Running Head: Chronic Lung Disease and Health Care Experiences
Funding Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The survey data collection was sponsored by the COPD Foundation. DLD is supported by K24 HL17190.
Date of Acceptance: July 28, 2025 | Published Online: August 6, 2025
Abbreviations: BE=bronchiectasis; BMI=body mass index; CAAT=Chronic Airways Assessment Test; COPD=chronic obstructive pulmonary disease; NTM=nontuberculous mycobacteria; SD=standard deviation
Citation: Choate R, Aksamit TR, Torrence J, et al. Navigating COPD and bronchiectasis: a COPD Foundation survey of differences in patient-perceived health care experiences by sex. Chronic Obstr Pulm Dis. 2025; 12(5): 399-410. doi: http://doi.org/10.15326/jcopdf.2025.0620
Online Supplemental Material: Read Online Supplemental Material (223KB)
Introduction
Chronic lung diseases are among the leading causes of morbidity and mortality, posing substantial public health challenges both in the United States and globally.1 Conditions such as chronic obstructive pulmonary disease (COPD) and bronchiectasis (BE) exhibit notable sex differences in disease prevalence, progression, and severity, which are partly attributable to biological sex-related variations in lung development and physiology between males and females.2,3 However, patient-perceived differences in health care experiences, disease burden, and diagnostic delay by sex remain underexplored.
Historically, COPD was considered a predominantly male disease associated with tobacco smoking and was often under- or misdiagnosed in women, even when they presented with respiratory symptoms.4,5 Recent evidence indicates that COPD is not only highly prevalent in women but may also manifest with greater severity, influenced by factors such as smoking, occupational exposures, indoor air pollution, and susceptibility to these exposures.6 Additionally, the underdiagnosis of COPD in women may result from delayed health care access or engagement, leading to inadequate testing, delayed diagnosis, and suboptimal management.7,8
BE, unrelated to cystic fibrosis, is predominantly a female-prevalent obstructive lung disease across diverse age groups and etiologies.5 The reasons for this sex disparity remain unclear but are thought to involve greater susceptibility to small airway inflammation and a higher prevalence of nontuberculous mycobacteria (NTM) infections in females.5 Research has shown that patients with BE often experience significant diagnostic delays, which are particularly pronounced in women and frequently lead to disease progression, a decline in lung function, and increased exacerbation rates.9
Disparities in patient-reported outcomes, such as quality of life, perceived symptom severity, and health care experience, are increasingly recognized as being associated with sex.4,10,11 Women with COPD, for example, report greater dyspnea, higher levels of anxiety, and lower self-perceived quality of life compared to men.12,13 Understanding patient perspectives, such as their experiences with diagnostic timeliness, the perceived burden of disease, and the impact of chronic lung conditions on the mental and physical quality of life, is essential to advancing knowledge of these conditions.14 Gaps remain in understanding both similarities and differences in these experiences, highlighting the need for further evaluation and research.
The primary objective of this study was to describe self-perceived experiences in men and women related to their diagnosis of chronic lung disease.
Methods
Study Design
This cross-sectional study employed a survey-based approach to evaluate factors associated with differences in health perceptions and health care experiences among individuals with self-reported COPD, BE, NTM infections, or any combination of these conditions. Participants were primarily recruited from the COPD Foundation’s online community platform, COPD360social, which facilitates dialogue, advocacy, and connection among its 60,100 U.S.-based and international members.15 Recruitment efforts were supplemented via other COPD Foundation social media platforms, including Facebook, Instagram, X (formerly Twitter), and LinkedIn. The survey was developed using SurveyMonkey and disseminated using 4 advertisement styles across 17 social media posts from March 15, 2024 to April 12, 2024. Data collection remained open until April 22, 2024.
Questionnaire Development
The survey was designed by a multidisciplinary steering committee comprising COPD Foundation leadership, clinicians with expertise in lung disease research, patient stakeholders, and other researchers. The 33-item survey invited participation from individuals who self-reported a diagnosis of COPD, BE, or NTM.
For the purposes of this study, participants were categorized into 2 groups: (1) a COPD group, which included all individuals who reported a diagnosis of COPD, regardless of the presence of bronchiectasis or NTM, and (2) a bronchiectasis group, which included individuals who reported a diagnosis of bronchiectasis or NTM but did not report having COPD. The survey included questions about respondents’ sex assigned at birth. For the purposes of this manuscript, we use the terms sex, male, man, female, and woman.
