Running Head: Patient Survey of COPD Experience
Funding Support: This study was funded by Verona Pharma, plc., which contributed to its design. Medical writing assistance was also funded by Verona Pharma, plc.
Date of Acceptance: May 30, 2025 | Published Online: June 9, 2025
Abbreviations: COPD=chronic obstructive pulmonary disease; EHR=electronic health record; HCP=health care provider; ICSs=inhaled corticosteroids; IRB=institutional review board; SD=standard deviation
Citation: Mannino DM, Trac S, Seth J, Dixon A, Aggarwal K, Kuhn B. Patient burden and insights in COPD: a survey analysis. Chronic Obstr Pulm Dis. 2025; 12(4): 317-327. doi: http://doi.org/10.15326/jcopdf.2025.0616
Online Supplemental Material: Read Online Supplemental Material (792KB)
Introduction
Chronic obstructive pulmonary disease (COPD) is a common lung disease that causes persistent yet dynamic airflow obstruction1 due to chronic inflammation of the respiratory tract, airway remodeling, and excessive mucus production.2-5 In the United States, COPD affects 16 million people and is listed as the sixth leading cause of death.6 COPD is a highly underdiagnosed disease, as more than 50% of adults with impaired pulmonary function are not aware that they have COPD.7 Current pharmacotherapy for COPD consists of bronchodilators to open the airways and inhaled corticosteroids (ICSs) to reduce airway inflammation.5 Select patient phenotypes may be eligible for treatment to reduce exacerbations with roflumilast or azithromycin.5 Even when treated with these therapies, patients experience persistent worsening of symptoms and recurring exacerbations, significantly impacting their quality of life.8,9
Studies have shown that patient–provider discussions are essential for achieving more effective and timely management of COPD, as effective communication can lead to more accurate symptom reporting, better adherence to treatment plans, and improved overall disease management to prevent future exacerbations and hospitalizations.10,11 Furthermore, the Global Initiative for Chronic Obstructive Lung Disease 2025 Report emphasizes the importance of selecting optimal inhaler therapy based on patient needs and of regularly reassessing handling techniques.5 Therefore, efforts to build a greater understanding and awareness of patients’ perceptions of COPD and their interactions with their health care providers (HCPs) are warranted in order to better manage treatment and outcomes in this large patient population.
The Phreesia PatientInsights survey leverages aggregated information collected with consent on an electronic intake platform to deliver customized surveys to key patient populations. Phreesia is used across a variety of health care organizations, including doctors’ offices, specialty practices, hospitals, and health systems. Over 4000 health care organizations use Phreesia across all 50 states, which totals 150 million patient visits annually. For this study, the survey aimed to collect self-reported insights from patients with COPD to explore their symptom experience and impact. The survey also sought to identify gaps in patients’ knowledge of COPD and their abilities to communicate effectively with their HCPs about their symptoms. Finally, this survey analysis explored COPD patients’ treatment journeys, particularly concerning maintenance medications and experiences with treatment devices.
Methods
Study Overview
In January 2025, Phreesia conducted a quantitative survey of patients diagnosed with COPD. The survey was conducted for 20 days to allow adequate sample sizes for questions only shown to select patients. Respondents had to indicate their COPD diagnosis to proceed with the survey; those who did not select COPD as a condition they had been diagnosed with were excluded from the survey.
Study Participation and Survey Administration
The survey was offered to Phreesia platform users who had a diagnosis and/or treatment of COPD indicated in their electronic health record (EHR). The survey was administered digitally to individuals after the check-in process for their doctor’s appointment using the Phreesia platform. Individuals using the Phreesia platform are presented with an optional Health Insurance Portability and Accountability Act authorization. The information of those who consented was analyzed, and those who qualified were given the opportunity to complete the survey. Respondents had to sign an additional consent form to start the survey. Participation was voluntary, and respondents who began the survey could exit it at any time. The study was reviewed by Advarra Institutional Review Board (IRB) (#00000971) and was determined to be exempt from IRB oversight. Study participants provided informed consent prior to completing the survey. The full survey can be found in the online supplemental material.
