Running Head: Falls and Medications Among Patients With COPD
Funding Support: Grant support provided by National Iinstitutes of Health/National Heart, Lung, and Blood Institute K23 HL159239 (CLM), Cambia Foundation (RAE, JRC), American Lung Association (LCF), Patient-Centered Outcomes Research Institute (LCF, LD), and the Department of Veterans Affairs (LCF, LJS, LD).
Date of Acceptance: October 21, 2024 | Publication Online Date: October 25, 2024
Abbreviations: CM=Clinical Modification; COPD=chronic obstructive pulmonary disease; EHR=electronic health record; FRID=fall-risk increasing drug; ICD=International Classification of Diseases; SD=standard deviation; SNRI=serotonin norepinephrine reuptake inhibitor; SSRI=selective serotonin reuptake inhibitor
Citation: McDermott CL, Feemster LC, Engelberg RA, Spece LJ, Donovan LM, Curtis JR. Fall risk and medication use near end of life among adults with chronic obstructive pulmonary disease. Chronic Obstr Pulm Dis. 2024; 11(6): 604-610. doi: http://doi.org/10.15326/jcopdf.2024.0551
Online Supplemental Material: Read Online Supplemental Material (1174KB)
Introduction
Patients with chronic obstructive pulmonary disease (COPD) are significantly more likely to experience a fall compared to patients without COPD,1-4 with increased fall risk due to increased frailty,5 impaired gait,2 and tripping hazards from oxygen tubing.6 Falls and resulting injuries such as fractures can result in emergency department visits or hospitalizations, which lower patient quality of life and increase health care costs.7-10 Despite COPD being the sixth most common cause of death in the United States, little is known about falls among these patients near the end of life.11
One modifiable risk factor for falls is medication use, including fall-risk increasing drugs (FRIDs) such as benzodiazepines, sedative-hypnotics, antihypertensives, and other psychoactive agents.12 Patients with COPD have a high prevalence of comorbidities for which FRIDs are often used as treatment, including anxiety, depression, diabetes, and hypertension. The burden of polypharmacy also increases as patients’ functions decline, and they receive additional medications for insomnia and pain.13-15
While these medications are intended to alleviate patient symptoms, they also increase the risk of injurious falls.16-20 Reducing FRID burden represents an opportunity to improve patient outcomes. While previous work has found an association between polypharmacy and increased fall risk,21 FRID burden among patients with COPD, and the relationship between FRID burden and fall risk has not been previously described. FRID use among patients with COPD is of particular concern given the large number of FRID indications (e.g. anxiety, insomnia, dyspnea) among patients with COPD.
We conducted a retrospective cohort study in the University of Washington Medicine system, which is the largest public health system in the Puget Sound area. It includes an academic medical center, a county safety-net hospital, and 2 community hospitals, plus outpatient clinics. With these data, we evaluated the association between FRID use and injurious falls in the last 2 years of life among decedents with COPD. As FRID exposure by class is not well described among patients with COPD, we describe the frequency of FRID prescriptions for different classes of FRIDs in this cohort (e.g., benzodiazepines, sedative-hypnotics, tricyclic antidepressants), comparing the frequency of FRID prescriptions among patients with COPD who experienced an injurious fall to patients with COPD without an injurious fall. We included anticonvulsants for patients without comorbid seizure disorder. Our hypothesis is that among patients with COPD, injurious falls are associated with FRID burden.
Methods
Study Design and Population
For this study, we used a linked database between Washington State death certificates and the electronic health record (EHR) of the University of Washington Medicine system to evaluate patterns of care for adults with serious illness. The goal of the study was to identify factors associated with an increased risk of injurious falls for adults with COPD who died from any cause between 2014–2018. COPD was defined using International Classification of Diseases (ICD) codes, specifically ICD-9-Clinical Modification (CM) 491.xx, 492.xx, or 496, and ICD-10-CM J41, J42, J43, J44. Patients had to have at least 2 codes assigned to be classified as having COPD.
Exposure and Outcome
Primary Exposure of Interest
We identified the presence or absence of prescriptions for FRIDs in the EHR and grouped medications by class.18,22,23 These medication classes included anticonvulsants, antihypertensives, antipsychotics, antispasmodics, atypical antidepressants (e.g., bupropion, mirtazapine), benzodiazepines, opioids, sedative-hypnotics, selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, plus tricyclic and tetracyclic antidepressants. Medications were identified using brand or generic names in the EHR (full list available in Supplemental Table 1 in the online supplement). Patients with a prescription for a FRID of any duration were categorized as exposed to the medication, and we reported the total number of FRID prescriptions per patient by class (i.e., FRID burden).
