Running Head: COPD and Mortality in Arthritis Patients: NHANES
Funding Support: This study was funded by the Medical Key Laboratory Construction Project (No. ZDXK2021006).
Date of Acceptance: December 6, 2024 | Publication Online Date: December 12, 2024
Abbreviations: BMI=body mass index; CAPI=Computer-Assisted Personal Interviewing; CDC=Centers for Disease Control and Prevention; CI=confidence intervals; CLRD=chronic lower respiratory diseases; COPD=chronic obstructive pulmonary disease; CVD=cardiovascular disease; HR=hazard ratio; ICD-10= International Classification of Diseases, Tenth Revision; MEC=Mobile Examination Center; NHANES=National Health and Nutrition Examination Survey; PIR=poverty-to-income ratio; RA=rheumatoid arthritis; SD=standard deviation; Th=T-helper cell
Citation: Zhang Y, Chen G, Huang A, Hu Y, Fu C. Association between chronic obstructive pulmonary disease and mortality in participants with arthritis: data from the National Health and Nutrition Examination Survey 1999–2018. Chronic Obstr Pulm Dis. 2025; 12(1): 61-71. doi: http://doi.org/10.15326/jcopdf.2024.0573
Online Supplemental Material: Read Online Supplemental Material (230KB)
Introduction
Arthritis, a common chronic disease, is one of the leading causes of disability worldwide.1 Its incidence and prevalence have notably increased alongside population aging and improvements in patient survival rates.2,3 Research forecasts that by 2040, the number of adults in the United States diagnosed with arthritis by physicians is projected to rise by 49%, reaching 78.4 million and accounting for 25.9% of the total adult population.4 Concurrently, the number of adults with limited activity due to arthritis will increase by 52%, reaching 34.6 million, accounting for 11.4% of all adults.4 Moreover, the World Health Organization predicts that the proportion of the global population aged 60 years and older will escalate from 12% to 22% between 2015 and 2050.5 Consequently, with the accelerated global aging of the population, effectively mitigating the disease burden associated with arthritis and its related complications has emerged as a pressing public health concern that necessitates urgent attention.
Chronic obstructive pulmonary disease (COPD), being a condition with a high disability rate and ranking as the third leading cause of death globally, also exerts considerable pressure on clinical medicine and public health.6 Persistent airflow limitation is a hallmark of COPD, and the condition typically progresses over time. It is closely associated with chronic inflammatory responses within the airways and lung tissue, which are primarily triggered by exposure to harmful gases or particles, notably tobacco smoke.6,7 COPD patients commonly exhibit symptoms such as chronic cough, sputum production, chest tightness, wheezing, shortness of breath, or dyspnea. As the disease advances, these symptoms gradually worsen, potentially culminating in respiratory failure and death.8 It is worth noting that the impact of COPD on lung aging becomes more pronounced with increasing age, further compounding the burden of the disease.9
Recent studies have suggested a complex interplay between COPD and arthritis, which may influence patient outcomes through various mechanisms, including shared inflammatory pathways, lifestyle factors, and potential genetic predispositions. A study by Hyldgaard et al10 involving 31,333 patients with rheumatoid arthritis (RA) in Denmark, revealed that COPD as a comorbidity significantly increased the mortality rate among RA patients by 10%. Nikiphorou et al in their analysis of 6591 RA patients in the United Kingdom, identified COPD as a major predictor of early death among those with early-stage RA.11 However, the prognostic relationship between COPD and arthritis remains unclear in the American population.
Given this background, a longitudinal analysis was conducted using data from the National Health and Nutrition Examination Survey (NHANES) database spanning from 1999 to 2018. The aim was to explore the association between COPD and mortality risk among adult arthritis participants in the United States. Our objective is to provide scientific evidence for mitigating the negative impacts of these 2 diseases on individual health, improving patient outcomes and quality of life, and effectively addressing this significant public health challenge.