Survey Design
The survey, which comprised a total of 28 questions, used single-choice, multiple-choice, and slider question/answer formats. Some questions were intentionally shown only to certain respondents depending on their selections within the survey. Respondents were required to answer every question before continuing, and a “decline to answer” response option was included for every question. Partial responses were collected and included in the study. Demographic data were derived from a patient’s EHR to allow for the segmentation of survey results by sex, age, race, and ethnicity. “Decline to answer” options for each question were excluded from the results.
Sampling Technique
The sampling technique was a combination approach that included elements of random sampling, convenience, and volunteer sampling. Only patients who had visits between January 6 and 26, 2025, limited to practices utilizing Phreesia, had the opportunity to participate in the survey. Patients from across the United States had the opportunity to participate; although the survey was not restricted geographically, it was dependent on where these patient check-ins were taking place. The study did not have predetermined demographic quotas.
Statistical Methods
Categorical variables were summarized using frequency and percentages, and continuous variables were summarized using mean (standard deviation [SD]). Between-group comparisons were made using Chi-square tests to assess group differences at the 95% confidence level, with P<0.05 considered significant.
Results
Survey Sample Demographics
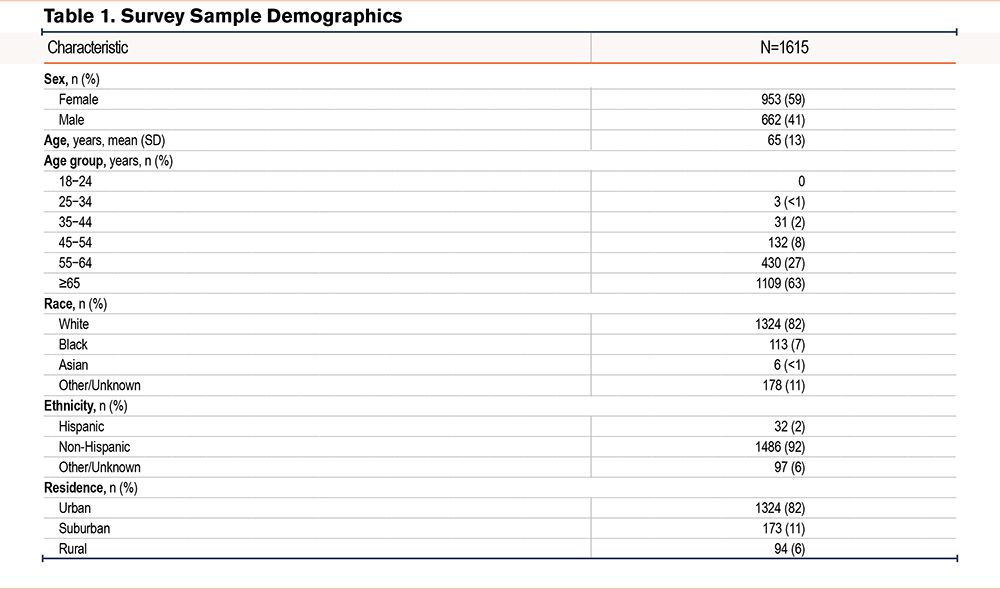
The survey was offered to 31,903 patients diagnosed with COPD who checked in for any medical appointments during the specified timeframe. Of these patients, 4537 consented yes to the survey and 1615 completed it, resulting in a response rate of 5.1%. Overall patient demographics collected from each patient’s EHR are shown in Table 1. Most patients were female (59%) and identified as White (82%). The mean (SD) patient age was 65 (13) years.
