Running Head: BMI on Risk of Exacerbation in Patients With COPD
Funding Support: Funding was provided by the Jinhua Science and Technology Bureau (2022-4-207)
Date of Acceptance: August 18, 2024 | Publication Online Date: August 29, 2024
Abbreviations: BMI=body mass index; CAT=COPD Assessment Test; CI=confidence interval; COPD=chronic obstructive pulmonary disease; FEV1=forced expiratory volume in 1 second; FVC=forced vital capacity; GOLD=Global initiative for chronic Obstructive Lung Disease; HRQL=health-related quality of life; MENA=Middle East and North Africa; NOS=Newcastle Ottawa Scale; PEF=peak expiratory flow; RR=relative risk; WHO=World Health Organization
Citation: Wang M, Ni X, Yu F. Impact of body mass index on the risk of exacerbation in patients with COPD: a systematic review and meta-analysis. Chronic Obstr Pulm Dis. 2024; 11(5): 524-533. doi: http://doi.org/10.15326/jcopdf.2024.0507
Online Supplemental Material: Read Online Supplemental Material (1118KB)
Introduction
Chronic obstructive pulmonary disease (COPD) is a debilitating respiratory condition.1,2 Current estimates suggest that in 2019 alone, the global prevalence of COPD among people aged 30–79 was around 10%, equating to about 392 million affected people.3 COPD exacerbations, marked by acute worsening of symptoms, are pivotal events in the natural course of the disease,4,5 and significantly contribute to the progression of COPD, accelerating declines in pulmonary function, compromising health-related quality of life (HRQL), and increasing mortality rates.6-8 Notably, patients with frequent or severe exacerbations are at higher risk of subsequent episodes, further increasing the overall high health care burden associated with this disease.9,10
Several meta-analyses that have documented the relationship between body mass index (BMI) and mortality in COPD, demonstrated an association between high BMI and lower mortality. These studies also reported that low BMI is linked to higher mortality.11,12 A review of Guo et al11that included 17 observational studies, summarized the evidence of the dose-response relationship between BMI and mortality in patients with COPD, and showed increased mortality risk in underweight but not in overweight and obese patients. The review also found that an increase in BMI resulted in a decrease in the risk of mortality.11 Similarly, a review by Cao et al12 that included 22 studies, documented that compared to patients with a normal BMI, underweight COPD patients had a higher mortality rate. In contrast, overweight and obese status was associated with lower mortality.12
In recent years, the role of BMI in influencing health outcomes, including COPD exacerbations, has become a focus of extensive research,13-15 While COPD is often accompanied by weight-related complications, such as involuntary weight loss and altered body composition.16 the intricate relationship between BMI and the risk of exacerbations remains inconclusive. Understanding this relationship holds substantial clinical implications, potentially guiding health care providers in risk stratification and the development of targeted interventions. This study aims to summarize current data on the association between BMI status and the risk of exacerbation in patients with COPD.
Methods
A systematic search strategy was conducted to identify relevant studies from 3 electronic databases: PubMed, Embase, and Scopus. Search criteria incorporated a combination of key terms: (“body mass index” OR “BMI” OR “underweight” OR “overweight” OR “obese” OR “obesity”) AND (“COPD” OR “obstructive lung disease” OR “chronic bronchitis” OR “pulmonary disease”) AND (“exacerbation” OR “remission” OR “worsening”). The search scope was confined to studies up to December 31, 2023, ensuring the inclusion of the latest and most relevant literature in the field. In addition to electronic searches, manual searches of reference lists and pertinent review articles were done to guarantee the comprehensive inclusion of relevant literature. However, this supplementary step did not result in the identification of additional relevant studies.
The primary outcome of interest was the risk of COPD exacerbation. Meta-analysis was performed in strict adherence to the Preferred Reporting Items for Systematic Reviews guidelines.17 The study protocol was registered in PROSPERO, an international prospective register of systematic reviews, before the initiation of the review (registration number CRD42024501386).
Study Selection Criteria
Eligible studies must have reported BMI measurements covering a spectrum of BMI categories such as underweight, average weight, overweight, and obese. We did not restrict selection based on specific criteria (such as World Health Organization [WHO] criteria) for categorizing BMI. Eligible studies must have reported on the association between BMI (either as continuous or categorical) and risk of COPD exacerbation. The definition of exacerbation should have been done according to recognized clinical criteria. Accepted study designs comprised cohort (prospective and retrospective), case-control, and cross-sectional studies published in peer-reviewed journals with no limitations on follow-up duration.
