Running Head: Childhood Cigarette Smoking and Risk of COPD
Funding Support: All phases of this study were supported by R21HL161758, National Institutes of Health (NIH). The findings reported herein do not necessarily represent the views of NIH.
Date of Acceptance: October 4, 2024 | Publication Online Date: October 11, 2024
Abbreviations: ARR=adjusted risk ratio; CI=confidence interval; COPD=chronic obstructive pulmonary disease; FEV1=forced expiratory volume in 1 second; NHIS=National Health Interview Survey; PATH=Population Assessment of Tobacco and Health; W=Wave
Citation: Ozga JE, Sargent JD, Steinberg AW, Tang Z, Stanton CA, Paulin LM. Childhood cigarette smoking and risk of COPD in older U.S. adults: a nationally representative replication study. Chronic Obstr Pulm Dis. 2024; 11(6): 549-557. doi: http://doi.org/10.15326/jcopdf.2024.0514
Online Supplemental Material: Read Online Supplemental Material (360KB)
Introduction
Although cigarette smoking prevalence in the United States has been declining1,2since the 1960s, it remains the leading cause of preventable death and disease in the United States, and it is the primary driver of chronic obstructive pulmonary disease (COPD).2 Today, most adults begin smoking cigarettes during adulthood1 (after age 25), and adolescent smoking (before 18 years) is relatively uncommon.3 However, in 2012, more than 80% of adults who smoked cigarettes reported smoking before 18 years of age, and 99% had initiated before 26 years old.4 Smoking initiation even earlier during adolescence (between 12–16 years of age) was highly prevalent before 1980, with current smoking among this age group reaching 25% at the time.5 Today, adults who initiated cigarette smoking as adolescents before 1980 would be at least 55 years old.
Lung growth and development extends through adolescence, with the majority of lung function developing between 10 and 20 years of age.6 Adolescent cigarette smoking has been associated with reduced forced expiratory volume in 1 second (FEV1) to forced vital capacity ratios and increased peripheral airway resistance among 16-year-olds.7 Some studies have reported that earlier ages of cigarette smoking initiation significantly increases COPD risk in later adulthood.8-12 However, these studies were all limited in that they were either restricted to samples of males only9,12 or failed to adjust for important smoke-related factors that could have confounded their findings, such as lifetime smoking (e.g., cigarette pack years or smoking duration),10,11 current smoking status,8,11 and smoking intensity.11 Indeed, adults who began smoking during childhood tend to have more pack years of cigarette exposure than those who began smoking in adulthood due to a combination of smoking more cigarettes per day and having a longer duration of smoking.8 In addition, none of the prior studies cited above accounted for secondhand smoke exposure,8-12 which has been associated with increased COPD risk independent of lifetime smoking for adults who currently smoke cigarettes.13
A recently published study of U.S. adults aged 40+ in the 2020 National Health Interview Survey (NHIS) aimed to address the limitations of prior studies by assessing the relationship between age of cigarette smoking initiation and COPD risk independent of current smoking status, pack years of smoking, smoking intensity, and smoking duration.14 That study found increased COPD risk for cigarette smoking initiation during childhood (<15 years of age) after controlling for these potential confounders. Although those who began smoking <15 years of age were at greatest risk for COPD, adults who began smoking between ages 15–19 were also at significantly increased risk for COPD14 compared to those who began smoking at or after age 20. That study also found that the higher risk of COPD for childhood smoking (<15 years of age) occurred at all smoking intensity levels for adults who currently smoked cigarettes. Together, findings are consistent with the window for known lung development, suggesting that early cigarette initiation may negatively influence this process and predispose individuals to future disease regardless of lifetime smoking, current smoking status, and smoking intensity. Still, a limitation of this recently published study is that NHIS does not include a measure for secondhand smoke exposure.
