Running Head: Variations in COPD Health Care Access and Outcomes
Funding Support: This research was supported by funding from the Scientific Office of the Respiratory Health Section of the Medicine Strategic Clinical Network, Alberta Health Services.
Date of Acceptance: January 12, 2024 | Publication Online Date: January 19, 2024
Abbreviations: ACOS=asthma-COPD overlap syndrome; AHS=Alberta Health System; AI=American Indian; aRR=adjusted relative risks; BRFSS=Behavioral Risk Factor Surveillance System; CAT=COPD Assessment Test; CCG=Clinical Commissioning Group; CI=confidence interval; COPD=chronic obstructive pulmonary disease; ED=emergency department; FFS=fee for service; GP=general practitioner; HR=hazard ratios; ICD-9 (-10): International Classification of Diseases-9th Revision (10th Revision); IMD=Index of Multiple Deprivation; IP=inpatient; LBs=long-acting bronchodilators; LOS=length of stay; NR=not reported; mMRC=modified Medical Research Council; NHB=non-Hispanic Black; NHW=non=Hispanic White; NOS=Newcastle Ottawa Scale; NZDep=New Zealand Index of Deprivation; OR=odds ratio; PCP=primary care provider; PCT=primary care trust; PR=pulmonary rehabilitation; QoL=quality of life; SES=socioeconomic status; VHA=Veterans Health Administration
Citation: Shatto JA, Stickland MK, Soril LJJ. Variations in COPD health care access and outcomes: a rapid review. Chronic Obstr Pulm Dis. 2024; 11(2): 229-246. doi: http://doi.org/10.15326/jcopdf.2023.0441
Online Supplemental Material: Read Online Supplemental Material (230KB)
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic condition characterized by progressive airflow obstruction, which has a substantial impact on both patients1 and health care systems.2 Effective and integrated management of COPD, both on an individual and population-wide scale, requires an understanding of how health equity and social determinants of health can impact a person’s illness experience. Health equity or inequity is also intrinsically tied to health care access; defined as the ability to obtain health care services, including the diagnosis, treatment, and management of diseases.3 Furthermore, an individual’s level of access to health care has a profound effect on their health outcomes, including morbidity and mortality.
Health inequities are described as the unjust differential allocation of health care resources and/or differing health status between different population groups, arising from social factors.4 Consequently, health inequities may develop when variations in health care access and outcomes, between different demographic groups of patients, are unwarranted.5 Such inequities can result in poorer health outcomes for already marginalized populations.4 Health inequities have been identified among individuals with COPD worldwide.6 Individuals with COPD of lower socioeconomic status (SES), living in rural settings, and those from marginalized communities often have decreased access to health care that is necessary to manage and treat their condition.6 Furthermore, this correlation between the aforementioned demographic variables and decreased access to COPD care has been investigated and established in grey literature reports from multiple countries.7-9 Thus, these determinants of health care access are considered important in the study of COPD care and policy and continue to be the focus of many health authorities.
To inform solutions aimed at resolving health inequities experienced by individuals with COPD, it is imperative that we identify whether and where equity-related variations in health care access and health outcomes exist. As such, the objective of this research was to examine the existing literature surrounding equity-related variations in health care access and health outcomes for individuals with COPD.
Methods
A rapid review of the published and grey literature reporting variations in health care access and/or relevant health outcomes for individuals with COPD was completed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses,6 where applicable. For this review, we considered variations in terms of differential patterns of health care access indicators or health outcome metrics within any of the sociodemographic categories examined by an included article, which included but were not limited to sex, gender, age, geographic location (or rurality), race, ethnicity, SES, level of education, and income.
Search Strategy
A comprehensive electronic database search strategy for published literature was developed by an information specialist. Specifically, MEDLINE and EMBASE were searched from January 1, 2012 to August 2, 2022; the complete search strategies for both databases are outlined in Appendix 1 in the online supplement. Terms such as “variation* in care,” “health inequity,” and “health care access” were combined using the Boolean operator “and” with terms such as “length of stay,” “quality of life,” and “hospital discharge,” as well as terms such as “COPD” or “chronic obstructive pulmonary disease.” Results were limited to studies in English, published within the past 10 years, and conducted in North America, Europe, Australia, and New Zealand only. Limiting results to these countries was necessary due to the rapid nature of this review. As we approached this work from the lens of a provincial Canadian health care system context, studies from these limited jurisdictions were also selected due to the comparable aspects of their health care systems and their routine comparison in terms of health care system performance.10 Only original research and review articles were included. A scan of the grey literature using the first 5 results pages of a Google search was also performed to supplement the information collected from the published peer-reviewed literature. The search terms used in this grey literature scan were “COPD,” “atlas of variation,” “health outcomes,” and “health care access.” Eligibility of grey literature reports was assessed in accordance with the same inclusion and exclusion criteria listed in Appendix 2 in the online supplement.
