Running Head: Activation in COPD and Education Session
Funding Support: None.
Date of Acceptance: March 17, 2024 | Published Online Date: March 22, 2024
Abbreviations: ρ=Spearman’s Rho coefficient; BMI=body mass index; BODEx=Body mass index-airflow Obstruction-Dyspnea-Exercise capacity plus exacerbations; CAT=COPD Assessment Test; COPD=chronic obstructive pulmonary disease; COTE=Comprehensive Occupational Therapy Evaluation; FEV1=forced expiratory volume in 1 second; FVC=forced vital capacity; HADS=Hospital Anxiety and Depression Scale; IPAQ=International Physical Activity Questionnaire; IR interquartile range; mMRC=modified Medical Research Council; MSE=mean standard error; PA=physical activity; PAM-13=Patient Activation Measure-13 questionnaire
Citation: Fernández-Sánchez MC, Ruiz-López FJ, Ros-Lucas JA, Andújar-Espinosa R, Del Coso J. García-Pastor T. Persons with chronic obstructive pulmonary disease and high levels of activation improved their physical activity skills after an educational session. Chronic Obstr Pulm Dis. 2024; 11(3): 270-281. doi: http://doi.org/10.15326/jcopdf.2023.0456
Online Supplemental Material: Read Online Supplemental Material (183KB)
Introduction
Daily physical activity (PA) has benefits for chronic obstructive pulmonary disease (COPD) and is considered part of a patient’s self-management routine. However, conducting self-management requires patient education with adequate information and advice. Although it is assumed that improving patient knowledge is an important part of self-management,1 it has been proven2,3 and also assumed by experts,4 that group didactic sessions are insufficient for promoting self-care skills. A critical aspect of self-care is activating patients with the skills, knowledge, and motivation needed to participate as members of their care development team.5 Today, several tools, such as the Patient Activation Measure (PAM)-13 questionnaire, can be used to measure patient activation that are valid, reliable, and offer good psychometric properties that can be used individually.6 The PAM-13 scale measures the level of patients’ engagement in their health care. The patient's activation ranges from believing that their role is important to keeping their healthy behavior under stress. These tools are very useful because activation can condition the results of a patient intervention. Simple, self-administered care interventions can be cost-effective and, when combined with monitoring technologies, can produce changes in patients’ self-management in the short term by measuring daily PA in real-time using a smart device with haptic feedback via actigraphy.7 However, these same studies have highlighted the weak recruitment of patients to PA programs, probably due to their inadequate activation levels. Therefore, we investigated whether the activation of COPD patients, as assessed by the PAM-13 questionnaire, determines their responses, quantified in steps/day by actigraphy, to a group educational activity based on simple interventions in their daily activities.8
Methods
Study Design
A nonrandomized quasi-experimental study, with a pretest/posttest for one group, was conducted at the pneumology service of a hospital. Patient recruitment took place during the months of January, February, March, and October 2019. All study participants received oral and written information about the objectives of the study and the procedures that would be performed. To start the study, a signed informed consent form was required from each participant. This study was previously approved by the Clinical Research Ethics Committee of the Clinical Hospital.
Study Population
The study participants had to meet the following criteria:
- Age of 50–80 years;
- Diagnosed with COPD with forced expiratory volume in 1 second (FEV1) between 30% and 80% of the predicted value according to the Spanish Society of Pneumology and Thoracic Surgery reference values;
- A Body mass index-airflow Obstruction-Dyspnea-Exercise capacity-plus severe exacerbations (BODEx) index of less than 5 points;
- Nonexacerbators (defined as no or one exacerbation per year that did not lead to ahospital admission);
- Owned a mobile phone with the WhatsApp® application;
- Agreed to participate in the study by signing an informed consent form.
The BODEx index was calculated using the score proposed by Celli et al9: body mass index (BMI), dyspnea assessed using the modified Medical Research Council (mMRC) scale, FEV1 and 3 categories generated by exacerbations (0, 1, or 2 points), replacing the walking test (the absence of severe exacerbation was scored as 0, the presence of 1–2 severe episodes received 1 point, and ≥3 severe exacerbations were scored as 2). Therefore, the score range for this index is between 0 and 9 points.10 The occurrence of an exacerbation during the monitoring time would condition the results of the study.
