Running Head: Impact of COVID-19 Vaccine Among COPD Individuals
Funding Support: This study was funded by the National Institutes of Health (NIH), National Heart, Lung, and Blood Institute (NHLBI) U01HL128951, and the American Lung Association.
Date of Acceptance: August 6, 2024 | Publication Online Date: August 12, 2024
Abbreviations: CAT=COPD assessment test; CDC=Centers for Disease Control and Prevention; CI=confidence interval; COPD=chronic obstructive pulmonary disease; FDA=Food and Drug Administration; FEV1=forced expiratory volume in 1 second; FEV1%pred=forced expiratory volume in 1 second percentage predicted; GAD-7=generalized anxiety disorder; GEE=generalized estimating equation; IQR=interquartile range; LEEP=Losartan Effects on Emphysema Progression; MCID=minimal clinically important difference; NIH=National Institutes of Health; NIH-IS=National Institutes of Health Toolbox Items Bank v2.0 – Instrumental Support; OR=odds ratio; PHQ-8=Patient Health Questionnaire; PROMIS-4A=Patient-Reported Measurement Information System Social Isolation Short Form 4a; WHO=World Health Organization
Citation: Fawzy A, Wang JG, Krings JG, et al. Impact of COVID-19 vaccine rollout on mental health, social determinants of health, and attitudes among individuals with COPD. Chronic Obstr Pulm Dis. 2024; 11(5): 496-506. doi: http://doi.org/10.15326/jcopdf.2024.0537
Online Supplemental Material: Read Online Supplemental Material (340KB)
Introduction
The COVID-19 global pandemic, which was confirmed1 to have spread to the United States in January 2020, disproportionately affected individuals suffering from chronic diseases.2 Chronic medical conditions, including chronic respiratory disease, were quickly recognized as risk factors for poor outcomes after a COVID-19 infection.3 National guidance promoted voluntary social distancing, and 42 out of 56 U.S. states and territories issued mandatory stay-at-home orders4 from March to May 2020. These policies led to decreases in population movement, increased the amount of time people spent at home, and reduced viral transmission and fatalities.4-6 Increased prevalence of major depressive disorder and anxiety has been linked to reduced mobility during the pandemic.7 Likewise, studies have also reported increased social isolation during the early part of the COVID-19 pandemic when mitigation policies focused on social distancing and quarantine.8
The first highly effective vaccine against COVID-19 was granted emergency use authorization by the U.S. Food and Drug Administration (FDA) on December 11, 2020 but was initially only available to health care workers.9 Vaccine eligibility criteria varied by state or locality but individuals with chronic respiratory disease were among the first general population groups eligible for vaccination and all states expanded vaccine eligibility to all adults10 by mid-April 2021. COVID-19 vaccine availability has been associated with reduced social distancing and improvements in mental health symptoms among U.S. general population respondents to the Household Pulse Survey.11,12
Individuals suffering from chronic obstructive pulmonary disease (COPD) are a particularly vulnerable population. In addition to the increased risk of adverse clinical outcomes resulting from a COVID-19 infection, attempts to avoid exposure to COVID-19 and social distancing policies likely led to reduced access to health care and delay or avoidance of seeking medical care by individuals with COPD.13,14 Individuals with COPD have a higher baseline prevalence of depression, anxiety, and social isolation compared with the general population, and these factors have been associated with adverse clinical outcomes.15-19 Specifically, social isolation has been associated with a range of health problems including the prevalence of dementia, worse mental health, cardiovascular disease, and risk for hospital admission for respiratory disease among older adults.20,21 This study evaluated whether broad availability of vaccines against the COVID-19 virus was associated with a change in mental health symptoms, social determinants of health, and attitudes related to the COVID-19 pandemic. There is evidence from studies of general populations of spillover effects, where community vaccination rates improve individual mental health outcomes, although similar effects in patients with COPD are unknown.22 We hypothesized that the broad availability of highly effective vaccines targeting the COVID-19 virus would reduce anxiety, depression, and social isolation among individuals with COPD.