The survey primarily assessed participant-perceived health care experiences related to diagnosis and disease management, self-reported symptoms and comorbidities, and disease-related burden. For example, participants were asked whether their health care provider explained their diagnosis in a way that they understood, with possible answers of explained, not explained at all, and explained in a way they did not understand. Treatment burden was assessed using the question, “How do you feel about the burden of disease management and/or therapy?” with responses rated on a Likert scale ranging from “0=no burden” to “5=very burdened.” The Chronic Airways Assessment Test (CAAT) was included to assess the overall health impact of lung conditions.16 The CAAT score ranges from 0 to 40, with higher scores indicating a greater impact of chronic airway disease on an individual’s health and well-being. Women were also asked menopause-related questions.
Ethical Considerations
Participants were informed that completing the survey constituted their consent to participate, therefore, no formal further informed consent process was required. Participants could optionally provide their contact information for follow-up opportunities. The Western Institutional Review Board granted the study an exemption status on March 4, 2024. Survey data were de-identified prior to analyses to ensure confidentiality.
Statistical Analysis
Descriptive statistics were calculated, with categorical variables presented as frequencies and proportions and continuous variables as means and standard deviations. Data were stratified by sex and by the type of lung conditions reported by participants. Values across sexes and lung condition groups were compared using t-tests for continuous variables and Chi-square or Fisher’s exact tests for categorical variables. The significance level for all analyses was set at 0.05. Given the exploratory nature of this observational study, no adjustments for multiple comparisons were applied. We used SAS software, Version 9.4, to perform the analyses.
Results
Characteristics of the Study Sample
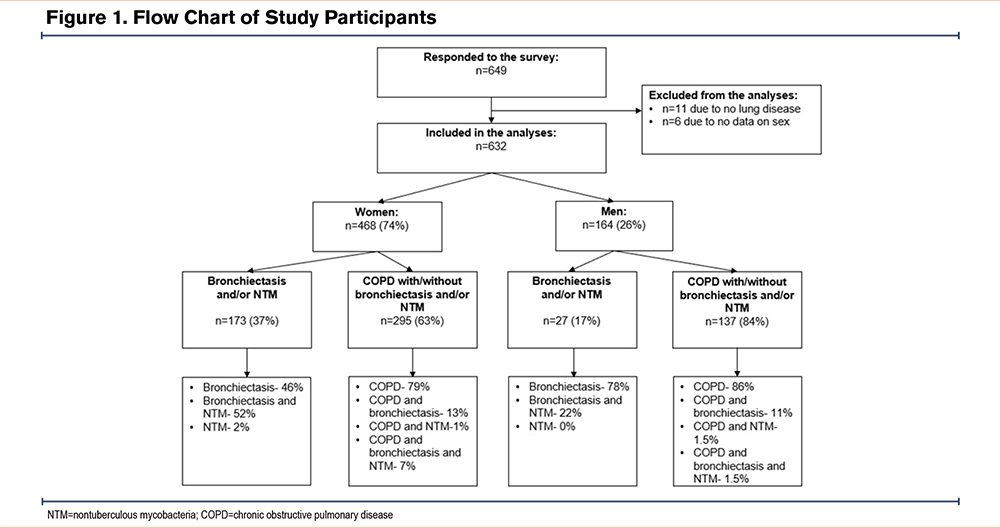
A total of 649 individuals with self-reported COPD, BE, or NTM responded to the survey during the 38-day data collection period. Of these, 632 were included in the final analyses, while 17 were excluded for reasons detailed in Figure 1.
Over 80% of respondents reported the United States as their primary residence, followed by the United Kingdom (6.5%) and Canada (4.6%), with smaller proportions representing other countries worldwide. Among U.S. participants, individuals resided in 45 different states.
