from 8 European countries were recruited. This is the sub-analysis of the survey data on patients’ perspectives on NTM-LD-care. The survey consisted of an online questionnaire, supported by semi-structured interviews providing qualitative insights (both in local language).
Results:
543 NTM-LD patients met inclusion criteria of which 82% (n=443) were >50 years of age, 73% (n=195) were female and 68% (n=369) were currently under treatment. 23 patients participated in an interview.
About one-third of patients were highly satisfied with care aspects like finding an expert (31%, n=125), efforts needed to get referred (32%, n=128) or and time to diagnosis (30%, n=114). The majority of patients (56%, n=262) noticed first symptoms more than 2 years before diagnosis. An expert was responsible for therapy for only 16% (n=38) of patients. About one-third of patients were highly dissatisfied with information received, specifically on NTM-LD in general (31%, n=108) or how patients can support their treatment (31%, n=69)). Most patients (62%, n=179) did not participate in support services. Of those who used support services, only 29% (n=32) used psychological support while simultaneously 75% (n=203) reporting suffering from a negative emotional impact of NTM-LD. From the conducted interviews, it appears that psychological support was not always offered.
Conclusions:
NTM-LD patient care needs to be improved. Special attention should be paid to faster diagnosis and improving access to specialized care and information for patients.
Sputum and Airway Clearance—Abstract 44
Mucus Clearance from the Trachea in a Helix: A Novel Angle on Airway Diseases
David Abelson, BSc, MBBS, FRACP1 James Di Michiel1 Clayton Frater1 Mark Pearson1 Robert Russo1 Martin Wechselberger2 Alice Cottee1 Lucy Morgan, Bmed, PhD1
Author Affiliations:
1. Concord Hospital, Sydney, New South Wales, Australia
2. University of Sydney, Sydney, New South Wales, Australia
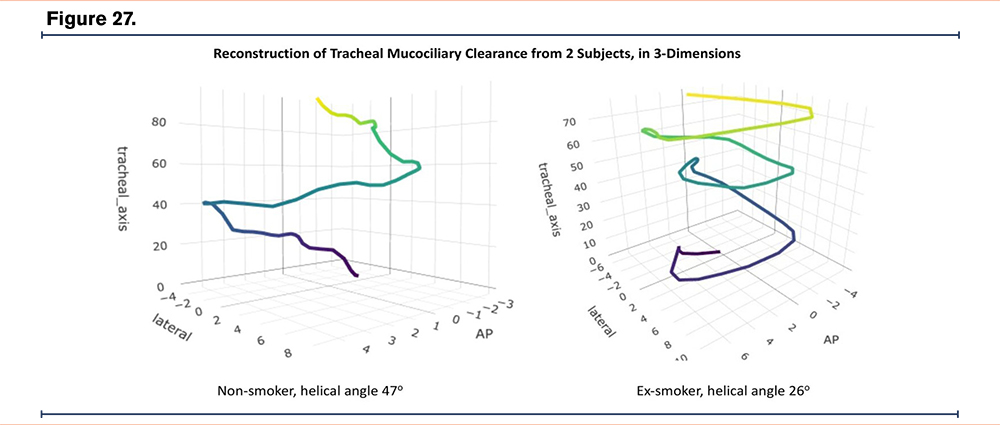
Background:
Mucociliary clearance (MCC) is critical to lung health. In ex-smokers, we have previously shown that MCC in the trachea, measured by cephalad velocity (distance, solely in the cephalad direction, over time), is reduced. This may be because MCC in ex-smokers is slower, assuming that MCC travels linearly, axial to the trachea. However, the path of MCC in the trachea has never been rigorously studied.
Methods:
Tracheal MCC was imaged in twelve ex-smokers and three non-smokers. Droplets of radio-labelled macro aggregated albumin were injected through the cricothyroid membrane; to coat the carina. Scintigraphy recorded MCC from anterior and lateral cameras. MCC coordinates were tracked and an axial versus helical model compared.
Results:
MCC was helical in 9/12 ex-smokers and 3/3 non-smokers (p ≤ 0.05 compared to axial transit, for each study). In 3/12 ex-smokers, MCC was negligible.