Selection of Literature
Studies were included if:
- they were primary observational studies or review articles in which the population studied were adult patients with COPD,
- the study objective was to evaluate and/or define health care access and/or related health outcomes for individuals with COPD,
- the outcome assessed potential variation or disparities in health care access and/or outcomes and,
- such outcomes were assessed within sociodemographic subgroups of COPD patients (e.g., females, older age, lower SES, etc.).
Studies were excluded if they did not meet the criteria above and were also excluded if the primary study objective was to assess the effectiveness of an intervention and/or quality improvement initiative/program. A complete list of inclusion and exclusion criteria is available in Appendix 2 in the online supplement. An initial sample of 20 citations was screened by 2 independent reviewers to assess reliability, with any disagreement between reviewers resolved through discussion and consensus. All remaining screening was performed by one reviewer, with final inclusions discussed and reviewed by the entire research team.
Data Extraction and Analysis
Data from the included studies was extracted using standardized data extraction forms. For all studies, author, study design, publication year, country, the number of participants, and population characteristics including age, study duration, quantitative and qualitative data assessing variations in health care access indicators, as well as quantitative and qualitative data assessing variation in health care outcomes were extracted. When reported, the breakdown of study participants by relevant sociodemographic variables was also extracted. Major themes among included studies were identified inductively and synthesized narratively. Specifically, studies that assessed variation in health care access indicators were grouped according to which aspect of the continuum of care (prevention, diagnosis, and treatment or management) was most relevant to the indicators assessed. Studies that assessed variation in health care outcomes were grouped according to whether their outcome metrics reflected the patient and/or systems level. The Newcastle Ottawa Scale (NOS) was used to assess the risk of bias among included cohort studies.11 As this scale was originally designed for cohort and case-control studies, a previously adapted NOS was also utilized to assess risk bias among the included cross-sectional studies.12 The risk of bias assessment was completed by one reviewer.