Methods
Participants
Individuals from 21 of 26 American Lung Association Airways Clinical Research Centers were recruited into an ancillary study of the Losartan Effects on Emphysema Progression (LEEP) clinical trial (ClinicalTrials.gov NCT02696564) with the aim of evaluating the impact of the COVID-19 pandemic on patients with COPD. LEEP was a randomized placebo-controlled clinical trial23 that did not show an effect of losartan on emphysema progression among current or former smokers ≥40 years of age with moderate-to-severe COPD (forced expiratory volume in 1 second [FEV1] to forced vital capacity ≤0.70 and FEV1 20%–80% of predicted), ≥10 pack years of smoking, and mild-moderate emphysema on high-resolution computed tomography recruited from May 2017 to January 2020 with follow-up completed in January 2021. As part of the ancillary study, COVID-19 infection status was ascertained using kits for collecting dried blood spot specimens mailed from the study sites to participants and analyzed for 2 immunoglobulin G antibodies to SARS-COV2, the spike protein and nucleocapsid protein at a commercial laboratory (ZRT Laboratory, Beaverton, Oregon).24
Data Collection
Individuals currently or previously enrolled in LEEP were recruited from May 2020 to November 2020 to participate in the ancillary study that started as bi-weekly telephone interviews conducted by trained study staff to ascertain COVID-19 status and was later reduced to monthly interviews. All interviews were conducted from May 2020 to September 2022 (Supplemental Figure 1 in the online supplement). Structured validated questionnaires were administered every 8 weeks evaluating respiratory symptoms (COPD Assessment Test [CAT]), generalized anxiety symptoms (Generalized Anxiety Disorder-7 [GAD-7], range: 0–21), and depressive symptoms (Patient Health Questionnaire [PHQ-8], range: 0–24). Clinically, GAD-7 and PHQ-8 scores ≥10 indicated clinically significant anxiety and depressive symptoms,25,26 and the reported minimal clinically important difference (MCID) for GAD-7 ranges from 1 to 4, whereas, for PHQ-8 the MCID is 3.7.27-29 Social isolation (Patient-Reported Outcomes Measurement Information System Social Isolation Short Form 4a [PROMIS-4a]) and instrumental support (National Institutes of Health Toolbox Items Bank v2.0 – Instrumental Support [NIH-IS]), 2 social determinants of health that have been associated with risk for poor health outcomes in older adults,20,30 were evaluated every 8 weeks during the initial part of the study then again at the exit interview. PROMIS-4a and NIH-IS scores are presented as population-normalized t-scores31,32 (U.S. population mean 50, standard deviation 10). In addition, participants were asked questions about their attitudes and actions related to the COVID-19 pandemic every 8 weeks. Interim results of the ancillary study have been previously reported.33
Data Analysis
For analysis, the ancillary study follow-up was divided into 3 periods defined by the availability of a vaccine targeting the COVID-19 virus. Emergency Use Authorization by the FDA was granted to the Pfizer–BioNTech and Moderna mRNA COVID-19 vaccines by mid-December 2020, but initial availability was limited. Accordingly, the prevaccine period was defined as May 2020 through December 2020. Since broad availability of the COVID-19 vaccine was achieved by April 2021 when every U.S. state expanded its eligibility criteria to all persons ≥16 years old,10 the postvaccine period was defined as May 2021 through September 2022. January 2021 through April 2021 was defined as the transition period and data collected during this time were not included in the longitudinal analyses.
Participant characteristics were summarized with medians and interquartile ranges (IQRs), or proportions. Data from all interviews including the transition period were evaluated to determine the rate of hospitalization, death, cumulative incidence of all-cause death or hospitalization, and COVID-19 infections during follow-up. For analysis of the structured questionnaires (CAT, PHQ-8, GAD-7, PROMIS-4a, and NIH-IS), maximum questionnaire scores for each participant were summarized for each vaccine period. Generalized estimating equation (GEE) models were performed to evaluate changes in patient-reported scores from the prevaccination to postvaccination periods; data from the transition period were not included. Respiratory, anxiety, and depressive symptoms were evaluated as dichotomous outcomes in the GEE models. Severe respiratory symptoms (CAT>20) were compared to moderate or mild symptoms34 (CAT<20). Anxiety and depressive symptoms were assessed using GAD-7 and PHQ-8, respectively, with moderate or greater symptom scores used as cut-offs for both25,26 (GAD-7≥10 versus GAD-7<10 and PHQ-8≥10 versus PHQ-8<10). Social Isolation PROMIS-4a and the NIH-IS scores were evaluated as continuous outcomes, albeit with fewer data points in the postvaccination period, using similar GEE models to evaluate changes from the pre- to postvaccine periods. A paired sample t-test was also used to compare maximum individual scores between pre- and postvaccine periods. A sensitivity analysis limited to participants who were interviewed during both the pre- and postvaccine periods was conducted.