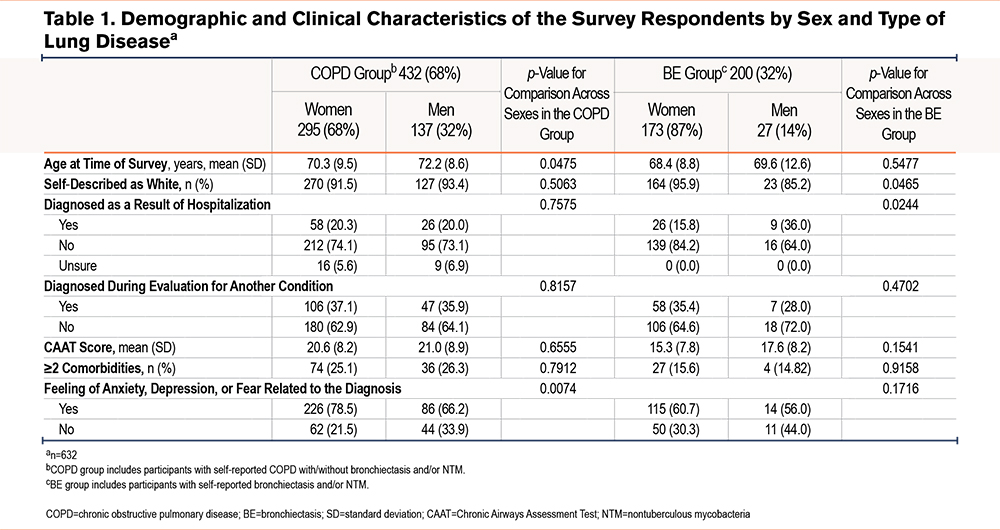
Women comprised 74% of respondents (n=468), with 63% reporting COPD (with or without BE or NTM) and 37% reporting BE (with or without NTM). Among men, who accounted for 26% of respondents (n=164), 83.5% reported COPD and 16.5% reported BE. Men with COPD were slightly older than women (72.2±8.6 versus 70.3±9.5, p=0.0475), and no age difference by sex was noted in the BE group (Table 1).
Health Care Utilization and Diagnosis
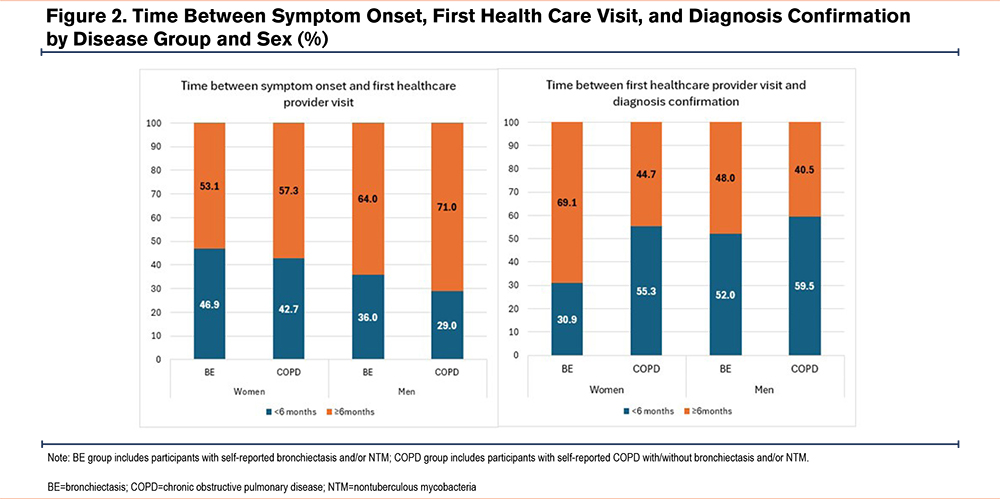
Time from onset of symptoms to first health care visit differed between men and women with COPD and BE (Figure 2). In BE, 47% of women had their first health care visit within 6 months of symptom onset compared to 36% of men, although the overall number of men with BE was low. This difference was even more pronounced and statistically significant in participants with COPD (43% of women versus 29% of men, p=0.0078). Conversely, the time from a first health care visit to a confirmed diagnosis was reversed. Only 31% of women with BE received a confirmed diagnosis within 6 months of their first health care visit, compared to 52% of men (p=0.0376). For COPD, these proportions were similar (55% of women and 60% of men).
In the BE group, more women were diagnosed during evaluation for another condition compared to men (35% versus 28%), while significantly more men were diagnosed during hospitalization (36% versus 16%, p=0.0244). For COPD, the diagnosis setting was more comparable across the sexes (Table 1).
Communication and Resources
When asked, “When you were first diagnosed, did the health care provider explain your diagnosis in a way you understood?”—with response options including “not explained,” “not explained in a way I understood,” and “explained in a way I understood”— most respondents (65%–83%) indicated that their provider explained the diagnosis in an understandable manner. However, a substantial proportion (17%–35%) reported that the explanation was either unclear or entirely absent (Table 2). Among individuals with COPD, more women than men reported not receiving any explanation of their diagnosis (not explained at all; 27% versus 18%, p=0.0381). Conversely, more men than women reported receiving an explanation they did not understand (16% versus 9%). In the BE group, more women reported either not receiving an explanation or receiving one they did not understand compared to men (14% versus 8% for both).