Results
Search Results
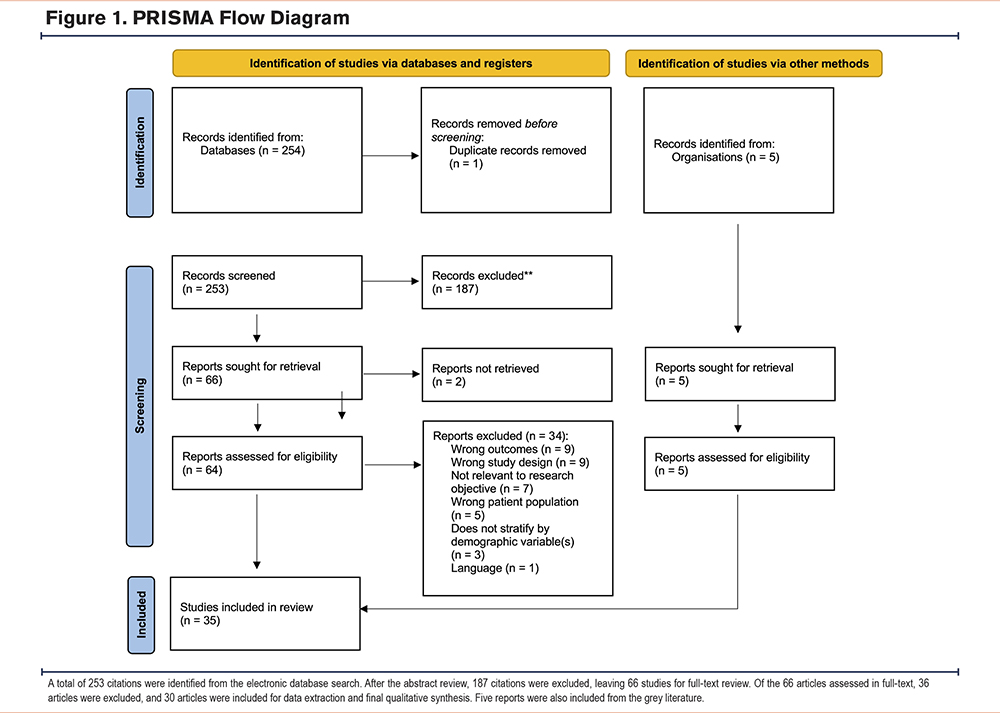
A total of 253 citations were identified through the electronic database search. Of those, 187 were excluded after abstract review, leaving 66 studies for full-text review. Thirty-six studies were excluded after full-text review and 30 articles were included in the final analysis (Figure 1). Five reports were included from the grey literature scan, all of which assessed and identified geographical variation in COPD access to care and/or outcomes.7-9,13,14
Characteristics of Included Studies
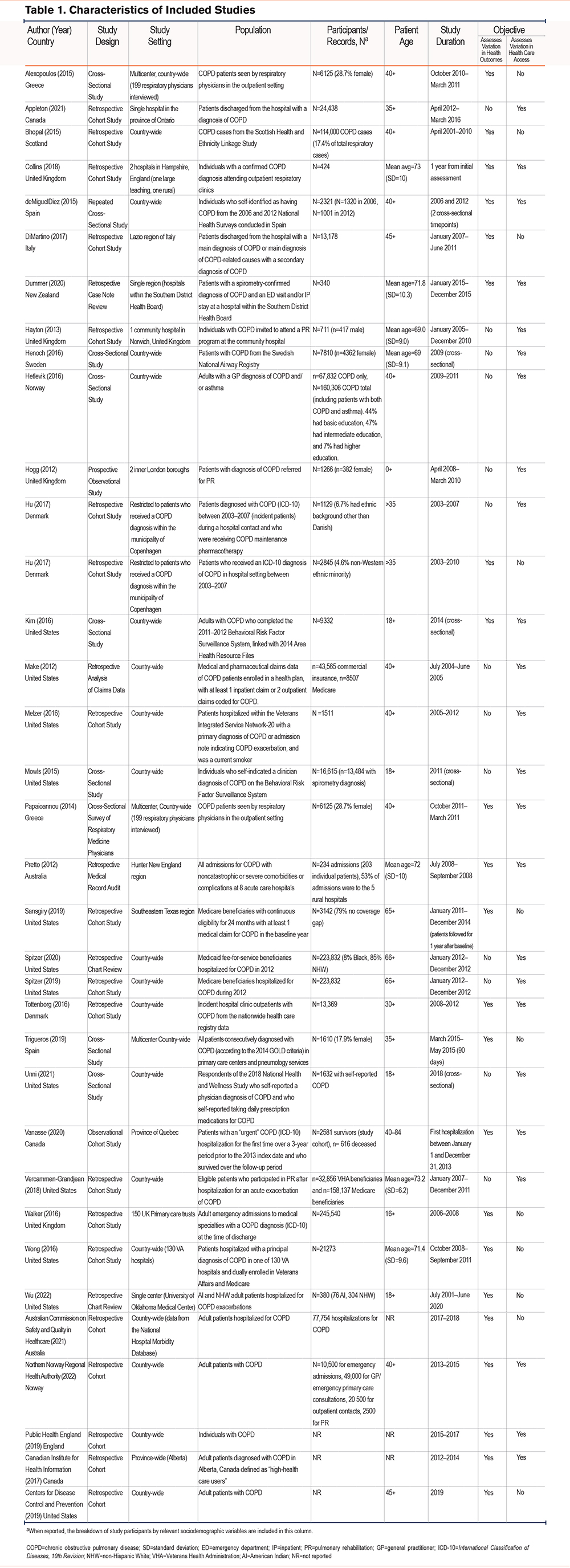
The characteristics of the 35 included studies are summarized in Table 1. The included articles were published between 2012 and 2022. The majority of studies were conducted in Europe (n=17) and the United States (n=12) with 3 published in Canada, 2 in Australia, and 1 in New Zealand. Most studies were retrospective cohort studies (n=24)7-9,13-33 and the majority reviewed administrative health data or patient charts with a physician diagnosis of COPD (e.g., COPD case definition based on International Classification of Diseases-10th Revision [ICD-10] codes). The remaining studies were prospective observational cohort studies (n=2)34,35 and cross-sectional studies (n=9),36-44 which included, for example, health surveys that rely upon the self-reporting of a COPD diagnosis by patients. In terms of study setting, 21 studies were country-wide,7,13,14,16,23,24,27-30,32,36-44 9 were specific to a smaller region of a country (e.g., the province of Alberta, Canada),9,18,19,21,22,25,26,31,35 and 5 were set in either a single center/hospital or multiple hospitals.15,17,20,33,34 All patients in the included articles were adults (age 18+) diagnosed with COPD. Appendices 3 and 4 in the online supplement detail the NOS risk of bias scores for all included cohort studies, including those from the grey literature, and cross-sectional studies, respectively. Broadly, the 26 included cohort studies from the published and grey literature scored between 4 and 9 on the NOS suggesting minimal risk of bias. The median score among studies was 7, with the majority of studies (n=20) scoring 7 and above (e.g., low risk of bias). Similarly, the NOS risk of bias scores for the 9 included cross-sectional studies ranged from 5–9, with a median score of 7 (e.g., low risk of bias). Importantly, no included studies had unsatisfactory scores (e.g., 0–3).