The ancillary study was approved by each participating site’s local institutional review board and all participants provided informed consent. Data analysis was performed using SAS 9.4 (SAS Institute Inc., Cary, North Carolina) and R 4.3.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
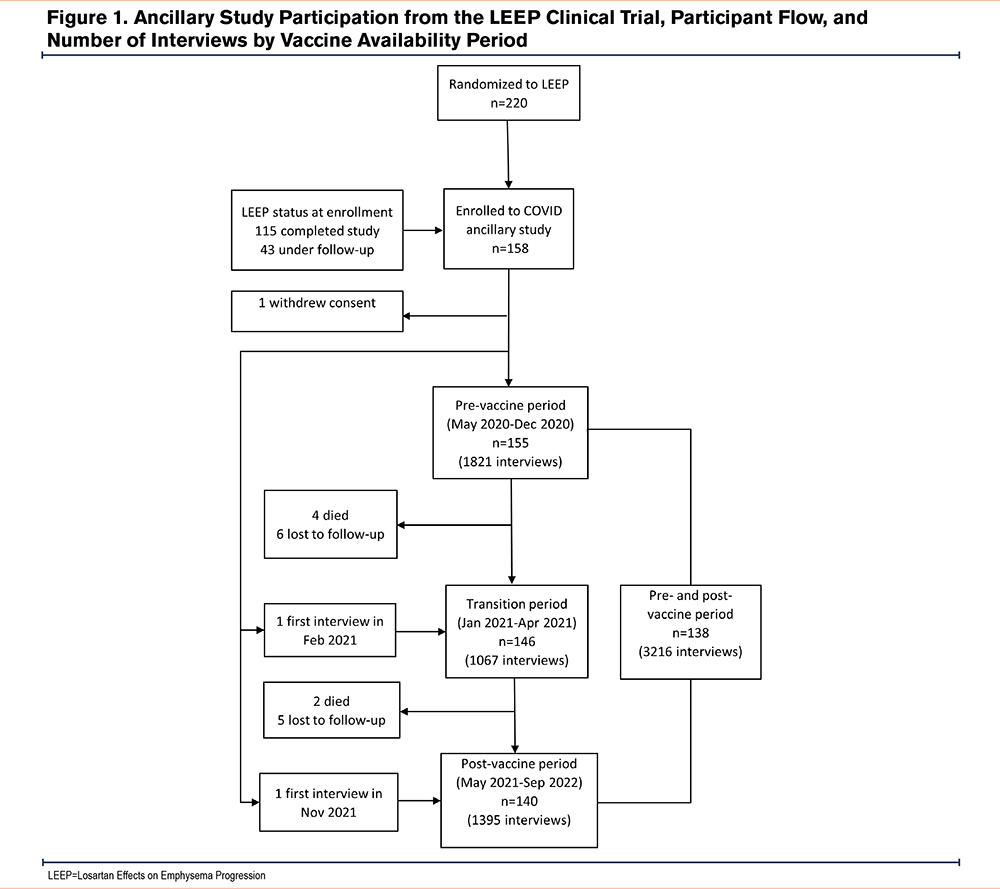
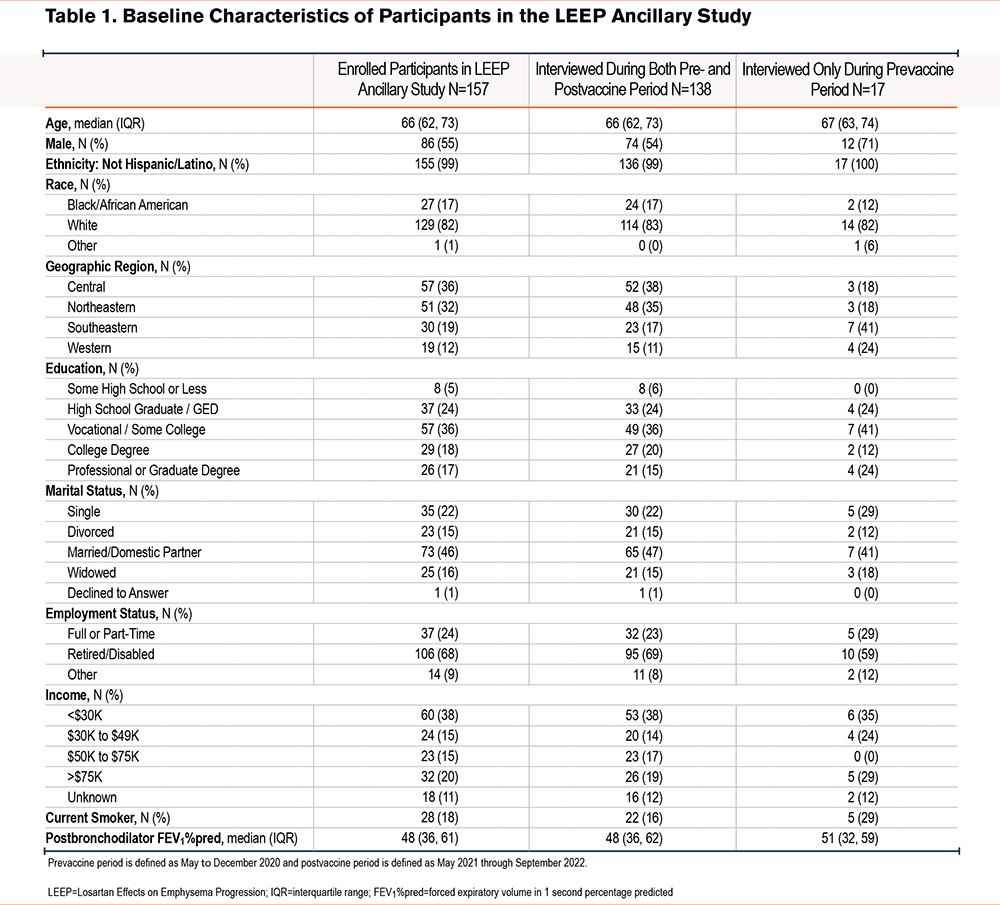
Of the 220 individuals randomized in LEEP, 157 were enrolled and contributed at least one interview to the ancillary study; 138 had follow-up during both the pre- and postvaccination periods (2154 interviews); 17 had only prevaccination interviews, and 2 only had postvaccination interviews available (Figure 1). Baseline characteristics are presented in Table 1 with a comparison of participants who were only interviewed during the prevaccination period to those who were interviewed during both periods. The median (IQR) age of the sample was 66 (62, 73) years; most self-identified as White, non-Hispanics, and just over half were male. Compared with individuals who were interviewed during both periods, those who only had prevaccination interviews were more commonly male and lived in the southeastern or western United States. Compared to enrollees in the ancillary study, individuals who did not participate were more likely to identify as Hispanic/Latino or Black/African American, hail from the western United States, not have graduated from high school, be single or divorced, have lower income, and be current