Running Head: Wildfire Readiness in Airway Disease Patients
Funding Support: This manuscript was sponsored by Takeda Pharmaceuticals USA, Inc., Cambridge, Massachusetts. Under the direction of the authors, medical writing services were provided by Jacqueline Register, MSc, and Samantha Wronski Holloway, MS, of Oxford PharmaGenesis Inc., Newtown, Pennsylvania, and were funded by Takeda Pharmaceuticals USA, Inc., Cambridge, Massachusetts. The content of this manuscript, the ultimate interpretation of data or results, and the decision to submit it for publication in Chronic Obstructive Pulmonary Diseases: Journal of the COPD Foundation were independently under the control of the authors.
Date of Acceptance: May 20, 2024 | Publication Online Date: June 5, 2024
Abbreviations: AATD=alpha-1 antitrypsin deficiency; COPD=chronic obstructive pulmonary disease; DIY=do-it-yourself; HHS=U.S. Health and Human Services; HPI=Healthy Places Index; NLP=natural language processing; OCCHE=Office of Climate Change and Health Equity; PM2.5=particles 2.5 micrometers or fewer in diameter; PM10=particles with diameters less than 10 micrometers; PPM=parts per million; UCDH=University of California Davis Health
Citation: Kuhn BT, Gupta R. Improving wildfire readiness among patients with chronic obstructive pulmonary disease and asthma: applying a population health approach to climate change. Chronic Obstr Pulm Dis. 2024; 11(4): 427-435. doi: http://doi.org/10.15326/jcopdf.2024.0509
Air Pollution Impacts Health Outcomes
The Camp Fire of 2018 wiped out the city of Paradise overnight, devastating communities throughout Northern California.1 Other large fires, including the Carr, Dixie, and Caldor fires, left much of the state mired in dense smoke with dangerous air quality for weeks.2 Due to climate change, fire season in California now lasts up to 6 months of the year and has become increasingly regular and severe.3 These fires, and specifically the resulting wildfire smoke, have harmful health effects, especially among the most clinically at-risk and underserved patients (measured by both clinical conditions and medical access, location, economic situation, and social support) and patients with preexisting lung and airway diseases.1,4,5
Multiple components of wildfire smoke can have adverse impacts on health.6 Wildfire smoke is comprised of thousands of individual components, including particulate matter, carbon dioxide, water vapor, carbon monoxide, hydrocarbons, nitrogen oxides, and trace minerals. Particulate matter can irritate the eyes and the respiratory tract, leading to cough, phlegm, wheezing, and difficulty breathing, and exacerbating preexisting health conditions. Particulate matter is categorized by size—particles with diameters less than 10 micrometers (PM10) can be inhaled and impact the lungs and circulatory system, and particles less than 2.5 micrometers in diameter (PM2.5) are especially damaging because they can travel deep into the lungs and potentially enter the bloodstream. Carbon monoxide dissipates rapidly but is a concern for individuals with preexisting cardiovascular conditions, individuals within 3 miles of the fire line, and firefighters. Ozone, while not emitted directly from fires, can develop as smoke moves, and can lead to reductions in lung function, airway inflammation, and other symptoms.6 While comparison of wildfire smoke with air pollution from other sources is challenging because of inconsistent exposure, a study assessed cardiopulmonary hospitalization rates in a population of older adults and determined that hospitalizations associated with an increase of 10 µg/m3 in PM2.5 were similar between wildfire smoke and nonwildfire smoke exposures.7
Wildfire smoke represents a specific detriment to the health of patients in rural Northern California, who experience impaired access to an overstretched health region.1 As the regional academic center, University of California, Davis Health (UCDH) has adopted a targeted approach, leveraging new technologies and population health methods to overcome the challenges of climate change. In the United States, wildfire frequency, severity, and duration are increasing and affecting clinically at-risk and underserved communities.8,9 Exposure to wildfire-related air pollutants escalates all-cause mortality and respiratory morbidity in the general population and leads to more severe health outcomes among populations with preexisting respiratory diseases.8,10,11 In exposed communities, the development of chronic pulmonary diseases, such as emphysema, can be exacerbated by inflammation, oxidative stress, and insufficient clearance of pollutant fine particles from the lungs.12 For patients being treated for preexisting asthma or chronic obstructive pulmonary disease (COPD), physician visits, emergency department visits, hospitalizations, and exacerbations of symptoms increase in the setting of wildfire smoke exposure.8,10,13,14