Patients were excluded if they declined to participate in the study, were unable to perform any of the tests, did not speak the language of the country, did not know how to read, or had any of the following: COPD exacerbating phenotype, an uncontrolled heart disease, uncontrolled pulmonary hypertension, an exacerbation in the previous 4 weeks, severe psychiatric illness, cognitive impairment, or concomitance with another severe pulmonary pathology (e.g., severe sleep apnea syndrome, diffuse interstitial lung disease, bronchiectasis). A consecutive nonprobabilistic sampling was carried out in which patients who attended the pneumology service and met all the inclusion criteria (and none of the exclusion criteria) were selected sequentially until the proposed sample size was achieved.
Data Collection
First, each patient underwent a clinical interview during which their clinical data were collected (sex, age, anthropometric data, degree of dyspnea on the mMRC scale, number of exacerbations in the previous year, current smoking habits, and accumulated consumption).
Next, we reviewed their electronic medical records to obtain the necessary data on the clinical phenotype of their COPD and their main comorbidities, which were necessary for the calculation of the BODEx, Charlson Comorbidity Index, and Comprehensive Occupational Therapy Evaluation (COTE) Scale clinical indices. We also obtained the most recent post bronchodilator spirometry.
Procedure
The patients were provided with the COPD Assessment Test (CAT), Hospital Anxiety and Depression Scale (HADS), International Physical Activity Questionnaire (IPAQ), and PAM-13 questionnaires, as well as a GT3x® accelerometer (ActiGraph, LLC, Pensacola, Florida) with a wrist bracelet for use over the next 15 days. They were then given an appointment for a 45-minute educational group session of 6–8 patients on day 8, during which they were educated on nutrition and inhaler use and were provided with PA information related to the “on your feet to earn your seat” principles11 (online data supplement–section 1). At the end of the session, the participants were provided with complete information in writing, (online data supplement−section 2). They were instructed to continue using the accelerometer for the next 7 days. Motivational reinforcement was carried out on days 2 and 6 at 9 am and on day 4 at 9 pm (online supplement–section 3).
Outcomes
The primary outcome was the change in the number of steps/day before and after the intervention, which was extracted from the GT3x accelerometer according to the level of activation by the PAM-13 questionnaire. PAM-13 consists of 13 items on a Likert scale. Each item has 5 response categories with scores from 1 to 5: (1) “Strongly Disagree,” (2) “Disagree,” (3) “Agree,” (4) “Strongly Agree,” and (5) “Not Applicable.” Data were entered into the PAM-13 online score sheet to obtain the activation score (1–100) and activation level (1: disengaged and overwhelmed; 2: becoming aware but still struggling; 3: taking action and gaining control; 4: maintaining behaviors and pushing further) for each patient. Since both Level 1 and Level 2 are less numerous in individuals with COPD,12,13 PAM levels were dichotomized, as in other studies, into “low activation” (PAM Levels 1 and 2), and “high activation” (PAM Levels 3 and 4).
The secondary outcomes, which complemented the activity extracted from the accelerometer, were as follows: the percentages of moderate activity and inactivity (seated and lying), and other as the percentages of light activity and standing time. Other secondary outcomes were the BODEx index, Charlson score, COTE score, anxiety and depression score, FEV1 (ml and percentage of the predicted value), age (years), weight (kg), and BMI (kg/m2) according to the activation level measured by the PAM-13 questionnaire.
Sample Size
The initially estimated population to be recruited was calculated to produce a proportional increase of 43% in steps per day compared with a previous study.8 The 51% estimate of losses according to the same study was probably conditioned with activation for 0.05 of alpha risk and 0.10 of beta risk. For the current study, we needed a minimum sample of 23 patients, as this was a unilateral test. To obtain a mean difference of at least 1548 steps/day between dichotomized PAM-13 levels, with an effect size of 0.72 according to a previous study,14 and an alpha risk of 0.05 and a beta risk of 0.20, a minimum of 25 patients per group as sample size would be required in a one-tailed test.
However, as we were obliged by Insignia Health® (Portland, Oregon) to conduct the PAM-13 questionnaire with 75 patients, which was the minimum number to obtain the research license, the latter sample size was used.
Statistical Analysis
The level of significance used throughout the study was p<0.05. Data analysis was conducted using the statistical application SPSS, Version 22 (IBM, Armonk, New York).
Previously, the normality of the variables was verified with the Kolmogorov-Smirnov test and the application assumptions of this test were used in our analysis. If the variables had been distributed according to the normal distribution, the paired Student’s t-test would be used to analyze the difference between means before and after the group session. Subsequently, the Student’s t-test would be used to analyze the difference between the change before and after the group session by pooled PAM levels. If the variables had not been distributed according to the normal distribution, the Mann-Whitney U test would be used to analyze the difference between the change before and after the group session by pooled PAM levels.
