Running Head: Virtual PR in Oxygen-Dependent COPD Patients
Funding support: Dr. Buhr is supported by the National Institutes of Health/National Heart, Lung, and Blood Institute award L30HL134025 and the Solovy Award for Advancement in COPD from the Respiratory Health Foundation, indirectly related to this work.
Date of Acceptance: February 7, 2025 │Online Publication Date: February 28, 2025
Abbreviations: 1MSTS=1-minute sit-to-stand; CAT=COPD Assessment Test; CI=confidence interval; COPD=chronic obstructive pulmonary disease; GOLD=Global initiative for chronic Obstructive Lung Disease; IQR=interquartile range; MCID=Minimal clinically important difference; mMRC=modified Medical Research Council; PHQ-9=Patient Health Questionnaire-9; PR=pulmonary rehabilitation
Citation: Filizola H, Kumar A, Buhr RG, Schwab Jensen K. Outcomes of virtual pulmonary rehabilitation in oxygen-dependent COPD patients. Chronic Obstr Pulm Dis. 2025; 12(2): 184-189. doi: http://doi.org/10.15326/jcopdf.2024.0572
Introduction
Although pulmonary rehabilitation (PR) has been shown to improve quality of life, hospital readmission rates, and mortality in patients with chronic obstructive pulmonary disease (COPD), it remains widely underutilized, particularly for those at the highest risk for decompensation.1,2 Patient factors associated with decreased attendance to traditional PR include long-term oxygen use, higher frailty, increased travel distance, decreased social support, active smoking, and lower socioeconomic status.3,4
Virtual PR, defined as PR delivery via a home-based telehealth model, may offer an attractive alternative in this landscape. Studies suggest that virtual PR confers comparable benefits to traditional PR, and the 2023 American Thoracic Society guidelines now recommend that providers consider offering virtual PR as an option to patients with stable chronic respiratory disease when traditional pulmonary rehabilitation is not as accessible or feasible.2,5-8
Currently, there is global heterogeneity in virtual PR programs, with a lack of standardized quality metrics and uncertainty regarding the optimal model for virtual PR. Furthermore, neither the safety nor effectiveness of virtual PR is established for patients with advanced disease and higher disease severity, particularly those requiring supplemental oxygen. We, thus, aimed to compare the outcomes of virtual PR in patients requiring oxygen to those not requiring oxygen.
Methods
We conducted a retrospective review of all patients with COPD who enrolled and completed a virtual PR program through a telehealth pulmonary rehabilitation company (Kivo Health; San Francisco, California) from October 2022 to November 2023. All patients were referred at the discretion of their treating pulmonologist and had to be on less than 5 liters of oxygen to be included in the program. At enrollment, all patients had baseline pulmonary function testing and a physician-adjudicated diagnosis of COPD. The decision of whether patients were safe for a virtual mode of pulmonary rehabilitation at the time of the referral was guided by patient-specific factors at the clinician's discretion.
This virtual PR program was developed by experienced respiratory therapists and exercise physiologists from American Association of Cardiovascular and Pulmonary Rehabilitation certified programs.9 Patients began with a 1:1 intake appointment to create an individualized exercise plan, which included moderate-to-high-intensity aerobic exercise that progressively increased over time. Classes were led by a respiratory therapist in small groups of 2–5 patients via a 2-way audiovisual platform, with real-time monitoring of heart rate and oxygen levels using a pulse oximeter wristwatch. Intensity was tracked through heart rate and modified Borg scores. The training program also incorporated resistance training with bands and discussions on key pulmonary rehabilitation topics. The program lasted 8 weeks, with 16 semiweekly sessions of 90 minutes each.