Methods
Data Sources
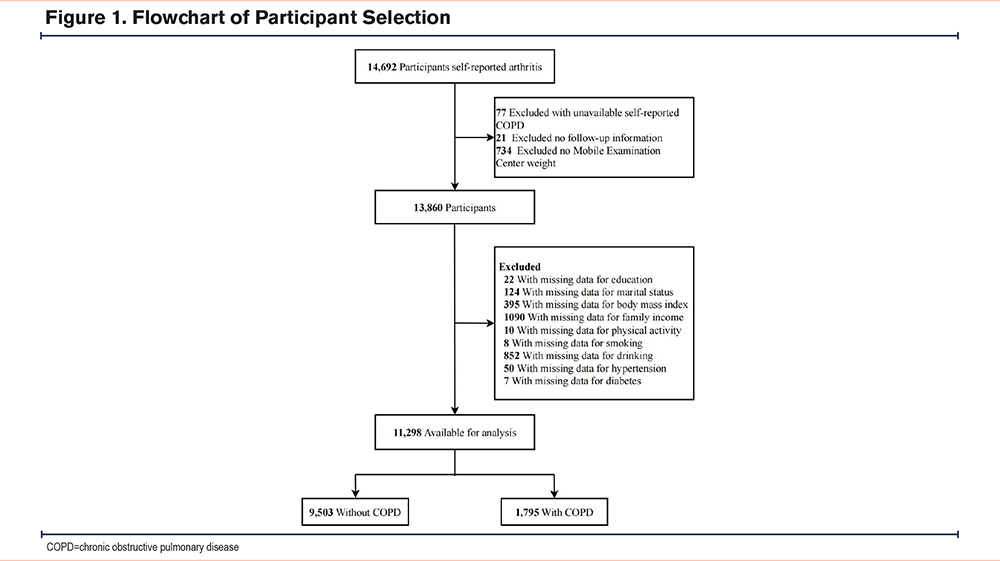
This study examined data from 10 cycles of the NHANES (1999–2018). The NHANES collects comprehensive data through structured interviews at home, physical examinations at mobile centers, and laboratory tests, employing a scientific multistage probability sampling design.12 A professional team consisting of physicians, medical technicians, and interviewers is distributed across the United States to ensure the accuracy and extensiveness of data collection. This study focused on 14,692 participants who self-reported having arthritis diagnosed by a physician and were subject to long-term follow-up. During the data cleaning phase, 77 participants with missing COPD data were initially excluded, followed by the exclusion of 21 participants with incomplete follow-up information. Subsequently, 734 participants without Mobile Examination Center (MEC) weights were excluded. Finally, 2562 participants with incomplete data on other key variables (such as demographics, risk behaviors, and relevant comorbidity data) were excluded. The ultimate study cohort consisted of 11,298 participants, including 1795 self-reported COPD participants and 9503 non-COPD participants. The detailed screening process is shown in Figure 1. All NHANES protocols have been approved by the Ethics Review Board of the National Center for Health Statistics at the Centers for Disease Control and Prevention (CDC), and written informed consent was obtained from all survey participants.13
Diagnosis of Arthritis and COPD
The diagnoses of arthritis and COPD in this study were both based on responses to the disease and health survey questionnaire. Trained interviewers administered these questions to participants at home using the Computer-Assisted Personal Interviewing (CAPI) system, and this system is programmed with built-in consistency checks to minimize data entry errors. Additionally, the CAPI system utilizes online help screens to assist interviewers in clarifying key term definitions within the questionnaire.14 After data collection, rigorous data review and editing were conducted to ensure data integrity, consistency, and logical coherence. Previous research has validated and supported this method.15-18
For the diagnosis of arthritis, participants were asked the following question: "Has a doctor or other health professional ever told you that you had arthritis?" Participants were required to choose either "Yes" or "No" as their response. If the participant answered "Yes," they were considered to have arthritis.
COPD was determined by a positive response to any of the following 3 questions: "Has a doctor or other health professional ever told you that you had chronic bronchitis?"; "Has a doctor or other health professional ever told you that you had emphysema?"; and "Has a doctor or other health professional ever told you that you had COPD?" If the participant answered "Yes" to any of these questions, they were classified into the COPD group; if they answered "No" to all, they were classified into the non-COPD group.
