Running Head: Telerehabilitation Continues Post-COVID-19
Funding Support: No funding was received for this research.
Date of Acceptance: November 14, 2024 | Publication Online Date: November 26, 2024
Abbreviations: ACT=Australian Capital Territory; ATS=American Thoracic Society; CBPR=center-based pulmonary rehabilitation; COPD=chronic obstructive pulmonary disease; IQR=interquartile range; NSW=New South Wales; NT=Northern Territory; PR=pulmonary rehabilitation; QLD=Queensland; SA=South Australia; TAS=Tasmania; VIC=Victoria; WA=Western Australia
Citation: May AK, Holland AE, Alison JA, Herrmann K, Cox NS. Telerehabilitation services remain increased post-COVID-19 in Australia. Chronic Obstr Pulm Dis. 2025; 12(1): 93-97. doi: http://doi.org/10.15326/jcopdf.2024.0575
Online Supplemental Material: Read Online Supplemental Material (298KB)
Note: A portion of this work was presented in abstract form at the Thoracic Society of Australia and New Zealand 2024 Annual Scientific Meeting
Introduction
Pulmonary rehabilitation (PR) is a highly effective, yet widely underused treatment for people with chronic obstructive pulmonary disease (COPD) as well as other chronic respiratory diseases.1,2 Typically, PR is an 8–12 week program delivered within a hospital or health care center.2 However, patients may experience significant barriers to attending center-based PR (CBPR).2 The opportunity to undertake PR at home via telerehabilitation may help overcome some patient-related barriers to attending CBPR, such as travel and transport issues, thereby supporting increased service access.2-4 Prior to the COVID-19 pandemic, very few programs (just 4% in the Australian context) delivered home-based PR.5 Telerehabilitation use expanded during the pandemic. However, postpandemic it is unclear how many services continue to deliver telerehabilitation, and how telerehabilitation delivery may have impacted CBPR programs, for people with COPD and other chronic respiratory diseases.
Telerehabilitation programs may use synchronous (e.g., telephone calls, video conferencing) or asynchronous communication (e.g., email),3 and can be available across a variety of platforms. A recent Cochrane review has demonstrated that, for people with COPD, telerehabilitation achieves similar clinical outcomes to CBPR for exercise capacity, quality of life, and breathlessness, although findings for other outcomes, such as hospitalization, remain limited by the certainty of available evidence.4 Telerehabilitation is, however, associated with greater program completion rates.4 International clinical practice guidelines recommend that people with chronic respiratory disease should be provided a choice of CBPR or telerehabilitation.2 For telerehabilitation to be a clinically acceptable alternative to CBPR, program models should meet similar standards to those of CBPR in delivering the essential components of effective PR.6 Defined essential components include an initial pre-program center-based assessment, individually prescribed and progressed endurance and resistance training, and delivery of the program by health care professionals trained in the specific telerehabilitation model.1 The extent to which telerehabilitation models deliver the essential components of PR in clinical practice is unclear.
This study aimed to characterize PR service delivery, investigate the impact of the COVID-19 pandemic on PR services, and describe telerehabilitation and CBPR with reference to the essential components of PR in the Australian context.
Methods
An online, cross-sectional survey was undertaken between July 19, 2023, and August 28, 2023 (Qualtrics; Provo, Utah), with pilot testing and expert review prior to launch. Email invitations for completion of the voluntary anonymous survey were sent to all PR programs listed within the Lung Foundation Australia national database, the most comprehensive record of programs available. A preference was indicated for the PR coordinator of each service to complete the survey if possible. Only one survey could be completed for each PR site. Ethics approval was granted prospectively (Monash University [ID 39264]).
The survey was comprised of 27 questions (Supplementary Table S1 in the online supplement). A total of 25 questions were in closed categorical form (plus subquestions as required), and 2 questions required open responses. The survey explored PR program availability, program structure, and satisfaction with the essential components of PR. Respondents were asked to describe PR program delivery: (1) at the time of survey completion, and (2) to recall program delivery practices prior to, and during (2020−2022) the COVID-19 pandemic. Demographic information relating to the role of the respondent, professional makeup of the PR team and PR service setting were also collected.
All responses received, including from incomplete surveys, were included in the data analysis (IBM SPSS Statistics V28.0 [IBM Corp; Armonk, New York]). Descriptive statistics were reported as number (%) or median (interquartile range [IQR]). Open responses were coded thematically. Service availability at the time of survey completion was compared with availability pre-COVID-19 pandemic for CBPR, and during the pandemic (2020-2022) for telerehabilitation (McNemar’s test; significance p<0.05).