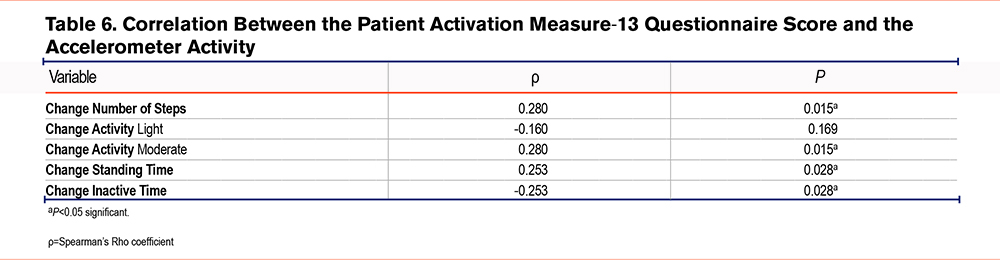
Spearman’s Rho coefficient was applied to study correlation between number of steps, activity change, and the PAM-13 questionnaire score, because this variable was not normally distributed.
Quantitative variables were described by mean±mean standard error or median and interquartile range (median ; IR) if they were not distributed normally. The descriptive variables of the sample were expressed qualitatively as frequencies and percentages. These variables included gender, smoking habit, hypertension, dyslipidemia, diabetes, obstructive sleep apnea-hypopnea syndrome, COPD phenotype, anxiety and depression dimensions, and the description of the level of PA.
Results
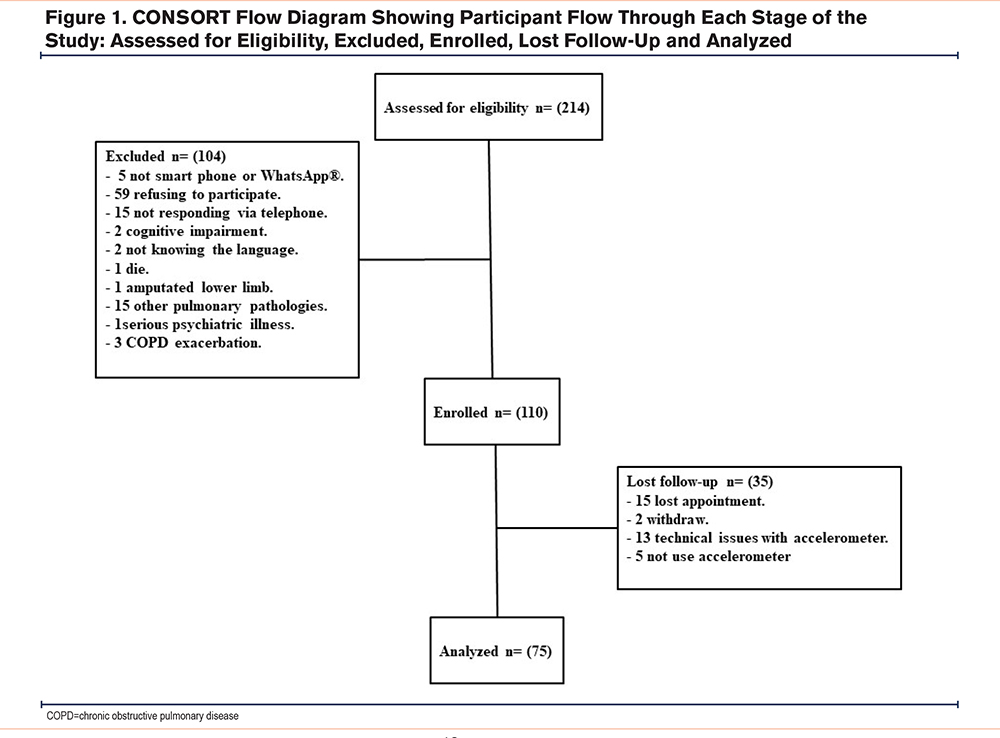
A total of 214 patients with COPD were selected. Of these, 104 were excluded (5 for not having a smartphone or not being familiar with the WhatsApp® mobile application, 59 for refusing to participate, 15 for not responding via telephone, 2 for cognitive impairment, 2 for not knowing the language, 1 due to death, 1due to an amputated lower limb, 15 for concomitance with other pulmonary pathologies, 1 for suffering a serious psychiatric illness, and 3 due to a COPD exacerbation). Of the 110 patients included in the study, 15 missed their appointment. Of those who started the study, 2 withdrew; 13 experienced technical problems related to the recording by the accelerometer, making it impossible to obtain the complete record; and 5 did not sufficiently use the accelerometer. Finally, 75 patients completed the study (Figure 1).
