Running Head: Pneumothorax in Bronchoscopic Lung Volume Reduction
Funding Support: None
Date of Acceptance: June 20, 2024 | Publication Online Date: June 27, 2024
Abbreviations: 6MWD=6-minute walk distance; BLVR=bronchoscopic lung volume reduction; COPD=chronic obstructive pulmonary disease; EMR=electronic medical record; FEV1%pred=forced expiratory volume in 1 second percentage predicted; PFT=pulmonary function test; RV=residual volume; TLC=total lung capacity
Citation: Burgei JW, Alsheimer K, Lantry JF, Swalih M, Hehn BT. Retrospective review of pneumothorax rates in a rural, micropolitan area after bronchoscopic lung volume reduction. Chronic Obstr Pulm Dis. 2024; 11(5): 534-537. doi: http://doi.org/10.15326/jcopdf.2024.0502
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive disease with an estimated prevalence of 6% of adults and is the 6th leading cause of death in the United States.1,2 When looking at the demographics of patients with COPD, the prevalence in rural areas is almost double compared to the overall population (15.4% versus 8.4%).3 Living in a rural area by itself is a risk factor for the development of COPD even when accounting for socioeconomic factors and exposures that are more common in rural communities.3 There are numerous health care disparities in rural communities, and studies have shown greater morbidity and obstacles to care. Reasons for this include financial barriers, less education, worse overall health, and issues with transportation.4
Treatment for COPD has mainly focused on smoking cessation and pharmacologic therapy using inhalers. Recently, bronchoscopic lung volume reduction (BLVR) was approved for people with emphysema and air trapping after the TRANSFORM5 (2017) and LIBERATE6 (2018) trials. The procedure involves implanting endobronchial valves to intentionally cause atelectasis to improve ventilation-perfusion matching and to decrease air trapping. Studies have shown that BLVR results in clinically significant improvements in lung function, exercise tolerance, dyspnea, and quality of life.5,6 These studies, however, were mostly performed in urban academic hospitals. The goal of this study is to perform a retrospective review of BLVR procedures performed at a rural community hospital located in a rural micropolitan area to determine if the procedure is safe to perform in this population.
Methods
The study was a single-center retrospective review of the electronic medical record (EMR). The hospital was a 288-bed tertiary care center with a pulmonary fellowship in Bradford County, Pennsylvania with a town census of 5461 residents located in the Sayre micropolitan statistical area.
Patients were included in the study if they underwent BLVR at the hospital for treatment of their COPD. The EMR was reviewed from January 2022, when the procedure was first performed at the hospital, until December 2023. If a patient had a redo of the procedure, only the original procedure was included in this review.
To be considered a candidate for the procedure, patients had to: (1) have COPD with a forced expiratory volume in 1 second percentage predicted (FEV1%pred) between 15%–45%, (2) have a total lung capacity (TLC) greater than 100% predicted, (3) have a residual volume (RV) greater than 150% predicted, (4) have a diffusion capacity for carbon monoxide greater than 20% predicted, (5) have a 6-minute walk distance (6MWD) between 100–500 meters, (6) have a body mass index of less than 35, (7) be a nonsmoker for at least 6 months, (8) have an arterial blood gas partial pressure of carbon dioxide of less than 50 mmHg, and (9) have a target lobe on the StratX report. All procedures were performed by the same interventional pulmonologist with a pulmonary fellow. Post-procedure patients were hospitalized for 72 hours with daily chest X-rays to monitor for pneumothoraxes. Patients were scheduled for a 14-day follow-up in the pulmonary clinic after the procedure.
Results
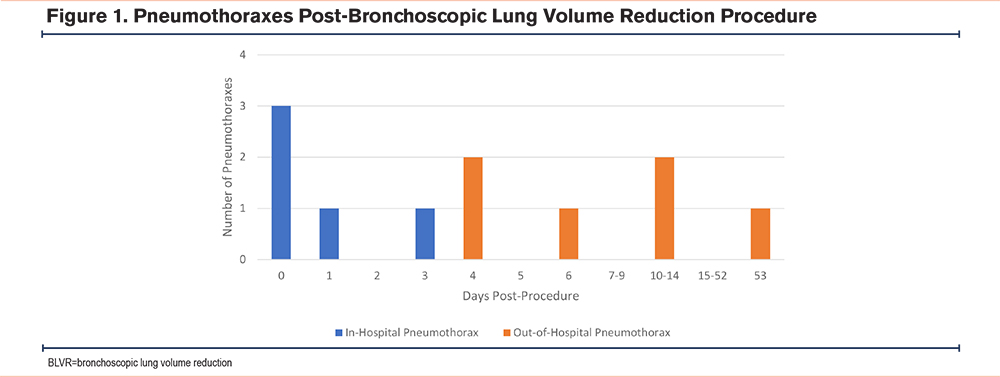
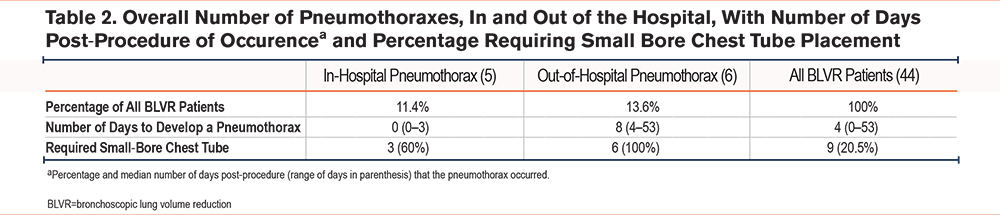
A total of 44 patients were included in the study with 11 (25%) developing a pneumothorax. The development of a pneumothorax ranged from 0–53 days post-procedure, with a median time of 4 days. Six of the 11 pneumothoraxes (54.5%) occurred outside of the hospital (Figure 1).