Results
Survey invitations were sent to 295 PR programs with 117 responses received (40% response rate; n=9 [8%] incomplete). Respondents represented all Australian states and territories, were located across metropolitan, regional and rural areas, and provided services in a variety of clinical settings (Figure 1). A total of 92% of respondents were the service PR coordinator. PR services included team members across a variety of occupations, most commonly physiotherapists (96%), allied health assistants (61%), and nurses (55%).
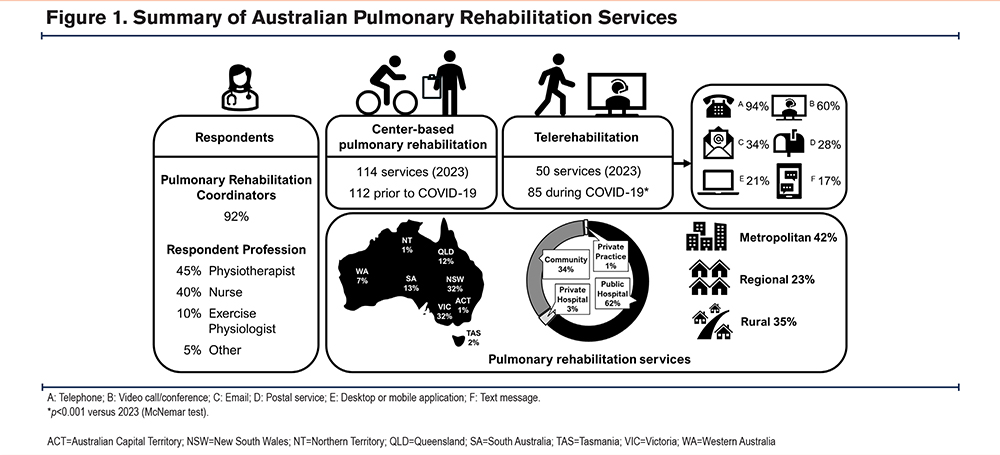
Among respondents, 97% (n=114/117) reported delivery of CBPR at the time of survey completion (Figure 1), which was similar to recall of prepandemic groups CBPR availability (96%). CBPR was primarily delivered in a group setting (n=109/110, 99%), to median (IQR) 7 (6–8) participants per group. Among respondents, 39% (n=42/109) reported CBPR group size to be smaller than prepandemic groups. The most common CBPR training modalities were walking (90%), free/machine weights (78%), stationary cycling (68%), and resistance bands (53%).
Telerehabilitation was reported to be delivered by 43% of respondents (n=50/116) current at the time of survey completion (Figure 1). Availability of telerehabilitation at the time of survey completion was significantly reduced compared with recall of availability during the pandemic (74%, n=85/114; p<0.001). The most cited reasons for telerehabilitation cessation were staffing limitations, patient preference for CBPR, and staff perception of greater ease/benefits of CBPR. All services except one delivered telerehabilitation in addition to CBPR. Multiple telerehabilitation models were used, including telephone (94%), video interaction (60%), and email (34%). Of synchronous (video) telerehabilitation programs (n=28), group video conferencing (n=11/28, 39%; median [IQR] 3 [2–4] participants per session) was less commonly delivered than 1:1 video calls (n=26/28, 93%; Figure 2). Reported session durations for telephone (median [IQR] 30 minutes [20–30]) and video interaction (median [IQR] 45-minute [30–60]) were shorter than for CBPR (median (IQR) 60 min [60–90]). Synchronous (video) telerehabilitation was more often delivered from a metropolitan setting (65%) than a rural/remote setting (35%). The most common telerehabilitation training modalities were walking (89%), free/machine weights (63%), bodyweight resistance exercises (58%), and resistance bands (50%).
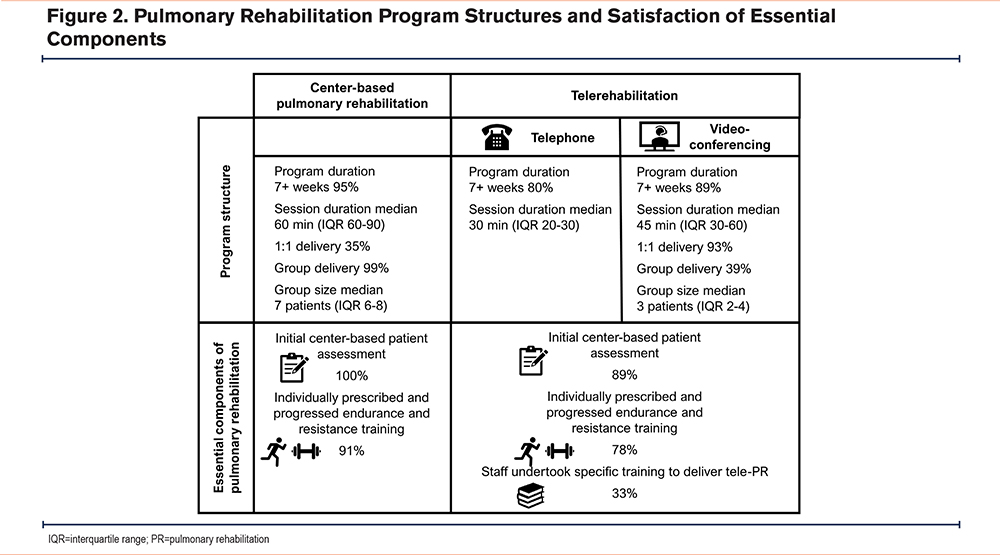
The PR essential component of an initial in-person center-based assessment was performed in 100% of CBPR and 89% of telerehabilitation programs (Figure 2). Individually prescribed and progressed endurance and resistance training was delivered in most CBPR programs (91%), but fewer telerehabilitation programs (78%). Staff training specific to the telerehabilitation models being delivered was undertaken by 33% of services delivering remote programs (n=15/45).