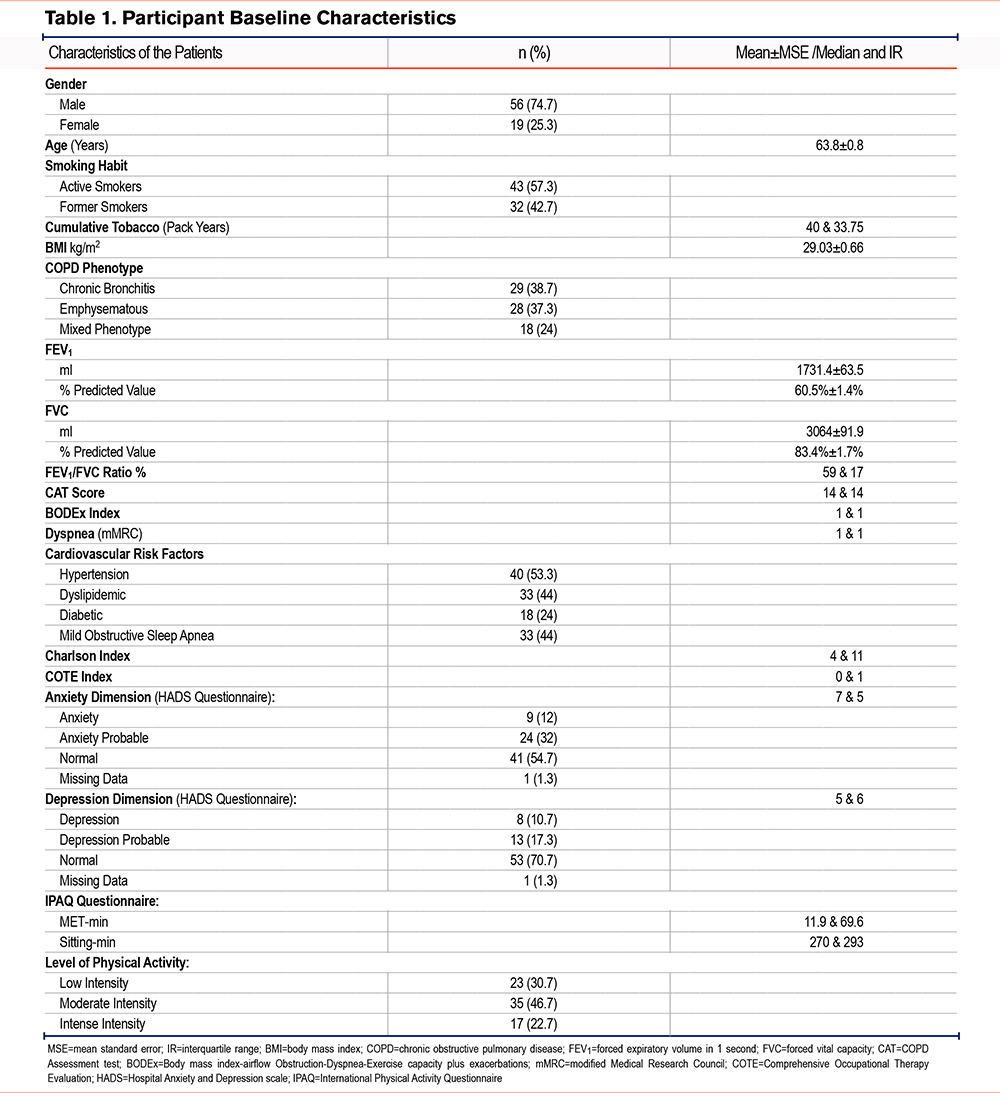
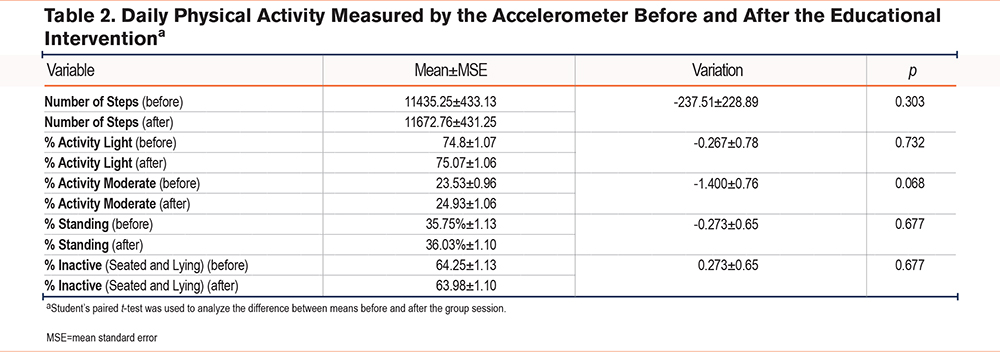
The descriptive characteristics of the patients included in the study are shown in Table 1. When globally measured, daily PA was analyzed using an accelerometer, and no significant differences were observed before and after the intervention for the number of steps and the rest of the variables (Table 2).