The current study aimed to expand upon results from the recently published NHIS study14 by additionally accounting for secondhand smoke exposure in multivariable models. Further, recognizing the importance of replication in drawing conclusions from observational studies,15 we examined a separate nationally representative dataset of adults in the United States, the Population Assessment of Tobacco and Health (PATH) study. Using the PATH study allowed us to replicate the results of the NHIS study in another nationally representative sample of older (aged 40+) U.S. adults and test whether the COPD-childhood smoking association is independent of lifetime smoking, current smoking status, smoking intensity, and secondhand smoke exposure. Similar to results from NHIS, we hypothesized that childhood cigarette smoking (i.e., <15 years of age) would be associated with increased COPD prevalence among older adults, independent of current cigarette smoking status, smoking intensity, pack years of smoking, smoking duration, and secondhand smoke exposure.
Method
Study Design and Sample
Data were selected from Wave (W) 5 of the PATH study, a national longitudinal cohort survey of U.S. youth and adults. Data were collected in respondents’ households using computer-assisted self-interviews administered in English or Spanish as appropriate. Survey data were collected from adults (aged 18+) in 2013–2014 (W1), 2014–2015 (W2), 2015–2016 (W3), 2016–2017 (W4), and 2018–2019 (W5). The current secondary data analysis used the W1–W5 Adult Restricted Use Files16 and was limited to adults aged 40+ years at W5 (N=10,126). This study qualified as exempt per guidelines of the Westat Institutional Review Board and the Dartmouth Health Human Research Protection Program.
Measures
COPD Prevalence
At W1, participants were asked, “Has a doctor, nurse, or other health professional EVER told you that you had any of the following lung or respiratory conditions? Choose all that apply: COPD, chronic bronchitis, emphysema, asthma, some other lung or respiratory condition, none of the above, don’t know, refused.” At W2–W5, participants who had not reported respiratory disease at prior waves were asked about new respiratory disease diagnoses from the past 12 months. Any COPD, chronic bronchitis, and emphysema diagnoses across W1–W5 were combined to create one COPD composite prevalence measure17,18(yes/no) at W5.
Childhood Cigarette Smoking
The primary exposure of interest was childhood cigarette smoking. Adult respondents who reported ever cigarette smoking, defined as smoking at least 100 cigarettes in their lifetime, were asked, “How old were you when you first started smoking cigarettes fairly regularly?” Responses were used to create 2 separate variables: one with 3 categories, which included adults who never smoked, those who began smoking before age 15 (childhood smoking), and those who began smoking after age 15; and one with 4 categories, which included adults who never smoked, those who began smoking before age 15, those who began smoking between 15–19 years of age, and those who began smoking at or after age 20. For the NHIS study, categories were created based on a lowess curve showing an inflection point between age of cigarette smoking initiation and COPD prevalence occurring between 15 and 20 years of age; the lowess curve for the current dataset (Supplemental Figure 1 in the online supplement) is almost identical to the one derived from the NHIS data.14
Cigarette Smoking Covariates
W5 smoke-related covariates included cigarette smoking status, pack years of cigarette smoking, secondhand smoke exposure, and number of cigarettes smoked per day. We used the PATH study-derived variables for never, current established, and former established cigarette smoking to create a 3-category smoking status variable capturing never, former, or current smoking. Pack years were determined by first calculating the duration of cigarette smoking (in years) for respondents reporting current or former smoking and then multiplying the duration of smoking by cigarette packs smoked per day19 (cigarettes smoked per day divided by 20). Pack years were winsorized by reassigning values from the 99th percentile to the top and bottom 1% of values to reduce undue influence of outliers.20 Secondhand smoke exposure was included as a continuous measure based on responses to the question, “In the past 7 days, number of hours that you were in close contact with others when they were smoking?”21
Cigarettes smoked per day were coded into 3 categories: <10 (light intensity), 11–19 (medium intensity), and 20+ (heavy intensity). Using the 3-category variable for age of cigarette smoking initiation, smoking status, and smoking intensity, we created a 9-category variable that stratified childhood smoking by cigarette smoking status and smoking intensity: never smoking, former smoking <15, former smoking 15+, current light smoking <15, current medium smoking <15, current heavy smoking <15, current light smoking 15+, current medium smoking 15+, and current heavy smoking 15+.
