Running Head: Misused Inhaler in Patients Hospitalized With COPD
Funding Support: This work was funded by a Hospital of Fribourg grant (grant-2307), HFR Fribourg, Fribourg, Switzerland. The funder of the study was not involved in the study design, data collection, data analysis, data interpretation, and writing of the report.
Date of Acceptance: June 14, 2024 | Publication Online Date: June 20, 2024
Abbreviations: BMI=body mass index; CAT=COPD assessment test; CI=confidence interval; COPD=chronic obstructive pulmonary disease; DPIs=dry powder inhalers; HFR=Hospital of Fribourg; ICU=intensive care unit; LTOT=long-term oxygen therapy at home; mMRC=modified Medical Research Council; PIF=peak inspiratory flow; pMDI=pressurized metered-dose inhaler; SD=standard deviation
Citation: Grandmaison G, Grobéty T, Vaucher J, Hayoz D, Suter P. Prevalence of critical errors and insufficient peak inspiratory flow in patients hospitalized with COPD in a department of general internal medicine: a cross-sectional study. Chronic Obstr Pulm Dis. 2024; 11(4): 406-415. doi: http://doi.org/10.15326/jcopdf.2024.0505
Online Supplemental Material: Read Online Supplemental Material (455KB)
Introduction
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and the third leading cause of mortality worldwide.1 The pharmaceutical treatment of COPD relies mainly on the administration of medications via inhalation. However, the effectiveness of these treatments is very often hampered by the suboptimal utilization of inhalers, which may arise due to errors in inhalation technique, insufficient peak inspiratory flow (PIF), or the use of unsuitable inhaler devices.1
Errors in inhalation techniques are remarkably prevalent and associated with inefficient symptom control, a reduction in quality of life, an upsurge in exacerbations, and an escalated reliance on health care systems.2-5 In addition, specific inhaler types, such as dry powder inhalers (DPIs), demand a robust and profound inhalation effort to de-agglomerate the medication-containing powder within the inhaler and enable its deposition within the distal airways.6,7 The use of an inhaler with insufficient PIF is also associated with an increase in exacerbations and a higher frequency of hospital admissions.8-10 Furthermore, certain patient characteristics, such as lack of manual dexterity or cognitive impairments, impose limitations on the capacity to optimally use inhalers.11
The prevalence of errors in inhalation technique and insufficient PIF has predominantly been described in the outpatient setting. Furthermore, few studies have simultaneously examined the presence of errors in inhalation technique and PIF, despite the fact that both are critical factors for achieving optimal inhaler utilization.12,13 Finally, there is little information regarding the prevalence of inhalers unsuited to patient characteristics, including those that cannot be used optimally even with proper instruction.
In this cross-sectional study, we describe the prevalence of misused inhalers among COPD patients upon admission to an internal medicine department. An inhaler was considered to be misused if employed with critical errors in inhalation technique and/or insufficient PIF.
Methods
Study Design and Participants
This monocentric cross-sectional study recruited patients in the internal medicine department of the Hospital of Fribourg (HFR), Fribourg, Switzerland, from August 1, 2022 to April 3,2023. The study was approved by the Ethics Commission of the Canton of Vaud (project #: BASEC 2022-00910) and all participants provided written consent. The results are reported in accordance with the “Strengthening the Reporting of Observational Studies in Epidemiology” statement.14
All adult patients with a COPD diagnosis mentioned in their electronic record admitted to the HFR general internal medicine department and using an inhaler before hospitalization were assessed for eligibility. Exclusion criteria were an inability to complete the initial assessment due to language, physical or cognitive problems, and previous inclusion in the study. Each participant underwent an interview conducted by a research nurse within 72 hours of admission to the internal medicine department to collect demographic data and information concerning the diagnosis and the treatment of COPD and inhaler utilization. Patients were then assessed by a physiotherapist to check the inhalation technique, to measure the PIF, and to test the ability to correctly use their inhaler following comprehensive therapeutic education. This assessment was carried out for all inhalers used at the time of admission to internal medicine. Each physiotherapist conducting the assessment received a 30-minute training session to standardize the evaluation and teaching technique.
