Running Head: COPD in LGBTQ+ Individuals
Funding Support: None
Date of Acceptance: March 19, 2024 | Publication Online Date: April 1, 2024
Abbreviations: BRFSS=Behavioral Risk Factor Surveillance System; COPD =chronic obstructive pulmonary disease; ICD=International Classification of Diseases; LGBTQ+=lesbian, gay, bisexual, transgender, queer, and others; LMIC=low- and middle-income countries; NHIS=National Health Interview Survey; SGM=sexual and gender minority; VA=Veterans Affairs
Citation: Maniar NT, Drummond MB. From invisibility to inclusion: a call to action to address COPD disparities in the lesbian, gay, bisexual, transgender, and queer+ community. Chronic Obstr Pulm Dis. 2024; 11(3): 326-330. doi: http://doi.org/10.15326/jcopdf.2024.0496
Introduction
Chronic obstructive pulmonary disease (COPD) is a heterogeneous lung condition characterized by chronic respiratory symptoms (dyspnea, cough, sputum production) due to abnormalities of the airways (bronchitis, bronchiolitis) and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction.1 COPD accounts for most of the deaths from chronic lower respiratory diseases, currently the sixth leading cause of death in the United States2 in 2021. Tobacco use and inhaled environmental exposures have been implicated in the pathogenesis of COPD.1 The outcomes and health burden of COPD have been shown to be different in different demographic groups.3,4
The term “LGBTQ+” refers, in this perspective, to people who are lesbian, gay, bisexual, transgender, or queer with the plus sign indicating inclusion of people who are questioning, intersex, asexual, or who hold other gender/sex/romantic identities not specifically identified.5 The LGBTQ+ community reflects a population with unique risk factors for an increased COPD risk. The rate of cigarette smoking has been shown to be higher in lesbian, gay, and bisexual adults compared to their heterosexual counterparts6 and higher in transgender compared to cisgender adults.7 LGBTQ+ people have also been targeted by advertising and marketing from commercial tobacco companies.8 An increased exposure to stress of any kind, including discrimination has been shown to predispose people to substance use of all kinds, including tobacco exposure.9,10 LGBTQ+ people experience marginalization, discrimination, and harassment often as a result of national and regional polices leading to decreased access to preventative care.11,12 Given these observations, it stands to reason that there is an increased risk of developing COPD in LGBTQ+ individuals. Despite this intersection of risk factors, the prevalence of COPD in LGBTQ+ individuals remains poorly characterized.
The Existing Literature on COPD in Lesbian, Gay, Bisexual, Transgender, and Queer+ Individuals
We conducted a focused review of the existing literature to inform this perspective. We searched PubMed using “COPD” and terms related to LGBTQ+ —gay, lesbian, transgender, queer—and separately “COPD” and "sexual and gender minorities" [medical subject headings] from 1966 to 2023. With this search strategy, we identified 7 relevant studies that reported COPD prevalence in subgroups of the LGBTQ+ population in comparison with the straight (heterosexual, cisgender, non-LGBTQ+) population. We found one additional study referenced in an article on tobacco cessation that was not discovered in the initial search.
We found 2 large studies that examined responses from the Behavioral Risk Factor Surveillance System (BRFSS), a national telephone survey that collects information on demographics and health, including underlying conditions and health-related behavioral risk factors. The first study, by Heslin and Hall,13 included BRFSS participants from 2017−2019, and focused on disparities in chronic health conditions that predispose to adverse outcomes from a COVID-19 infection. The study included 24,582 sexual minority individuals and 619,347 heterosexual individuals. Sexual minority individuals had a 10.3% prevalence of self-reported COPD compared to a 6.9% prevalence among heterosexual individuals, with an adjusted prevalence ratio of 1.49 (1.37–1.61). In the second study, Pinnamaneni et al14 examined BRFSS data from 2014–2020, and included 64,696 adults who identified as gay, lesbian, bisexual, other, and/or transgender and 1,369,681 adults who identified as cisgender and straight. They found that sexual and gender minority (SGM) adults had a 30% greater odds of being told that they had COPD or chronic bronchitis than non-SGM adults. Although the reasons behind these correlations were unclear, the authors suggested that poorer access to preventative care resulting from larger societal discrimination against SGM individuals may have been responsible for an increased prevalence of chronic medical conditions in this population. A smaller BRFSS-based study on tobacco use in the Puerto Rican lesbian, gay, bisexual, transgender, and transsexual population also showed that smokers in this group had higher odds of having COPD than the general population (OR: 4.81, p=0.014).15
Two studies examined data from the National Health Interview Survey (NHIS). The first one, by Ward et al,16 included a total of 34,557 adults, of which 571 identified as gay/lesbian and 233 identified as bisexual. Bisexual adults had a 12.7% prevalence of self-reported COPD, more than twice as high as that in gay/lesbian adults (4.6%) or straight adults (5.7%). The second study by Hutchcraft et al17 of lesbian and bisexual women survivors of cancer, included 141 lesbian, 95 bisexual, and 10,830 heterosexual women. The authors showed that lesbian women reported higher odds of COPD than heterosexual women (OR: 1.98, 95% CI 1.09–3.56). The main limitation of studies from the BRFSS and NHIS is that COPD is based on self-report and may not reflect a confirmed diagnosis.