Poor air quality induces inflammation in the lungs, especially affecting those with preexisting lung diseases such as asthma and COPD.15,16 The Environmental Protection Agency has lower thresholds of acceptable air quality for “sensitive” populations, but their definition of sensitive only applies to patients with diagnosed diseases, including lung diseases like asthma.17 Over 40% of patients in the COPD Genetic Epidemiology study with a smoking history had no obstruction on spirometry (therefore, not meeting most criteria for a label of COPD), but were in fact found to have emphysema and bronchitis on imaging.18 Hence, while not a sensitive population, this group with pre-COPD is at an increased risk of progression toward COPD in the setting of poor air quality, and is included in wildfire/poor air quality-targeted interventions at UCDH. Higher concentrations of small particulate matter (PM2.5) and nitrogen dioxide are associated with a lower forced expiratory volume in 1 second to forced vital capacity ratio, with a stronger association seen in those with low incomes.19
Similarly, those with alpha-1 antitrypsin deficiency (AATD) are likely at higher risk of lung damage after exposure to wildfire smoke.20,21 Alpha-1 antitrypsin is a protease inhibitor that maintains lung tissue architecture by counterbalancing neutrophilic inflammation, which is important during acute insults such as wildfire smoke inhalation.22 Protection against pollution-related inflammation is compromised in patients with AATD, resulting in intensified symptoms including coughing, wheezing, dyspnea, and respiratory infections.20,21,23 The implications of acute versus chronic exposure to air pollution in patients with AATD are not well understood; however, a study of lung function over time in patients with AATD found that high ozone and PM10 exposure were significant predictors of lung function decline.21 Both of these factors are components of wildfire smoke and could potentially have adverse impacts on patients with AATD, even with acute exposure. While clearly a sensitive population, an estimated 90% of individuals with AATD in the United States are undiagnosed, resulting in thousands of people unaware of this underlying health risk when exposed to wildfire smoke pollutants.24
Structural Factors Preventing Optimal Care in Wildfire-Impacted Communities
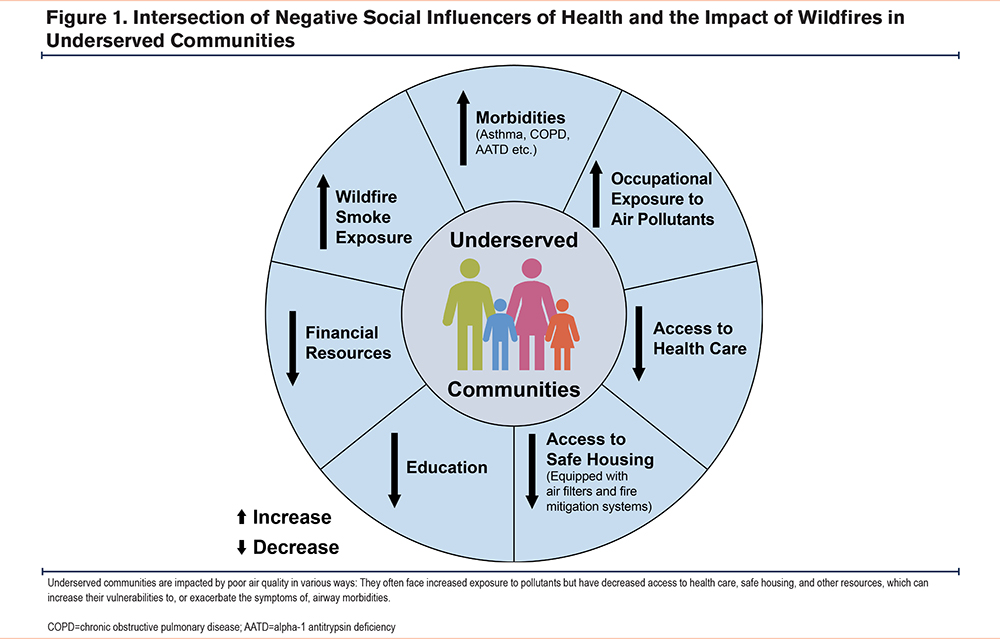
Communities vulnerable to wildfires and wildfire smoke are often from underserved areas that face negative social influencers of health (Figure 1). Low socioeconomic status and increased prevalence of concurrent conditions, including chronic respiratory diseases, make it difficult to isolate the distinct effect that poor air quality has on the health of exposed populations.4,25,26 Inadequate access to health care in these communities further impedes clinicians’ visibility into the problem.1 Moreover, the implementation of wildfire preparedness safety measures, such as home air filters and tree trimming, requires financial resources that underserved communities often lack.4
Measuring the Impact of Wildfire Smoke in Clinically At-Risk and Underserved Communities
Although it is known that wildfire smoke negatively impacts the health of exposed populations and that underserved communities are disproportionately affected, the true extent of this impact is not well characterized.10,27,28 This poor understanding is partially due to the challenges of measuring wildfire exposure and associated outcomes.21 Wildfire smoke exposure results in symptoms including coughing, wheezing, throat and eye irritation, drowsiness, and shortness of breath or bronchitis, which overlap with common respiratory illnesses, including asthma, allergies, or viral infections.12,21 During a wildfire, individuals may increase their use of medication, which may mask symptoms.12 Lack of air pollution-monitoring networks in rural areas susceptible to wildfires further prevents the ability to measure the impact of wildfire smoke on population health.8,21,29,30 Thus, we feel that there is a need for improved surveillance and improved measurements of exposure to wildfire smoke-related health outcomes.