The physiotherapist examined the inhalation technique through direct observation using tailored checklists designed for each type of inhaler (Supplemental Figure S1 in the online supplement). Based on the patient information leaflets and previous literature, a critical error was defined as an action or inaction that could have a detrimental impact on the delivery of the drug to the distal airways.3-5 In the case of critical errors, the patient benefited from a targeted teach-to-goal intervention focused on the specific gaps identified during the initial assessment. The teaching was repeated until the inhalation technique was performed without critical errors. The inhalation technique was classified as "not teachable" if the patient continued to exhibit critical errors despite receiving 3 repetitions of the instructions.
PIF was assessed using the In-Check Dial G16® (Alliance Tech Medical, Inc, Hillsborough, North Carolina), a hand-held device designed to replicate the internal resistance profile of the different inhalers.15 PIF was measured at the resistance level corresponding to the inhaler used by the patient. The highest value among 3 consecutive inspiratory maneuvers was considered as the PIF measurement. If the measured PIF was below the minimum flow for optimal use, the inhaler was considered to be used with an insufficient PIF.6,15 As nebulized aerosols are administered by health care professionals during hospitalization and do not require a minimum PIF, they were considered to be used optimally and were not included in the study.
Outcomes
The primary outcome was the proportion of misused inhalers. The inhaler was considered misused when used with at least one critical error and/or insufficient PIF measured prior to the teach-to-goal intervention. This composite outcome was chosen because it combines 2 factors of suboptimal inhaler use associated with poor disease control. The primary outcome was assessed in the following subgroups: male versus female; <65 years versus ≥65 years; admission for an acute COPD exacerbation (present versus absent); or for a respiratory problem (present versus absent). The presence of a COPD exacerbation or hospitalization due to a respiratory complaint was defined by reviewing the patient's admission document and electronic record. A diagnosis of COPD exacerbation was based on information documented in the electronic record by the patient's doctor. A hospitalization with increased respiratory symptoms compared to the usual symptomatology was considered a hospitalization with a respiratory complaint.
Secondary outcomes included the prevalence of inhalers used with at least one critical error, used with insufficient PIF, unable to be used despite adequate teaching, and unsuitable inhalers. An unsuitable inhaler was defined as an inhaler that cannot be used optimally, either because of an insufficient PIF or because of an inability to use an inhaler optimally despite specific teaching. These outcomes were presented for all inhalers, by patient and by type of inhaler.
Statistical Analysis
Data from the literature suggest that 60% of hospitalized patients with COPD make critical errors when handling their devices.16 In order to have a margin of error of 10% when assessing the proportion of misused inhalers with a statistical significance level of 5% and considering that each patient uses one inhaler, we estimated that we needed a sample size of 93 patients.17 To allow for intrapatient correlation (cluster=patient), a clustered sandwich estimator was specified to calculate the standard errors. Critical errors, insufficient PIF, and inhalers unable to be used despite adequate teaching and unsuitable inhalers were expressed by proportions with their confidence interval estimated from the above-mentioned statistical model.18 If missing data were less than 5%, the analysis was based on complete cases only.19 Study data were collected and managed using REDCap electronic data capture tools hosted at the University of Fribourg.20
Data are presented as mean +/- standard deviation (SD) for normally distributed values, as median and interquartile range for non-normally distributed values, and as number and percentage for categorical values. Continuous variables were compared with a Student’s t-test for normally distributed variables and with a Mann-Whitney U-test for variables with an abnormal distribution. Categorical values were compared using an χ2 test. The level of statistical significance was defined as a p-value <0.05. Secondary analyses have not been adjusted for multiple comparisons. Statistical tests were performed using STATA version 17 (StataCorp LLC, College Station, Texas).