The study with the largest sample size in our analysis comes from the U.S. Veterans Health Administration (VA) and includes 108,401 adults with minoritized sexual orientation and 6,511,698 with nonminoritized sexual orientations.18 Lynch et al extracted data from the VA corporate data warehouse, a national repository of VA electronic health records, and identified individuals with minoritized sexual orientation using natural language processing of clinical notes. They identified health outcomes such as COPD using the International Classification of Diseases (ICD), 9th and 10th revision codes. Minoritized veterans had a higher prevalence of COPD compared to nonminoritized veterans (36.3% and 22.7%, respectively), with an adjusted prevalence ratio of 1.24 [1.23–1.26]. The authors found a higher overall prevalence of COPD, likely attributable to a higher mean age (~54 years) and higher incidence of tobacco smoking in this population of veterans. While this study used ICD-9 codes rather than self-report to infer COPD diagnosis, the classification of minoritized sexual orientation was not based strictly on self-report but rather on machine learning-based review of provider documentation, which is susceptible to its own bias. Another study by Dragon et al19 retrospectively analyzed Medicare claims data using ICD-9 codes, and included 7454 transgender adults with a mean age of 53.1 years and 39,136,229 cisgender adults with a mean age of 70.9. Transgender Medicare beneficiaries had a higher observed percentage of COPD (27%) compared to cisgender Medicare beneficiaries (20.8%).
Abramovich et al in a population-based study of electronic health records in Ontario, Canada, identified transgender individuals (n=2085) from outpatient health centers within the province and matched them 1:5 on age to a random 5% sample of the general Ontario population meant to include cisgender individuals (n=10,425).20 In this study cohort, the mean age was ~30 years. The authors found that transgender individuals were more likely than cisgender individuals to experience COPD (2.4% versus 1.5%; p < 0.001). Interestingly, they reported an overall lower prevalence than previously described studies, which may be explained by differences in study design or age of individuals analyzed.
The data summarized in this focused review consistently show an increased prevalence of COPD in LGBTQ+ people. Importantly, all studies were from the United States and Canada, with none representing individuals from low- and middle-income countries (LMIC). While the increased prevalence among LGBTQ+ populations can be explained in part by an increased rate of smoking as a result of social-environmental stressors and targeted marketing by commercial tobacco companies,8 the literature is lacking assessments of other risk factors unique to LGBTQ+ people. Despite heterogeneous study designs, methods of COPD diagnosis ascertainment, and different subgroups of the LGBTQ+ population studied, the net effect of increased prevalence of COPD was well demonstrated across different age groups.
A Call to Action to Improve the Health of Lesbian, Gay, Bisexual, Transgender, and Queer+ Individuals with COPD
Given the available evidence identifying the LGBTQ+ community as particularly susceptible to COPD risk, we propose a call to action to address the burden of COPD in the LGBTQ+ community (Figure 1). This call to action is informed by the structure of the COPD National Action Plan21 proposed by the National Institutes of Health in 2019. The call to action is 3-pronged: to improve education about COPD, develop interventions to improve prevention and treatment of COPD, and implement research to better characterize the burden of COPD in the LGBTQ+ community.