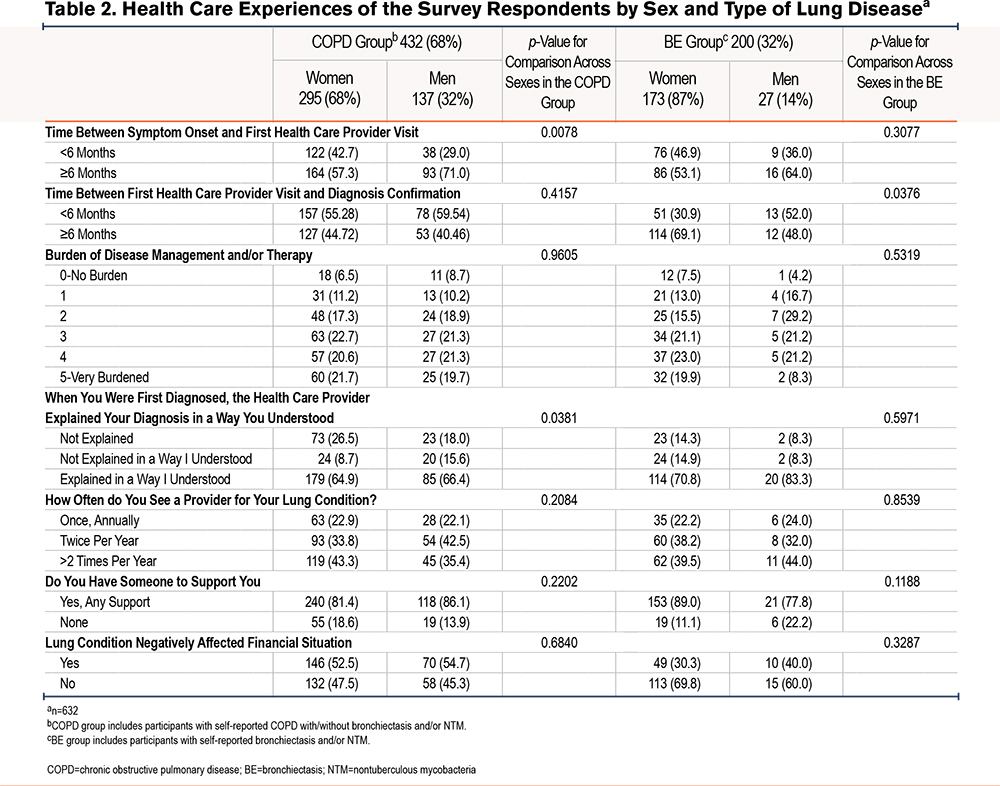
The frequency of pulmonary health care provider visits was similar across conditions and sexes, with 2 or more visits per year being the most common (Table 2). Educational brochures and verbal consultations were the most provided resources, though 37%–46% of respondents reported receiving no resources (Supplemental Table 1 in the online supplement).
Disease Burden and Support Systems
Perceptions of disease management burden were generally similar across groups. However, men with BE reported lower levels of burden, with fewer describing themselves as "very burdened" compared to other groups (Supplemental Figure 1 in the online supplement), though the sample size for men with BE was small.
In the overall cohort, perceived treatment burden decreased with age in both men (p=0.0045) and women (p=0.0095). When comparing by number of comorbidities, men (but not women) with 2 or more comorbidities reported higher perceived treatment burden than those with fewer comorbidities (p=0.0289) (Supplemental Table 2 in the online supplement).
Most participants reported having a support system, primarily comprising life partners or family members. However, 22% of men with BE and 19% of women with COPD reported having no support. Financial strain was more frequently reported by individuals with COPD, regardless of sex, compared to those with BE.
Clinical Characteristics and Symptoms
The clinical characteristics and self-reported comorbidities of the study participants are outlined in Supplemental Table 1 in the online supplement. Participants selected relevant comorbidities from a predefined list provided in the survey. Among the listed conditions, osteoarthritis was the most prevalent condition in women (29% in BE, 32% in COPD), while coronary artery disease was most common in men (15% in BE, 13% in COPD). Multimorbidity was more prevalent in participants with COPD (25% of women, 26% of men) compared to those with BE (16% of women, 15% of men), with no clear sex difference.