Study Outcomes
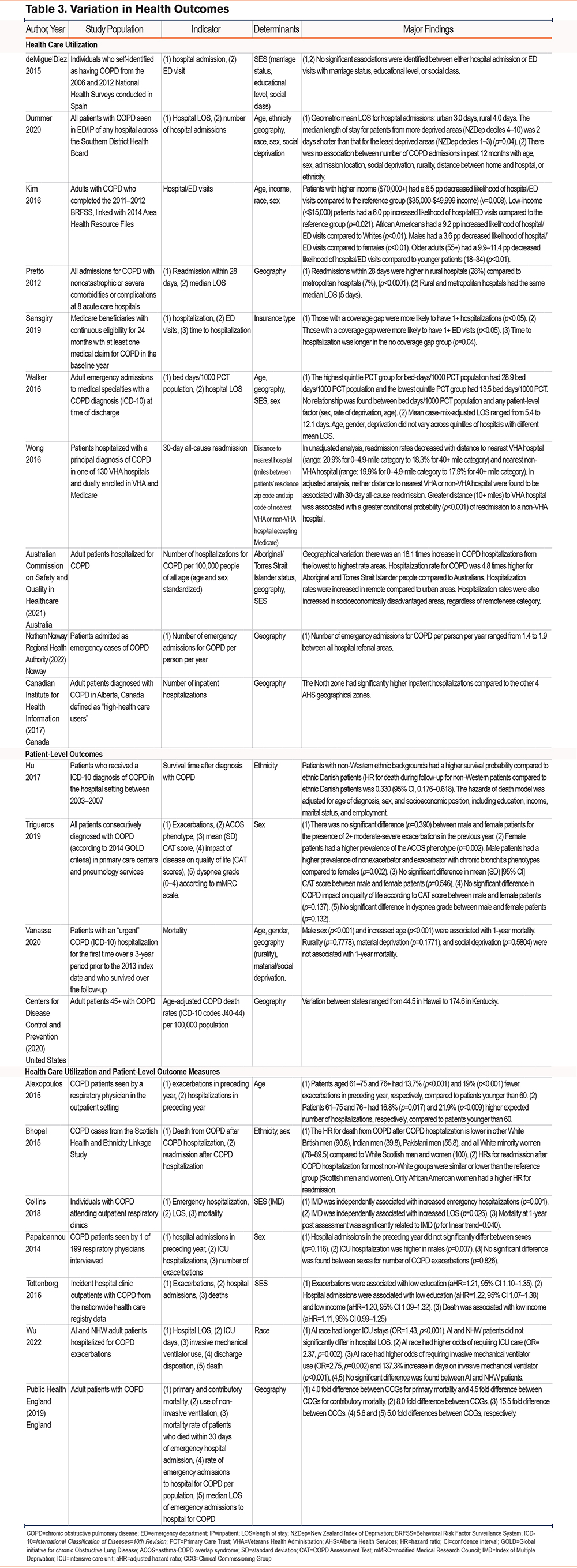
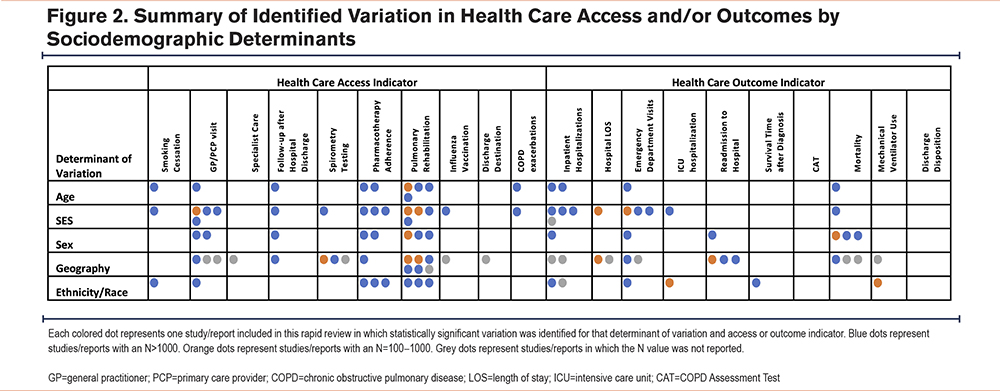
The major findings from the included studies are reported in Table 2 and Table 3. Statistically significant findings from the included studies are also summarized in Figure 2.