With an expanding wildfire season in the United States, health systems need to identify populations at high risk for adverse health outcomes and implement interventions to mitigate the consequences of poor air quality.9 The aim of this manuscript is to share an action plan with health system leaders and care teams to achieve preparedness in underserved communities to deal with the impacts of wildfires and wildfire smoke.
UCDH Experience in Serving Vulnerable Communities Most Impacted by Wildfires
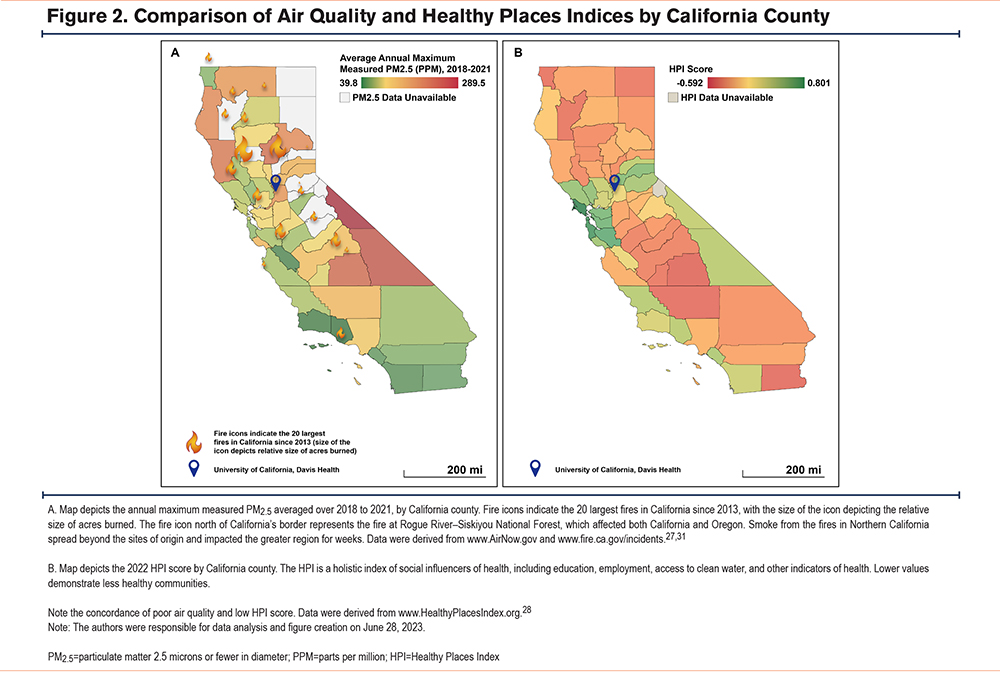
As shown in Figure 2A, between 2018 and 2021, many California counties experienced large fires and dangerous air quality, as measured by annual maximum PM2.5 levels, especially in the Central Valley and Northern California.27,31 The counties with the most days of poor air quality correlate with areas of the lowest health measured by the Healthy Places Index (Figure 2B).28 UCDH is at the epicenter of these wildfires and cares for many patients in the most affected counties. Our clinicians routinely care for patients with physical, financial, and occupational barriers to clean air, so we are uniquely equipped to share experiences serving communities impacted by wildfires. In the next sections, we propose strategies to support vulnerable and high-risk patients.