Results
Patient Characteristics
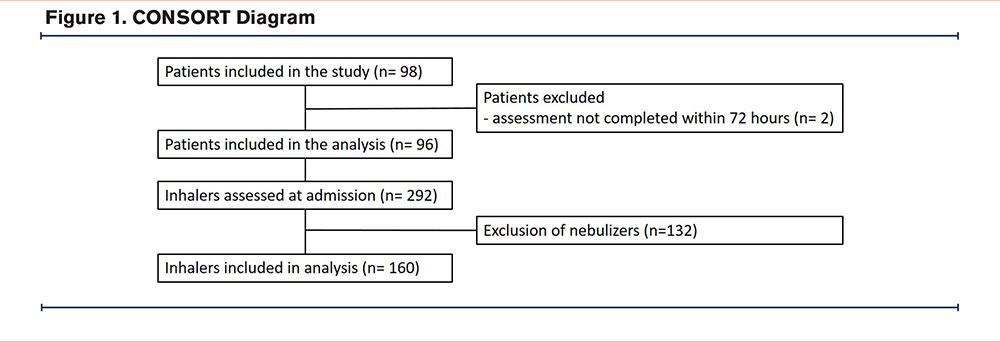
The consort flow diagram is shown in Figure 1. Of 98 patients included in the study, 2 were excluded as the physiotherapist assessment could not be completed within 72 hours of admission. Baseline demographic and medical characteristics of patients are shown in Table 1. Mean age was 71.6 (SD 9.8 years), 60 (63 %) were men, and 64 (67%) were hospitalized with a COPD exacerbation. Patients used an average of 3.0 inhalers (SD 1.2) and 292 inhalers were assessed. The distribution of inhalers is described in Supplemental Table S1 in the online supplement. Nebulizers are considered to be used correctly as they are administered by nursing staff and not reliant on a minimum PIF. Consequently, 132 nebulizers were excluded and a total of 160 inhalers were included in the final analysis (Figure 1).
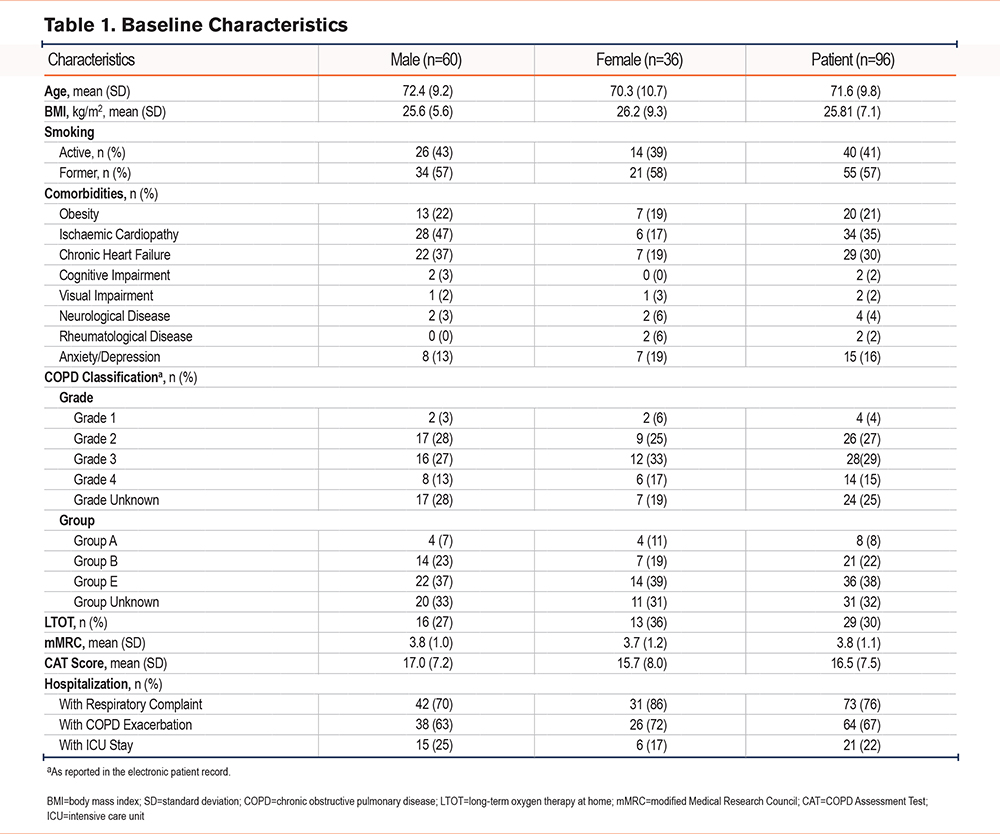
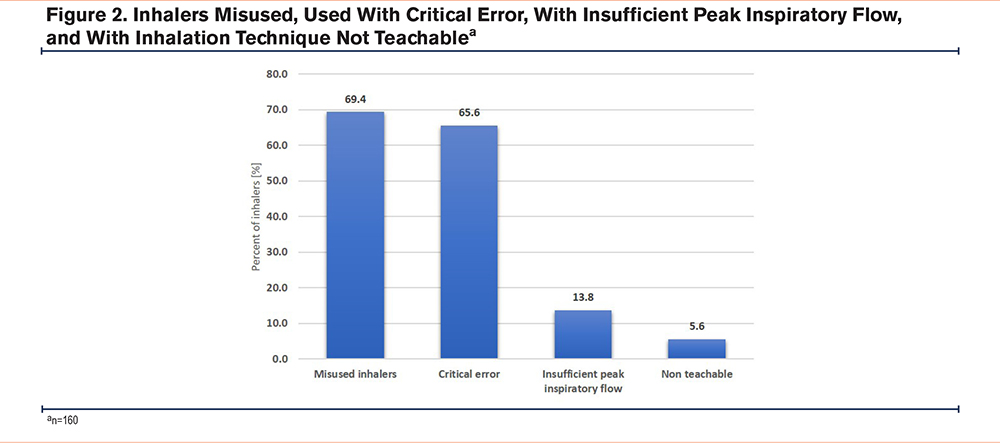
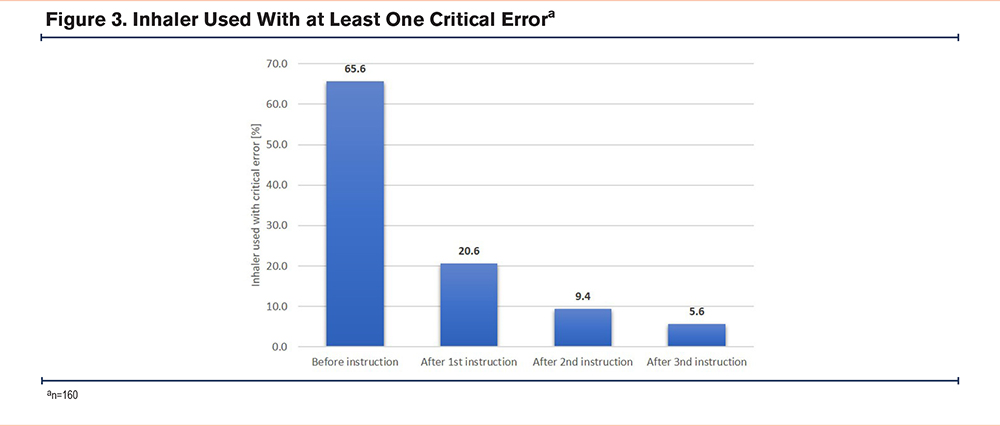
During the assessment conducted by physiotherapists, 111 (69.4%) inhalers were misused. Among these, 105 (65.6%) were used with at least one critical error and 22 (13.8%) with an insufficient PIF (Table 2; Figure 2). Inhalers were used with a mean of 1.4 errors (SD 1.4) and 1.3 critical errors (SD 1.3). The types of errors made are described in Supplemental Table S2 in the online supplement. Over the course of teaching sessions, there was a notable reduction in the number of inhalers being used with critical errors. After one teaching session, 33 inhalers (20.6%) exhibited critical errors, decreasing to 15 inhalers (9.4%) after 2 teaching sessions. Even after 3 teaching sessions, the inhalation technique used for 9 (5.6%) inhalers still presented with at least one critical error and was considered not teachable (Figure 3). Several factors were identified to explain the inability to achieve an adequate inhalation technique, including cognitive disorders (n=5), fine motor disorders (n=2), a lack of coordination between inhaler activation and inspiration (n=4), and the inability to hold one's breath sufficiently (n=2). Moreover, 27 inhalers (16.9%) were deemed unsuitable for optimal use, even after adequate training, due to the persistence of a critical error and/or insufficient PIF.