Helical angle varied widely (range: -13 to 61 degrees) (see figure for two examples). Mean helical angle was 21 degrees in ex-smokers, 49 degrees in non-smokers (p=0.04).
Mean cephalad velocity was 2.8mm/min versus 8.4mm/min (p=0.02) and correlated to helical angle (r=0.91, p=0.00003), but was independent of overall speed (velocity on helical path) (r=0.29, p=0.32).
Ten subjects repeated imaging after long-acting bronchodilator (LABA). All had helical MCC (p< 0.05 each) including two who previously had negligible MCC. In those with existing helical MCC, LABA increased overall speed (p=0.019) but did not effect helical angle or cephalad velocity.
Conclusions:
We have shown for the first time that tracheal MCC is helical. Two phenotypes of MCC disease were identified, first muco-stasis; second, individuals in whom changes in helical angle (rather than speed) affect cephalad velocity.
Phenotype specific effects of medications were identified using scintigraphy. In muco-stasis LABA re-started helical movement, while in helical transport it increased overall MCC speed without affecting helical angle or cephalad velocity.
Sputum and Airway Clearance—Abstract 45
Rationale and Design of the Pilot Study to Evaluate the Use of The Vest System for Treatment of Non-Cystic Fibrosis Bronchiectasis Patients in the Home Setting
Martha Camacho Urribarri, RN, BSN1 Ashwin Basavaraj, MD2 Clyde Southwell, MD3 Daniel Belz, MD, MPH4 Brian Becker, MEd, RRT1
Author Affiliations:
1. Baxter, St. Paul, Minnesota, United States
2. NYU Grossman School of Medicine, New York, New York, United States
3. Tennessee Comprehensive Lung and Sleep Center, Hendersonville, Tennessee, United States
4. The Johns Hopkins University School of Medicine, Baltimore, Maryland, United States
Background:
High frequency chest wall oscillation (HFCWO) therapy is prescribed to provide routine airway clearance in patients with bronchiectasis. HFCWO is generated via an air pulse generator and an inflatable garment that delivers pressure pulses to the thorax. These pressure pulses against the chest wall create oscillation of the chest wall and generate high-frequency air pulses within the lung. Oscillation airflow has been shown to mobilize pulmonary secretions and study outcomes have shown improved mucus production and pulmonary function. There is limited clinical data evaluating HFCWO in patients with non-cystic fibrosis bronchiectasis (NCFBE). Study rationale is to assess the efficacy of HFCWO compared to a standard airway clearance modality in the NCFBE population.
Methods:
The study is a non-blinded prospective randomized control trial (RCT) comparing patients with NCFBE randomized to HFCWO therapy (interventional group) to patients randomized to oscillating positive expiratory pressure (OPEP) therapy (control group). The primary endpoint is frequency of acute pulmonary exacerbations. Secondary endpoints include the impact on pulmonary function and quality of life. Patient inclusion criteria include high resolution CT scan diagnosis of bronchiectasis, history of at least 2 acute pulmonary exacerbations in the past 24 months, clinically stable, latest FEV1 ≥ 30% predicted, age 18-80 years.
Results:
This pilot study began enrolling patients in the fall of 2019, with an enrollment goal of 70 patients (1:1 randomization between the two groups). All patients will be followed for up to 18 months, resulting in an estimated trial end date of Q3 2025.
Conclusions:
This trial is a multi-centered RCT to evaluate and compare the efficacy between HFCWO and OPEP therapies in patients with NCFBE. This trial hopes to provide more insight into airway clearance therapies in patients with bronchiectasis.
Sputum and Airway Clearance—Abstract 46
Effects of High Frequency Chest Wall Oscillation on Quality of Life in Bronchiectasis
Christina Cheng1 Meaghan Bruner1 Clarissa Bazan1 Bo Liu2 Lloyd Edwards1 George M. Solomon, MD1 Chad Marion3
Author Affiliations:
1. University of Alabama at Birmingham, Birmingham, Alabama, United States
2. University of Alabama at Birmingham Internal Medicine, Birmingham, Alabama, United States
3. Wake Forest University, Winston-Salem, North Carolina, United States
Background:
Chronic sputum production impacts quality of life (QOL) in many patients with bronchiectasis; thus, enhancement of mucociliary clearance is a mainstay of therapy. High Frequency Chest Oscillation (HFCWO) therapy is a cornerstone of mucus clearance treatment in bronchiectasis. We hypothesized that routine utilization of HFCWO therapy (SmartVest®, Electromed, Inc.) would improve QOL in bronchiectasis patients.