Symptom Experience
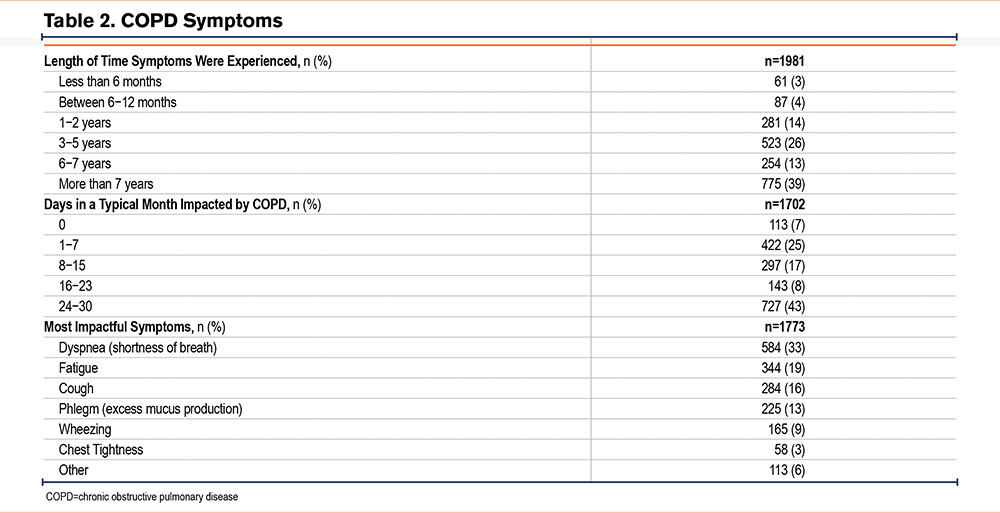
At the time of the survey, 39% of patients had experienced COPD symptoms for more than 7 years (Table 2). Additionally, 43% of patients reported experiencing symptoms for at least 24 days in a typical month, and 25% of patients experienced symptoms for all 30 days of the month. Dyspnea was identified as the most disruptive symptom by 33% of patients, followed by fatigue (19%), cough (16%), and phlegm (13%). Other symptoms not specified in the survey were experienced by 6% of patients.
Impact on Quality of Life
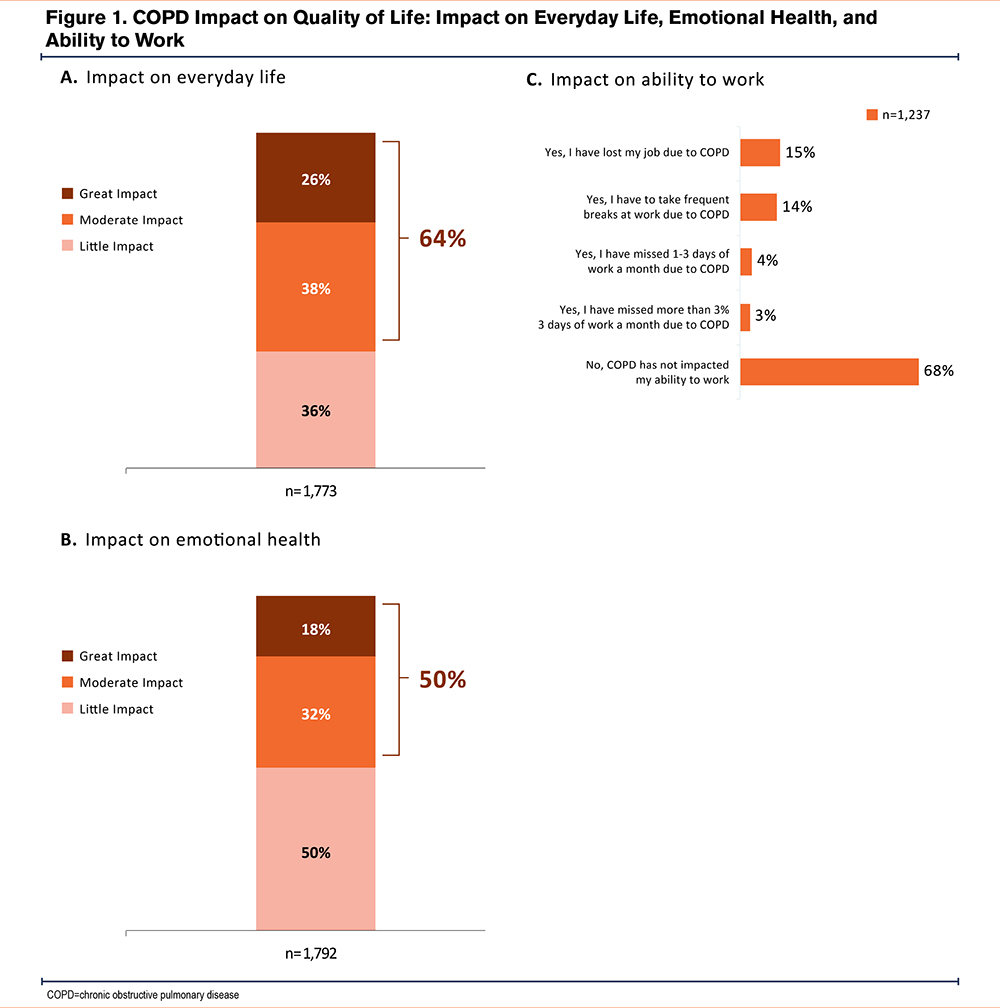
A total of 64% of patients reported a moderate-to-great impact of COPD on their daily lives (Figure 1A). Additionally, 50% reported a moderate-to-great impact on their emotional health (Figure 1B). Younger patients (aged 45−64 years) were much more likely to report a moderate-to-great impact on their emotional health (63% versus 43% of those aged ≥65 years). Moreover, 36% of patients reported that their COPD had impacted their ability to work, and 15% of patients had lost their jobs due to COPD (Figure 1C). Patients currently on maintenance medication were more likely to report a higher impact of COPD on their daily lives (68%) and emotional health (52%) compared to those not on maintenance medications (53% and 39%, respectively), while those not on maintenance medications for their COPD were more likely to report that