Outcome Ascertainment
The National Center for Health Statistics determines mortality data by matching participants' detailed information, including Social Security number, name, date of birth, race/ethnicity, sex, place of birth, and residency status, with the National Death Index. The International Classification of Diseases, Tenth Revision (ICD-10), is used to determine mortality rates for specific causes of death. This classification system provides a standard method for coding and categorizing causes of death. The primary endpoint of this survey is all-cause mortality, which is defined as death occurring from any cause. CVD mortality, specifically, is defined by the ICD-10 codes I00-I09, I11, I13, I20-I51, and I60-I69, which cover a range of heart and vascular diseases.19
Covariates
Based on previous research, information on various covariates was collected, including sex, age, race/ethnicity, education level, marital status, household income, physical activity, body mass index (BMI), smoking status, drinking status, and the presence of hypertension or diabetes. Specifically, demographic characteristics such as age, sex, race/ethnicity, education level, household income, and marital status were chosen due to their known associations with both COPD and arthritis.20,21 For instance, age and sex are risk factors for both conditions, while socioeconomic status, reflected by education level and household income,22 can influence disease outcomes. Marital status may impact the social support and stress levels of individuals with either disease.23 Race/ethnicity is important to consider due to potential variations in disease prevalence, severity, and response to treatment across different populations.24,25
Regarding health indicators, we selected physical activity, BMI, smoking status, drinking status, hypertension, and history of diabetes based on their established relationships with COPD and/or arthritis. Smoking is a major risk factor for COPD and has also been linked to arthritis through mechanisms such as inflammation.26,27 Alcohol consumption, BMI, and physical activity have been shown to influence both diseases, either directly or indirectly.28-30 Hypertension and diabetes are common comorbidities that can complicate the management and outcomes of both COPD and arthritis.1,31
Race/ethnicity was classified into 4 categories: non-Hispanic White, non-Hispanic Black, Mexican American, or other.32 The participants' education levels were categorized into 3 groups based on the number of years of schooling: less than 9 years, 9-12 years, and more than 12 years. Marital status was categorized as married/living with a partner or living alone, which included categories such as never married, separated, divorced, and widowed. Following the guidelines of U.S. government reports,33 household income was classified into 3 levels based on the poverty-to-income ratio (PIR): low (PIR ≤ 1.3), middle (1.3 < PIR ≤3.5), and high (PIR >3.5).34 Physical activity levels were categorized based on the presence and intensity of activities performed during leisure time or at school over the past 30 days.13 Individuals were classified as sedentary if they did not engage in any leisure-time physical activity. They were classified as having moderate activity if they participated in at least 10 minutes of activity that caused light sweating or slight to moderate increases in breathing or heart rate (e.g., brisk walking, bicycling for pleasure, golf, dancing). Individuals were classified as having vigorous activity if they engaged in at least 10 minutes of activity that resulted in heavy sweating or significant increases in breathing or heart rate (e.g., running, lap swimming, aerobics classes, fast bicycling).32 Individuals who had smoked less than 100 cigarettes throughout their lifetime were categorized as having never smoked. Those who had smoked more than 100 cigarettes and were still engaging in the habit were considered current users of tobacco, while those who had smoked more than 100 cigarettes but had since made the decision to quit were deemed former users of tobacco. Drinking status was assessed annually based on alcohol intake. Participants who reported consuming at least 12 alcoholic beverages of any type were categorized as "Yes," while those who did not meet this criterion were categorized as "No." BMIs were calculated based on participants' height and weight. Information about hypertension or diabetes was self-reported and relied on previous diagnoses by a doctor.
Statistical Analysis
This study adopted the weighting method advocated by the CDC, specifically designed to address the issue of oversampling of ethnic minorities and ensure accurate evaluation of the impact on the general population. In conducting all analyses, comprehensive consideration was given to sample weights, stratification, and primary sampling units, with the aim of obtaining more precise national estimates. Specifically, MEC weights were utilized. For the data cycle from 1999 to 2002, the weight calculation formula used was 2/10 × wtmec4yr; for the data cycle from 2003 to 2018, the weight calculation formula used was 1/10 × wtmec2yr.