smokers (Supplemental Table 1 in the online supplement). The median (IQR) follow-up time was 176 days (141, 209) in the prevaccine period and 332 days (318, 367) in the postvaccine period. Overall, there was a median (IQR) of 30 (22, 34) interviews per participant, with 31 (26, 35) among those interviewed during both periods and 10 (5, 13) for those who were only interviewed in the prevaccine period.
Receipt of a full series of the initial COVID-19 vaccine regimen (at least one dose adenovirus vector vaccine or at least 2 doses of mRNA vaccine) was reported by 75% of enrollees through September 2021 and 92% by the end of the study. In the prevaccine period, 5.8% of participants interviewed reported experiencing a COVID-19 infection (0.12 events per person-year) compared to 17.9% of participants in the postvaccine period (0.20 events per person-year). High self-reported vaccination rates and low clinical infection rates were consistent with the high rates of S1 spike antibody positivity (88%) and low rates of nucleocapsid positivity (9%) in the 113 participants with antibody testing results. The cumulative incidence of all-cause hospitalization across all follow-up was 34% (95% confidence interval [CI]: 16.8% to 47.6%; 0.25 event per person-year) and 6.3% (95%CI: 2.2% to 10.2%; 0.04 event per person-year) for deaths (Supplemental Figure 2 in the online supplement). Only 2 of the 60 reported hospitalizations and 1 of the 9 deaths were reported as related to COVID-19 infection.