Studies were excluded if they reported on outcomes other than the risk of COPD exacerbation (e.g., mortality risk). Additionally, studies not focusing on BMI as the exposure were excluded. Non-English language studies were excluded unless English translation was accessible. Moreover, studies conducted before the year 2000 were excluded, as we intended to consolidate contemporary evidence. Case reports, case series, and reviews were excluded.
Process of Identifying Relevant Studies
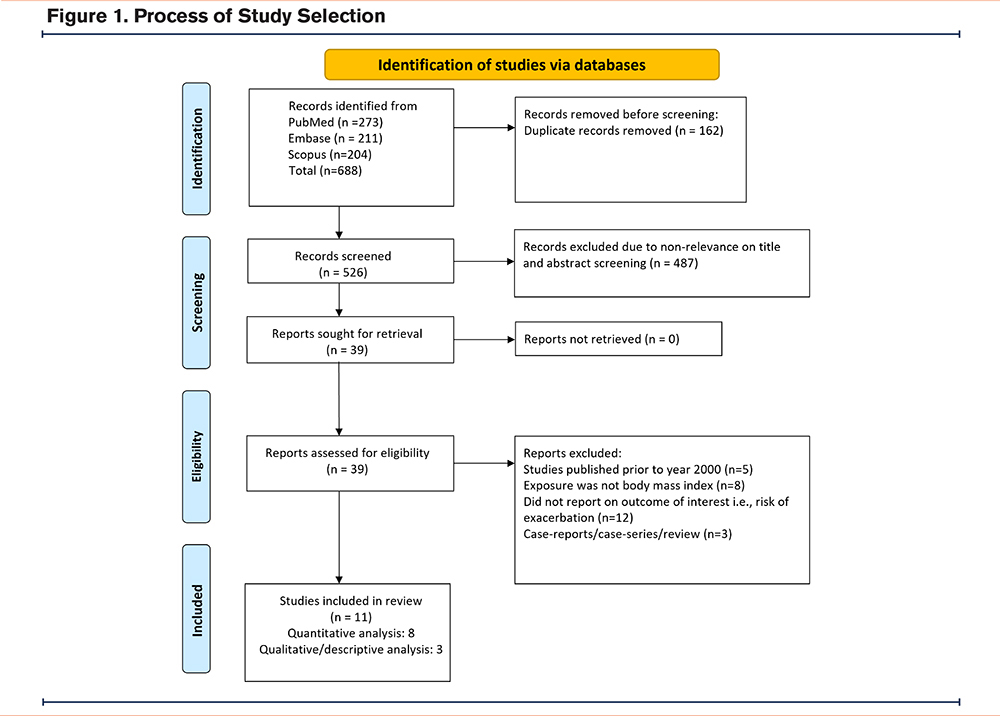
After compiling the initial pool of studies by executing the search strategy across the databases, duplicate studies were removed, and 2 study authors independently screened the titles and abstracts of the remaining studies. Studies that aligned with pre-established criteria were then selected for further full-text evaluation to establish their eligibility for inclusion. Discussions were conducted among the study authors in the case of discrepancies or disagreements regarding study inclusion.
Data Extraction
Relevant data were extracted by the 2 independent authors using a standardized data extraction form that included essential variables such as first author, year of publication, geographic location where the study was conducted, study design, baseline characteristics of the study participants, sample size, operational definitions adopted (for BMI and COPD exacerbation), and relevant findings for critical outcomes. Discussions between the 2 authors addressed any disparities in the data extraction process.
Quality Assessment and Statistical Analysis
The Newcastle-Ottawa Scale (NOS) was used for quality assessment.18 NOS is commonly used for assessing the methodological quality and bias risk in nonrandomized studies. The total score indicates the overall study quality, with higher scores denoting better methodological quality. The maximum achievable score is 9.
Pooled effect sizes were reported as relative risk (RR) with corresponding confidence intervals (CI). A random-effects model was used in all analyses to account for potential heterogeneity that was expected due to differences in baseline characteristics among the included studies. Publication bias was examined using Egger’s test and funnel plot.19
Throughout the comparisons, a normal BMI served as a reference. Sensitivity analysis was conducted after excluding studies with proportionately high assigned weights (due to large sample size) as well as subgroup analysis wherein studies with similar BMI-based cut-offs were pooled together. P<0.05 was considered statistically significant.