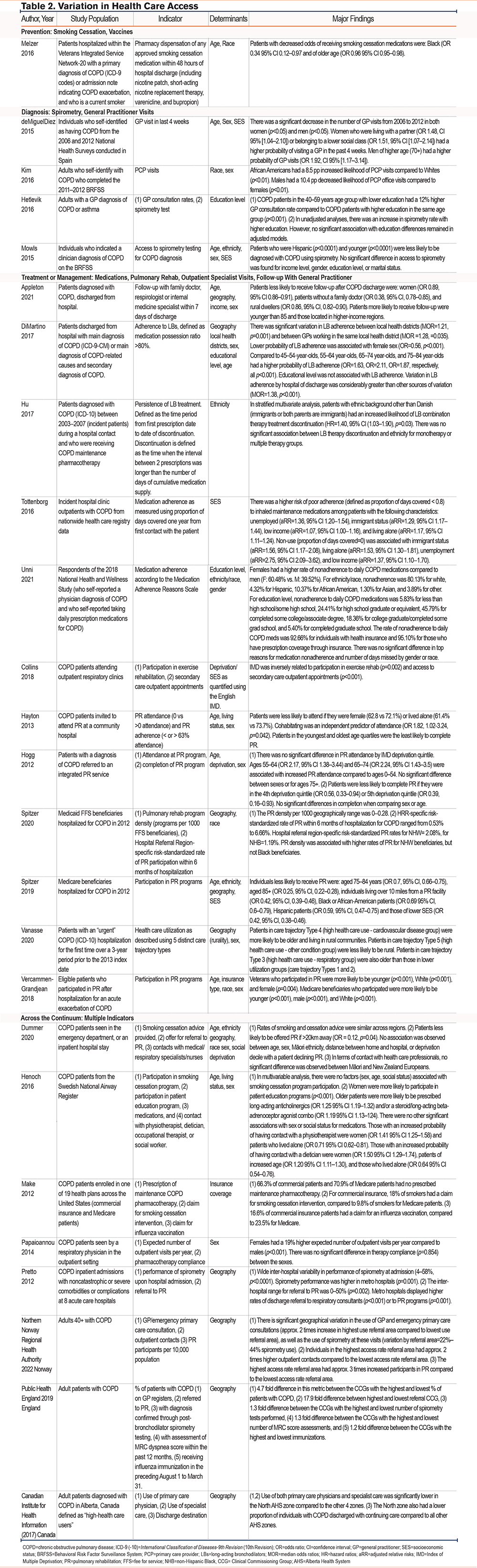
Variation in Health Care Access
Table 2 presents a summary of the main findings from the 25 studies that assessed variations in access to health care for COPD patients. Studies were identified across the following stages within the continuum of care: prevention (n=1)24,45; diagnosis (n=4)37,39-41; treatment or management (n=12).15,17,18,20,21,27-30,34,35,44 Additionally, 8 studies reported indicators across the continuum and were grouped into a “pan-continuum” category.8,9,13,19,23,25,38,42 No studies investigated variation in access to palliative care or primary prevention interventions.