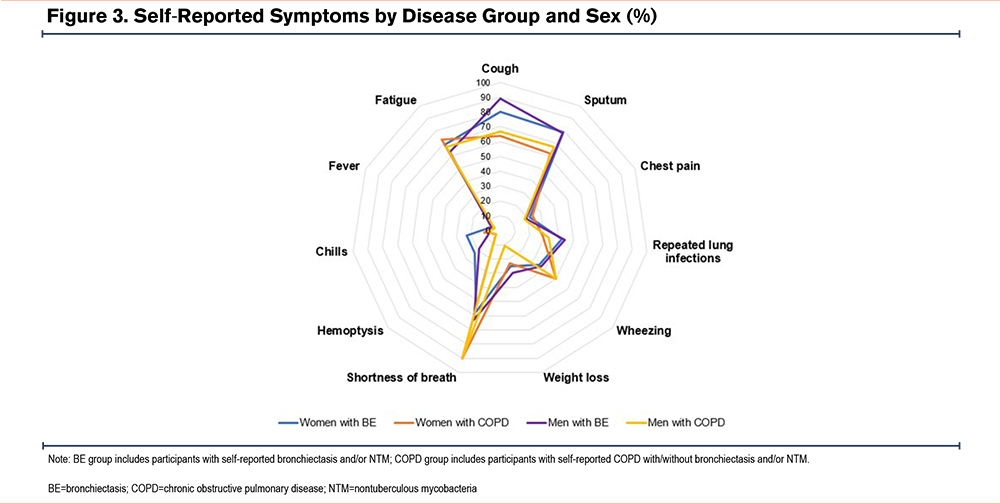
The most common symptoms across groups were shortness of breath, cough, sputum production, and fatigue (Figure 3). Shortness of breath was more prevalent in individuals with COPD (90% in both sexes), while cough and sputum production were more common in those with BE, with men reporting more cough than women. Fatigue was highly prevalent across all groups (63%–73%). The mean CAAT score was higher in participants with COPD (men: 21±9, women: 21±8) compared to those with BE (men: 18±8, women: 15±8), with no differences by sex.
Psychological Impact
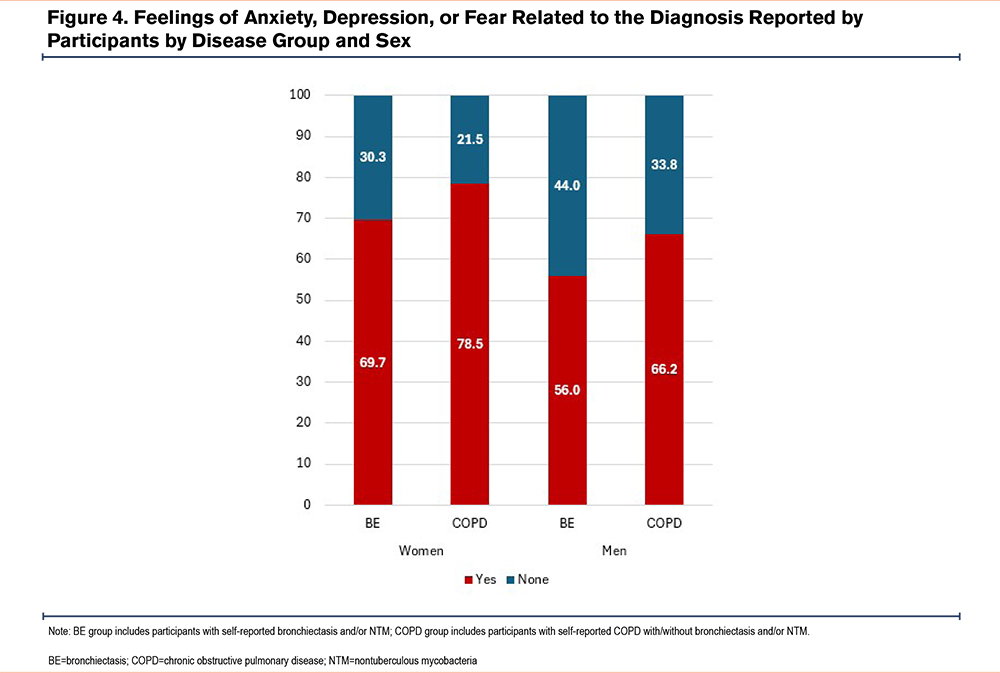
A high proportion of respondents reported experiencing anxiety, depression, or fear related to their diagnosis (Figure 4). These feelings were more commonly reported in women (61% in BE and 78% in COPD) than in men (56% in BE and 66% in COPD), with a significant difference by sex in COPD (p=0.0074). There was no association between receiving support and experiencing anxiety, depression, or fear across the diagnoses by sex.