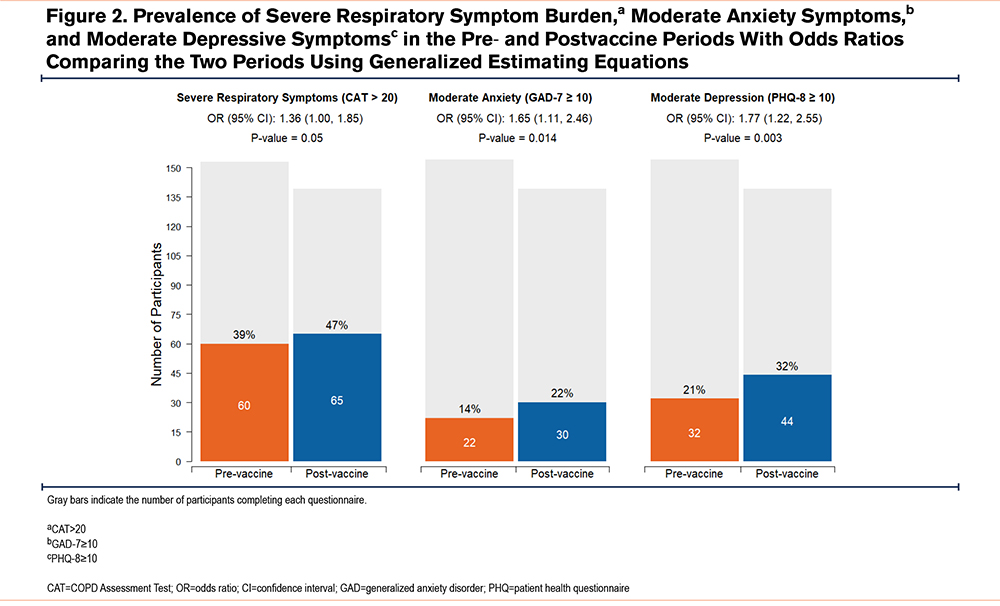
Respiratory and Mental Health
Respiratory symptom burden as assessed by maximum individual CAT score during each period increased nonsignificantly from the pre- to postvaccination periods (mean difference: 0.87±0.89, P=0.06). However, the odds of reporting severe symptom burden (CAT score > 20) were significantly higher in the postvaccination period (odds ratio [OR]: 1.36, 95% CI: 1.00 to 1.85, Figure 2). The prevalence of moderate anxiety symptoms (GAD-7≥10) and moderate depressive symptoms (PHQ-8≥10) increased by 8% and 11% respectively between the pre- and postvaccine periods (Figure 2), which was associated with statistically significant increases in the odds of reporting moderate anxiety symptoms (OR: 1.65, 95% CI: 1.11 to 2.46) and moderate depressive symptoms (OR: 1.77, 95% CI: 1.22 to 2.55) in the postvaccine period. Results were similar in a sensitivity analysis that limited the sample to participants who were interviewed during both periods (Supplemental Table 2 in the online supplement) and there were no differences based on personal vaccination status (Supplemental Tables 3 and 4 in the online supplement).