Demographic and clinical metrics were collected virtually through enrollment and exit surveys. Patients were further divided based on their need for supplemental oxygen during PR. The primary outcome was program attendance. Secondary outcomes included adverse events and clinical endpoints, including change in COPD Assessment Test (CAT) score,10 modified Medical Research Council (mMRC) dyspnea scale,11 Patient Health Questionnaire-9 (PHQ-9),12 and 1-minute sit-to-stand (1MSTS).13
Analyses were conducted in Stata 16.1 (StataCorp; College Station, Texas). Categorical variables were compared using Fisher’s exact tests, and continuous variables using Wilcoxon rank-sum tests. We performed panel linear regressions for patient-reported outcomes and a zero-inflated negative binomial regression with clustered standard errors for 1MSTS. To explore differences between those who were and were not oxygen users, we fit a difference-in-differences analysis, interacting time with oxygen use at baseline. We estimated at least 80% statistical power for our 4 outcomes based on our sample of 167 patients to minimally detect an effect size of 0.225 for mMRC, 1.6 for CAT, 1.05 for PHQ-9, and 1.4 for 1MSTS. Marginal predicted estimates were derived, and confidence intervals were estimated using Bonferroni adjustment for multiple comparisons. Complete case analyses were employed for all models. All study procedures were approved by the University of California Los Angeles Institutional Review Board (IRB 23-1267), with a waiver of informed consent. All data were furnished to the investigators from Kivo Health under a preexisting data use agreement, and all study procedures and analyses were designed and executed by the investigators without input from Kivo Health personnel.
Results
A total of 167 patients with complete data (out of 173 eligible) were included in the study, of which 107 required oxygen with exertion and 60 did not. Patients requiring oxygen had more advanced COPD based on Global initiative for chronic Obstructive Pulmonary Disease (GOLD)14 stage than the nonoxygen group and higher baseline dyspnea scores based on CAT; otherwise, there were no significant differences between the 2 groups (Table 1).
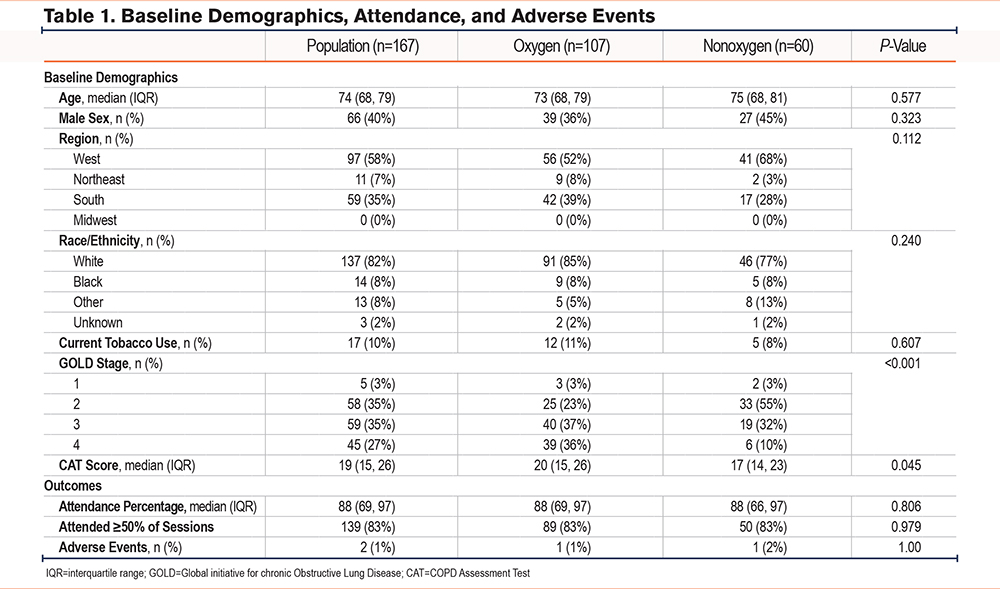
The median program attendance was 88%, with no significant difference between the oxygen and nonoxygen groups, respectively (Table 1). Aside from smoking status, no other significant differences in demographics (age, sex, region, race/ethnicity, and GOLD stage) were observed to be associated with attendance. Adverse events were noted in only 2 (1%) participants: one in the oxygen and one in the nonoxygen group. The patient in the oxygen group experienced symptomatic bradycardia and was advised to follow up with cardiology before restarting the program; the patient in the nonoxygen group experienced asymptomatic hypertension but was able to complete the program. We defined completion as attending ≥50% of available sessions, of which 139 (83%) completed. When comparing those who did or did not complete at least 50% of sessions, there were no significant differences observed for age, sex, race/ethnicity, COPD stage, or oxygen use; those still actively smoking were less likely to complete the program (75% versus 93% in those not smoking, P=0.004).