Menopause-Related Findings
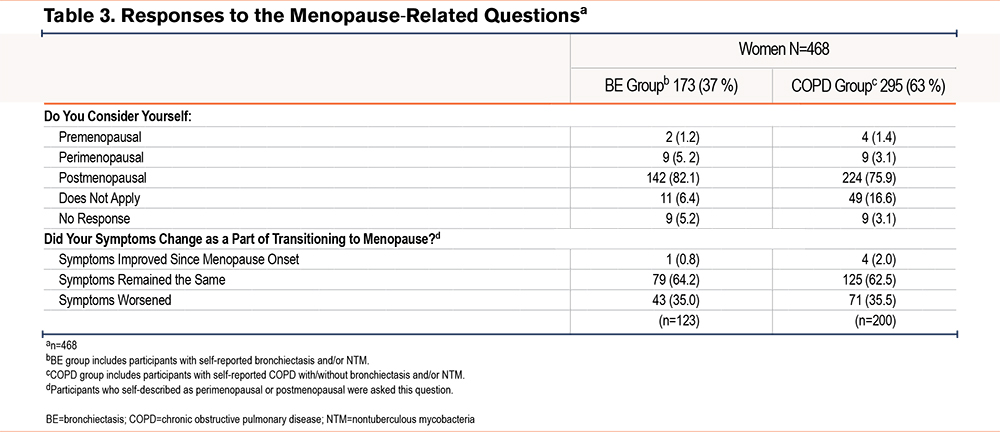
Among women who answered menopause-related questions, most were postmenopausal (82% with BE, 76% with COPD). Over one-third of perimenopausal and postmenopausal women reported worsening pulmonary symptoms during the transition to menopause (35% with BE, 36% with COPD) (Table 3). Women who experienced symptom worsening had higher CAAT scores (20.8±7.8) compared to those without worsening (18.4±8.4, p=0.0108), indicating a greater impact of lung disease on overall health and well-being. Postmenopausal women with worsening symptoms reported a higher prevalence of all evaluated symptoms, particularly weight loss and chest pain. Women with BE experiencing worsening of symptoms more frequently reported repeated lung infections, chills, and weight loss, while those with COPD experienced more chest pain, weight loss, and fatigue (data not shown). There was no difference in the average number of reported comorbidities in women with and without worsening of symptoms during menopause in both disease groups.
Discussion
This observational study successfully recruited and surveyed participants through the COPD Foundation’s online community platform, COPD360social, and other social media-based resources to gather their perspectives on experiences with diagnosis, disease management, and the impact of their lung condition on overall health status. We evaluated participant responses according to their lung condition and sex. We incorporated a patient-centric approach to enhance our understanding of the variability of health care experiences in people with chronic lung diseases.
Our study included a high prevalence of women in both disease groups: COPD (68.3%) and BE (86.5%) in our study population. The predominance of women with BE aligns with findings from previous studies and cohorts and a global prevalence5,17,18of approximately 70%. While historically, COPD has been reported as more prevalent in men, extensive research suggests that sex differences in COPD prevalence are narrowing in economically advanced countries, likely due to similar lifestyles and risk factors across sexes in these regions.12,19 The higher prevalence of women with COPD in our sample may be attributed to the convenience sampling method and potentially greater research engagement among women.
