Running Head: Rural-Urban COPD Disparities in COVID-19 Era
Funding Support: This research was supported by the National Institutes of Health’s National Heart, Lung, and Blood Institute grant T32 HL007741-23 (CR) and the National Center for Advancing Translational Sciences’ grants KL2TR002492 and UL1TR002494 (AKB). This material is the result of work supported with resources and the use of facilities at the Minneapolis VA Health Care System.
Date of Acceptance: August 19, 2024 | Publication Online Date: August 29, 2024
Abbreviations: AECOPD=acute exacerbation of COPD; BHLS=Brief Health Literacy Screening tool, CAT=COPD Assessment Test; COPD=chronic obstructive pulmonary disease; ED=emergency department; FEV1=forced expiratory volume in 1 second; FVC=forced vital capacity; PHQ-4=Patient Health Questionnaire 4; PSS=Perceived Stress Scale 4; RUCA=rural-urban community Area; SD=standard deviation; VA=Veterans Affairs
Citation: Robichaux C, Zanotto A, Wendt CH, Michalik M, Gravely A, Baldomero AK. Rural versus urban health disparities in the COVID-19 era among veterans with COPD. Chronic Obstr Pulm Dis. 2024; 11(5): 538-543. doi: http://doi.org/10.15326/jcopdf.2024.0521
Introduction
Prior to COVID-19, chronic obstructive pulmonary disease (COPD) was the fourth leading cause of death in the United States and continues to affect people living in rural areas disproportionately.1 Rural counties have a higher prevalence of COPD, more COPD-related hospitalizations, and more deaths than urban counties.1 Veterans are an important population in which to study rural disparities in COPD since they are twice as likely to suffer from COPD compared to the general U.S. population and more than 30% of Veterans Affairs (VA) patients reside in rural areas.2 The health of rural Veterans with COPD has not been assessed during the COVID-19 pandemic. Knowledge of how this high-risk population experienced the COVID-19 pandemic is important for future outbreaks and for understanding social factors that affect this group in relation to other infectious respiratory illnesses.
Individuals living in rural areas in the United States experienced disparities in COVID-19 incidence and mortality rates.3 The fourth wave of COVID-19 in the United States (June 2021 to March 2022) was the first wave with widespread access to vaccines across the United States, yet individuals in rural areas were more likely to be unvaccinated.4 Additionally, access to care may have been limited by a lack of access to broadband services and closures of health care systems in rural areas.5,6 Rural residents were less likely than urban residents to engage in prevention behaviors like masking, social distancing, and vaccination, but it is unclear if this was true for veterans with COPD.7
We sought to determine whether veterans with COPD living in rural areas experienced different perceptions and practices of COVID-19 mitigation strategies, access to care, and health disparities during the COVID-19 pandemic, compared to their urban-living counterparts.
Methods
Study Design
We performed a one-time telephone survey of rural and urban veterans with COPD between March 2021 and February 2022. We collected COVID-19−related information including individual perceptions and practice of mitigation strategies, COVID-19 vaccination status, access to care, and respiratory symptoms stratified by rural-urban status. We assessed these outcomes between March 2020 and March 2021. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology reporting guidelines for cross-sectional studies.8
Participants
We identified veterans with COPD using the Minneapolis VA Spirometry Registry. We included veterans aged ≥40 years with spirometry-confirmed COPD (defined as forced expiratory volume in 1 second [FEV1] to forced vital capacity [FVC] ratio of <0.7). Because the majority of the obtained spirometry was prebronchodilator, we opted to use prebronchodilator spirometry measures for consistency. Potential participants were sent a letter explaining the study and an option to opt out of the survey. We offered $10 for completing the survey. Those who did not opt out were called by a study personnel to complete the survey. Each participant’s rural-urban status was determined using home address zip codes to assign a rural-urban commuting area (RUCA) code from 1-10, with RUCA code 1 as urban and RUCA codes 2-10 as rural.9 Patients living in rural areas typically receive their primary care at satellite clinics associated with the Minneapolis VA that are situated in those rural regions. These clinics generally lack subspecialty care and services. In contrast, urban patients usually receive their care at the main Minneapolis VA facility, where both primary and extensive subspecialty services are readily available.