For data description, continuous variables were presented as mean values with their corresponding standard deviations (SD), while categorical variables were represented by unweighted frequencies and weighted percentages. To investigate differences between variables, t-tests were utilized for comparisons of continuous data, and Chi-squared tests (χ²) were employed for comparisons of categorical data.
To visually represent survival outcomes, Kaplan-Meier survival curves were utilized for visualization analysis. The log-rank test was applied to assess differences in cumulative mortality rates. Additionally, the Cox proportional hazards model was employed to investigate the association between COPD and all-cause mortality as well as CVD mortality. Hazard ratios (HR) and their corresponding 95% confidence intervals (CI) were determined.
To account for potential confounding factors, 4 models were constructed sequentially for stepwise adjustment. Model 1 was the crude model. Model 2 adjusted for sex, age, race/ethnicity, education level, marital status, and household income. Model 3 further added physical activity, BMI, smoking status, and drinking status. Model 4 considered hypertension and diabetes based on Model 3.
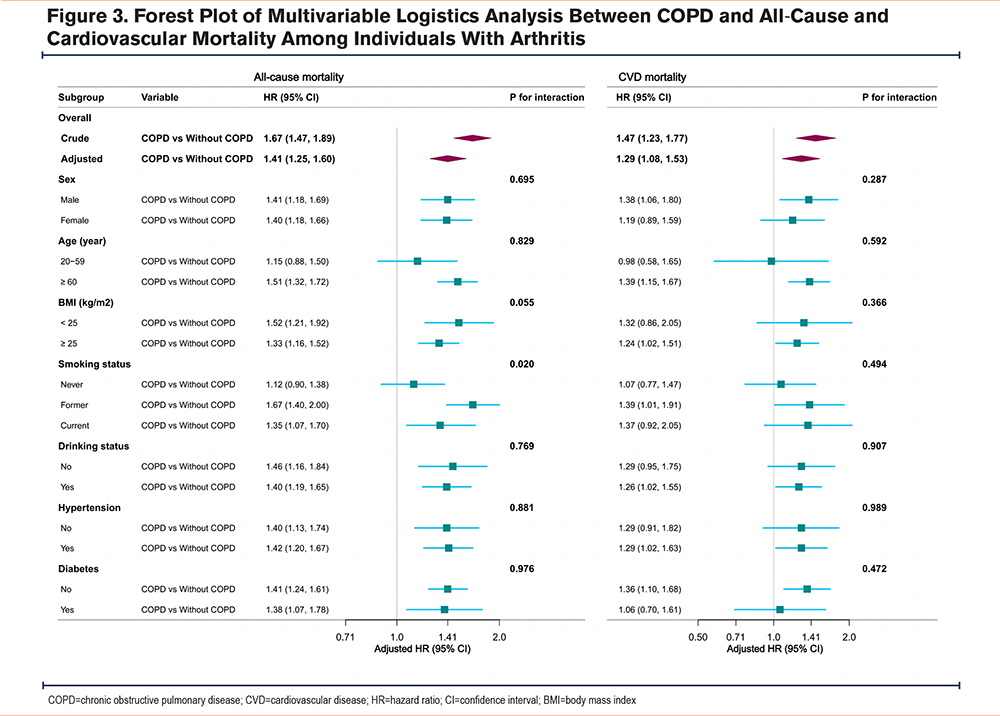
Furthermore, to comprehensively understand the intricate relationship between COPD and arthritis, participants’ mortality, subgroup analyses, and interaction analyses were conducted to explore the associations between COPD and both all-cause and CVD mortality. The subgroup analyses were primarily based on variables such as age (<60 years and ≥ 60 years), sex (male and female), BMI (< 25kg/m2 and ≥ 25kg/m2), smoking status (never, former, current), drinking status (no, yes), hypertension (no, yes), and diabetes (no, yes).