Prevention: Four studies examined variation in the secondary prevention stage.19,23,24,38 In a cohort of 1511 individuals with COPD, the authors identified that individuals who were Black or of older age had significantly reduced odds of receiving smoking cessation medication within 48 hours of hospital discharge.24
Diagnosis: The most common access indicator around diagnosis was access to spirometry testing (n=5 studies).13,25,39,41 Mowls et al identified that patients who were Hispanic and younger were less likely to be diagnosed with COPD using spirometry. Access to spirometry testing does not appear to vary according to educational level.39 In a retrospective medical record audit of 234 COPD admissions at 8 acute care hospitals in the Hunter New England Region of Australia, Pretto et al (2012) identified wide interhospital geographical variability in access to spirometry testing upon admission.25
Treatment or Management: Key access indicators around the treatment of COPD were primarily focused on medication adherence (n=7 studies)18,21,23,29,38,42,44 and referral to or completion of pulmonary rehabilitation (PR) (n=10 studies).8,13,17,19,20,25,27,28,30,34 The probability of adherence to COPD maintenance medications was found to be lower for female patients.18,44 In a retrospective study of 13,369 incident outpatients with COPD, adherence to COPD maintenance pharmacotherapy was also found to be lower in individuals with a lower SES, specifically those who are unemployed, living alone, immigrants, or of low income.26 Interestingly, Di Martino et al (2017) found that the geography of a patient’s hospital of discharge was a stronger determinant of adherence to long-acting bronchodilators, and therefore, a stronger source of potential unwarranted variation compared to other patient-level factors, including age, educational level, and sex.18
Across studies, PR access at the patient level was examined by frequency of PR program attendance, adherence (e.g., > 63% attendance rate), and/or completion. The included studies report conflicting results regarding the influence of age, sex, and SES on an individual’s PR access. For example, Hayton et al found that women were less likely than men to attend PR at a community hospital in the United Kingdom.20 However, a prospective observational study in 2 inner London (United Kingdom) boroughs suggested that there was no significant difference in PR attendance between males and females.34 Access to PR was also examined at a health care system level in terms of regional program density and was found to vary considerably by geographic region within the United States.27,28 Similar findings were observed in the United Kingdom, with metropolitan hospitals reporting more frequent referrals of discharged patients to pulmonary specialists or PR in comparison to rural hospitals.25 Also, for outpatient COPD treatment, 3 studies compared general practitioner (GP) and primary care provider (PCP) visits among patient populations and found that patients with a significantly decreased likelihood of visiting a GP/PCP were male.40 Patients with a significantly increased likelihood of visiting a GP/PCP were women belonging to a lower social class,37 older (age 70+) men,37 African Americans,40 and middle-aged COPD patients with lower education.39
Six studies also assessed variation in access to long-term COPD care or management, including outpatient specialist visits and follow-up with GPs following an initial hospitalization.8,9,13,15,35,42 One large 4-year retrospective cohort study of COPD patients following hospital discharge in Ontario, Canada found that patients were significantly less likely to receive follow-up with a family doctor, respirologist, or internal medicine specialist within 7 days of discharge if they were female, did not have a family doctor, or lived in a rural location.15 Patients from higher-income regions and those younger than 85 years old were more likely to receive follow-up.15 In a report of adult patients diagnosed with COPD in Alberta, Canada, geographical location in terms of patient residence prior to hospitalization was concomitantly associated with variation in GP access, and specialist care, as well as discharge destination from acute care.9 No studies focused on patient access to respiratory therapists.
Variation in Health Outcomes
A total of 21 of the included studies examined variation in health outcomes in COPD (Table 3) in terms of health care utilization (n=10),7-9,19,25,26,31,32,37,40 patient-level outcomes (n=4),14,21,35,43 or both (n=7).13,16,17,29,33,36,42
Health Care Utilization: The health care utilization outcomes focused primarily on hospital-based resource use, including COPD exacerbations requiring inpatient hospitalization,26 emergency department (ED) visits,37 hospital length of stay (LOS),19 and hospital readmissions.32
The impact of age, geography, sex, and SES on variations in hospitalizations and ED visits is mixed (Table 3). For example, a retrospective medical record audit from Australia found that despite increased readmission rates in rural hospitals, the median LOS did not significantly differ between rural and metropolitan settings.25 In contrast, a similar study from New Zealand found that the geometric mean LOS was 1.0 day longer for rural hospital admissions compared to urban.19 In addition, the impact of an individual’s SES—which may include related determinants such as education, insurance coverage, and living status—on health resource utilization was examined in n=6 studies.7,19,26,31,37,40 Various indices were used to quantify aspects of SES, including the English Index of Multiple Deprivation (IMD). For instance, in a retrospective cohort study of COPD patients attending outpatient respiratory clinics, higher IMD scores (more deprived areas) were independently associated with increased emergency hospitalizations, longer LOS, and patient mortality at 1-year post-initial-assessment.17
COPD Patient Outcomes: The most common patient-level outcome evaluated was mortality (n=3).14,22,35 One study also investigated patient quality of life (QoL), dyspnea grade, and COPD Assessment Test (CAT) score.43 Increased mortality in COPD patients may be associated with male sex,35 increased age,35 and lower SES.17,29 Associations between mortality and ethnicity/race were less conclusive.16,22,33 A cross-sectional analysis investigating the impact of COPD on QoL found no significant difference in CAT scores between males and females.43
Acute COPD exacerbations, which affect health outcomes at the patient level but also commonly result in the need for inpatient hospitalization, are more likely in younger patients36 and those with lower education.29 Two cross-sectional studies in Europe found no significant difference in COPD exacerbations by sex.42,43
Four studies evaluated mortality among COPD patients concomitant to health system-level outcomes, such as acute care LOS and readmissions, and found that SES,17,29 age,36 and race33 led to statistically significant variations in these outcomes.