Discussion
This study characterizes availability and delivery of PR in Australia. CBPR program availability is largely consistent with prepandemic levels, but with a reduction of group size. Telerehabilitation availability, although less than during COVID-19 restrictions, remains substantially higher than prepandemic availability.5,7,8 Despite diversified program delivery models, the majority of both CBPR and telerehabilitation programs complied with the essential components of PR.
In the current postpandemic era, there is greater availability of telerehabilitation services for people with chronic respiratory disease. In keeping with the increased telerehabilitation service availability seen here, 86% of UK PR programs now offer a remotely delivered home-based PR option, up from 34% prepandemic.8 Expanding the modalities of PR delivery offered within clinical practice may support broader, more equitable, access to PR for people with chronic lung diseases.2 Importantly, this continued telerehabilitation availability also does not detract from the quality and availability of CBPR. Telerehabilitation program models are not suitable for all patients,2 likewise there is increasing patient preference for a return to in-person consultation, waning concerns about COVID-19 infection, and variable administrative and regulatory support for hybrid care delivery models (i.e., face-to-face as well as telehealth),9 which all support the ongoing need for CBPR. Given that telerehabilitation is a recommended alternative to CBPR in international guidelines,2 continuing to support the implementation of telerehabilitation along with CBPR across a variety of health care contexts is important if equitable delivery is to be sustainable.
While most telerehabilitation programs (89%) complied with the PR essential component of a center-based assessment, individualized prescription/progression of endurance and resistance training was less often reported to be undertaken (78%). In addition, relatively few services provided telerehabilitation model-specific training. Experience and competency with technology are known factors in the successful delivery of remote health care.10 Whether enhanced telerehabilitation model-specific training would improve clinician confidence to deliver telerehabilitation, including compliance with individualized prescription and progression of exercise training, remains to be determined.
Access to PR is an issue on a global scale.2,11 The potential to improve PR service access is a proposed benefit of telerehabilitation models.1,2 This study highlighted that CBPR group size reduced postpandemic, along with telerehabilitation being more commonly delivered 1:1 rather than in a group format. This indicates the possibility that overall PR program capacity could have reduced postpandemic, impeding program access for patients. Whether changes in program funding, or other contributors such as referral practices, have contributed to reduced service capacity requires exploration. In Australia, health care is largely funded under a universal scheme for subsidization and reimbursement, however, in regions where PR reimbursement is complex, such as the United States, fluctuating service capacity based on financial drivers may have profound effects on access to PR for patients.6
The cross-sectional nature of this work relied upon participant recollection of service delivery over the previous 4-year period. This requirement for extended recall, coupled with the potential for changes to staffing during the intervening period, may have impacted historical program knowledge held by the respondent. The response rate for this study was 40%, which is lower than a previous Australian survey of PR services.5 This may be attributed to the use of an online method of survey delivery without incentive,12 although is in keeping with accepted online survey response rates (mean 44.1%).13 That all Australian states and territories are represented, including rural, regional, and metropolitan services, supports the data being largely reflective of the current state of Australian PR.
Conclusion
Telerehabilitation services continue to be more available to people with COPD and other chronic respiratory diseases than prepandemic. Most Australian telerehabilitation programs currently meet PR essential components, supporting the ability of such models to deliver effective PR programs. However, telerehabilitation services and CBPR program capacity have both declined post-COVID. This highlights the importance of ensuring the sustainability of effective PR programs, irrespective of the model of delivery, to support widespread access to this recommended treatment for people living with COPD and other chronic respiratory diseases.
Acknowledgements
Author contributions: NSC conceptualized the study. All authors developed the study protocol and data analysis plan. AKM collected and analyzed data. AKM and NSC interpreted the data. AKM and NSC drafted the manuscript. All authors revised and approved the final manuscript.
We would like to extend our thanks to Emma Halloran for her input during survey development.
Declaration of Interests
The authors declare no conflicts of interest.