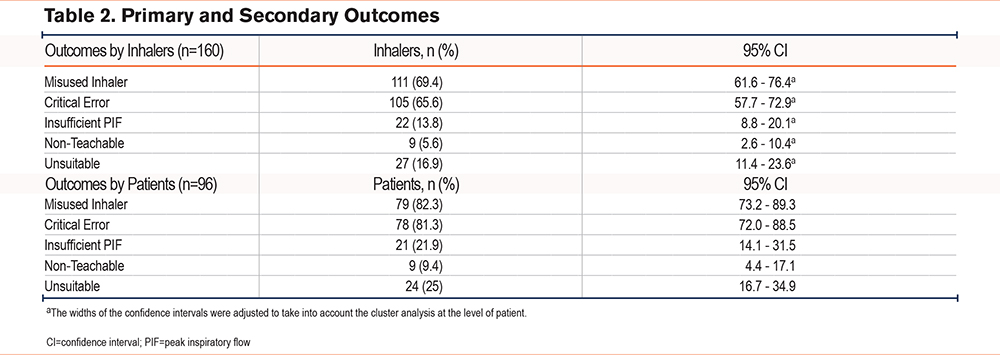
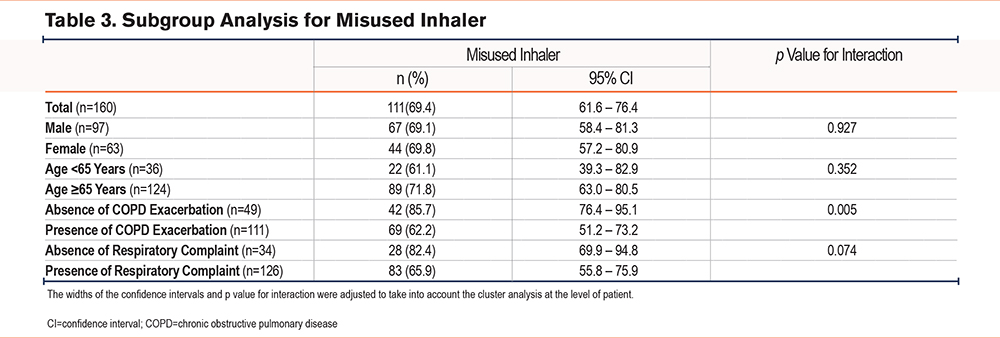
In the subgroup analysis, the proportion of inhalers used with at least one critical error was lower when patients were hospitalized for a COPD exacerbation or a respiratory cause (Table 3; Supplemental Table S3 in the online supplement). These results were consistent in a sensitivity analysis including all types of inhalers, including nebulizers. Age and gender were not associated with the proportion of misused inhalers, used with at least one critical error or with insufficient PIF. Analysis by patient showed that 79 (82.3%) patients used at least one misused inhaler, 78 (81.3%) used at least one inhaler with a critical error, and 21 (21.9%) with insufficient PIF (Table 3). After 3 teachings, 9 patients (9.4%) continued to use at least one inhaler with a critical error. A total of 24 patients (25%) were using at least one unsuitable inhaler, either because of an inability to use an inhaler without a critical error after 3 teachings or because of an insufficient PIF. Results by inhaler type are shown in Supplemental Table S4 in the online supplement. Due to the heterogeneous number of inhalers in each category and sometimes the small number of inhalers in each category, a direct comparison between different types of inhalers was not possible.