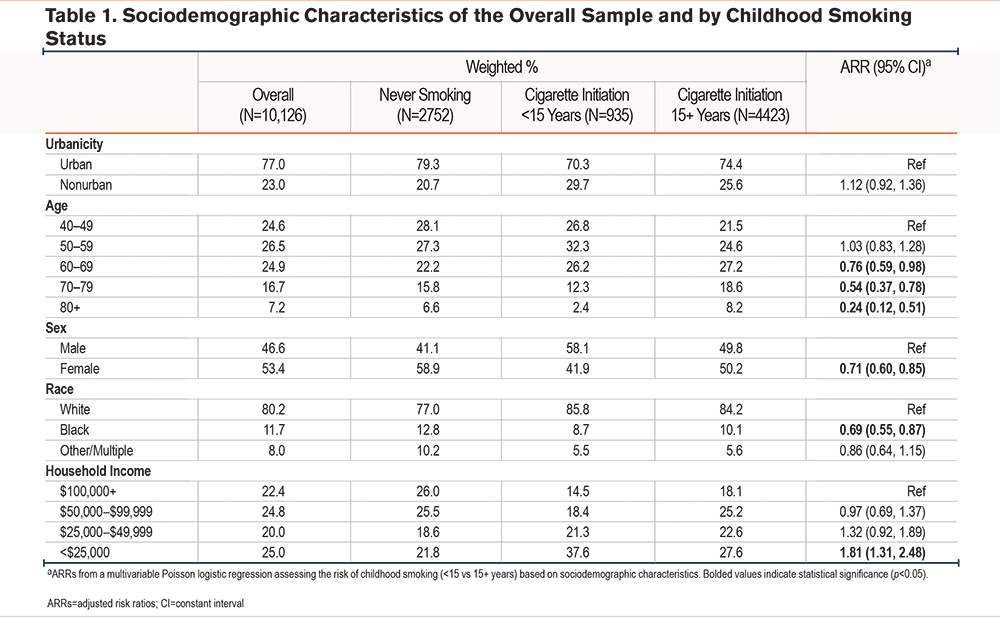
Sociodemographic Covariates
Sociodemographic covariates were categorized as shown in Table 1. From W5, these included age, sex, race, and total household income in the past 12 months. Missing data on age, sex, and race were imputed as described in the PATH study Restricted Use Files User Guide.16 Urbanicity, which was only available at W1, was also included as a covariate. Respondents’ geographic locations were categorized as “urban” if the majority of the sampling area’s total population resides in areas classified as urban according to the 2010 U.S. Census and “not urban” otherwise.16
Statistical Analysis
Weighted descriptives and multivariable Poisson regression were used to evaluate associations between sociodemographic characteristics and risk of childhood smoking. Then, weighted descriptive statistics and multivariable Poisson logistic regressions were used to evaluate associations between childhood smoking and COPD prevalence. Unadjusted models and models adjusted for age, sex, race, household income, cigarette pack years, smoking status, and secondhand smoke exposure were examined to estimate risk ratios and adjusted risk ratios (ARRs). The primary analysis included the 3-category age of initiation variable with 15+ as the reference category. A secondary analysis included the 4-category age of initiation variable with 20+ as the reference category. A third analysis included the 9-category variable that stratified the 3-category age of cigarette smoking initiation by smoking status and intensity. Within each smoking status/intensity category, aRRs were compared across ages of cigarette smoking initiation (e.g., <15 was compared to 15+ among adults reporting current light smoking) to delineate how childhood smoking relates to COPD prevalence while accounting for differences in smoking status and current smoking intensity. All analyses were weighted using the W5 all-waves survey weights, which included full sample and 100 replicate weights, to produce nationally representative estimates. Variances were computed using the balanced repeated replication method with Fay’s adjustment set to 0.3. All analyses were conducted using State/MP 17.0 (StataCorp LLC, College Station, Texas).