Primary Outcome
We identified24 an injurious fall using ICD-9 code V15.88 and ICD-10 code Z91.81. Our outcome is documentation of an injurious fall requiring medical attention, drawn from previously published algorithms and defined as emergency department visits, hospitalizations, and outpatient visits with a fall-related diagnosis and with a code for: brain injury; contusion; dislocation of the hip, jaw, knee, shoulder, wrist; or nonpathological fracture of the skull, face, spine, clavicle, ribs, humerus, wrist, pelvis, hip, fibula, tibia, foot, or ankle.24,25 We excluded visits for a motor vehicle collision.26 The full list of ICD codes is available in Supplemental Table 2 in the online supplement.
Adjustment Confounders
The following confounders were selected based on prior data suggesting an association with risks of a fall27-30: comorbidities, race (previously self-reported), level of education (completed some college or higher), and marital status (married or not married at the time of death) from the Washington State death certificates; age, sex, and insurance status (private, Medicare, Medicaid, other) were identified from the EHR.
Using an adaptation of the Dartmouth Atlas31 criteria for serious illness, we identified comorbidities and fall history from the EHR using ICD code versions 9 or 10, using ICD-10 codes for diagnoses after 2015. In addition, all patients could have an additional comorbidity as defined by the Dartmouth Atlas31: advanced renal disease, coronary artery disease, dementia, diabetes with end organ damage, end-stage liver disease, heart failure, pulmonary disease other than COPD (e.g., idiopathic pulmonary fibrosis), peripheral vascular disease, or poor prognosis cancer (e.g., metastatic solid tumor or aggressive hematologic malignancy such as acute myeloid leukemia).31 Together, these conditions comprise the most common causes of death in America, excluding suicide, accidents, and infections.32
We refined and updated these codes through continuous quality improvement, using the general equivalency maps provided by the Centers for Medicare and Medicaid Services33 in addition to manual review by 2 clinicians to resolve any potential discrepancies in mapping codes to conditions. Each comorbidity was assessed separately rather than using a summed comorbidity score. Since comorbidity prevalence varies among patients with COPD, this afforded us the opportunity to illustrate the comorbidity patterns in this population. We used ICD codes to identify the presence of comorbidities. Unfortunately, ICD codes do not indicate condition severity, thus, we assigned all comorbidities equal weight.
Statistical Analysis