To further validate the robustness of the research findings, a series of sensitivity analyses were conducted. First, given the strong association between COPD and deaths caused by chronic lower respiratory diseases (CLRD), further analyses were performed specifically for deaths attributed to CLRD and those not attributed to CLRD. By calculating the risk ratios of COPD for these 2 types of deaths, the influence of COPD on mortality risk among participants with arthritis was further explored. Additionally, to minimize potential reverse causality bias, participants who died within the first 2 years of follow-up (a total of 426 individuals) were excluded, and the Cox proportional hazards model was rerun based on this adjusted dataset. Lastly, to ensure data stability, multiple imputations were performed for all missing covariates, and sensitivity analyses were conducted based on 5 complete datasets.
All statistical analyses were performed using R Statistical Software (Version 4.2.2, R Foundation; Vienna, Austria) and Free Statistics analysis platform (Version 1.9.2; Beijing, China). Statistical significance was defined as a 2-sided P-value <0.05.
Results
Characteristics of Arthritis Participants
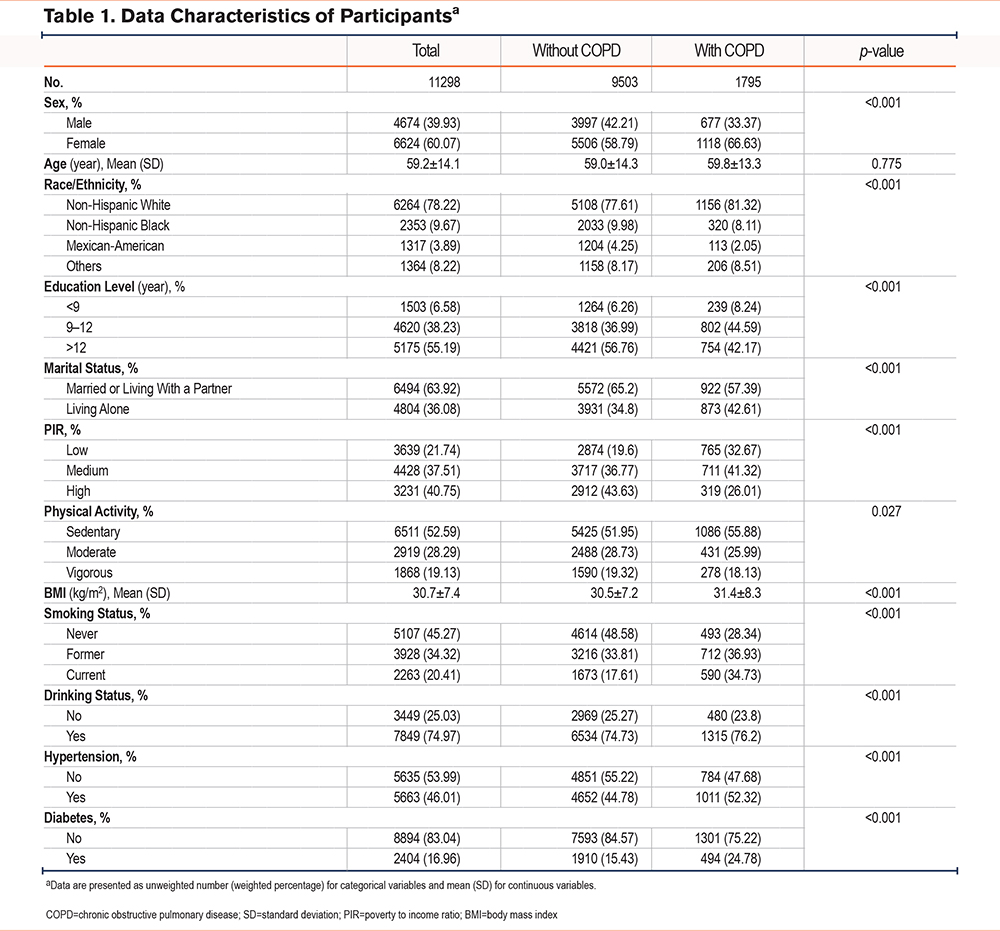
A total of 11,298 participants who self-reported having arthritis were recruited, representing approximately 41.88 million American adults aged 20 and above. The mean age of the participants was 59.2 ± 14.1 years, with a sex distribution of 39.93% male and 60.07% female. Table 1 outlines the baseline characteristics stratified by the presence or absence of COPD. Among participants with arthritis, those who also had COPD were generally older and more likely to be female, non-Hispanic White, have a higher education level, be married or living with a partner, and have a lower household income. These participants tended to be less physically active, have a higher BMI, and have a higher preference for smoking and alcohol consumption. Furthermore, they had a higher prevalence of hypertension but a relatively lower prevalence of diabetes.