Discussion
In this study evaluating inhalers used by 96 patients diagnosed with COPD and hospitalized in a department of general internal medicine, 69.4% of inhalers were misused due to a critical error (65.6%) or insufficient PIF (13.8%). Despite adequate instruction, 5.6% of inhalers could not be used without a critical error. When combining inhalers that could not be used adequately after instruction and those used with an insufficient PIF, 16.9% were unsuitable for the patient.
The findings of this study underscore a prevalent issue in the management of patients with COPD within hospital settings, i.e., the widespread occurrence of suboptimal inhaler use. These results align with previous observations in both outpatient settings and limited hospital-based investigations2,4,10 and highlight several important issues when considering inhaler use among patients hospitalized with COPD. First, critical errors in inhalation technique are common and require the use of every available opportunity to control inhalation technique. Second, 13.8% of inhalers are used suboptimally due to patients’ inability to generate sufficient PIF. This figure rises to 26.5% when focusing solely on DPIs that mandate sufficient PIF for optimal function. Integrating PIF measurements, therefore, seems necessary to ensure an optimal use of the inhaler. Third, the therapeutic education provided during the evaluation led to a 45% reduction in the number of inhalers used with a critical error after one teaching round, 11.2% after the second lesson, and 3.8% after the third lesson. These results highlight the benefit of repeated therapeutic education. Although, the number of instructions to be given before concluding that the inhaler cannot be used remains to be determined, the literature emphasizes the importance of repeating the instruction over time, and hospitalization seems a good opportunity to do so.21,22 Finally, despite repeated and targeted instruction, a significant number of inhalers persistently elude correct usage. Simply demonstrating the correct inhalation technique, even if targeted to the patient’s specific errors, does not rectify improper inhalation techniques for each patient. This inability to perform an optimal inhalation technique despite adequate teaching is explained in our study by the presence of patient-related characteristics, namely cognitive impairment, fine motor impairment, inability to coordinate activation of the inhaler and inspiration when using a pressurized metered-dose inhaler (pMDI), and inability to hold sufficient inspiration. These factors limiting the possibility of using inhalers correctly are consistent with the data in the literature.2,11 This last point underlines the importance of considering patient-specific characteristics when selecting an inhaler and of regularly evaluating the technique of inhalation, given the potential evolution of these characteristics over time.11
In our study, 82.3% of patients were using at least 1 of their inhalers in a suboptimal manner, characterized by either one critical error (81.3%) or insufficient PIF (21.9%). A subgroup analysis showed that, paradoxically, the fact of not being admitted to the hospital for a COPD exacerbation or a respiratory complaint was associated with a higher prevalence of suboptimal inhaler use and with a critical error. This association poses a challenge for interpretation as the suboptimal use of inhalers typically correlates with a higher frequency of exacerbations.2,4 As the assessment was carried out during the first 72 hours of hospitalization, it is possible that patients hospitalized for a COPD exacerbation or respiratory problem received more focused attention regarding their inhalers during their stay in the emergency ward or during the early phase of hospitalization. In any case, this observation emphasizes the importance of evaluating the inhalation technique of all patients with COPD using an inhaler and not solely confined to those hospitalized due to a COPD exacerbation or poorly controlled disease.