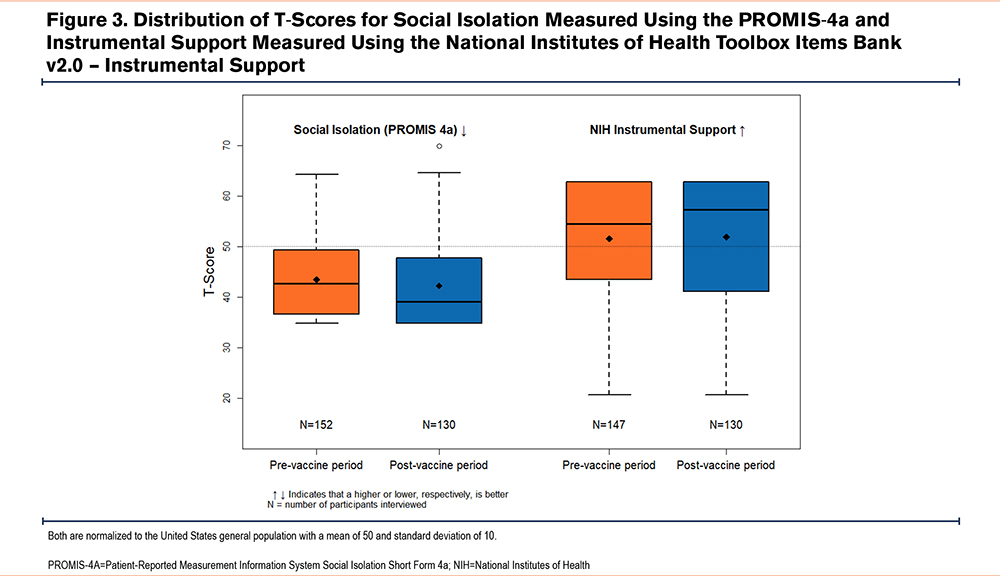
Social Determinants of Health
The average PROMIS-4a social isolation t-scores were 43.5±1.2 in the prevaccine period and 42.2±1.5 in the postvaccine period (Figure 3), which is less social isolation than the U.S. population mean (t-score=50) but within one standard deviation (SD=10). The t-score improved by an average of 1.25 points between the pre- and postvaccine periods, although this was not statistically significant (95% CI: -2.56 to 0.06, P=0.06). Conversely, instrumental support scores were close to the reference population mean (t-score= 50) during the prevaccine (51.6±1.8) and postvaccine (51.8±2.3) periods and did not significantly change (t-score mean difference of 0.28, 95% CI: 1.76 decrement to 2.33 improvement, P=0.79). Results were similar when limiting the sample to participants who were interviewed during both periods (Supplemental Table 2 in the online supplement) and there were no differences based on personal vaccination status (Supplemental Tables 3 and 4 in the online supplement).
COVID-19 Related Attitudes
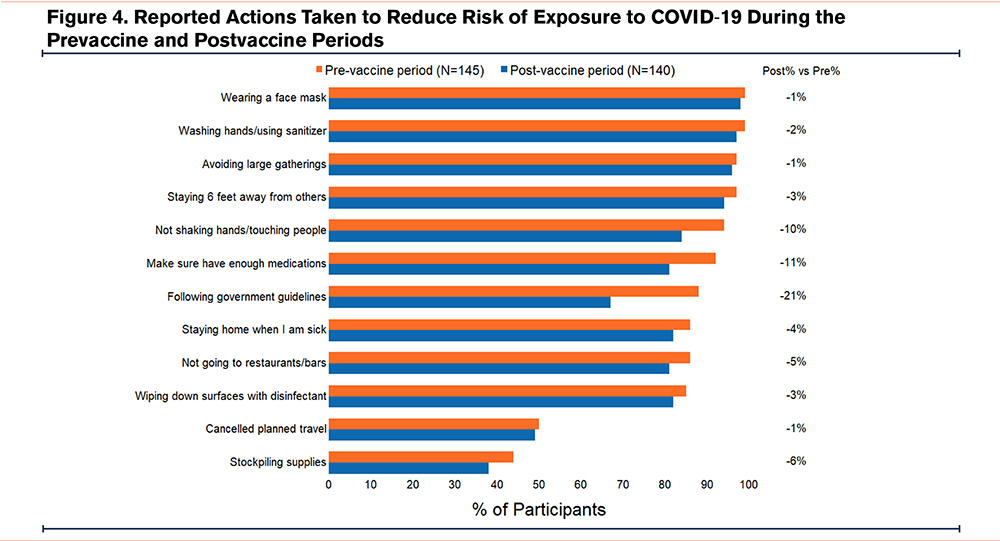
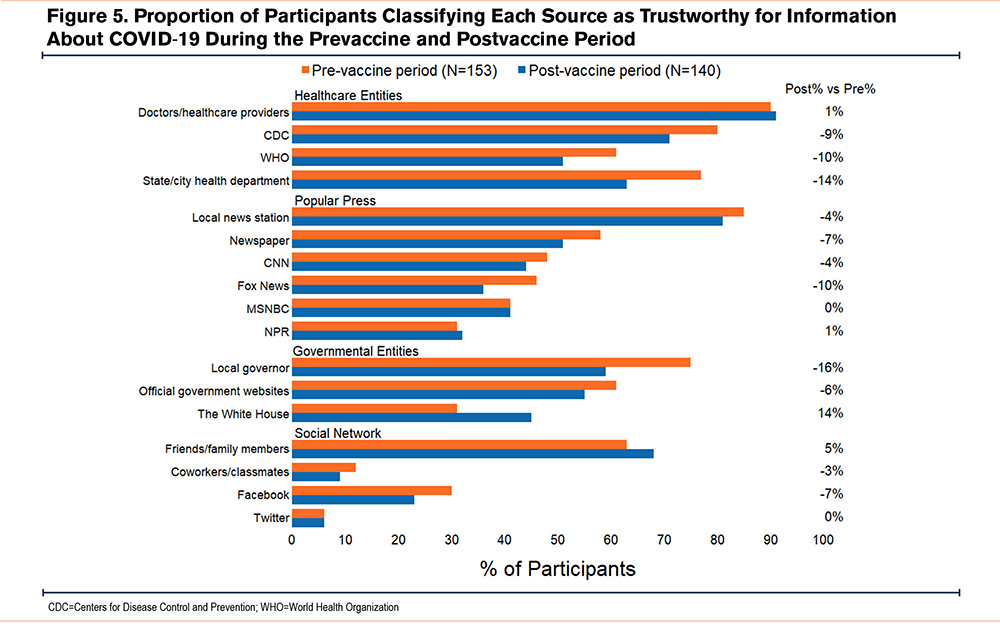
Compliance with personal actions meant to mitigate COVID-19 transmission was high and there remained a high prevalence of many actions such as wearing a face mask, hand washing/sanitizing, and avoiding large gatherings in the postvaccine period. Other practices such as avoiding shaking hands or touching people, making sure they had enough medications, and following government guidelines declined in prevalence by 10% to 20% from the pre- to postvaccine periods (Figure 4). Doctors or health care providers, other health care entities (Centers for Disease Control and Prevention, the World Health Organization, and local health departments), local news stations, local governors, official government websites, and friends or family members were identified as trustworthy by most respondents during the prevaccine period (Figure 5). While there was no change in the proportion of participants who viewed their doctor or health care provider as a trustworthy source of information between the pre- and postvaccine periods, the proportion of participants who considered certain press outlets (local news station, newspaper, CNN, Fox