Association Between COPD and Mortality
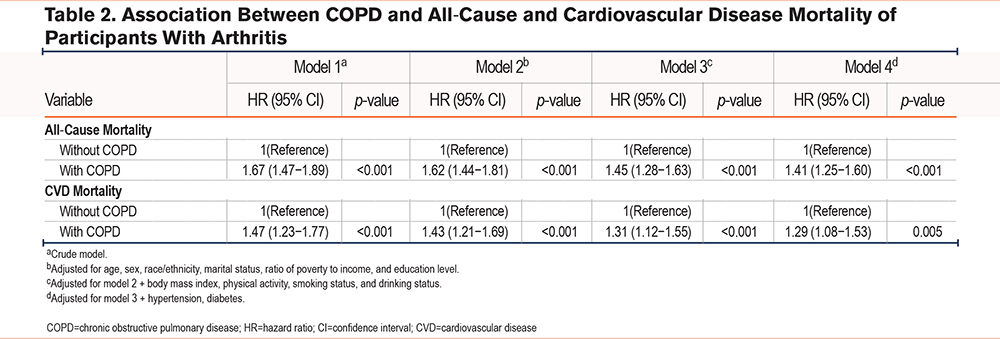
During the average follow-up period of 8.8 years, a total of 3061 all-cause deaths were observed, with 1024 CVD-related. To comprehensively assess the effect of COPD on all-cause and CVD mortality among participants with arthritis, 4 models were constructed for stepwise analysis. In the crude model, compared to arthritis patients without COPD, participants with COPD had an HR of 1.67 (95% CI: 1.47–1.89, p <0.001) for all-cause mortality and an HR of 1.47 (95% CI: 1.23–1.77, p <0.001) for CVD mortality. Even after multivariable adjustment, this association remained significant (see Table 2 for details). Specifically, arthritis patients with COPD had an HR of 1.41 (95% CI: 1.25–1.60, p <0.001) for all-cause mortality and an HR of 1.29 (95% CI: 1.08–1.53, p <0.001) for CVD mortality.
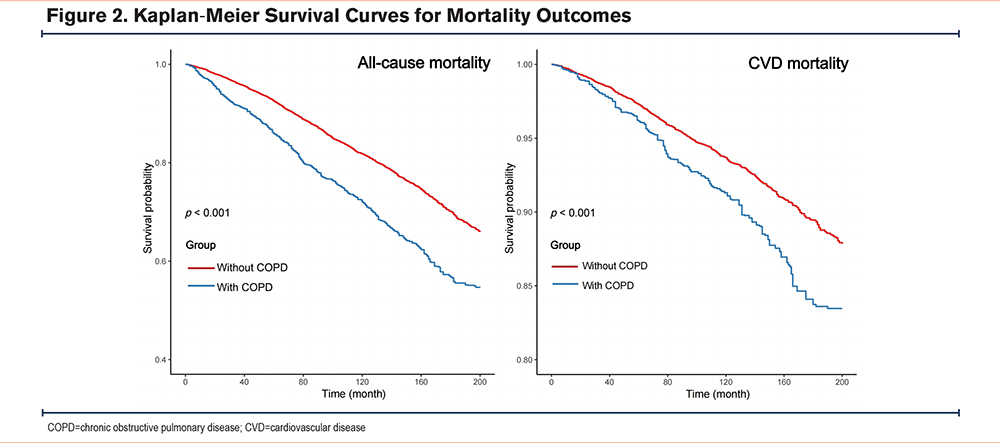
Furthermore, to further validate the significance of this association, Kaplan-Meier survival curves were employed to analyze the crude cumulative all-cause mortality and CVD mortality rates (Figure 2). The results showed that in comparison to arthritis patients without COPD, participants with COPD exhibited significantly elevated all-cause and CVD mortality rates (log-rank test, p <0.001).