Sensitivity Analyses
Based on prior work suggesting that smoking duration alone may be a stronger predictor of COPD than pack-year exposure,22 we performed a sensitivity analysis that substituted smoking duration for pack years. This was done first by including smoking duration as a continuous measure, replicating the NHIS study.14 However, lowess curves (Supplemental Figure 2 in the online supplement) showed a stronger relationship between smoking duration and COPD prevalence for adults smoking 25+ years (versus <25 years), so we created a dichotomous smoking duration variable (smoking <25 years versus 25+ years) in a subsequent analysis.
To explore the potential that adults who initiated smoking <15 years under-report their cigarette use, leading to biased pack years estimates, we systematically increased cigarette pack years in 5% increments for those who initiated smoking <15 years in a series of multivariable Poisson regression models.
Results
Sample Characteristics and Childhood Smoking
Table 1 shows sociodemographic characteristics overall and by childhood smoking status. Overall, participants were largely from urban areas (77.0%), female (53.4%), and of White race (80.2%). There was a relatively even distribution of respondents across total household income levels and age categories, though there were fewer adults aged 70+ compared to adults aged 40–69. We found that Black/African American (versus White) adults (aRR=0.69; 95% confidence interval [CI]=0.55, 0.87), females (aRR=0.71; 95% CI=0.60, 0.85), and older participants (aged 60+ versus 40–49) were at significantly lower risk for childhood smoking, whereas participants reporting a household income of <$25,000 (versus $100,000+) were at significantly higher risk for childhood smoking (aRR=1.81; 95% CI=1.31, 2.48).
Associations Between Childhood Smoking and COPD Prevalence