The inhaler evaluation method employed in this study comprises a 3-step approach. First, patients demonstrated their inhalation, and the technique was assessed using a checklist specific to each inhaler. Second, the assessment involved measuring PIF using the In-Check Dial G16®. Finally, targeted education was provided to address any errors identified during the demonstration of the inhalation technique. These steps were conducted by a trained physiotherapist. The expertise required to carry out this evaluation involved a 30-minute training session, while the actual evaluation of the inhalers took between 10 and 15 minutes, depending on the number of inhalers used and the number of identified errors. Involving a person trained in inhaler evaluation seems to be a good strategy to compensate for physicians' lack of knowledge and/or time constraints.23 Consequently, this method presents as an easily implementable approach, not only enabling targeted therapeutic education to be given but also to identify inhalers that need to be replaced because of an inability to generate a sufficient PIF or to perform an adequate inhalation technique. Considering the established association between suboptimal inhaler usage and adverse outcomes such as poor disease control, more frequent exacerbations, and increased costs, integrating such a strategy should be an integral part of the management of hospitalized patients diagnosed with COPD.4,10,13
It is, however, important to emphasize that our study assessed the inhalers used in the hospital. Therefore, the reason for hospitalization could have played a role in the results obtained by influencing the patient's ability to use their inhaler correctly or to generate a sufficient PIF. For example, two-thirds of the participants in our study were experiencing a COPD exacerbation at the time of their admission. The impact of a COPD exacerbation on PIF is uncertain, and it is possible that PIF could be transiently decreased.10,24,25 The information obtained during the initial assessment allows for the selection of an inhaler suitable for the acute phase, but does not determine the patient's ability to use a type of inhaler outside of this context. An evaluation of the inhalation technique and PIF seems to be necessary when the patient's condition changes.1,10
Strengths and Limitations
This study has several strengths. First, it included all patients hospitalized with a diagnosis of COPD and highlighted that the suboptimal use of inhalers is a problem, regardless of the reason for hospitalization. Second, we were able to detail the causes of suboptimal use, namely errors in inhalation technique, insufficient PIF, or an unsuitable inhaler. We were also able to specify the reasons why an inhaler might remain unusable despite adequate teaching.
There are also some limitations to this study. First, we explored PIF with the help of the In-Check Dial G16® by asking the patient to inhale as rapidly and forcefully as possible. PIF measurement under these conditions does not necessarily represent the PIF used by the patient when using an inhaler under real-life conditions.13 Consequently, our results may underestimate the true prevalence of inhalers used with inadequate PIF. Second, the assessment was carried out within 72 hours of admission. Patients, particularly those with respiratory complaints, may have benefited from teaching or adaptation of their inhaler prior to the assessment, again leading to an underestimation of the prevalence of misused inhalers. Third, there is no consensus on which errors should be considered critical. Consequently, the steps defined as critical errors could have an influence on the proportion of inhalers used with a critical error. Fourth, the evaluation relies on a visual assessment by the physiotherapist. Consequently, the evaluation of certain stages of the inhalation technique, such as the coordination between inhaler activation and inspiration when using a pMDI, may lack precision. Similarly, when using a pMDI, it was not taken into account whether the patient was breathing too forcefully. Fifth, the small sample size in our study made it impossible to assess the association between patient characteristics and suboptimal inhaler use. Similarly, the size of our sample does not allow us to comment on the association between different types of inhalers and their misuse. However, our observations confirm that the problem of inhalers used with a critical error affects all types of inhalers and that insufficient PIF is a serious and substantial clinical problem for DPIs. Sixth, the diagnosis of COPD was made based on information found in the patient's electronic file. With pulmonary functions not available for 25% of the patients, it is possible that some diagnoses may be incorrect. However, a recent study in our department showed that 87% of the COPD diagnoses recorded in our patients' electronic files could be confirmed by pulmonary functions.26 Finally, this is a monocentric study whose results should be confirmed in different centers. Nevertheless, the results are consistent with the current literature.10,16,27
Conclusion
Misused inhalers in hospitalized patients with COPD is a major problem, irrespective of the reason for hospitalization. Causes are critical errors in inhalation technique, insufficient PIF, or an unsuitable inhaler. The assessment of the inhalation technique and the PIF should be part of the standard clinical assessment of patients with COPD during hospitalization, regardless of the reason for hospitalization.
Acknowledgments
Author contributions: The study was conceived and designed by GG, PS, TG, and DH. GG, PS, and TG oversaw conduct of the study. Data were acquired by GG, PS, and TG. Data were analyzed by GG and interpreted by all authors. All authors read and approved the final version.
Data Availability Statement: The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors thank all the patients and their families, as well as the team of investigators involved in this study. Statistical data analysis support, under the direction of the authors, was provided by Mohamed Faouzi, Division of Biostatistics, Center for Primary Care and Public Health (Unisanté), University of Lausanne, Switzerland. Medical writing support, under the direction of the authors, was provided by Rosemary Sudan.
Declaration of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.