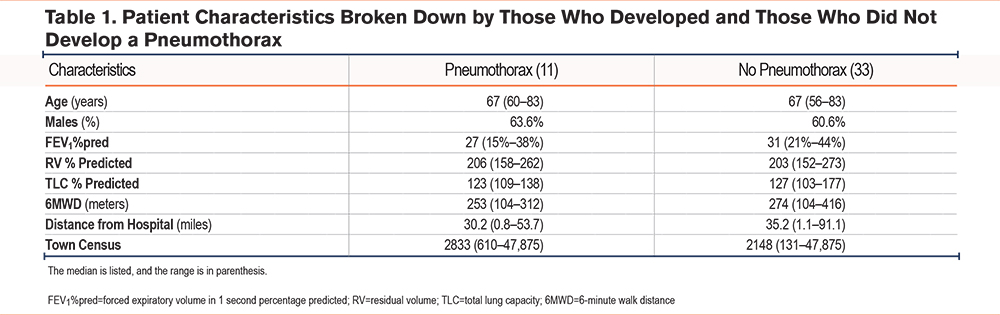
Patient characteristics are displayed in Table 1 based on age, the percentage that was male, FEV1%pred, RV, TLC, 6MWD, distance from the hospital, and town census. The distance from the hospital ranged from 0.8–91.7 miles (median 35 miles) and the town population sizes ranged from 131–47,875 people (median 2490.5). When reviewing occupations listed in the EMR, the most common jobs were laborers including construction, factory workers, carpenters, and mechanics. There were 4 patients who were nurses (median 2), a vet tech, and one who worked in customer service.
Pneumothoraxes were the only notable complication when reviewing the EMR. All pneumothoraxes, but 2 that occurred while in the hospital, required a small-bore chest tube. There was no reported death post-BLVR associated with the procedure (Table 2).
Discussion
BLVR has numerous benefits and this review showed that it is safe to perform in a rural micropolitan area. In reviewing the surgical literature, patients who live farther from their hospital had increased readmissions, postoperative complications, and delays in returning to daily activities.7 The major concern about BLVR is the risk for pneumothorax, which could go into tension if not treated quickly. In this study, patients lived in towns ranging from 131–47,875 people (median 2490.5) and traveled 0.8–91.7 miles (median 35 miles) to get to the hospital. This population is likely different than those studied at the clinical sites in the TRANSFORM trial (where only 2 of the 11 sites were in a city with a population of less than 100,000) or the LIBERATE trial (only 1 site had a population less than 80,000). This study is important as rural patients not only have double the incidence of COPD but also have higher levels of chronic disease and poor health outcomes compared to those in urban areas.8 However, the rates of pneumothoraxes in this study (25%) were similar to the LIBERATE (26.6%) and TRANSFORM (29.2%) Trials. Additionally, there were no deaths or other major complications from the procedure noted. One reason why the complication rate was probably similar in this study compared to the urban centers is that all of the procedures are performed by the same interventionalist. This allows one person to become more proficient with only a limited number of procedures available per year, rather than dividing the cases amongst multiple pulmonologists.
One main difference in our data collected was the increased number of postdischarge pneumothoraxes compared to the original studies. In this study, 54.5% of the pneumothoraxes occurred outside of the hospital with a median time of 4 days. In the TRANSFORM trial5 the median time to develop a pneumothorax was 1 day, and in the LIBERATE trial6 a total of 76% of the pneumothoraxes occurred by day 3. The difference likely has to do with the disparities the patients experience living in a rural environment. These disparities such as transportation, financial constraints, and fear of stigmatization from asking for help may have caused the patients to return to their regular activities sooner than recommended.4,7-9 One patient noted that she developed her pneumothorax the day after she returned home when she was bending down and twisted while lifting a laundry basket. A possible intervention to try and reduce this risk would be to recommend minimal lifting or activities for 14 days, rather than 7 days, until they are evaluated in the office. Another intervention should be to provide written and verbal instructions multiple times about appropriate activities that they can and cannot perform tailored to the community of the hospital (i.e., hunting, hiking, yard work, housework). Lastly, another important intervention would be to make sure that the patients have enough support in place prior to the procedure. However, even with the increased number of out-of-hospital pneumothoraxes, there was no major adverse outcome noted other than temporarily requiring a small-bore chest tube.
Our review had a few limitations. The first limitation is that this was a single-center review with only a limited number of procedures performed. All the original BLVR procedures performed at the hospital were included in the study, but the absolute number performed was 44 with only 11 pneumothoraxes identified. Another limitation to the study is that all procedures were performed by the same interventional pulmonologist. However, this is most likely typical for rural hospitals with a limited number of specialists.10
BLVR has been shown to have clinically significant benefits in quality of life, lung function, dyspnea, and exercise tolerance. This study is the first to look specifically at the rural population and review the risks of the procedure which appears safe to perform in a rural community setting.
Acknowledgements
Author contributions: JWB was in charge of the writing and analysis of the manuscript. JWB and BTH contributed to the design. JWB, BTH, KA, JFL, and MS contributed to the interpretation. BTH, KA, JFL, and MS contributed to the acquisition.
Data sharing statement: Individual de-identified participant data will only be shared in this article. There will be no related documents available.
Declaration of Interests
The authors have no conflicts of interest to declare.