Data Collection Methods, Study Preparation, and Survey Administration
The survey consisted of 93 questions. We used validated health survey scales including the Brief Health Literacy Screening (BHLS) tool,10 COPD Assessment Test (CAT),11 Patient Health Questionnaire (PHQ)-4,12 and Perceived Stress Scale (PSS)-4.13 Nonvalidated questions were modeled from other COVID-19 publications and contained open-ended, Likert scale, and binary questions.
Our outcomes were divided into 4 categories. First, we assessed confidence in mitigation strategies (safety of vaccines and perception of the effectiveness of wearing a face mask, hand washing, avoiding sick contacts, and social distancing) and second, the likelihood of practicing mitigation strategies and receipt of COVID-19 vaccination. The third category was access to care including questions on difficulty making an appointment, canceled appointments, and receiving medications via mail delivery. Lastly, we evaluated health outcomes including COVID-19 diagnosis, COPD exacerbation, health care visits for respiratory symptoms, number of acute exacerbations of COPD (AECOPD) requiring an emergency department visit or hospital admission, CAT, PSS-4, and PHQ-4. Outcomes were assessed between March 2020 to March 2021.
Statistical Analysis
We compared survey results by rural versus urban status. We estimated that a total sample of 80 participants would provide 80% power to detect a 30% difference, assuming a 2-sided alpha of 0.05. We used Pearson’s Chi-square test and independent t-text for categorical and normally distributed continuous variables, respectively; we used a nonparametric independent t-test equivalent for continuous measures that were not normally distributed.
Study Oversight
This study was reviewed and deemed exempt by the Minneapolis VA Health Care System Institutional Review Board (VAM-20-00653) due to its minimal risk to participants.
Results
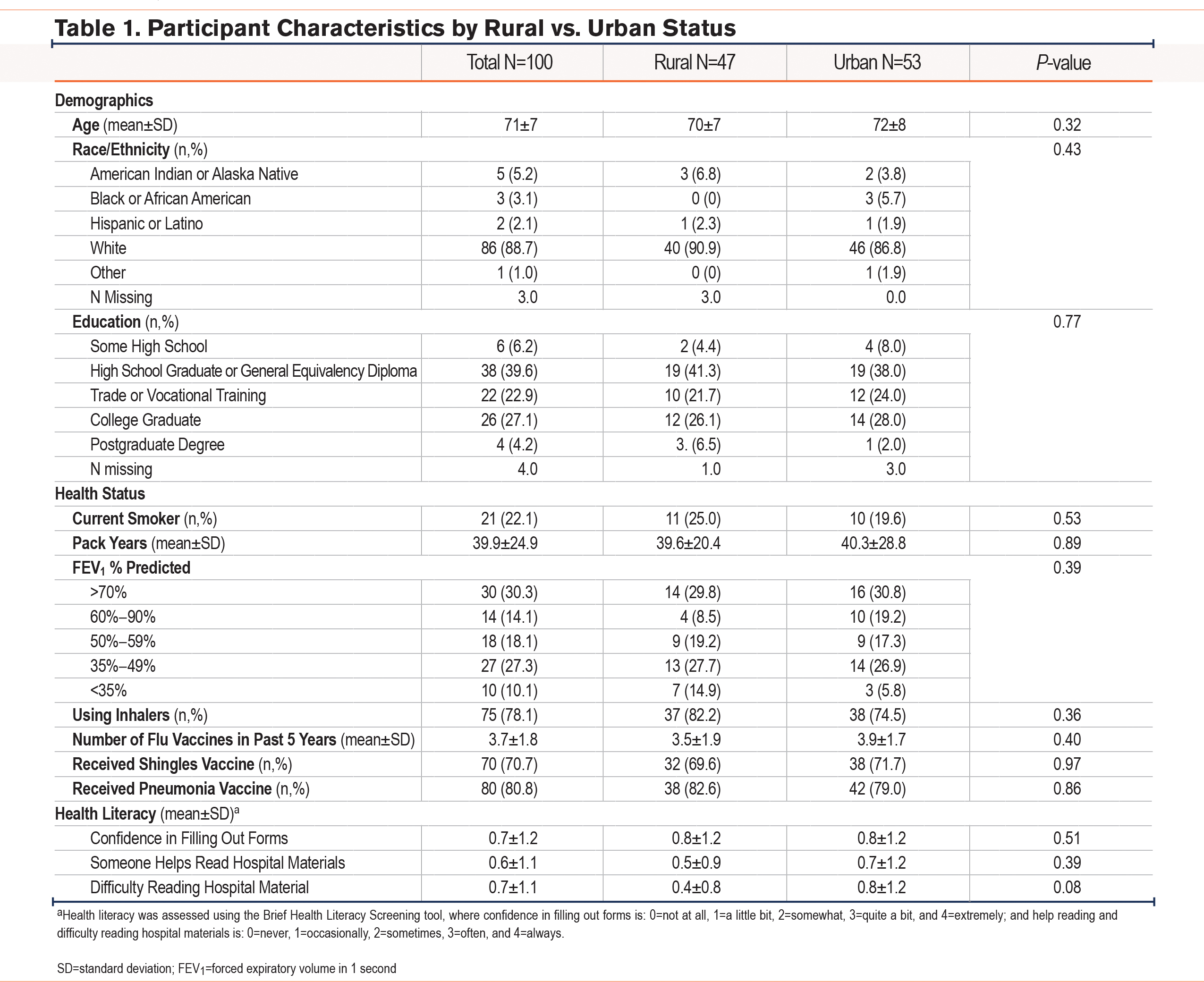
Surveys were sent to 234 patients and 100 patients responded (42.7% response rate). Of the 100 participants who completed the survey, 47 lived in a rural area (Table 1). The mean age was 71±7 years and 88.7% were of White race/ethnicity. Forty percent reported graduating from high school or obtaining a General Equivalency Diploma, 22.9% had trade or vocational training, and 31.3% graduated from college or