News) trustworthy declined by 4%–10%. Substantial declines in the proportion of participants who viewed governmental health care entities (-9% to -14%) and local governors (-16%) as trustworthy (Figure 5) paralleled the decline in following government guidelines (-21%). The trustworthiness of the White House improved the most, from 31% to 45% of respondents deeming it trustworthy between the pre- and postvaccine periods.
Discussion
Broad availability of COVID-19 vaccines decreased the degree of social isolation but did not improve anxiety or depressive symptoms, or instrumental support measures among clinical trial participants with COPD and high personal vaccine uptake. Contrary to our initial hypothesis, individuals reported significantly higher rates of anxiety and depressive symptoms in the postvaccine period of the COVID-19 pandemic compared to the prevaccine period. During this time, respiratory symptom burden worsened with a significant increase in the proportion of individuals reporting severe symptoms. The average change in the CAT score over the approximate 2-year period of this study is on par or slightly higher than the yearly change reported in another study with a substantially higher COPD exacerbation rate (13% in one year) than this study (5% over 2 years),35 but lower than in a sample of individuals with COPD living in a country with more stringent COVID-19 lockdown procedures (Germany).13
To mitigate viral spread and curb mortality in the early part of the COVID-19 pandemic, many U.S. states and municipalities implemented mandatory stay-at-home orders in addition to widespread public health messaging encouraging social distancing. This select group of individuals with COPD who joined a clinical trial had very high compliance with these mitigation efforts implying they were aware of their heightened risk for poor outcomes from a COVID-19 infection. Furthermore, individuals reported high levels of trust in health care entities that were disseminating messages about mitigation efforts. Despite waning trust in governmental health care entities after broad vaccine availability, individuals maintained a very high level of compliance with most efforts to mitigate COVID-19 transmission, such as avoiding large gatherings and maintaining social distance.