COPD had minimal impact on their daily lives and emotional health (Table S1 in the online supplement). Associations between demographic variables and key survey responses on the COPD impact on quality of life are detailed in Table S2 in the online supplement.
HCP Interactions
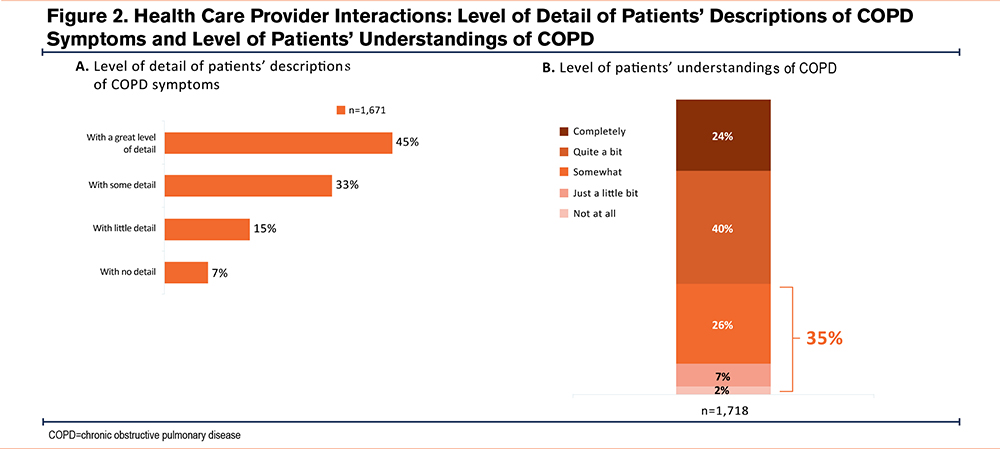
Survey findings highlighted a need for improved communication between patients and their HCPs. Only 45% of patients engaged in detailed discussions about their COPD symptoms with their HCPs (Figure 2A). Indeed, 22% of patients provided little or no detail when describing their COPD symptoms to their main HCPs who treated their COPD, which could lead to awareness gaps for HCPs that could hinder comprehensive care. Patients aged 45−64 years used a greater level of detail than patients aged ≥65 years (49% versus 42%, respectively; P<0.05). Additional results support the finding that a patient’s knowledge level about their COPD remains low (Figure 2B). A total of 35% of patients expressed having limited or no understanding of COPD. Patients who identified as Black (46% versus 35% of patients who identified as White; P<0.05) and patients aged 45−64 years (41% versus 33% of those aged ≥65 years; P<0.05) were more likely to have limited or no understanding of their COPD. Associations between demographic variables and key survey responses on patient−HCP interactions are detailed in Table S2 in the online supplement.