received postgraduate degrees. The average number of flu vaccines received in the past 5 years was 3.7. The confidence in filling out forms was consistent with “inadequate or marginal health literacy” but difficulty reading hospital materials and frequency of having someone help with reading hospital materials were not consistent with low health literacy. Overall, there was no significant difference in participant characteristics between rural and urban veterans.
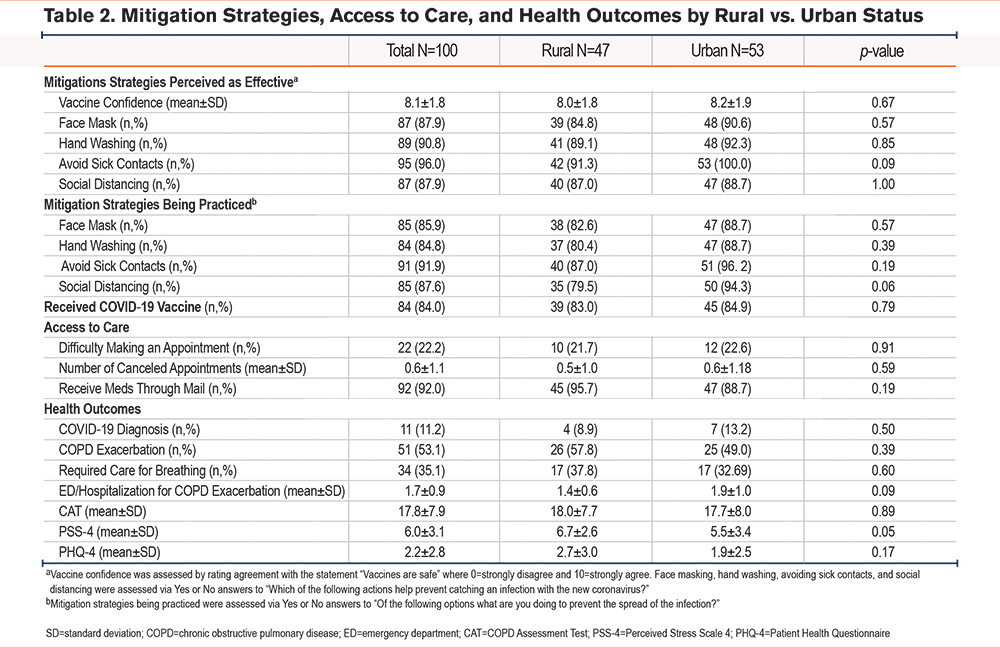
There were no significant differences in perceptions and practices related to COVID-19 mitigation strategies which included vaccine confidence, wearing of face masks, hand washing, avoiding sick contacts, and social distancing between veterans with COPD living in a rural versus urban area (Table 2). Eighty-four patients received COVID-19 vaccination; there was no significant difference in COVID-19 vaccination rates between rural and urban veterans with COPD. Similarly, there was no significant difference in challenges in accessing care, such as making clinic appointments, canceled appointments, and receiving medications through mail delivery. Additionally, there were no significant differences in health outcomes including COVID-19 diagnoses (9% versus 13%), COPD exacerbations in the preceding 6 months (58% versus 49%), CAT scores (18 versus 17), PSS-4 scores (7 versus 5), and PHQ-4 scores (3 versus 2) between rural versus urban veterans with COPD.
Discussion
Rural veterans with COPD experienced no difference from their urban-living counterparts in perceptions or practices of COVID-19 mitigation strategies, access to care, or respiratory outcomes.
This cohort is unique and differs from prior studies of urban-rural disparities in COVID-19 as all participants are veterans with COPD. VA health system attributes such as a long history of providing telemedicine, a mail-based outpatient pharmacy, and a single-payer system may help explain these findings.14 The benefits of these factors were manifested in the relatively low rates of difficulty accessing medical care reported in this survey. People with COPD and other chronic respiratory diseases may have been more likely than the general population to adopt protective behaviors. By the end of our study period in March 2021, 64% of Minnesota state residents who were 65 and older had received