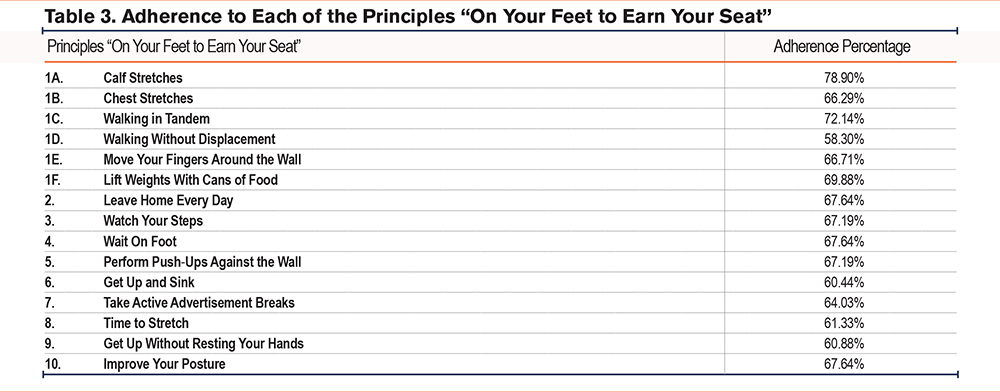
However, the median compliance with the PA program, as reported by the patients through their daily completion of the exercise chart, was 81.91% ± 44.76% (Table 3).
The median score on the PAM-13 questionnaire was 60.6; 14.6 (median IR) points. The level obtained in the PAM-13 questionnaire is shown as a percentage in Figure 2. As can be seen, 5 participants were placed in Level 1, 21 were placed in Level 2, 34 were placed in Level 3 (the most numerous), and 15 were in Level 4.
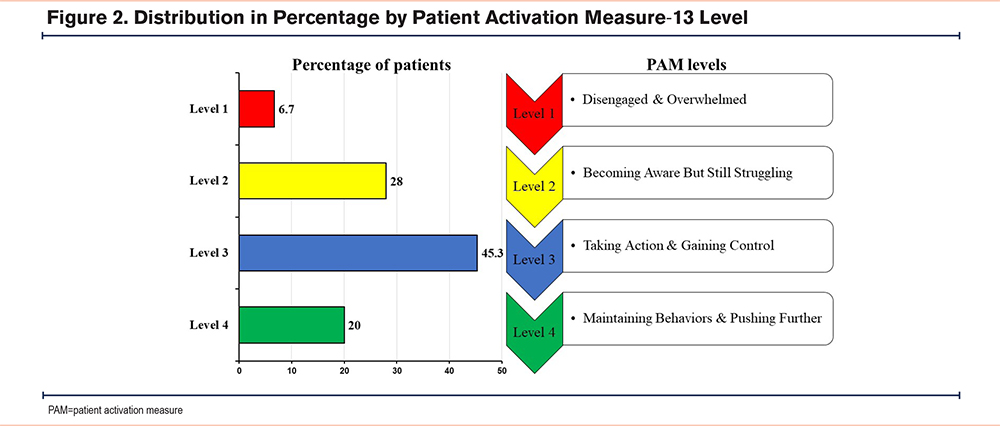
As there were only 5 participants in activation Level 1, we regrouped the 4 levels into 2: the 2 lowest activation levels (1 and 2) and the 2 highest activation levels (3 and 4).