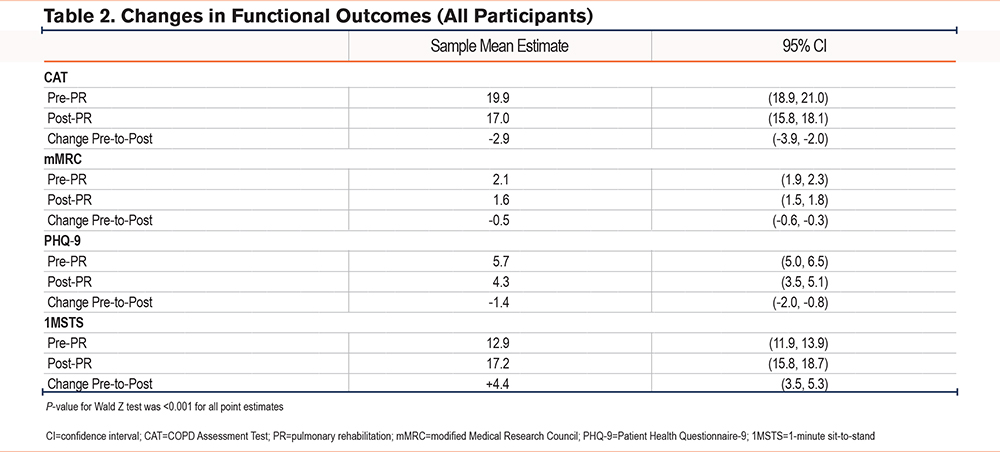
All functional outcomes showed significant improvements following PR. Amongst all patients, the CAT score improved by 2.9 points, the mMRC by 0.5 points, the PHQ-9 by 1.4 points, and the 1MSTS by 4.4 repetitions (P<0.001 for all outcomes) (Table 2). Additionally, 7 patients went from being unable to perform any 1MSTS repetitions at program onset to being able to perform repetitions upon program completion.
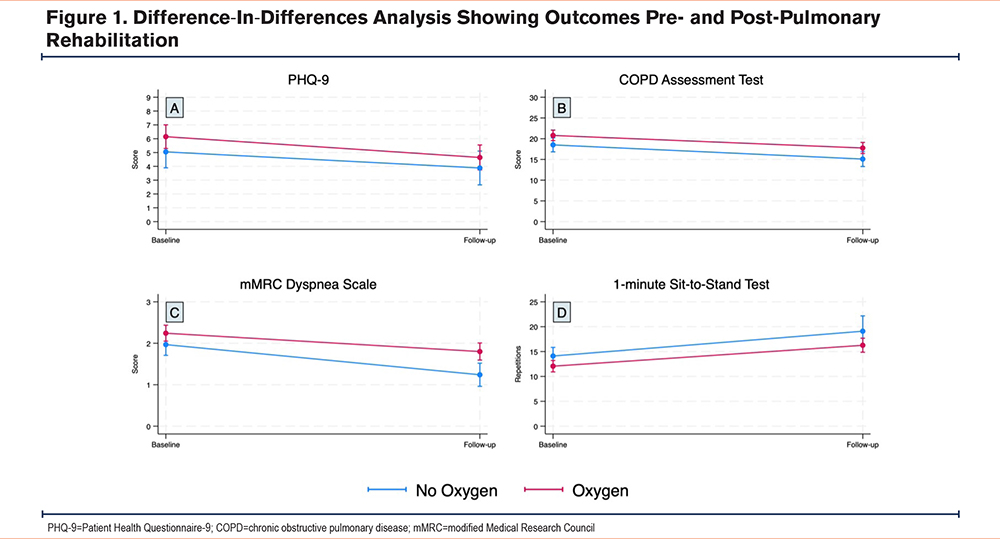
When comparing the oxygen-dependent and nonoxygen groups, there were no significant differences in the degree of improvement for CAT, PHQ-9, and 1MSTS (Figure 1). For mMRC, those on oxygen improved by 0.3 fewer points than those not on oxygen (P=0.052).