Although individuals with COPD tend to spend the majority of their time at home,36 social distancing measures likely compounded social isolation, as demonstrated by improvement in reported social isolation in this study following broad vaccine availability and concurrent relaxation of public health measures. Notably, though, the majority of individuals in this study, drawn from a clinical trial that enrolled prepandemic, experienced less social isolation than the U.S. population average. Despite decreased social isolation from the pre- to postvaccine period, the prevalence and odds of having moderate anxiety and depressive symptoms significantly increased, implying that mental health symptoms were related to factors other than social isolation. Importantly, the prevalence of severe respiratory symptoms also increased during the period when anxiety and depressive symptoms increased, and these factors are known to be strongly correlated in this population. With respect to social factors, studies during the COVID-19 pandemic have demonstrated that it is the feeling of loneliness rather than absence of social contact which was most strongly associated with adverse emotional health.37,38 Furthermore, the high prevalence (>80%) of compliance with social distancing measures throughout the study period may have led to increased physical isolation. During periods of physical isolation in the context of the COVID-19 pandemic, over half of individuals with nonmalignant severe respiratory disease (severe COPD and interstitial lung disease) reported reduced physical activity at home and two-thirds reported reduced physical activity outside the home.39 A persistent reduction in physical activity may explain the increased prevalence of anxiety, depressive, and severe respiratory symptoms in the latter part of the study, and participation in an inpatient pulmonary rehab program has been shown to improve levels of anxiety, depressive, and respiratory symptoms.40,41 However, progression of these symptoms is also part of the expected progression of COPD.
This study leveraged participants from an ongoing clinical trial that started before the COVID-19 pandemic to collect longitudinal information from socioeconomically diverse individuals in different regions of the United States, however, there are several limitations. The frequency and number of interviews conducted during the pre- and postvaccine periods were not consistent among participants and differences in demographic characteristics may have impacted the findings of this study. Furthermore, we were unable to account for the impact of differences in COVID-19 hospitalization and mortality rates between the pre- and post- vaccine periods unrelated to broad vaccine availability that may be related to seasonality or viral virulence. The generalizability of our results is limited by the small size and select population, with most of the study participants being White, married, and engaged with the health care system. The screening questionnaires used in this study may overestimate the prevalence of depressive and anxiety symptoms compared with more rigorous clinical assessment.42 Furthermore, the questionnaires about actions taken to reduce COVID-19 risk and trustworthiness of information sources were not validated and data on COVID-19 infections and vaccinations were self-reported. Finally, rather than considering the time of individual vaccination, the exposure in this study was the broad availability of the COVID-19 vaccine based on time periods corresponding to vaccine policies in the United States which may limit the application of this study’s findings.
In conclusion, individuals with moderate-severe COPD reported lower levels of social isolation after broad availability of COVID-19 vaccines in the United States but had higher levels of anxiety, depressive, and respiratory symptoms. The availability of highly efficacious vaccines against COVID-19 did not mitigate symptoms of anxiety and depression in this vulnerable population with high personal uptake of vaccination and risk-mitigating actions. This study’s findings imply that periods of prolonged social isolation may have a persistent deleterious impact on the physical and mental health of individuals with COPD that are not readily reversible, which may have applicability beyond the context of the pandemic.
Acknowledgments
Author contributions: AF, JGW, JK, JH, JTH, and RAW were involved in the conceptualization and methodology of this study. ME was also involved in the methodology of this study. JH and JTH performed data curation and formal data analysis. AF wrote the original draft of the manuscript. JGW, JGK, JH, OO, ME, JTH, and RAW all reviewed and edited the manuscript and approved the final version.
Declaration of Interest
AF and JGK have grants from the NIH’s NHLBI outside the submitted work. JGW and JGK received grant funding from the American Lung Association outside the submitted work. JGW also reports consulting fees from Sanofi/Regeneron and Genentech in the prior 36 months. JH, OO, MNE, JTH, and RAW have nothing to disclose.