Table 2 shows COPD and smoking-related characteristics overall and as a function of childhood smoking status. The overall weighted prevalence of COPD was 13.4%, with 7.5% of adults who never smoked, 29.0% of adults who initiated during childhood (<15 years), and 21.1% of adults who initiated 15+ years reporting a COPD diagnosis. Bivariate tests comparing respondents who initiated cigarette smoking at <15 years versus 15+ years showed higher prevalence of COPD, higher prevalence of current smoking, longer smoking duration, and greater cigarette pack years for respondents who had initiated during childhood (p’s<0.05). Those who initiated during childhood also had a lower prevalence of former smoking (p<0.05).
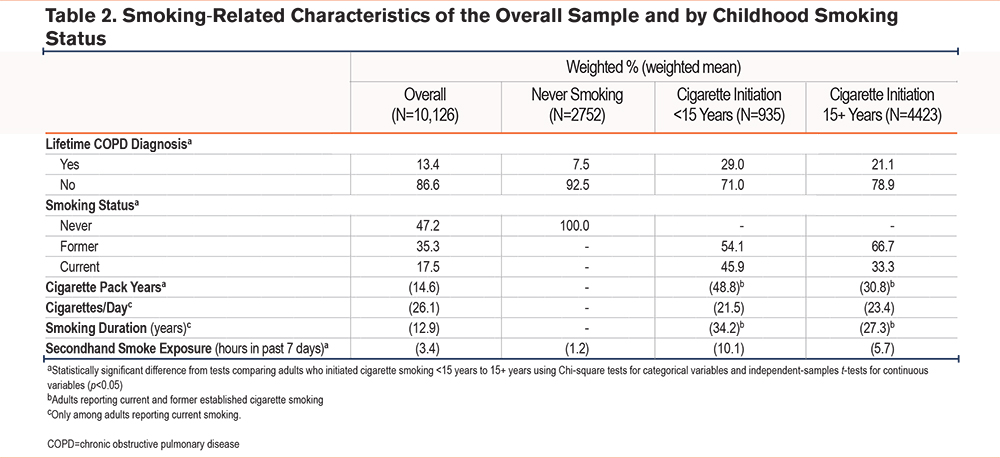
Table 3 shows results from bivariable and multivariable Poisson logistic regressions. In the primary analysis (Table 3a) where age of initiation was entered as a 3-category variable, initiating during childhood (versus 15+ years of age) was associated with an aRR of 1.27 (95% CI=1.06, 1.51). Current (versus never or former) cigarette smoking (aRR=1.37; 95% CI=1.19, 1.59), cigarette pack years (per 10 pack years; aRR=1.02; 95% CI=1.01, 1.03), and secondhand smoke exposure (per 5 hours in the past 7 days; aRR=1.06; 95% CI=1.02, 1.04) also significantly increased the risk of COPD. Supplemental Table 1 in the online supplement shows results from the secondary analysis where age of initiation was entered as a 4-category variable. Results were similar to the 3-category model, with childhood smoking (versus 20+ years) significantly increasing the risk of COPD (aRR=1.40; 95% CI=1.13, 1.75), though starting smoking between 15–19 years did not significantly increase risk.
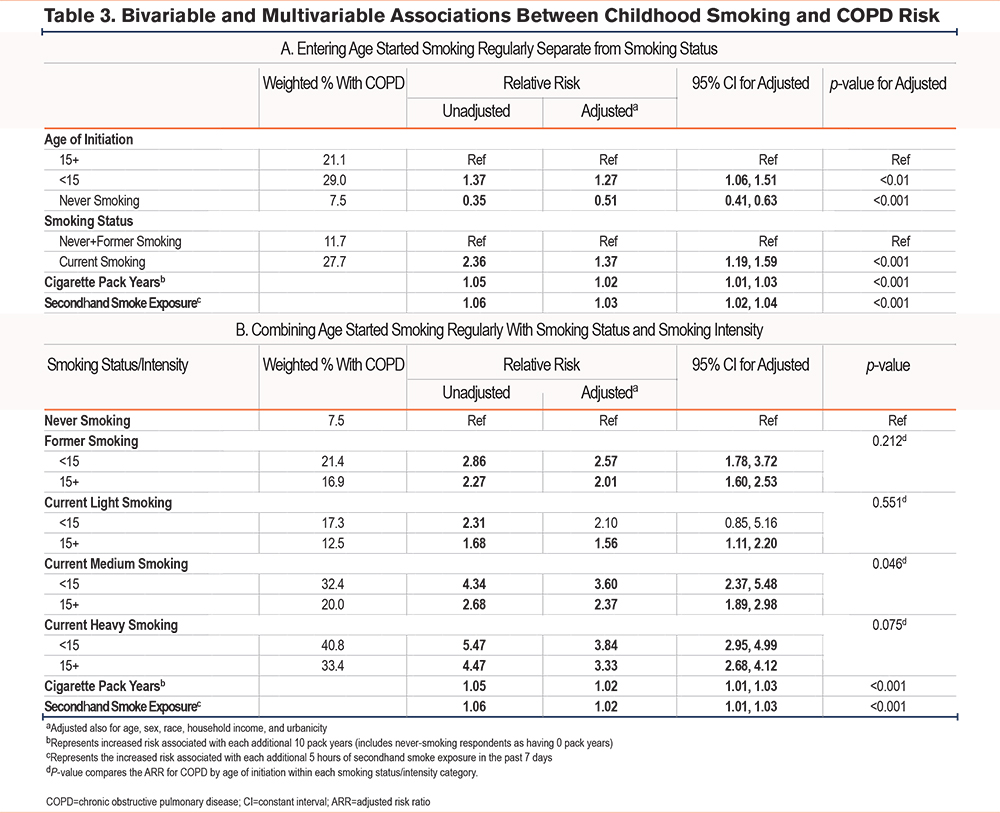
Table 3b shows results from the third analysis where the 9-category variable combining age of cigarette smoking initiation, smoking status, and smoking intensity was included. Only one of the pairwise comparisons within smoking status/intensity category reached statistical significance: the aRR for adults currently smoking 10–19 cigarettes per day (medium intensity) was significantly higher for those who started smoking before the age of 15 as compared to 15+ years (p=0.027). aRRs did not significantly differ between <15 and 15+ years of age at cigarette smoking initiation within the other smoking status/intensity combinations.