Discussion
Through this rapid review, we identified several studies from the published and grey literature that report differential patterns of health care access and health outcomes for individuals with COPD. As summarized in Figure 2, substantial variation was detected in health care access in terms of PCP or GP visits, pharmacotherapy adherence, and pulmonary rehabilitation. Considerable variation in health outcomes was also observed for inpatient hospitalizations, and ED visits, as well as mortality. Most studies included in the present review characterized observed variation by differential access to care and/or health outcomes due to specific sociodemographic variables or determinants, such as a patient’s age, SES, sex, geography, and/or ethnicity or race. Geography was the most widely evaluated determinant of variation among included studies, with nearly half of the studies reporting statistically significant geographical variation in access to care (10 of 25 studies) and health outcomes (10 of 21 studies) for those with COPD.
The present rapid review expands on the current evidence base6 regarding health inequities for patients with COPD by examining how access and health outcomes can vary across the continuum of COPD care for a greater variety of patient subgroups (i.e., age, sex, SES, geography). It is important to note that the objective of most of the included studies was not necessarily to identify variation in COPD care, but rather to assess the differential impact of one or more sociodemographic variables on specific quality indicators relevant to individuals with COPD. However, in doing so, the findings from these studies suggest that variation in access and outcomes does exist in different subgroups, across a variety of clinical settings, and in varying health care systems.
A particular strength of this review is that we were able to understand how, where, and the extent to which variation has currently been studied and identified, as well as visualize where current gaps in the literature exist. For example, the current literature was primarily centered on the following indicators: inpatient hospitalizations (71%), mortality (38%), access to pulmonary rehabilitation (36%), access to primary care providers (32%), pharmacotherapy adherence (28%), and ED visits (24%). We found that, among included studies, health care access (Table 2) was studied more extensively—with more statistically significant findings—compared to health outcomes in different patient groups (Table 3), with much of the literature on variation in access focused on the treatment or management of COPD. In contrast, few studies examined variation in access to preventative care and no studies examined key prevention-related measures such as influenza vaccination rates; this represents a clear gap in the current literature (Figure 2). Given the importance of both primary and secondary preventative approaches in chronic disease progression, further study of variation in access to preventive care is warranted. Importantly, only 2 studies evaluated access to pulmonary subspeciality care.9,15 Referral and access to pulmonary physicians and/or respiratory therapists are critical to the overall understanding of variation in health care access for individuals with COPD, especially when considering geographic variation.
Of the different sociodemographic determinants studied, as noted, geography was most commonly associated with variation in both health access and outcomes. Three of the grey literature reports were described as “atlases of variation,” which are a series of reports summarizing how health care access and use vary depending on a person’s location within a country or region.7 All 3 atlases of variation identified significant variation in both access indicators across the care continuum, as well as health care utilization with geographical location.7,8,13 Specifically, patients living in rural and more deprived areas were frequently identified as being more likely to experience poorer health care access and health outcomes, even across different countries of study and COPD patient populations. However, geography alone is unlikely to be a sufficient surrogate for the effects of other determinants of variation. Thus, future atlas of variation projects would benefit from considering how additional sociodemographic factors, such as race, education, income stability, and gender, may intersect with geography and influence metrics of interest. Atlases of variation are important from both population surveillance and quality improvement stances, as they provide a context-specific visualization of where and for whom health policy changes and/or health care system intervention would be most impactful in reducing health inequities within a given region.