In our study, women were younger than men in both disease groups, with this difference being particularly pronounced in COPD, consistent with findings from previous research.2,13,20 BE is more commonly reported in middle-aged women, whereas its prevalence in men surpasses that of women in older age groups.21,22
Diagnostic delay is common in chronic respiratory conditions.9 Research highlights significant diagnostic disparities in COPD diagnosis between men and women, partly attributed to physician bias, with men being more readily diagnosed with COPD than women.7 Sex differences in symptom reporting and health care utilization may also contribute to these disparities.7 However, some studies suggest that these differences are more related to the underuse of spirometry in primary care, which delays timely diagnosis and contributes to both under- or misdiagnosis of COPD.7
In our study, more women with COPD and BE than men with COPD and BE reported visiting health care providers within 6 months of symptom onset. However, a greater proportion of men with COPD or BE had their diagnosis confirmed within 6 months of seeking care. This finding is consistent with studies showing sex differences in perceptions of interactions with the health care system.11 For instance, women with COPD often report experiencing greater delays in diagnosis compared to men. This may be due to challenges in accessing health care or differences in how likely individuals are to recognize and seek care for their symptoms.11
For individuals with BE, research shows that obtaining an accurate diagnosis often takes years from symptom onset, reflecting substantial diagnostic delays.23 A study of the Spanish Historical Registry of Bronchiectasis revealed an average diagnostic delay of 12 years, with women experiencing an even longer delay—2.1 years more than men.23 In addition, patients with BE frequently report difficulties accessing health care, particularly specialist care.9
Patient-perceived disease burden in COPD is influenced by multiple factors, including symptom severity, the disease's impact on physical and psychological health, daily functioning, and overall quality of life.24,25 Evaluating patients’ real-world experiences and self-reported perceptions is essential for understanding the full impact of chronic lung diseases on individuals. To quantify this burden, patient-reported outcome measures, such as CAAT, were developed to capture patients’ perspectives on how the disease affects their lives.26 In our study, the mean CAAT score in the COPD group was 21, indicating a high disease burden on overall well-being. In the BE group, mean CAAT scores ranged from 15 to 18 across sexes, reflecting a moderate impact on health. These findings emphasize the importance of incorporating patient-reported outcomes into clinical care to better understand and address the challenges faced by individuals living with chronic respiratory conditions.
Among respondents with COPD, dyspnea was the most reported symptom, affecting 90% of both men and women. Previous studies have demonstrated that women with COPD experience more frequent and severe dyspnea compared to men, regardless of pulmonary function.27 This elevated dyspnea severity in women has been linked to greater airway hyperresponsiveness, hormonal influences, and higher rates of anxiety and depression.28,29
In the BE group, cough was the most prevalent symptom, reported more frequently by men (89%) than women (80%). Recurrent productive cough is a hallmark feature of BE, often accompanied by fatigue and a significantly reduced quality of life.30 Notably, published studies indicate that women with BE experience more intense coughing than men. One study, for example, found that female patients with BE had significantly higher cough counts over a 24-hour period compared to their male counterparts.31
Interestingly, our study participants reported a high prevalence of weight loss and fatigue. Weight loss was more commonly reported by participants with BE (25%–30%) compared to those with COPD (11%–23%). Fatigue also emerged as one of the most prevalent symptoms by sex and disease groups in this population, with women reporting higher levels of fatigue than men. Notably, both weight loss and fatigue are key components of frailty assessment in older adults, forming 2 of the 5 items in the FRAIL questionnaire.32 Studies have further demonstrated a significant association between frailty and dyspnea in older adults with chronic lung conditions, showing that dyspnea severity increases with greater levels of frailty.32 The role of frailty in predicting adverse outcomes in older patients with respiratory diseases is gaining recognition as an important consideration in clinical care; sex differences in frailty in people with COPD are a critical area for further investigation.
Over one-quarter of survey respondents with COPD reported having 2 or more comorbidities, meeting the definition of multimorbidity. In contrast, the prevalence of multimorbidity in the BE group was lower, at 15%–16%. Among both disease groups, osteoarthritis was the most commonly reported comorbidity among women (29%–32%). Published research supports these findings, indicating that women with COPD are more likely than men to develop osteoporosis and often at a younger age.33 Consequently, women receiving corticosteroid treatment for COPD should be closely monitored for bone density and the potential development of osteoporosis.33
Interestingly, men with COPD are more likely to develop cardiovascular disease compared to women.33 Our findings align with this research, as 15% of men with COPD reported having congestive heart failure, compared to 10% of women. Additionally, 5% of both men and women with COPD reported having lung cancer. Studies highlight the high incidence of lung cancer in individuals with COPD, which is associated with oxidative stress from cigarette smoking, chronic inflammation, and genetic susceptibility.34
Research also indicates that women diagnosed with COPD experience a more rapid decline in lung function and higher rates of hospitalizations, exacerbations, and mortality compared to men with similar smoking histories.35 Similarly, women diagnosed with lung cancer tend to experience more aggressive disease progression and shorter survival, partly due to the effects of estrogen.35 Timely lung cancer screening is critical for women, especially those who may not meet traditional tobacco exposure eligibility criteria, to ensure early diagnosis and treatment.35
In addition to physical comorbidities, individuals with COPD frequently experience psychological conditions such as anxiety and depression, which significantly impair quality of life and overall health status.36 Women with COPD are more likely than men to develop anxiety and depression, conditions often linked to loneliness and the severity of dyspnea, and associated with increased risks of mortality, exacerbations, and hospitalizations.36 In our study, participants across sex and disease groups reported a high prevalence of anxiety, depression, or fear related to their diagnosis, with women with COPD experiencing the highest rates of psychological comorbidities; this is an under-addressed area of COPD care that needs multidisciplinary efforts.