at least one dose of the COVID-19 vaccine, compared to 84% in our veteran COPD cohort, further supporting greater access to and motivation for preventative care in this group of patients with underlying lung disease.15 At the end of 2022, the Minnesota Department of Health data showed marked disparities in COVID-19 vaccination rates between urban and rural residents, so the lack of disparities in our cohort cannot be explained solely by regional or state-specific factors.15
The strengths of our study are its broad assessment of health, including physical, mental, and respiratory health. This survey was easy to complete for participants (a one-time survey without the chance for loss to follow-up). The timing of survey administration during the fourth wave of the COVID-19 pandemic, a particularly lethal wave during which the vast majority of the U.S. population had access to vaccines, provided important information on vaccine acceptance. Our limitations include a modest sample size, a single-center setting, and a high percentage of White and male participants, as this is a veteran population. Additionally, this one-time interview may not comprehensively represent individual practices and viewpoints that may have fluctuated during the pandemic.
In conclusion, rural living veterans with COPD had similar mitigation practices, access to care, and health outcomes as their urban living counterparts.
Acknowledgements
Author contributions: CR, AZ, CHW, and AKB conceived the current analysis. CR, AZ, CHW, and AKB designed the analysis. CHW obtained funding. AZ and MM acquired the data. AG performed the primary statistical analysis. CR and AZ drafted the manuscript. All authors provided critical input, revised the manuscript for important intellectual content, and approved the final manuscript. All authors take responsibility for the integrity of the data and the accuracy of the data analysis.
Disclaimer: The views expressed in this article are those of the authors and do not reflect the views of the United States Government, the Department of Veterans Affairs, the National Institutes of Health, the National Institutes of Health’s National Center for Advancing Translational Sciences, or any of the authors’ affiliated academic institutions.
Declaration of Interests
All authors declare that they have no conflict of interests related to this study.