Results
A systematic literature search across the databases identified 688 studies. After eliminating 162 duplicates, titles and abstracts of 526 unique studies were screened, and an additional 487 studies were excluded. The remaining 39 studies underwent full-text screening for eligibility. Finally, as shown in Figure 1, eleven studies were included in the final analysis.20-30 The manual searches of reference lists and pertinent review articles did not lead to the identification of additional relevant studies.
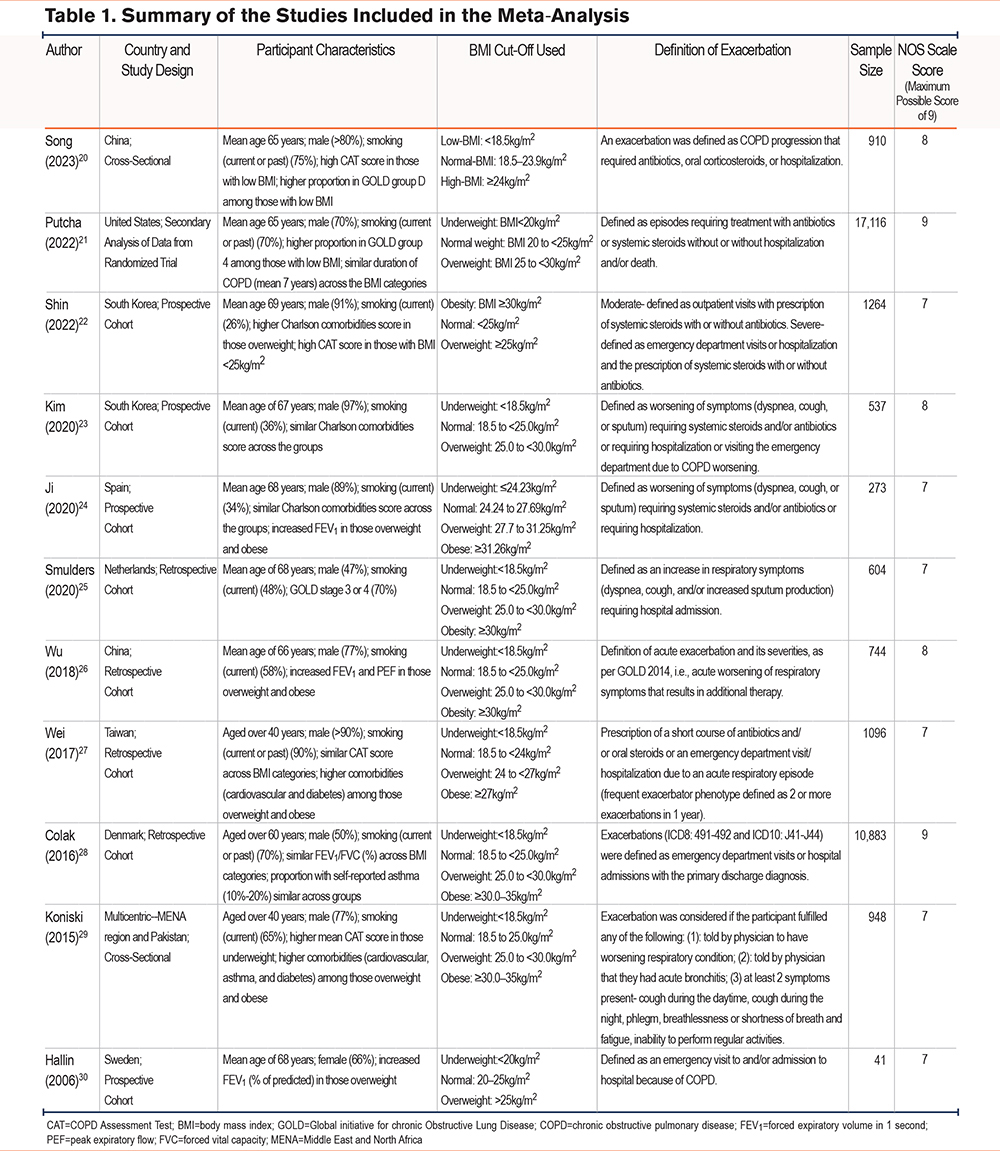
The 11 studies comprised 34,416 patients and were conducted in varied geographical locations. Two studies each were conducted in South Korea and China. One study each was performed in the United States, Spain, Netherlands, Taiwan, Denmark, and Sweden (Table 1). One multicentric study was conducted in the Middle East and North Africa (MENA) region and Pakistan. Four studies were prospective, and 4 were retrospective cohorts in design. There were 2 cross-sectional studies, and one study was a secondary data analysis from a randomized trial. Most patients were older than 60 years, and the majority were males. All studies had similar operational definitions for “exacerbation,” i.e., a worsening of respiratory symptoms that necessitates systemic steroids and/or antibiotics or requires hospitalization or a visit to the emergency department (Table 1). Six studies followed the standard WHO-based classification for categorizing patients based on their BMI (regular, underweight, overweight, and obese) (Table 1). All studies were of appropriate quality, with a mean NOS score of 7.54. Four studies obtained a score of 8, six obtained a score of 7, and one scored 9 (Table 1).