Positive social support from a partner, friend, family member, or health care professional plays a critical role in promoting positive health behaviors and fostering self-management in chronic lung conditions like COPD.37 Conversely, a lack of social support can lead to isolation, loneliness, and a declining quality of life. While most participants in our study reported having a support system, approximately 20% of women with COPD and men with BE reported lacking social support. Interestingly, in our study population, the absence of a support system was not associated with the prevalence of anxiety or depression in individuals with COPD or BE.
In women with chronic lung diseases, the transition to menopause and its timing can significantly affect respiratory health and may accelerate lung function decline.38 In COPD, key risk factors associated with the impact of menopause include early menopause, smoking, and BMI.8,38 Additionally, BE and NTM infections have been reported to occur more frequently and present more aggressively in postmenopausal women, potentially due to a drop in progesterone levels after menopause.39
A multinational study highlights an increase in pulmonary symptoms and a decline in lung function during the menopause transition, particularly among lean women with a BMI<23kg/m2, which may be linked to increased insulin resistance, recognized as a pro-inflammatory condition during menopause.40 In our study, over three-quarters of the female respondents were postmenopausal, and nearly one-third of these women reported a worsening of pulmonary symptoms during the menopause transition. These findings underscore the importance of considering menopause status—including age of onset of menopause, use of hormone replacement therapy, and BMI—in clinical trials and longitudinal studies. Addressing these factors is essential for accurately evaluating the impact of menopause on respiratory health and informing tailored approaches to treatment and management in women with chronic lung diseases. In addition, these findings highlight an opportunity to improve the care of women with COPD through collaborations with clinicians (e.g., primary care, gynecologists, endocrinologists) focused on midlife and menopause-related care.
Strengths and Limitations
One of the key strengths of our study is its large sample size and the diverse recruitment of participants, which ensured broad geographic representation. The high proportion of women in both the COPD and BE groups provided a valuable opportunity to explore sex-related differences in health care experiences, symptom reporting, diagnosis, and disease management in detail. Additionally, our study’s unique focus on patient-reported outcomes highlights real-world, patient-centered experiences, addressing an area often underrepresented in clinical research.
However, the findings should be interpreted with consideration of several limitations. Recruitment through online platforms and social media may have introduced selection bias, as participants are likely to be more health-conscious or have greater access to digital resources, which limits the generalizability of the results to the broader population. The reliance on self-reported diagnoses, symptoms, and health care interactions may have led to recall bias and potential misclassification, particularly regarding the timing and accuracy of diagnoses. The study’s observational and cross-sectional design precludes any causal inferences. Moreover, unmeasured confounding factors, such as socioeconomic status, health care access, or cultural differences, may have introduced bias into the findings. In addition, participants with BE and/or NTM were grouped together for analysis, which may obscure important clinical distinctions between these conditions. Although the majority of individuals in this group had BE alone, and NTM disease often co-occurs with BE, we acknowledge that BE and NTM are not equivalent conditions and that this analytic approach may limit the specificity of findings related to either condition. The relatively small subgroup of men with BE warrants cautious interpretation of any conclusions drawn about this group. Finally, as this was an exploratory observational study, adjustment for multiple comparisons was not performed.
Conclusion
Our study reveals differences in symptom burden, comorbidities, and health care experiences in COPD and BE, with women reporting greater challenges and delays in care. Postmenopausal symptom worsening underscores the need to consider hormonal factors in research, treatment, and multidisciplinary care of women. Patient-reported outcomes highlight the substantial impact of COPD and BE on quality of life, emphasizing the importance of addressing these challenges through patient-centered care strategies and patient education.
Acknowledgments
Author contributions: TRA, JT, PAD, JW, and DLD contributed towards conception and design of the study. AR and BM contributed to data interpretation. RC contributed to data analyses, interpretation, and manuscript writing. DLD provided critical interpretation of the data and contributed towards manuscript preparation. All authors have contributed substantially to the manuscript and have reviewed and approved the manuscript before submission for publication.
Declaration of Interest
RC, PD, JT, BM, AR, TRA, and JW declare no conflicts relevant to this work.
DLD has received support from the National Institutes of Health, the Alpha-1 Foundation, and Bayer.