Wildfire Population Health Approach
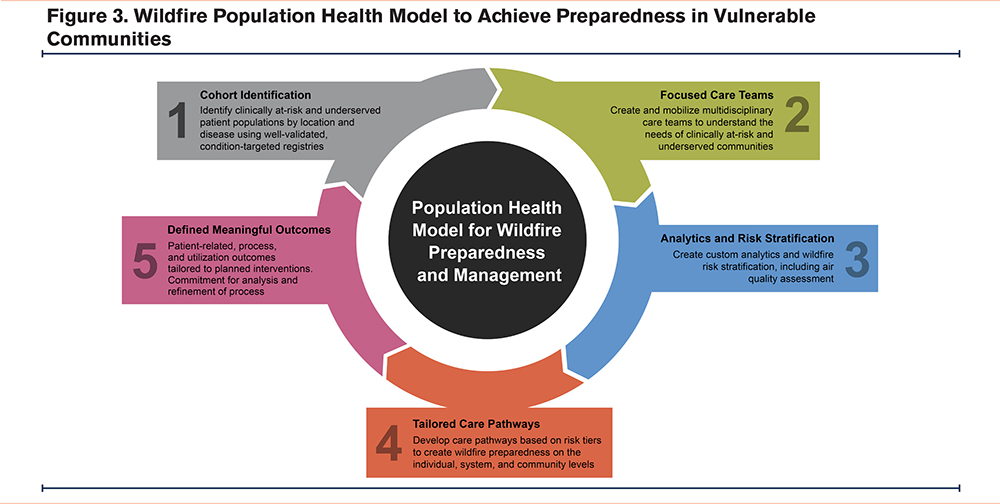
To best serve clinically at-risk and underserved populations, health systems must engage with community organizations and public health data to develop and mobilize a wildfire preparedness action plan on the individual, system, and community levels. To achieve this, UCDH developed the Wildfire Population Health Approach (Figure 3) consisting of 5 pillars: (1) identify clinically at-risk and underserved patient populations using well-validated, condition-targeted registries; (2) assemble multidisciplinary care teams (including community organizations, environmental scientists, public health professionals, and governmental institutions) to understand the needs of these communities and patients; (3) create custom analytics leveraging public health data to stratify wildfire risk; (4) develop care pathways based on wildfire risk by disease, risk of exposure, and health care access; and (5) identify outcome measures tailored to interventions with a commitment to continuous, iterative improvement efforts. Population health approaches have been successfully implemented for cost reductions in patients with dementia, chronic kidney disease, and cancer.32,33 In the following sections, we provide details on the pillars with practical examples of how to implement them.
Identify Clinically At-Risk and Underserved Patient Populations by Clinical Conditions and Social Factors
To direct wildfire preparedness interventions to those who need them, high-risk and underserved populations must be identified. Care teams at UCDH developed and charted validated condition-targeted registries, using institution-refined and validated cohort definitions for COPD and asthma, with efforts made to reduce false-positive diagnoses. Respiratory therapist care managers use these registries to identify patients with COPD or asthma at high risk for hospitalizations or emergency department visits within 12 months. Collaborating with public health entities is also vital to understanding how best to merge and leverage community public health and local data. To improve diagnostics at UCDH, near-continuous wildfire smoke exposure risk by zip code (as measured by the Air Quality Index available from the AirNow website27) is integrated into the electronic health records. Additionally, data are obtained from the Healthy Places Index scores for California zip codes and the Area Deprivation Index scores for non-California zip codes. Together, these integrated data help identify patients living in regions with active fires or smoke exposure, where the risk of disease exacerbation is high. By using these data in the Sacramento, California region during the 2021 wildfire season, local care teams identified patients living in specific zip codes at higher risk of wildfire exposure in nearly real time. Local individual patient data revealed that Black and Latinx individuals had a higher prevalence of COPD and asthma, and Black, Latinx, and non-English speaking individuals had greater rates of respiratory-related hospitalizations (Gupta R, Kuhn BT, unpublished data, 2023).