Treatment Journey
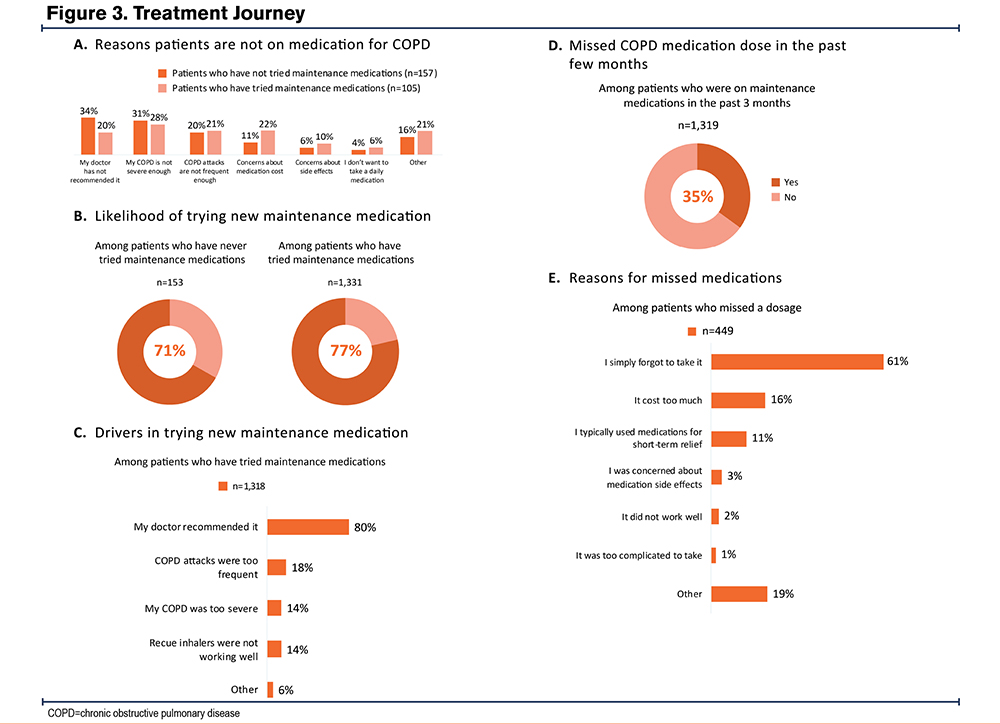
Among patients who had not tried maintenance medications or who were currently not on any maintenance medications (n=339; 21% of total), 27% said that their COPD was not severe enough, and 27% said that their HCP did not recommend it (Figure S1 in the online supplement). Although most patients had discussed rescue inhalers and maintenance medications for their COPD, 6% had never discussed these standard treatments (Figure S2 in the online supplement). A total of 11% of surveyed patients had not tried any maintenance medications, and among those who had tried maintenance medications, 8% were not currently on any. The perception that their COPD was not severe enough and a lack of HCP recommendation were the leading reasons why patients were not on maintenance medications (Figure 3A). Among patients who had not tried any medications for their COPD, 71% expressed that they were likely to try maintenance medications. Interestingly, 77% of those who had tried maintenance medications were open to exploring new options (Figure 3B). Among patients who had tried maintenance medications, the primary factor influencing a patient’s decision to start was an HCP recommendation, which largely outweighed other factors such as increased frequency of COPD exacerbations or worsening COPD severity (Figure 3C). In general, patients with COPD who were on maintenance medications were consistent in taking their medication; however, 35% of patients had missed a dose of their COPD medication in the past few months (Figure 3D). Of those who had missed a dose, 61% reported that they “simply forgot to take it,” and 16% said that the medications were too costly (Figure 3E).