Sensitivity Results
Supplemental Table 2 in the online supplement shows the distribution of cigarette pack years and cigarette smoking duration, highlighting the larger range for cigarette pack years as compared to smoking duration that was entered into each respective model.
Supplemental Table 3 in the online supplement shows multivariable models when smoking duration was substituted for cigarette pack years. When smoking duration was used as a continuous measure in place of cigarette pack years in the 3-category age of initiation model (Supplemental Table S3a in the online supplement), the association between childhood smoking and COPD was attenuated (aRR from 1.27 [95% CI=1.06, 1.51] to 1.16 [95% CI=0.99, 1.36]). However, when smoking duration was used as a dichotomous measure (<25 years versus 25+ years smoking, approximating childhood smoking versus not; Supplemental Table S3b in the online supplement), the association between childhood smoking and COPD remained significant (aRR 1.25; 95% CI=1.06, 1.46).
When we systematically added 5% to pack years for respondents who initiated smoking <15 years, an additional 85% was needed to confound the childhood smoking finding reported in Table 3a.
Discussion
In this large nationally representative study of childhood smoking and COPD risk, age of onset for cigarette smoking before 15 years of age was significantly associated with COPD risk, independent of cigarette pack years, current smoking status, secondhand smoke exposure, and smoking duration. The current study replicated the results of a prior study that used NHIS data from 2020 using data from Wave 5 of the PATH study, collected between 2018–2019. Lifetime COPD prevalence was higher in the current study as compared to NHIS overall (7.1% versus 13.4%), for each smoking status, and for each age of cigarette initiation category, reflecting differences in sampling strategies. At the time of the current data collection (W5, 2018–2019), adults in the PATH study had already participated in 4 prior data collection waves, beginning in 2011, resulting in cumulative lifetime COPD diagnoses over the period of 5 waves. In contrast, NHIS provides a snapshot of COPD prevalence for one point in time in a cross-sectional cohort of U.S. adults and does not capture cumulative diagnoses over time.
Despite differences in COPD prevalence, lowess curves examining the association between childhood smoking and COPD prevalence were similar across NHIS and the PATH study, both showing an inflection point at approximately 20 years of age. Also in both studies, it was clear that there was an increased risk for COPD based on age of cigarette initiation <15 (versus 15+ and 20+ years), and the aRRs for childhood smoking were similar to the aRRs for current smoking in both studies. However, the COPD risk associated with childhood smoking was somewhat lower in the PATH study than in NHIS (aRRs of 1.27 versus 1.41) and the risk for adults who initiated smoking 15–19 years was not statistically significant in the PATH study, whereas it increased COPD risk in NHIS. Also in NHIS, childhood smoking increased COPD risk independent of current smoking status and intensity. In this study, the adjusted risk associated with childhood smoking was only apparent for adults who currently smoked at medium intensity (i.e., 15–19 cigarettes per day). Together, findings from both studies show that childhood smoking (<15 years of age) significantly increases risk of COPD independent of current smoking status and pack years of cigarette smoking, though it is unclear what role smoking intensity may play.