A study conducted by UCDH on the impact of wildfires on the health and safety of agricultural workers found that many farm workers experience poor air quality regularly, and often have little protection or education on safety.34 There are challenges in reaching these workers, who are often undocumented and face legal and financial barriers to health care. Participants in this study suggested that campaigns on the radio, social media, and in-person training could increase awareness and safety-conscious behaviors among farm workers. The study concluded that safety messaging about wildfires and wildfire smoke should be tailored to this community and their unique needs.34 To do this, health systems need to work collaboratively and supportively with researchers, especially in their own institutions. UCDH has used this approach with the Western Center for Agricultural Health and Safety, which focuses on the understanding and prevention of illness and injuries in agriculture. They offer education and outreach in English and Spanish, and one of their programs is specifically on wildfire smoke exposure. They also offer free downloadable bilingual materials on their website.35
Machine-learning tools, including natural language processing (NLP) of clinician notes, are also used to identify patients with COPD or asthma at high risk for hospital admission.36 UCDH developed a model from local electronic health record-derived, readily available data, using structured data types (quantitative input such as laboratory and spirometry values) and NLP-derived data from patient notes, improving the ability to predict at-risk patients. While there are challenges with generalizability, for the purposes of local patient care and analysis, internally validated predictive models are effective tools for cohort identification, risk assessment, and measuring the delivery of care.37
Assemble Multidisciplinary Care Teams
Patients impacted by wildfires interact with many different care members during their health journey. Health systems can assemble targeted, trained care teams who can engage patients in different settings, such as clinics, hospitals, workplaces, and at home—where most smoke exposure occurs. Team members interacting in the clinic setting can include physicians (pulmonary, primary care, emergency medicine, and inpatient hospital-based physicians), respiratory therapists, nurses, care managers, discharge planners, and community health workers. Team members who work in the ambulatory setting or across settings can help to understand patient needs at home, such as protective air filtration systems and insulation. Local advocacy groups, such as migrant worker groups, can serve as liaisons between communities affected by wildfires and the health system. Care teams should aim to understand community needs, provide education, and implement customized, local interventions, as discussed further in the tailored care pathway section below.
Create Custom Analytics and Wildfire-Risk Stratification
A well-curated registry of clinically at-risk and underserved patients can provide various data, including health care utilization, symptom burden, prescription patterns, race and ethnicity/language information, geocoding indexes, and recent air quality scores. Registries defined with only diagnostic codes have poor specificity and sensitivity in detecting patients with COPD and asthma. Therefore, to accurately detect these patients in a registry, multiple variables are needed, including diagnostic codes, use of controller medications, spirometry data, and whether a specialist made the diagnosis. To optimize risk analysis for patients more vulnerable to wildfire smoke, the population health team at UCDH integrated air quality data from the AirNow website27 into the electronic health record. This website provides detailed information on air quality and wildfire maps throughout the United States and, thus, this strategy could be widely adopted by clinical teams across the country.
Develop Tailored Care Pathways
This population health approach aims to achieve wildfire preparedness on the individual, system, and community levels through equity-focused, proactive outreach and education. UCDH provides air quality health education and outreach strategies personalized to specific patients and where they live. Using patient registries, health systems can identify patients at high risk for an emergency department visit or hospitalization due to respiratory causes during wildfire exposures. Using this information, care teams can create care pathways tailored to specific high-risk groups, with whom they can engage in proactive and personalized outreach via telephone, texts, or in-person visits, and in home, community, and clinical settings. UCDH identified and hired a COPD and asthma care manager to focus on responding to these patients and providing guidance and care as needed—another strategy that could be widely adopted beyond UCDH.
To mitigate the disproportionate burden of climate change on underserved communities, care teams should focus on interventions that provide patients with supplies, information, quality air filtration, transportation, and proactive testing for underlying high-risk conditions, such as AATD. For example, care teams can set up electronic health record messages that are triggered when air quality reaches harmful levels for both sensitive and general populations, providing recommendations for maintaining air quality in the home. In addition, they can build and distribute COPD and asthma “go-bags” with basic supplies for at-risk patients. To reduce potential inequities, these teams can also focus on additional language-concordant outreach to high-risk patients. Further, by partnering with community organizers, care teams can provide vulnerable patients with information on local resources and safety measures to reduce adverse health outcomes during wildfires.
Unfortunately, during a fire, high-efficiency particulate air filters are hard to find and are too costly for financially vulnerable patients. Care teams can partner with public health and community leaders to ensure that community shelters are equipped with high-quality air filtration systems and can provide at-risk patients with education on do-it-yourself (DIY) air filters, which have been shown effective in reducing indoor levels of small particular matter.38 The California Air Resources Board recommends creating a temporary DIY air filter if individuals are unable to obtain a commercial air filtration product.39
For patients with reduced access to care, providing transportation to physician offices, emergency departments, and hospitals may reduce symptom burden. Programs also have been developed to provide mobile wildfire-related health assessment and treatment and to understand the experiences of vulnerable individuals, such as migrant workers, whose work exposes them to high environmental risk. UCDH has a mobile clinic with a designated spirometry area and examination room to provide flexible options for medical surveillance evaluations throughout their service area. Adoption of similar mobile clinics could be an asset in reaching patients with limited access to health care.