Devices for COPD Medication Delivery
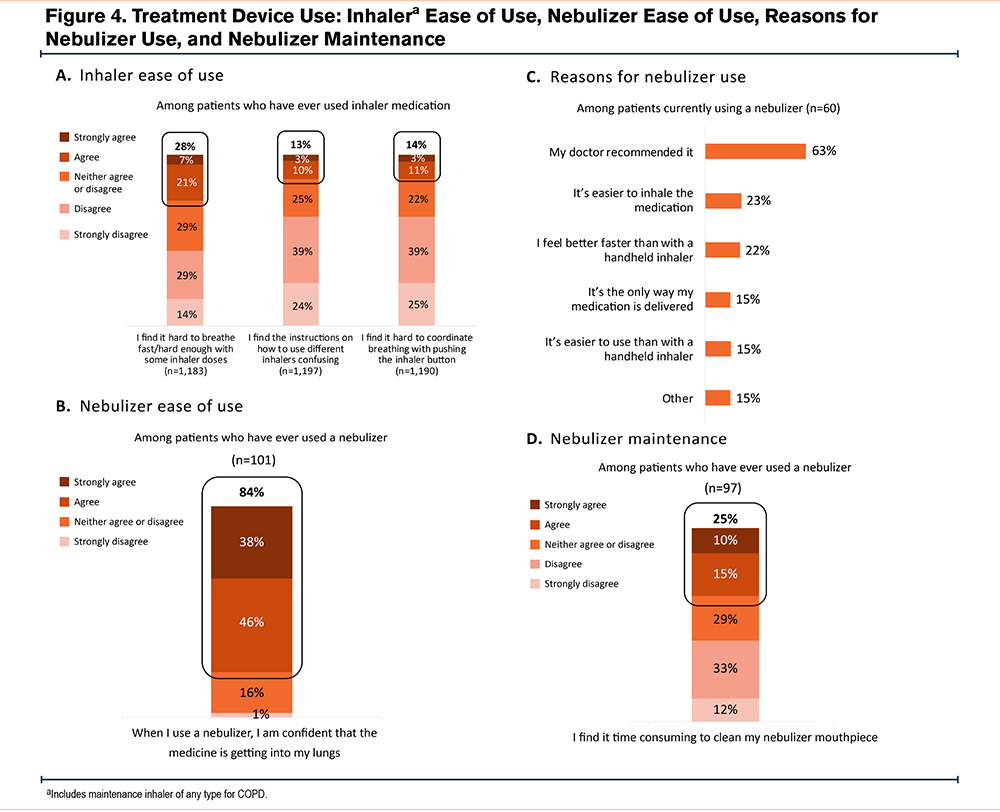
Of patients who had tried COPD medications, rescue inhalers were the primary type patients had discussed and tried, with the majority of patients aged 45−64 years having tried them (78% versus 71% of patients aged ≥65 years; P<0.05). Most patients who had used an inhaler medication did not report issues surrounding the inhaler technique (Figure 4A). However, 28% of these patients acknowledged experiencing occasional challenges in breathing quickly or forcefully enough with their inhaler. Patients were less likely to report difficulties following instructions (13%) or coordinating their breathing while using the inhaler (14%). Among patients with COPD who had used a nebulizer at some point, 84% felt confident that the medicine reached their lungs (Figure 4B). A total of 63% of patients with COPD were using a nebulizer because of an HCP recommendation. Other reasons for usage included feelings of ease of use (15%) or faster relief than a handheld inhaler (22%; Figure 4C). However, 25% of patients found cleaning their nebulizer mouthpiece time-consuming (Figure 4D).