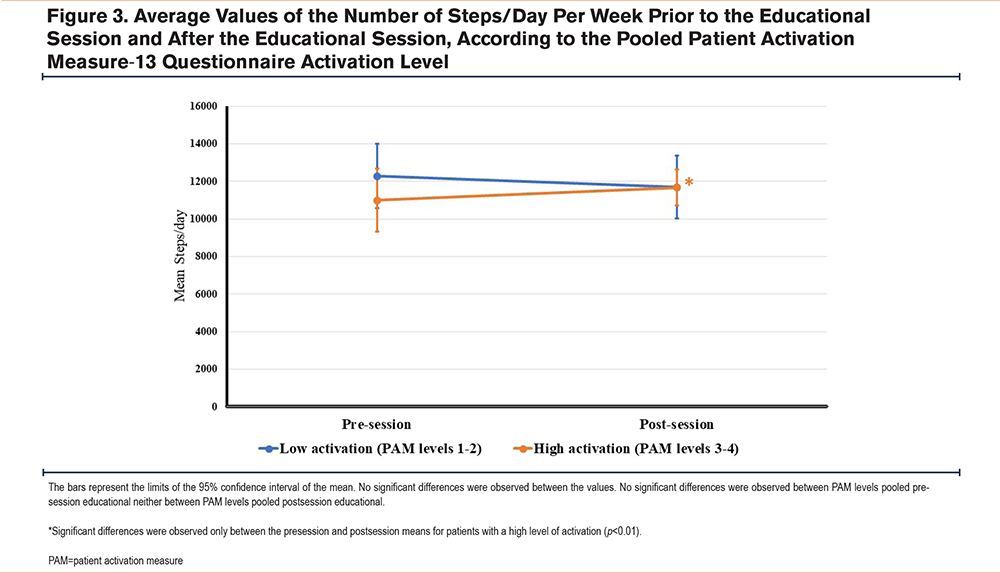
There were no significant differences in the mean number of steps per day between low- and high-activation patients during the week prior to the educational session (Figure 3). Significant differences were only observed between the pre-session and post-session means for patients with a high level of activation (Figure 3, Table 4).
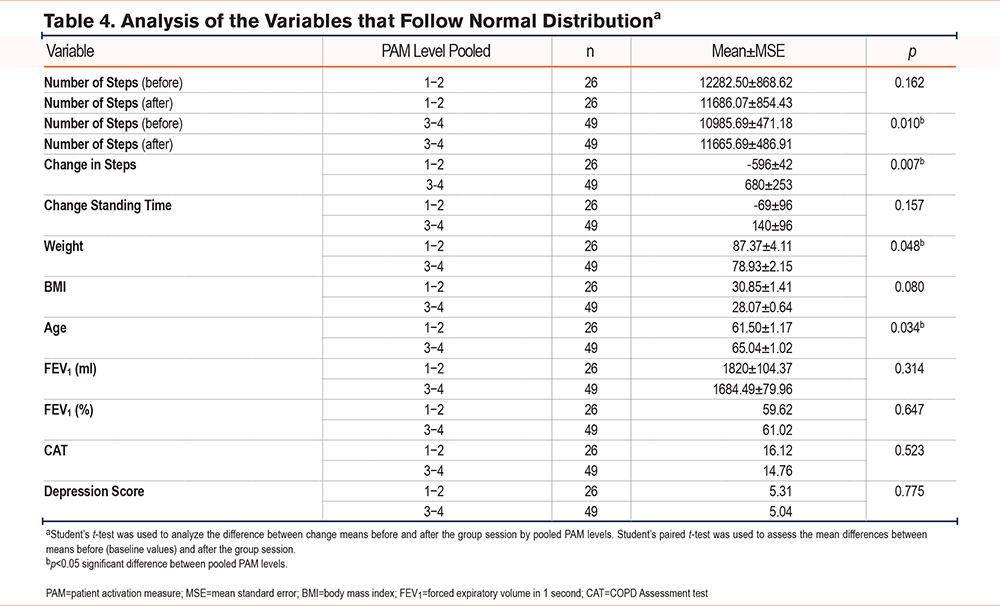
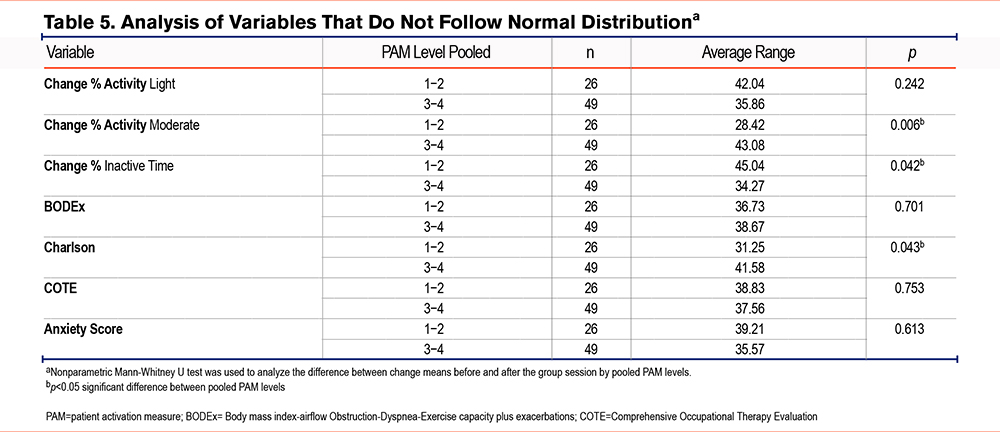
The variations among the different variables collected in the study (accelerometer data, age, anthropometric data, the CAT and HADS questionnaire, and clinical indices) were analyzed with the pooled results of the PAM-13 questionnaire (Tables 4 and Table 5).