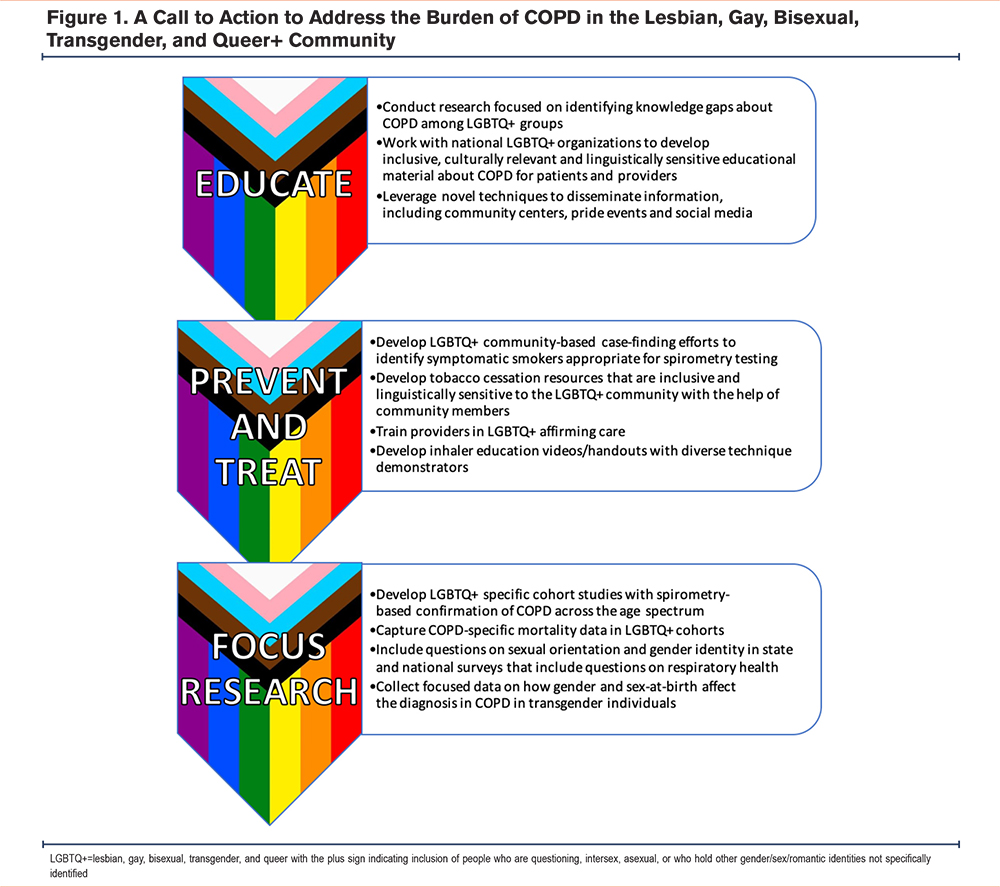
The first prong of our call to action is to increase awareness and education about COPD in the LGBTQ+ community. This should start with research focused on identifying the gaps in the existing knowledge in the community and include education on the role of tobacco smoking, both combustible cigarettes and electronic cigarettes. National organizations on respiratory and LGBTQ+ health should collaborate to develop educational materials on COPD for both patients and providers. Such material should be culturally relevant and linguistically sensitive. We must seek out novel ways to disseminate this information to at-risk communities, such as leveraging social media and distribution at community centers and pride events.
The second prong of our call to action is to improve preventative, diagnostic, and therapeutic efforts in this population. LGBTQ+ smokers, like their heterosexual, cisgender counterparts have reported “going cold turkey” as the most common tobacco cessation strategy though evidence-based tobacco cessation programs have been shown to be as successful in LGBTQ+ people as in straight people.22 Even today, LGBTQ+ people face discrimination in health care environments and as such, sensitive and inclusive tobacco cessation efforts are the most pressing need.8 Providers who treat LGBTQ+ patients for COPD and those who see these patients in preventative settings must be trained and competent in LGBTQ+ affirming care. Data exist demonstrating that LGBTQ+ specific interventions are successful at achieving tobacco cessation.23 Some examples of inclusive LGBTQ+ interventions are the involvement of community leaders in developing interventions and using local LGBTQ+ centers to disseminate information on smoking cessation resources.24 In terms of treatment of established COPD patients, both printed and video educational material should include representation from the LGBTQ+ community, for example by using diverse technique demonstrators in inhaler education videos.
The third prong in our call to action is to implement research to better characterize the scale of the problem of COPD among LGBTQ+ communities. Our review of the limited literature on this subject shows that COPD has a higher prevalence in LGBTQ+ people. However, the studies examine a variety of different cohorts and comparators. We must develop longitudinal LGBTQ+ specific cohort studies with spirometry-based confirmation of COPD across the age spectrum, which include standardized, culturally sensitive assessments of self-reported sexual identity. These cohorts should include a diverse group of individuals with representation from different racial and socioeconomic backgrounds and include LMICs. COPD as a cause of mortality must also be examined in these cohorts. At a national and state level, surveys that include questions on respiratory health must collect data on sexual orientation and gender identity. We also need to collect focused data on how sex-at-birth and gender affect the diagnosis of COPD in transgender individuals.
In conclusion, COPD is under-studied in the LGBTQ+ community despite a higher reported prevalence. We need to improve the awareness of COPD as a risk of tobacco smoking in the LGBTQ+ community and leverage unique methods to disseminate this information effectively. Tobacco cessation is a cornerstone of both the prevention and treatment of COPD, and thus, we need to prioritize the development of inclusive and culturally sensitive smoking cessation resources. Providers who work with patients with COPD need to receive training in LGBTQ+ affirming care. These efforts will require coordinated action at the local and national level to improve funding and create policies that will protect the LGBTQ+ community from increased exposure to commercial tobacco. The understanding of increased prevalence in this population is still at its infancy and needs to be better defined with well-designed cohort studies. On a broader scale, we must aim to improve access to all aspects of preventative care for the LGBTQ+ community and ensure that such care is provided in an evidence-based and culturally sensitive manner.
Acknowledgements
Author contributions: Both NTM and MBD contributed to the concept, design, analysis, and creation of the manuscript.
Declaration of Interests
The authors have no conflicts of interest to declare.