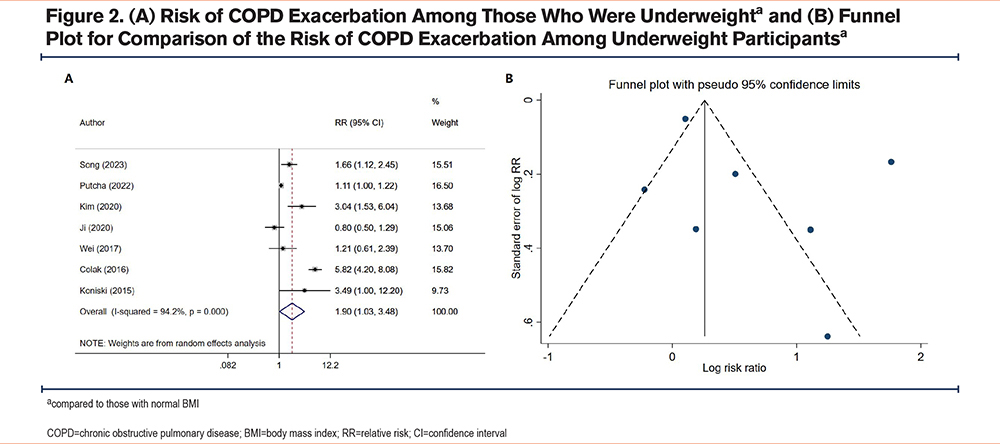
Risk of Exacerbation Among Underweight Participants
Compared to COPD patients with a normal BMI, underweight individuals were at increased risk of exacerbation (RR 1.90, 95% CI: 1.03, 3.48; N=7, I2=94.2%) (Figure 2A). There was no evidence of publication bias (Egger's test, p-value 0.28; Figure 2B). Sensitivity analysis after excluding the study by Putcha (2022) et al21 showed that being underweight was still associated with an increased risk of exacerbation (RR 2.11, 95% CI: 1.02, 4.38; N=6, I2=91.2%) (Supplementary Figure 1 in the online supplement). When the analysis was conducted with studies having a similar BMI-based cut-off to label “underweight” (i.e., BMI <18.5 kg/m2), the association was still significant i.e., underweight patients had an increased risk of exacerbation and the magnitude of association was stronger (RR 2.61, 95% CI: 1.31, 5.23; N=5, I2=87.2%) (Supplementary Figure 2 in the online supplement).
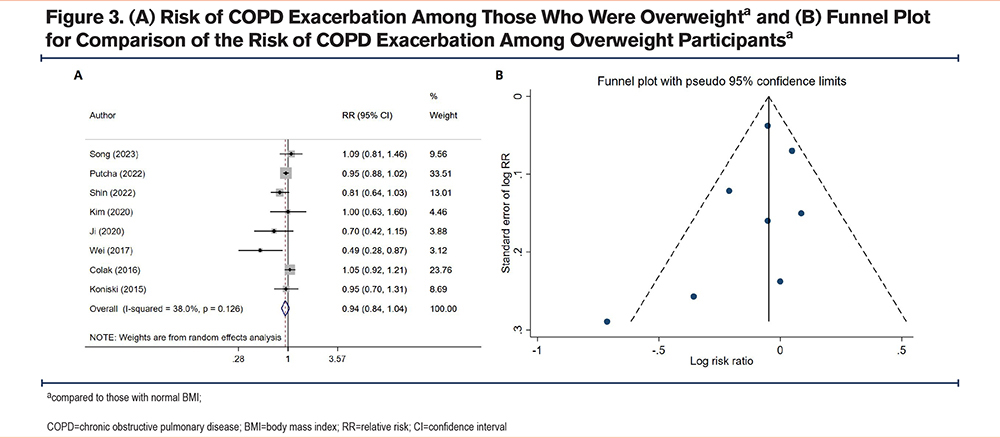
Risk of Exacerbation Among Overweight Participants
COPD patients with a normal BMI and overweight patients had similar risks of exacerbation (RR 0.94, 95% CI: 0.84, 1.04; N=8, I2=38.0%) (Figure 3A). There was no evidence of publication bias (Egger's test, p-value 0.30; Figure 3B). Sensitivity analysis after excluding the study by Putcha (2022) et al21 showed a similar risk of exacerbation (RR 0.91, 95% CI: 0.78, 1.07; N=7, I2=46.8%) in both groups (Supplementary Figure 3 in the online supplement). Additional analysis focusing on studies using similar BMI thresholds to classify “overweight” (i.e., BMI cutoff of 25 to <30 kg/m2) revealed a comparable risk of exacerbation between overweight and normal-weight individuals (RR 0.97, 95% CI: 0.91, 1.03; N=4, I2=0.0%) (Supplementary Figure 4 in the online supplement).