The group with the highest activation level (Group 3–4) demonstrated an increase in the number of steps per day after the educational session. However, the group with low activation (Group 1–2) decreased the number of steps.
The group with the highest activation level (Group 3–4) demonstrated an increase in the time dedicated to activities of moderate intensity after the intervention. Both age and the Charlson index were also higher in this group. In the group with less activation (Group 1–2), the time they remained inactive was greater, as was the individual weights of the participants.
The correlation between the PAM-13 scores and accelerometer activity was also analyzed. The findings showed a correlation between the change of steps and moderate activity and standing time, as well as an inverse correlation with inactive time (Table 6).
Discussion
One of the problems with the failure of rehabilitation programs to increase activity is the resistance of patients to enter the programs or the ease of withdrawing from them. The reasons for these situations are futile, and in many cases, there is no reasonable reason from patients for their withdrawal. Identifying these vulnerable patients will help us in the outcome of the programs.15,16
The PAM-13 scale measures the level of empowerment and self-management of patients with chronic diseases, such as COPD.17 The current study was designed to determine whether the score on the scale predetermines the patient’s response to an educational session.
The patients who did not enter the follow-up did not differ from those who later enrolled in the study, except for 16 patients, with 15 of them having myocardial dysfunction that could interfere in the results of the study and one with a severe psychiatric alteration that interfered with the follow-up, 15.38% of those rejected and 7.4% of the total.
Overall, the educational intervention did not lead to an increase in the number of steps or activities, as indicated in the literature.6 However, when the patients were subdivided by their degree of activation prior to the educational intervention, as measured by the PAM-13 scale, it became evident that the patients with the highest activation were the most positively influenced by the educational intervention. The intervention increased their number of daily steps (there was more than a 1000-step difference between the high- and low-activation groups) and the time they dedicated to activities of moderate intensity. In addition, they decreased their inactive time.
This confirms that the PAM-13 questionnaire, as its own authors pointed out, is useful for designing interventions in a clinical setting and such interventions on activated patients should be designed to increase their knowledge, skills, and confidence in self-management.6 A curious fact that reinforces the strength of this questionnaire to predict a positive response to a simple educational intervention was that, unlike other studies in which the presence of comorbidities or age negatively influenced activation,18 we observed that the more activated patients and, therefore, those with better responses after the intervention, had more comorbidities or were older. Similarly, our study did not observe that the severity of the obstruction before an educational intervention influenced the results.18 In addition, that greater activation determined greater daily activity after educational intervention was not found to be conditioned by the impact of COPD on health or quality of life. In contrast, prior studies have suggested that activation is conditioned by the impact on health, as determined by the CAT.12
The HADS questionnaire was used because it is known that more sedentary or older patients with COPD have higher levels of anxiety and depression.19,20 However, in our study, we found no differences in mood according to the level of activation, and it did not influence the response to exercise.
The literature further shows that low levels on the PAM-13 (Levels 1 and 2) questionnaire are associated with a poor state of health, greater dyspnea, and a lower BMI.13 However, in our study, there was no difference in BMI between activated and nonactivated patients.