Discussion
This retrospective analysis suggests that virtual PR is feasible, safe, and effective for COPD patients on oxygen. The oxygen group, with significantly higher baseline dyspnea scores and a higher proportion of severe COPD, represents a population with an expected higher disease burden. The comparable attendance rates and completion rates between groups speak to the feasibility and acceptability of virtual PR in this sicker population. Importantly, our study suggests that this may not come at a risk to patient safety, as 99% of participants safely participated without experiencing an adverse event, and there was no difference in risk between the 2 groups. Patients who were actively smoking were less likely to complete the program, which has also been found in prior studies.3,4
Importantly, both groups also showed comparable improvements in clinical outcomes. These outcomes improved by similar ranges to prior studies,2 and the improvements approached or exceeded the established minimal clinically important difference (MCID) values for CAT,15 mMRC,16 and 1MSTS17 (MCID for CAT=2, with our patients improving by 2.9; MCID for mMRC = 0.5, with our patients improving by 0.5, MCID for 1MSTS=3, with our patients improving by 4.4). While the MCID for PHQ-9 is harder to define and depends upon baseline severity,18 we found a significant improvement in PHQ-9 from 5.7 to 4.3, with scores less than 5 suggestive of no clinical depression.
Limitations include potential selection bias due to the retrospective nature of the data and the small sample size. Additionally, the study's generalizability may be limited by the heterogeneity of PR programs and the characteristics of the study population, which consisted of individuals referred to a private virtual PR company from both academic and nonacademic settings. Nonetheless, given the limited availability of noncommercial virtual PR options, this may more accurately reflect the “real-world” scenario for many patients. Finally, post-PR measurements were missing in some patients with lower attendance, though our regression analysis did not find any significant demographic differences (aside from smoking status) to be associated with attendance. Strengths include the broad geographic sampling, the standardization of the virtual PR regimen used, and the high burden of illness in our patient sample. To our knowledge, this is the first study to compare outcomes of virtual PR in patients on and off oxygen, as prior studies have excluded patients on oxygen5 or not stratified by oxygen use.6,8 A recent observational study comparing 2-way audiovisual PR with traditional PR found this method to be safe, feasible, and effective in significantly expanding geographic reach. However, the authors noted a relevant limitation, which was a smaller proportion of individuals in the virtual PR group required oxygen.8
In conclusion, our study suggests that oxygen-dependent patients can safely undergo virtual PR and benefit as much as nonoxygen-dependent patients. While larger trials are needed to confirm our findings, this offers hope for reducing health disparities in COPD and contributes to the growing literature on virtual PR to help individualize treatment decisions moving forward.
Acknowledgments
Author contributions: All authors had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the analysis. All authors contributed to the conception and design of the study and the drafting of the manuscript. All authors approved this version of the manuscript to be published. This data has not been previously published in a scientific journal.
The authors acknowledge Victor Sadauskas and the Kivo Health team for provision of the data.
Declaration of Interest
HF, AK, and KSJ report nothing to disclose. RGB reports personal consulting fees from Chiesi, Optum, Dynamed, and the American College of Physicians, not related to this work. RGB is employed by the Veterans Health Administration. This work does not necessarily represent the views and opinions of the Department of Veterans Affairs.
Kivo Health is a telehealth pulmonary rehabilitation company that accepts referrals from physicians to enroll chronic lung disease patients into virtual PR. The company frequently works with the University of California, Los Angeles (UCLA) patients who are referred by UCLA physicians. There are no conflicts of interests and neither the study authors nor Kivo Health received any form of compensation or incentives to perform this study. Kivo Health provided the data to the investigators but had no input on the study design, analysis, or interpretation of the results, nor the decision to publish.
Kivo Health takes responsibility for the integrity and accuracy of the data provided for analysis.