Discussion
This Phreesia study underscores the ongoing challenges patients with COPD in the United States face, demonstrating the need for comprehensive support and interventions to improve a patient’s quality of life. In this PatientInsights survey, patients reported that they continue to endure a great impact of symptoms that disrupt their daily and professional lives and negatively affect their emotional health. Moreover, patients aged 45−64 years versus patients aged ≥65 years reported more impact on their emotional health. Historically, COPD has been approached with a “nihilistic” attitude, likely causing HCPs to set low expectations for what improvements they can expect for their patients.12 The chronic and progressive nature of COPD may be a roadblock keeping patients from attaining realistic, measurable goals. Moreover, the fact that limited pharmacotherapeutic options exist beyond maximal bronchodilation and ICSs may have added to this attitude. As such, there exists a need for additional treatment options and a more unified agreement on treatment goals for COPD between HCPs and patients.
Results from this survey indicate that there are several elements that influence patients’ decisions regarding their own care and treatment options. The finding that the majority (77%) of patients who have tried maintenance medications would be willing to try another therapy may indicate that patients may not have known what to expect from their medications or that they may be unsatisfied with their current therapy. Moreover, the majority (71%) of patients who have not tried maintenance medications are open to trying one. Interestingly, patients who were currently on maintenance medications were more likely to report a higher impact of COPD on their daily lives (68%) and emotional well-being (52%) compared to those not on maintenance medications (53% and 39%, respectively). This could be an indication that patients on maintenance medications had more severe COPD, which is supported by another survey question wherein 27% of patients who had not tried or were not currently on any maintenance medication said that their COPD was not severe enough. Conversely, patients who were actively managing their COPD with medication may have been more attuned to the disease’s impact on their daily lives and emotional health. The finding that an HCP recommendation is the leading factor influencing patients’ decisions to try a new maintenance medication─even outweighing the frequency of COPD exacerbations or worsening disease severity─is promising and illustrates the power of HCP influence. Despite the implication that HCP influence is paramount, less than half of patients discussed their symptoms in great detail with the HCP who treated their COPD, and a large proportion of patients admitted to having limited-to-no understanding of their disease. Results from the survey also suggest suboptimal HCP awareness of the level of severity of their patients’ COPD. Aside from the communication gaps that exist between HCPs and their patients, it was found that 16% of patients who missed a dose of their COPD medication chose not to take it due to the underlying costs. While only 35% of patients in this study reported that they missed a dose of medication within the past few months, data from retrospective cohort studies indicate low adherence values of 15%−30%, depending on the type of medication, indicating possible inconsistencies in the patient perspective of the use of their COPD medication.13,14 Moreover, although a majority of patients reported using inhalers versus nebulizers for their COPD medication delivery, a large proportion (84%) of patients who used a nebulizer believed the medication reached their lungs. Interestingly, a low proportion of patients (28%) reported that they had difficulty using their inhaler devices, which is contrary to current literature suggesting that most patients do not have proper inhaler techniques.15,16 This may be attributed to the different perceptions of patients versus HCPs on discussing inhaler techniques for COPD medication, as data from another real-world study show that physicians reported lower confidence in their patients’ ability to use their inhaler devices correctly compared to patients’ self-reported confidence.17 Therefore, a limitation of the self-reported inhaler technique is that the patient may not realize their technique is incorrect. There remains a need for open dialogue between patients with COPD and their HCPs, including disease education, device or technique instruction, and observation. Future survey adaptations should, therefore, include questions about receiving inhaler education and observation of their use.