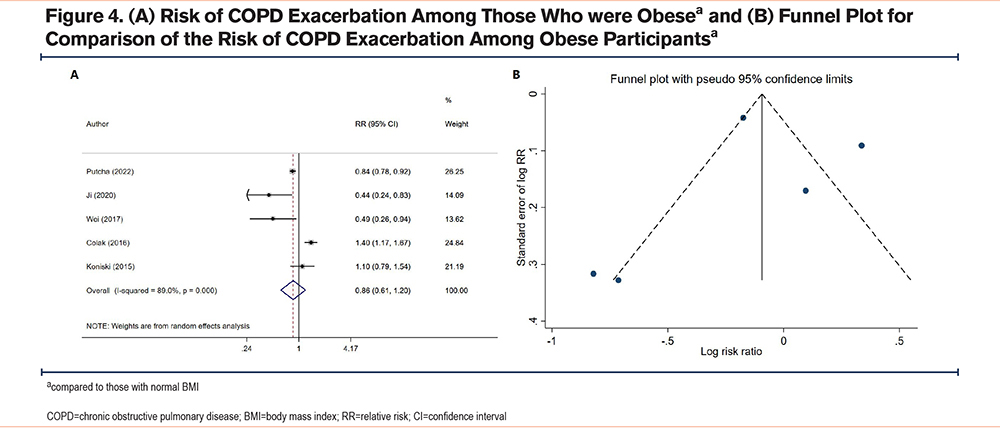
Risk of Exacerbation Among Obese Participants
Similarly to overweight patients, obese individuals had a similar risk of exacerbation (RR 0.86, 95% CI: 0.61, 1.20; N=5, I2=89.0%) compared to patients with a normal BMI (Figure 4A). No evidence of publication bias was found (Egger’s p-value of 0.96; Figure 4B). Sensitivity analysis after excluding the study by Putcha (2022) et al21 showed a similar risk of exacerbation (RR 0.82, 95% CI: 0.50, 1.36; N=4, I2=85.4%) in obese and normal-BMI patients (Supplementary Figure 5 in the online supplement). There were variations in obesity definitions across studies. Additional analysis that focused on studies using a BMI threshold of 30 kg/m2 or higher was conducted. A pooled analysis of 4 studies that met this criterion showed comparable risk of exacerbation in obese and normal-weight individuals (RR 0.94, 95% CI: 0.65, 1.34; N=4, I2=90.8%) (Supplementary Figure 6 in the online supplement).
Findings From Studies Not Included in the Quantitative Synthesis
A study by Smulders et al25 (2020) that included 604 COPD patients with a 5-year follow-up period, found that the average yearly rate of hospital admissions for exacerbation was 1.83 ± 1.60 per year among those with a normal BMI. Notably, exacerbation frequency showed annual decline in the overweight (1.60 ± 1.41), obese (1.20 ± 1.18), and severely obese group (1.09 ± 1.13). On the other hand, the underweight group did not show any significant difference in the frequency of exacerbation.25
Another study by Wu et al26 (2018), conducted among 744 patients, found that the yearly frequency of total exacerbations (median [interquartile range (IQR)]) was notably higher in the underweight group (1.85 [0.70 to 2.40]) compared to the normal (0.70 [0.30 to 1.00]), overweight (0.70 [0.30 to 2.00]), and obese (0.70 [0.30 to 1.85]) groups. This difference was significant26 (p= 0.03). In a small study of 41 patients, Hallin et al30 (2006) found that overweight patients were less likely to have an exacerbation (p=0.07) compared to underweight or normal-BMI COPD patients.