We describe the study population by comorbidities including fall history, demographics, and FRID prescriptions for those with and without an injurious fall, using a t-test to examine differences in FRID prescription type between groups at 95% significance. Using multivariable logistic regression in a single model, we examined the association of FRID burden with the outcome of injurious fall, dichotomized as a binary variable of 0 (none) or 1 (1 fall or more), while adjusting for demographic characteristics, types of comorbidities, fall history, and FRID burden, defined as number of FRID prescriptions for different FRID classes. The University of Washington Institutional Review Board approved this study and issued a waiver of consent to access decedent records in accordance with Washington State law. We performed all analyses using Stata version 16.0 (StataCorp; College Station, Texas).
Results
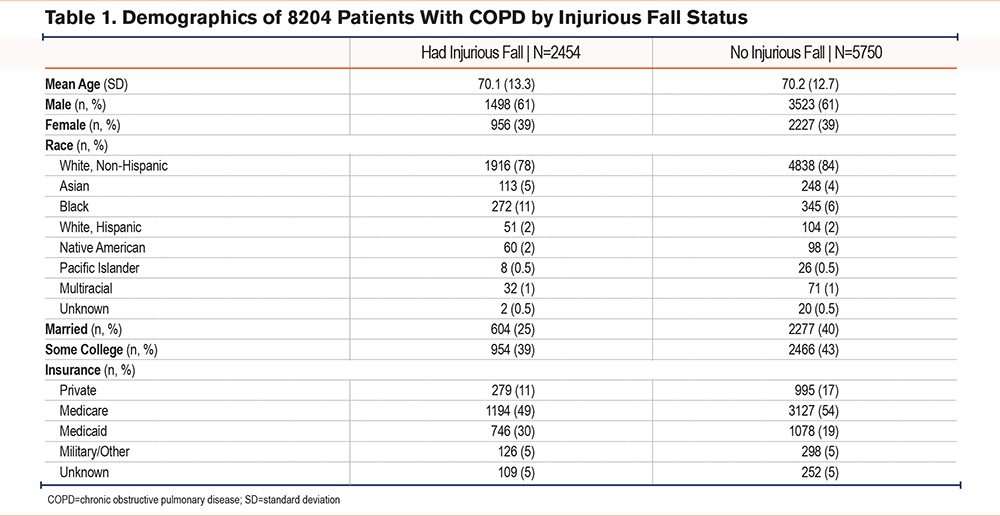
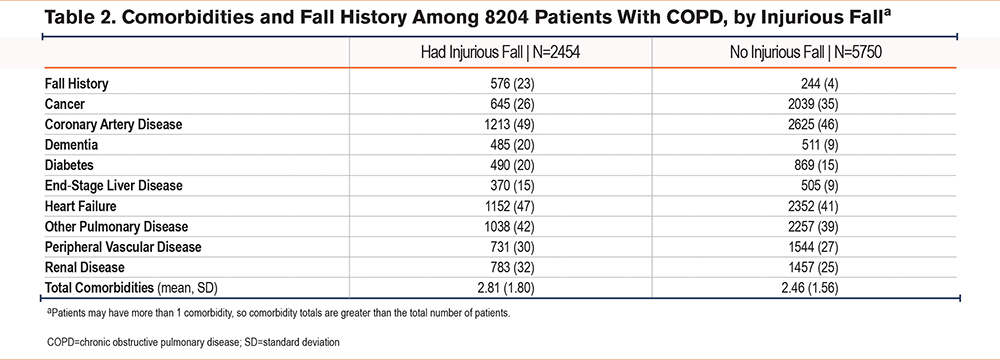
We identified 8204 decedents with COPD, and of these patients, 2454 (30%) had an injurious fall. Patients with COPD and an injurious fall were more likely to be Black, unmarried, and enrolled in Medicaid, while those without an injurious fall more frequently had private insurance and at least some college-level education (Table 1). A history of falling was markedly higher among patients experiencing an injurious fall compared to those without a fall (23% versus 4%). Patients with COPD who had an injurious fall also had more comorbidities compared to those with COPD who did not fall (Table 2). The average number of comorbidities was 2.81 (standard deviation [SD] 1.80) among those with an injurious fall versus 2.46 (SD 1.56) for those without a fall. The only comorbidity that occurred more frequently among those without an injurious fall was cancer (26% among patients who fell versus 35% with no fall).
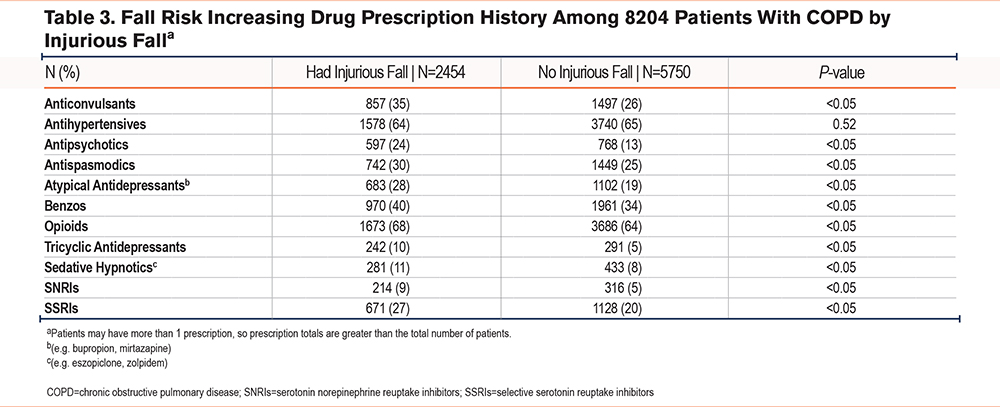
In multivariate logistic regression, a FRID prescription was associated with a higher risk of injurious falls (odds ratio 1.07, 95% confidence interval 1.04–1.09). FRID burden was higher among patients with an injurious fall, with a mean of 3.47 prescriptions across FRID classes (SD 2.66) whereas, those without an injurious fall had an average FRID burden of 2.85 FRIDs (SD 2.24) (Table 3). Across both groups, the most prescribed FRID classes were antihypertensives, opioids, and benzodiazepines. Comparing patients with an injurious fall to those without, the largest differences in prescriptions were noted for anticonvulsants (35% versus 26%), antipsychotics (24% versus 13%), atypical antidepressants (28% versus 19%), tricyclic antidepressants (10% versus 5%), and SSRIs (27% versus 20%). Across all medication classes, FRID use was statistically higher (p<0.05) among those with an injurious fall compared to those without a fall, except for antihypertensives (p=0.52).