Leveraging a population health approach has the potential to increase the identification of patients at high risk for development of COPD or asthma. The impact of wildfire smoke on airway health in patients with AATD has not been determined, but increased exposure to pollutants could be damaging to this vulnerable population. Utilizing guidelines-based care could improve the identification of high-risk patients who are vulnerable to disease deterioration during wildfires. While free and anonymous testing for AATD has been available to patients and providers, screening rates have remained low.40
Defining Meaningful Outcomes
As with other health system models, it is imperative to commit to ongoing process improvement informed by the experience gained from implementing the pathways. UCDH is currently involved in an ongoing clinical trial to assess the educational impact of their interventions. In COPD and asthma care, impactful outcomes can include reducing clinical exacerbations and hospitalizations, increasing patient-related outcomes (e.g., the number of patients provided with filters and perception of preparedness), and reducing inequities. However, sustaining these improved outcomes will require data and infrastructure monitoring to support evaluation and broad implementation.
Sustaining Health-System Climate-Change Interventions
To support rapid action in patient outreach during wildfires, health systems require policy changes. Health systems can build programs that support efforts similar to the Centers for Disease Control and Prevention’s “Building Resilience Against Climate Effects” framework, which guides communities to strategize and prepare for the health effects of climate change, such as wildfires.41 In 2021, the U.S. government established the Office of Climate Change and Health Equity (OCCHE) within the U.S. Health and Human Services (HHS) department to directly address climate change.42 OCCHE coordinates HHS departments to respond to threats due to climate change including: (1) strengthening the resiliency and response within health care and public health services; (2) supporting efforts to close information gaps, synthesize data, and identify practical applications of information; (3) coordinating efforts to develop communication and education on climate-related health threats, including materials tailored to vulnerable communities; and (4) aligning strategies to support health care systems in reducing carbon emissions.43 With a well-resourced national coordinating agency to provide guidance on how to rapidly respond during climate change threats, such as wildfires, health systems and public health organizations can be better prepared to meet community needs and keep patients healthier at home. Most immediately, however, health systems can partner with local public health entities to align strategies.
Conclusion and Call to Action
As climate change progresses, wildfires are now a yearly expectation. To meet the needs of clinically at-risk and underserved patients who are affected by this increasing health threat, health systems must replace reactionary approaches with collaborative, innovative, and proactive approaches. With the Wildfire Population Health Approach outlined here, we provide a plan of action for health systems and care teams to adapt to their communities, circumstances, and needs. The framework calls for investments in developing registries, demographic and social data, and analytics for risk stratification; partnership with public health and community organizations; leadership support to prioritize and develop multidisciplinary teams; and resourcing staff and technology to implement care pathways. In the coming years, it will be crucial to prepare health systems, clinicians, and communities to manage the profound health impacts of environmental events and prevent potentially devastating consequences. Additionally, policymakers can further support data and staff infrastructure to sustain this rapid outreach at scale to patients at risk from wildfire exposure. Climate change and increasingly frequent wildfires are changing the lives and threatening the health of our communities, especially those already at highest risk for poor health. Health systems can adapt to this threat by adopting an air quality-focused population health approach.
Acknowledgements
Author contributions: Both authors contributed equally to the development of the manuscript. The content of this manuscript, the ultimate interpretation, and the decision to submit it for publication in the Chronic Obstructive Pulmonary Diseases: Journal of the COPD Foundation were independently under the control of the authors.
Declaration of Interests
Dr. Gupta has nothing to disclose. Dr. Kuhn has received payment or honoraria for speakers’ bureaus from Regeneron, Takeda, and Grifols; has participated on advisory boards for GSK and Verona; and is the incoming president (unpaid) for the California Thoracic Society. Under the direction of the authors, medical writing services were provided by Jacqueline Register, MSc, and Samantha Wronski Holloway, MS, of Oxford PharmaGenesis Inc., Newtown, Pennsylvania, and were funded by Takeda Pharmaceuticals USA, Inc., Cambridge, Massachusetts. No payments were made to Drs. Kuhn or Gupta or to the University of California Davis team.