Subgroup Analyses and Sensitivity Analyses
Stratified analyses were performed according to sex, age, BMI, smoking status, drinking status, hypertension, and diabetes. After adjusting for all covariates, similar trends were observed across all subgroups (Figure 3). Except for an interaction found in smoking status regarding all-cause mortality (p for interaction=0.020), there were no significant interactions (p for interaction >0.05). This finding suggests that the risk of all-cause mortality among arthritis patients with COPD might be higher in those who smoke. However, due to multiple testing and the similarity in the direction of associations, the clinical significance of this interaction remains to be further elucidated.
In the sensitivity analysis, the causes of death were further categorized into CLRD and non-CLRD to delve deeper into the association between COPD and mortality risk among participants with arthritis. After adjusting for covariates, it was found that COPD significantly increased the risk of CLRD mortality, with an HR of 5.46 (95% CI: 3.48–8.56, p<0.001). Additionally, COPD was also found to be related to an elevated risk of non-CLRD mortality, with an HR of 1.24 (95% CI: 1.07–1.44, p=0.004; Supplementary Table 1 in the online supplement).
To exclude the potential impact of early deaths on the results, participants who died within the first 2 years of follow-up were excluded. Under this condition, the elevated risks of all-cause and CVD mortality among arthritis patients with COPD did not change substantially. Compared to participants without COPD, those with COPD exhibited higher risks of all-cause and CVD mortality (Supplementary Table 2 in the online supplement). The adjusted HR for all-cause mortality was 1.31 (95% CI: 1.13–1.52, p <0.001), and for CVD mortality, it was 1.35 (95% CI: 1.09–1.67, p=0.006).
To address potential data missingness, multiple imputation was performed for all missing covariates, and analyses were conducted on 5 imputed datasets. The results indicated that our main findings remained stable (Supplementary Figure 1 in the online supplement).
Discussion
In this prospective cohort study with an average follow-up of 8.8 years, we revealed a significant association between COPD and both all-cause and CVD mortality among participants with arthritis. This finding not only underscores the traditional understanding that COPD increases the risk of lower respiratory infection mortality but also explicitly points out that COPD similarly elevates the risk of non-lower respiratory infection mortality. This is crucial for comprehensively understanding the impact of COPD on the prognosis of arthritis patients.
Previous studies have shown a positive correlation between COPD and arthritis. Specifically, Ni et al found in Chinese elderly individuals that arthritis is positively associated with the risk of developing lung diseases.35 Chung et al discovered in a study involving 46,030 RA patients in Korea that RA is linked to an increased risk of COPD development, which further increases with a higher seropositive rate.36 Similarly, Liu et al reported that arthritis is linked to a greater prevalence of COPD among adult populations in the United States.37 In a recent study utilizing the U.K. Biobank Resource, Yang et al identified a significant bidirectional association between RA and COPD, partially mediated by systemic inflammation.38 Hyldgaard et al conducted an extensive analysis of 31,333 RA patients in Denmark and found that the mortality rate significantly increases when RA patients have comorbid COPD.10 The 5-year mortality rate for patients with both RA and COPD is 41.9%, compared to 20.5% for patients with RA alone.39 Furthermore, an analysis by Nikiphorou et al of 6591 RA patients in the United Kingdom also revealed that COPD is associated with mortality (HR 2.84, 95% CI 1.13–7.12), indicating that COPD is a major predictor of early death among patients with early RA.11 However, these studies mainly focus on specific regions or populations, and there is a lack of thorough investigation into this relationship within the broader populace of the United States.