Methods:
This was a prospective, non-randomized, open-label, observational study utilizing Quality of Life-Bronchiectasis (QOL-B) questionnaires administered at baseline (day 0), 30, and 90 days following HFCWO initiation. Repeated measures data were analyzed with paired t-tests or ANOVA with multiple comparisons tests as appropriate. A linear mixed model subsequently analyzed the contribution of race, gender, and days after initiation of HFCWO on QOL-B scores.
Results:
Our cohort of bronchiectasis patients (n=115) included 82 females (71%) and 33 males (29%). We observed statistically significant improvements in self-reported QOL-B scores in all parameters except for “Treatment Burden” at 30 and 90 days compared to baseline. Patients saw significant improvement in “Respiratory Symptoms” at day 30, which continued at day 90 (59.92+/−20.83 at baseline versus 63.56+/−17.44 at 30 days and 65.82+/−17.41 at 90 days), demonstrating clinical significance (greater than the MCID of 8.1). Large improvements were also observed in “Vitality” and “Health Perceptions” parameters within the same timeframe. A multivariable linear mixed model indicated that days after initiation of HFCWO was statistically significant but neither gender nor race were significant variables contributing to the primary outcome.
Conclusions:
This open-label study demonstrates statistically significant favorable responses to HFCWO as adjunctive therapy for patients with bronchiectasis. Significant improvements were observed in overall sub-scores of the QOL-B, indicating that mucociliary clearance promotion via HFCWO therapy has large implications on overall patient satisfaction and symptom burden in this population. Effects seen in this small cohort were independent of demographics, suggesting broad effectiveness.
Sputum and Airway Clearance—Abstract 47
Evaluation of Home Collected Sputum for Increased Access to High Quality Laboratory Testing of Nontuberculous Mycobacteria
Reeti Khare, PhD1 Helen Ballard2 Amy Leitman3 John Torrence2 Elisha Malanga2 Jane Baer1 Linda Walsh2 David Trollinger1 Charles L. Daley, MD1
Author Affiliations:
1. National Jewish Health, Denver, Colorado, United States
2. COPD Foundation, Miami, Florida, United States
3. NTM Information and Research, Palmetto Bay, Florida, United States
Background:
Approximately 180,000 people in the US suffer from nontuberculous mycobacterial (NTM) lung disease, with infections increasing by ~8% each year. Accurate diagnosis and monitoring can be burdensome and time-consuming for patients, and lack of access to full-service laboratories may result in inconclusive or inadequate test results. Home sputum collection may increase provider and patient access to appropriate diagnostic methods.
Methods:
Providers in the US (excluding New York) ordered home sputum collection (HSC) kits at no-cost to them. Kits were delivered from a full-service mycobacteriology laboratory directly to their patient’s home. Video and written instructions were provided to assist with proper collection of sputum, and pre-paid mailers allowed patients to return samples directly to the laboratory. Test results were reported to the provider. A multi-choice survey was required for provider participation in the program. Results from the survey and laboratory (SOFTLab) were analyzed.
Results:
Providers (N=57) reported seeing a median of 8 NTM patients/quarter. Only 30% reported being satisfied with their current testing options, with most needing complete organism identification (96%), susceptibility testing (96%), and genotypic drug resistance markers (89%). Most (74%) had no prior experience with HSC, but expected it to reduce turnaround time of testing (89%) and increase NTM diagnosis (86%). HSC was utilized by patients from 15 states from 9/1/2021-1/24/2023. Most samples originated from Florida (38%), followed by California (17%). A total of 82 patients (female=71%) sent 109 samples. Of these, 50% (41/82) of patients and 40% (44/109) of cultures were positive. Organisms recovered (n=47) represented 16 different NTM or aerobic actinomycetes.
Conclusions:
A range of organisms were recovered successfully from half of the patients collecting sputum at home. Most providers hypothesized that that the primary drivers of HSC is ease of access rather ran risk of contagion. Further data are being collected to assess patient perspectives.