Discussion
We found that FRID burden was associated with a higher risk of falls, after adjusting for demographic and clinical conditions. With this analysis, we provide additional information on which medication classes could be targeted by interventions to mitigate fall risk and improve patient outcomes.
In situations of polypharmacy, it can be difficult to decide which medications should be prioritized for dose reduction or discontinuation. We note that the most prescribed FRID class among all patients with COPD was antihypertensives. While the difference between the 2 groups with falls was not statistically significant, this still may be an area to consider deprescribing and/or dose reducing for patients with COPD, especially for those with episodes of orthostatic hypotension, well-controlled blood pressure, or limited life expectancy. In a previous study of older adults that explored ways to address medication-related symptoms, patients with COPD were more likely to prioritize reduction of fall injuries compared to reduction of cardiovascular events.34
The second and third most common FRID classes in our analysis were opioids and benzodiazepines. These medications can be prescribed as palliation to relieve breathlessness or anxiety among patients with COPD.35,36 While such medications are appropriate in this context, additional fall mitigation options should be considered. We noted that patients with falls were more likely to receive anticonvulsants, antipsychotics, atypical antidepressants, tricyclic antidepressants, and SSRIs. These medications are often used for pain, insomnia, and depression; nonpharmacological options could perhaps reduce some medication use and thus, lower fall risk.
Finally, dementia was a more common comorbidity among those with a fall compared to those who did not fall. This finding aligns with other studies that have found patients living with dementia are 2 to 3 times more likely to fall compared to patients without dementia,37,38 since gait control is negatively impacted when cognition is reduced. When possible, nonpharmacological alternatives to FRIDs, or using the lowest FRID dose possible for the shortest duration should be encouraged for patients living with both COPD and dementia.
There are limitations to this study. First, patients may have received care for falls in other health care systems, but these data were not available to us as we relied on one EHR, a known limitation of EHR-based studies.39 We relied on ICD-9 and ICD-10 coding to determine the presence of comorbidities, but these codes do not provide information as to condition severity, which may confound fall risk. We had access to medication orders rather than pharmacy claims that implied a prescription was filled. It is possible that patients did not take the prescribed medications or did not fill the prescriptions; additionally, we have no information on over-the-counter FRIDs such as diphenhydramine that patients may have taken. Finally, we do not have information about COPD severity/exacerbation history or home oxygen use, both of which are associated with falls.
Medication management is an area where pharmacists’ collaborations with pulmonologists and primary care providers can personalize care to reduce fall risk when engaging in shared decision-making and fall risk mitigation. Our study suggests that additional screening regarding medication use and collaboration across disciplines (e.g., pulmonary, primary care, cardiology, palliative care) may help mitigate fall risk while managing symptoms and comorbidities.
Acknowledgments
Author contributions: CLM, RAE, and JRC conceptualized the project and obtained funding. CLM conducted the formal analysis, and RAE and LJS contributed to the formal analysis. LCF contextualized the results of the formal analysis. RAE and JRC curated the data. CLM conducted the investigation, with RAE and JRC as co-conductors. CLM and RAE decided upon and executed the study methodology. LCF, LJS, and LD contributed to the study design and methodology, and JRC contributed to the study design. CLM administered the project, and RAE co-administrated. CLM wrote the original draft of the manuscript, with LCF, RAE, LJS, LD, and JRC as cowriters. All authors reviewed and edited the final manuscript version.
We appreciate the help of James Sibley with the creation of the database used for analysis.
Declaration of Interest
CLM reports grant funding from the National Institutes of Health (NIH)/National Heart, Lung, and Blood Institute (NHLBI). She is a consultant for the nonprofit Biologics and Biosimilars Collective Intelligence Consortium and received honoraria from the University of Utah in 2023 for speaking at 2 departmental seminars. LCF received grant support from the Patient-Centered Outcomes Research Institute (PCORI), the American Lung Association, the Department of Veterans Affairs Health Systems Research, and the NIH/NHLBI. She has received travel funding from the American Thoracic Society to attend leadership meetings, and consultant fees from the Society of Hospital Medicine and the National Quality Assurance Committee. RAE received funding support from the Cambia Health Foundation. LJS reports grant support from the NIH/NHLBI. LD reports grant support from the Department of Veterans Affairs Health Systems Research and the PCORI, plus an honorarium from the American Academy of Sleep Medicine as a continuing medical education speaker for the 2023 conference. JRC received funding support from the Cambia Health Foundation.