Currently, there exists an opportunity to improve communication between patients and HCPs and increase patient education. Provider visits may not be as effective due to factors such as limited patient knowledge of their condition, high numbers of comorbidities afflicting patients with COPD, and time constraints that HCPs have for any given patient visit. These potential gaps—both in available, appropriate therapies and in the needs/assessment of the patients—for HCPs could hinder comprehensive care. Of note, patients who identify as Black and patients aged 45−64 years were more likely than patients who identify as White and patients aged ≥65 years, respectively, to have limited or no understanding of their condition, highlighting specific demographic groups who could benefit the most from targeted efforts to close the knowledge gap. These types of racial and age disparities have been reflected in clinical outcomes of various diseases across the United States, including type 2 diabetes, heart disease, and asthma.18-23 Potential solutions to reduce disparities in these cases could be applied to COPD as well, including earlier detection and intervention, and making health care more accessible and affordable to those specific demographic groups who would benefit the most.24 There is also a need for more nuanced conversations between patients and their HCPs to make the best use of their limited time together. Patients have expressed the desire for more productive HCP visits facilitated by detailed discussion guides that can prompt insightful conversations about their COPD.25,26 In light of this, there is evidence that standardized management of patients with COPD in disease-specific clinics versus in primary care clinics may afford more keen awareness of the care needed and yield more patient engagement in their action plan of care.27 This highlights a critical need for modifications of health care systems to meet the needs of patients with COPD to better manage its impact through comprehensive care and treatment options.
This study has a number of limitations. Only patients checking into scheduled health care appointments on the Phreesia platform could participate in this survey after completing their check-in. Patients who did not have or were unable to access health care did not have the opportunity to participate; therefore, the survey sample may not be representative of the overall COPD population in the United States. Some of the survey questions were asked on a general level, such as the question on how well patients understood their COPD, and, therefore, may not reflect patients’ understanding of key issues related to COPD. Additionally, the survey questions did not ask patients which specific type of provider they visited, which would allow for more specific insight into how each type of HCP manages patient care. Patient smoking status was also not queried by the survey. In future surveys, more specific questions related to these topics will allow for a more nuanced understanding of patient perceptions and HCP practices. Lastly, the patient sample was skewed White and non-Hispanic, though the reasons for these racial and ethnic disparities within the context of this study are not known.
Conclusions
The patient burden and impact of COPD are multifaceted, with substantial effects in terms of compromised quality of life, activity impairment, and financial stresses. There is room for improvement in prioritizing patient awareness of COPD so that they can be their own advocates for their care and continually be kept abreast of the most up-to-date treatment and self-management strategies. It is crucial to equip patients with helpful resources to overcome barriers in their treatment journeys. These include providing education about COPD to help facilitate effective HCP discussions and enhance patient understanding of their medication.
Acknowledgments
Author contributions: All authors contributed to the conception of the work, the analysis and interpretation of data, drafting and revising the work critically for important intellectual content, and final approval of the version submitted for publication. Medical writing support was provided by Laura Weber, PhD, CMPP, from Citrus Health Group, Inc. (Chicago, Illinois), and was funded by Verona Pharma, plc (Raleigh, North Carolina) in accordance with Good Publication Practice 2022 guidelines.
Data sharing statement: Aggregate data that support the findings of this study are available from authors ST or JS upon reasonable request.
Declaration of Interest
DM is a consultant to GSK, AstraZeneca, Regeneron, Genentech, and the COPD Foundation, and receives royalties from Up to Date. ST and JS are full-time employees of Phreesia, Inc., and own stock and/or stock options as part of that employment. AD and KA are employees of Verona Pharma, plc, and may hold stock and/or stock options. BK is a consultant for Verona, Regeneron, and GSK and is a speaker for Regeneron.