Our study also objectively demonstrated concordance between the PAM-13 questionnaire and the reality of self-management in the promotion of PA in daily life. This finding is in contrast to the conclusions of other authors, who question this objective concordance in patients with chronic respiratory diseases, such as cystic fibrosis.21 These authors argued that patients answered the PAM-13 questionnaire, so they should have done more than what they actually did—an argument they confirmed when they objectively determined adherence to inhalers.21 However, when we objectively verified patient activity using actigraphy, we detected differences. This result is consistent with the finding of a cross-sectional study on a population in which a quarter of the participants were COPD patients: the greater the activation detected by the PAM-13, the stricter the adherence to prescribed medication.22
Another striking fact is that patients with low activation decreased their amount of steps/day after the educational intervention. We do not believe that education has a deleterious effect on patients. Our explanation is that the patients who agreed to join the study, who were given a description of the study and provided with an actigraph to monitor their usual daily activities prior to the session, most likely suffered from a Hawthorne23 effect, which increased their activity. However, the educational session may have been unable to meet their expectations, so they returned to their usual activities. In fact, patients with low PAM-13 scores are often dissatisfied with the proposals offered by doctors to manage their disease13 and feel little support from them.24 The paradox is that this effect could be used experimentally in patients with low activation, with a rehabilitation program managed within the usual clinical care of these patients. This could be achieved without generating great expectations beyond interactive telemonitoring that increases their activity.25
In our study, the patients demonstrated a high degree of activation, thus implying a high degree of individual competence regarding the assumption of new behaviors and efforts to manage their health.26 Such high activation would be conditioned by the predisposition to participate in the study, as it was conducted outside the usual visits.
In addition, the procedure used to inform and recruit participants, a telephone call with a pneumologist, has had an influence on communicating a warmer welcome and creating a more favorable environment for the integration of the team in patient care than did prior studies that conducted recruitment by mail.18,27 This level of activation, higher than that recorded in other studies, was probably also influenced by our exclusion of patients with exacerbations. Prior studies that included these patients reported a higher degree of comorbidity, as reflected in the Charlson index, and a greater impact on quality of life, as reflected by a higher score on the CAT questionnaire.28
In fact, in COPD, it has been observed that activation Levels 1 and 2 are associated with a poorer state of health and a greater number of exacerbations, as determined by the number of visits to the doctor.13 Other studies have presented higher levels of activation because younger patients with less comorbidity participated in such studies, thus ensuring a higher level of participant activation.13 Finally, the degree of activation in our study was also influenced by the fact that all our patients knew how to read: one study found a link between low literacy, lower level of activation, and inadequate self-management.29
Furthermore, adherence to the exercise program proposed after the educational intervention was superior to that in the pilot study, in which the “on your feet to earn your seat” principles11 were introduced: in its intention-to-treat analysis, an average adherence of 52.99% was observed for each of the exercises during the second week of the program.
As some authors have pointed out, given the great variation in the effectiveness of COPD interventions, it is unlikely that any single intervention can be adapted for all patients.30,31 Similarly, health professionals cannot apply just one approach.32 Therefore, using PAM-13 to identify COPD patients who are activated by an educational group is a cost-effective strategy for implementing effective and targeted interventions. On the other hand, the PAM-13 questionnaire identifies low-activation COPD patients who would not benefit from this simplified intervention. They would need to acquire knowledge jointly with a cognitive behavioral therapy program that includes psychological coping for a sustainable behavior.33
Limitations
This study has limitations in terms of duration of effect because the evaluation was conducted in the short term. Higher self-completed adherence outcomes of up to 64% have been observed in COPD patients after 8 weeks of intervention, but those studies had 6-month monitoring periods.34 Thus, it would be worthwhile to evaluate this situation in the longer term. Accepting this situation, the difference in activity, at least in the number of steps, because of a group session provides a hopeful answer. Nevertheless, long-term monitoring studies are needed to determine the duration of the session effect.
Further limitations were that the study was carried out at a single collection site, which excluded people without a level of medical literacy to understand the proposed tests or who did not use a smartphone.
Other limitations were that the observed effect may also be conditioned by a regression to the mean that we could estimate at 14%. A study designed with randomization of 2 groups, 1 with no intervention and 1 with intervention, according to the level of activation, would provide an estimate of the regression effect to the mean in the variation of steps through the control group and provide more definitive conclusions.
Conclusion
COPD patients with levels greater than or equal to 3 in the PAM-13 questionnaire are likely to improve their physical activities after attending an educational group session.
Acknowledgments
Author contributions: MCFS was responsible for data curation, formal analysis, and investigation. FJRL was responsible for conceptualization, project administration, and supervision. JARL was responsible for the investigation, methodology, and resources. RAE provided formal analysis and wrote the original draft of the manuscript. JDC and TGP were responsible for methodology and resources. All authors critically reviewed the manuscript and approved the final version for publication.
Data sharing statement: Data from this study are available in Excel format if requested.
Declaration of Interest
The authors have no conflicts of interest to declare.