Race and ethnicity were also frequently identified determinants of variation in health care access and health outcomes for individuals with COPD. A focus on race is especially prevalent in studies from the United States.40 Mixed results were identified in terms of variation by ethnicity, and such variation is likely closely knit with other social determinants of health, including SES. When interpreting these studies, it is important to remember that race is a social construct and social context must be considered.46 Moreover, other factors or determinants of variation, such as SES and experiences of interpersonal and/or systemic racism, are likely more relevant determinants of health disparities and inequities as compared to race alone and should be integrated into future studies. The latter was not considered among the included literature which likely reflects the difficulty in capturing and stratifying results by ethnicity in studies of secondary data.47
Variation in access and outcomes due to differences in SES and sex were also mixed. For instance, variation due to SES was observed in hospitalization rates, hospital LOS, and ED visits for those with COPD. However, hospital readmission rates did not appear to differ by patient SES. The included studies also represented a bias towards reporting sex rather than gender. As such, there is a lack of literature concerning gender-based variation in COPD care and outcomes. Certainly, there appears to be a link between lower SES and worsened health care access, along with poorer health outcomes as a result, indicating an opportunity for intervention to improve the care of individuals with COPD of lower SES. However, such an intervention would be complex, as other upstream social determinants of health, including housing, financial security, and social support, should ideally be addressed first.48
Implications for Future Research
Given the number of determinants of variation identified through this rapid review, future research assessing the impact of intersectionality on variation in COPD health care access and outcomes is warranted. Intersectionality involves assessing how multilevel interacting social locations, determinants of health, and power structures can shape and influence human life and health.49 Within the context of this research, such an approach may involve evaluating the differential effects of intersectional strata on COPD-related outcomes. Our research results highlight a dearth of research assessing the extent to which intersectional variables, or the cumulative effect of multiple determinants of variation, impact access to care and health outcomes for individuals with COPD. This is a gap in the current knowledge surrounding health equity and access to care in COPD. Further, studies incorporating theories of intersectional theory are lacking in COPD research; these would provide critical insights for improving patient-centered care in this field.
To better inform health care professionals and policymakers on the differential allocation of resources and outcomes of individuals with COPD, future work should consider broadening assessments of variation to all stages of the care continuum, from prevention and screening to palliative care. This is particularly important for indicators of access to preventative and palliative care, where current research is highly limited or nonexistent. Improved understanding of variation within specific contexts (e.g., geographical locations and patients with similar demographics) may additionally help tailor future interventions by providing indications of where such an intervention should be applied (e.g., acute versus community care, rural versus urban) and for which specific target population the intervention should focus. An example of such a tailored, evidence-informed intervention approach might include an initiative to improve rural primary care provider’s compliance to COPD guidelines in terms of ensuring diagnosis is confirmed with spirometry.
Finally, we suggest that further consensus on standard indicators and/or benchmarks to assess access to care for those with COPD is required. Such an initiative would not only improve the generalizability of individual study findings to other jurisdictions but also permit better comparability of interventions to address access across studies. For example, one health outcome recognized internationally to evaluate health care utilization and efficiency among hospitalized patient groups—including those with COPD—is hospital LOS in days.50 Without such standardized benchmarks of access to care for those with COPD, we were limited in our ability to interpret the extent of variation in access across studies and jurisdictions included in our present review. Specifically, we saw multiple indicators for access to PR in the included literature, such as referral to PR and PR program attendance or adherence. However, a metric or approach of measuring “PR density” would more adequately account for the availability of PR, and hence, access to PR, and if adopted would aid in generalizability when assessing geographic variation in access.
Study Limitations
The literature included in this rapid review does not address or insufficiently addressed longitudinal or temporal evaluation of variation in care, as well as potential variation in care and access for individuals with COPD within the unique context of the COVID-19 pandemic. Most included studies were conducted in the United States and Europe. Therefore, observed heterogeneity in findings may be attributable, in part, to differences in health care systems and/or patient populations between countries of study, and the generalizability of findings across jurisdictions with may be limited. Due to the rapid nature of this review, limitations in the breadth of literature included (i.e., language, date, country restrictions) may have introduced bias into our present findings. Pooled analysis of included articles was also not completed. Thus, we were unable to quantify the relative impact of different sociodemographic factors on variation in access and outcomes.
Conclusions
Through this rapid review, we identified multiple patterns of potential equity-related variations in health care access and health outcomes for individuals with COPD. Although the present findings may not be generalizable to all patient populations and/or health care settings, it is apparent that variations in both access to care and health care utilization likely exist for patients with COPD, on the basis of multiple determinants, including geography, sex, ethnicity, and SES. To mitigate unwarranted variation and resulting health disparities, these determinants of variation in COPD care and outcomes should be the focus of future research and policy work. Further, this understanding of sociodemographic variation should provide a starting point to evaluate the potential systemic underpinnings of the various health inequities experienced by individuals with COPD, as well as inform more equitable health policies and clinical practices in the care of those with COPD.
Acknowledgements
Author contributions: Design of the study was provided by LJJS. Acquisition and management of data, analysis and interpretation of data, and preparation of the manuscript were conducted by JAS and LJJS. All authors reviewed and approved the manuscript.
We gratefully acknowledge the assistance of Joycelyn Jaca (Alberta Health Services) in designing and executing the literature search.
Declaration of Interests
The authors have no conflicts of interest to disclose.