Another difference between studies occurred when continuous smoking duration was substituted for cigarette pack years. In NHIS, substituting smoking duration as a continuous measure confounded the association between current smoking status and COPD, but did not significantly impact the association for childhood smoking. In this study, substituting continuous smoking duration confounded both associations. However, in this study, lowess curves showed a stronger relationship between smoking duration and COPD prevalence for adults smoking 25+ years (versus <25 years); when smoking duration was substituted for pack years as a dichotomous measure that may approximate childhood smoking, the association between childhood smoking and COPD risk was no longer confounded. Results from both studies were consistent with findings from a recent report22 showing that smoking duration was a stronger predictor of COPD risk than cigarette pack years.
It is clear that active cigarette smoking is associated with worse lung function,23 including reduced lung growth and lower FEV1 during adolescence.24 By replicating and building on findings from the NHIS study,14 this work demonstrates that there is also an increased risk for long-term chronic disease due to childhood cigarette smoking. Importantly, the risk of COPD during adulthood associated with childhood smoking was found to be independent of current smoking status, secondhand smoke exposure, cigarette pack years, and smoking duration across 2 separate nationally representative datasets of the U.S. population, suggesting that it may be a direct result of the effects of childhood cigarette smoking on lung development during a critical window of time.6,7
In December 2019, the U.S. government passed a federal law that prohibits sales of nicotine and tobacco products, including cigarettes, to youth <21 years of age.25 Findings from the current study support preventing, or at the very least delaying, cigarette smoking initiation until adulthood to allow for critical lung development to occur and to reduce the longer smoking durations that put people at heightened risk for lung diseases like COPD. Such findings could be used to inform public health campaigns that are aimed at preventing the uptake of cigarettes among young people, highlighting the health effects of early cigarette smoking.
This study is not without limitations. First, the primary outcome of a COPD diagnosis relied on participants’ self-report, not spirometry, which could lead to biased estimates. Similarly, respondents were asked at what age they began smoking regularly; “regularly” was left to respondent interpretation. Second, there could be unmeasured variables that account for the associations between early age of cigarette smoking initiation and COPD risk, such as prenatal smoke exposure26 and unmeasured aspects of cigarette smoking not accounted for by pack years, smoking duration, or current smoking status. In addition, secondhand smoke exposure during childhood without primary smoking has been associated with impaired lung development and the development of respiratory diseases like asthma during childhood.2 The secondhand smoke exposure variable available in the PATH study used in the current study asked respondents about their exposure to tobacco smoke only in the past 7 days and did not capture secondhand smoke exposure during childhood. It is possible that alternative measures (e.g., years of living in a household where someone smoked)13 would have influenced results differently. Still, a strength of this study is the inclusion of any measure of secondhand smoke exposure, which was not available for inclusion in the NHIS study and has not been examined as a potential confounder of the relationship between childhood smoking and COPD risk in prior work. Though greater secondhand smoke exposure significantly increased COPD risk, it did not appreciably impact the relationship between age of onset and COPD. Other strengths of the current study include the use of a large nationally representative dataset and sensitivity analyses showing the robustness of findings regarding childhood smoking and increased COPD risk.
In conclusion, findings from the current analysis using PATH study data largely replicate those reported in a recent study using data from NHIS,14 after controlling for secondhand smoke exposure as an additional covariate. In both studies, smoking onset <15 years of age significantly increased COPD risk after controlling for sociodemographic covariates, current smoking status, cigarette pack years, and smoking duration. This study builds on our understanding of how childhood smoking increases the risk of COPD independent of current smoking status and smoking history, which is consistent with prior work suggesting that injury during this phase of known lung development can have lifelong impacts. Physicians should consider talking to their young patients about childhood cigarette smoking, informing them about the potential long-term impacts regarding disease risk.
Acknowledgements
Author contributions: JDS, LMP, and CAS contributed to the conception and design. JEO and ZT were in charge of the data analysis. JEO wrote the initial manuscript draft. All authors contributed to the data interpretation and the editing and final approval of the manuscript.
Declaration of Interests
All authors have no conflicts of interest to disclose.