This study fills a knowledge gap by employing a large-scale, long-term follow-up, multiethnic cohort design. We found that COPD is not only associated with an increased risk of all-cause mortality and CVD mortality among patients with arthritis but also with various causes of death, including lower respiratory infections and non-lower respiratory infections. This indicates that the influence of COPD on the outcome of arthritis patients may involve a broader range of pathophysiological mechanisms. On one hand, COPD patients, due to chronic dyspnea and systemic inflammatory responses, may be more prone to developing musculoskeletal system diseases.40 On the other hand, arthritis patients, experiencing pain, limited mobility, and reduced quality of life, may be more susceptible to lung infections and other COPD-related complications, thereby, further increasing their risk of mortality.13 Additionally, COPD and arthritis share common risk factors such as smoking, air pollution, and genetic factors (e.g., the HLA-DRB1 gene), which may exacerbate their interaction.41-43 Beyond recognized inflammatory arthritis, osteoarthritis is also considered a chronic low-grade inflammatory condition that can trigger multiple pathological changes, further supporting the complex interplay between COPD and arthritis.44 Persistent arthritis may induce immune cell infiltration and activation, leading to airway and alveolar epithelial cell damage.45,46 The immune dysfunction, T helper cell (Th)1/Th2 imbalance, and the potential role of Th17 cell immunity in RA patients may also hold significant importance in bridging the pathological processes of RA and COPD.47
This study represents the inaugural investigation into the association between COPD and mortality rates among adult arthritis participants in the United States. Furthermore, multiple potential confounding factors, including baseline characteristics, lifestyle factors, and comorbidities, were adjusted to enhance the accuracy of the findings. However, there are several limitations to be considered. First, due to its observational nature, this study cannot directly establish a causal link between COPD and mortality. Secondly, our study faces the potential for misclassification of COPD and arthritis due to inconsistencies in diagnostic criteria across different health care providers and settings. Even though we adhered to CDC recommendations by utilizing self-reported and physician-diagnosed data for our case definitions, these variations in diagnostic criteria could introduce bias and impact the accuracy of our disease status estimation. This, in turn, may affect the reliability of our findings related to COPD and arthritis. Additionally, the current study did not collect detailed information on the severity of COPD, which limits our understanding of the relationship between disease progression.
In summary, the findings of this study indicate that COPD significantly increases the risk of mortality among arthritis patients. These results not only offer valuable insights into the intricate relationship between COPD and arthritis but also imply that clinicians should adopt a more holistic approach to managing these patients, prioritizing the identification and management of comorbidities that may exacerbate clinical outcomes. Specifically, screening for COPD among arthritis patients, allowing for early detection and intervention, may emerge as an effective strategy to prevent disease progression and enhance patients' lung function and quality of life. Therefore, it is imperative for future research to further explore this area, including the relationship between different stages of COPD and arthritis prognosis, with the ultimate goal of providing more comprehensive and effective strategies and methods for the prevention and management of these diseases.
Acknowledgements
Author contributions: YZ was responsible for data curation, formal analysis, investigation, project administration, visualization, funding acquisition, and writing the original draft of the manuscript. GC was responsible for data curation, investigation, project administration, and writing the original draft of the manuscript. AH was responsible for visualization, data curation, and writing the original draft of the manuscript. YH was responsible for conceptualization, methodology, supervision, validation, and writing, reviewing, and editing the manuscript. CF was responsible for conceptualization, methodology, project administration, data curation, resources, supervision, validation, and writing, reviewing, and editing the manuscript. All authors agreed to submit the article to this journal and agreed to be accountable for all aspects of the work.
Data sharing statement: Data of publicly available datasets was analyzed in this study. All data are available on the NHANES website (https://www.cdc.gov/nchs/nhanes/).
Other acknowledgments: The authors express their sincere thanks to those who developed and maintain the database, and to the clinical scientist team for their ongoing support and insightful guidance.
Declaration of Interests
The authors declare no competing interests.