Discussion
This study showed that in COPD patients, underweight BMI status was associated with an elevated risk of exacerbation. In contrast, normal-BMI, overweight, and obese patients had comparable risks of COPD exacerbation. This observation prompts a critical examination of potential reasons for the increased exacerbation risk in underweight individuals, and the contrasting lack of such association in patients with a higher BMI. One plausible explanation for the increased risk in underweight individuals may be linked to compromised respiratory and immune functions. Underweight patients may have reduced respiratory muscle strength and diminished immune responses, making them more susceptible to respiratory infections and exacerbation.31-33 Malnutrition and a lower BMI might contribute to overall frailty, impacting the ability to cope with exacerbating factors in COPD.34,35
Conversely, the lack of a significant association between exacerbation risk and high BMI raises questions about the complex interplay between BMI and COPD outcomes. Previous reviews have indicated higher mortality rates in underweight patients and lower mortality rates in overweight and obese patients.11,12 We may speculate that in the case of underweight patients, there may be a potential immortal person time bias that can affect the estimates: increased risk of mortality in these patients results in a lower overall number of survivors who may experience exacerbations. This dynamic may influence risk estimates observed within the underweight group. For patients with a high BMI, the observed protective effects in terms of mortality rates may be influenced by improved nutritional reserves, which may indirectly translate into protection against potential triggers and mechanisms involved in exacerbations. Inflammatory processes and respiratory infections often prompt COPD exacerbations. A pro-inflammatory state, associated with a high BMI, might counterbalance any potential protective effects.4,36-38 Additionally, the mechanical effects of excess body weight, such as altered respiratory mechanics, may not confer protection against exacerbations.39,40 Patient characteristics, environmental factors, and behavioral aspects could further contribute to the nuanced associations between BMI and COPD outcomes. The complex interplay of inflammatory, respiratory, and environmental factors might contribute to the differential associations between BMI and various aspects of COPD morbidity and mortality, necessitating further research for a comprehensive understanding.
Our review has some limitations. One notable challenge is the inherent heterogeneity across the studies, encompassing variations in study design, participant characteristics, and outcome measures. Such diversity may affect the generalizability of the findings. The variability in BMI category definitions among studies poses another limitation that may impact the consistency of our results. Moreover, the retrospective nature of many included studies could have introduced the risk of recall bias. Finally, temporal considerations, such as changes in BMI over time, were not addressed in our review.
Our study findings provide valuable directions for future research. Mechanistic studies exploring the intricate pathways linking BMI to exacerbation risk are imperative to deepen our understanding of this association. Future studies should investigate adipose tissue distribution, systemic inflammation, and their interplay with respiratory function. Personalized medicine approaches should be explored, and tailored interventions based on individual BMI and other patient-specific factors should be examined to optimize COPD management. Longitudinal studies with extended follow-up periods are also needed to better capture the dynamic relationship between BMI and exacerbation risks over time. Further research should also investigate the interactions between BMI and the environmental or behavioral factors that may impact the risk of exacerbation. Clinical trials assessing the impact of weight management interventions on exacerbation rates are needed. Furthermore, new risk prediction models that incorporate BMI as one of the important components are needed. Overall, our findings pave the way for a comprehensive and multidimensional approach in research and clinical practice, offering opportunities for tailored interventions and improved outcomes in COPD patients across diverse BMI categories.
Conclusion
This review found an increased risk of COPD exacerbation in underweight patients. However, no such association was found in overweight or obese patients compared to patients with a normal BMI. The differential association between BMI categories and COPD exacerbation risk emphasizes the need for a nuanced understanding of the underlying pathophysiological mechanisms. Further research into the complex interplay between BMI, inflammation, and COPD outcomes may contribute to developing new personalized interventions and improved management strategies in this patient population.
Acknowledgements
Author contributions: MW and FY were responsible for the conception and design of the work. All 3 authors were responsible for the acquisition of the data, data analysis, and interpretation. MW was responsible for writing the manuscript and FY was responsible for substantial involvement in its revision prior to submission. In addition, all authors have read and approved the manuscript.
Declaration of Interests
The authors have nothing to declare.